Abstract
Objective
To evaluate the potential utility of 18F-FDG PET/CT to assess response to neoadjuvant immunochemotherapy in patients with resectable NSCLC, and the ability to screen patients who may benefit from neoadjuvant immunochemotherapy.
Methods
Fifty one resectable NSCLC (stage IA–IIIB) patients were analyzed, who received two-three cycles neoadjuvant immunochemotherapy.18F-FDG PET/CT was carried out at baseline(scan-1) and prior to radical resection(scan-2). SULmax, SULpeak, MTV, TLG, T/N ratio, ΔSULmax%,ΔSULpeak%, ΔMTV%, ΔTLG%,ΔT/N ratio% were calculated. 18F-FDG PET/CT responses were classified using PERCIST. We then compared the RECIST 1.1 and PERCIST criteria for response assessment.With surgical pathology of primary lesions as the gold standard, the correlation between metabolic parameters of 18F-FDG PET/CT and major pathologic response (MPR) was analyzed. All metabolic parameters were compared to treatment response and correlated to PFS and OS.
Results
In total of fifty one patients, MPR was achieved in 25(49%, 25/51) patients after neoadjuvant therapy. The metabolic parameters of Scan-1 were not correlated with MPR.The degree of pathological regression was negatively correlated with SULmax, SULpeak, MTV, TLG, T/N ratio of scan-2, and the percentage changes of the ΔSULmax%, ΔSULpeak%, ΔMTV%,ΔTLG%,ΔT/N ratio% after neoadjuvant therapy (p < 0.05). According to PERCIST, 36 patients (70.6%, 36/51) showed PMR, 12 patients(23.5%, 12/51) had stable metabolic disease(SMD), and 3 patients(5.9%, 3/51) had progressive metabolic disease (PMD). ROC indicated that all of scan-2 metabolic parameters and the percentage changes of metabolic parameters had ability to predict MPR and non-MPR, SULmax and T/N ratio of scan-2 had the best differentiation ability.The accuracy of RECIST 1.1 and PERCIST criteria were no statistical significance(p = 0.91). On univariate analysis, ΔMTV% has the highest correlation with PFS.
Conclusions
Metabolic response by 18F-FDG PET/CT can predict MPR to neoadjuvant immunochemotherapy in resectable NSCLC. ΔMTV% was significantly correlated with PFS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Lung cancer is the most common cause of cancer death worldwide [1, 2]. More than 70% of patients are already locally advanced at the time of diagnosis. Non-small cell lung cancer(NSCLC) accounts for approximately 80–85% of all lung cancers [3]. Immunotherapy, as a new adjuvant therapy, has shown encouraging efficacy and can restore the function of existing anti-tumor T cells. Chemotherapy enhances anti-tumor immunity through direct or indirect activation of the immune system [4, 5]. Neoadjuvant therapy can reduce tumor burden, increase R0 rate and improve survival rate.In recent years, with the emergence of PD-L1 inhibitors, the strategy of chemotherapy combined with PD-L1 inhibitors has changed the treatment prospects of non-small cell lung cancer [6,7,8]. The CheckMate 816 study showed that neoadjuvant nivolumab plus chemotherapy significantly improved event-free survival and pathological complete response (pCR) rates compared with chemotherapy alone in patients with resectable NSCLC [7].
Immunotherapy is notoriously expensive, and chemotherapy can cause adverse events such as vomiting and diarrhea in patients [9]. Due to the significant difference between the clinical management strategies of responders and non-responders, there is an urgent need for early assessment of patients who benefit from neoadjuvant immunochemotherapy before or during chemotherapy, and even to predict the treatment response. Finding suitable non-invasive methods is a major problem in clinical practice. 18F-fluorodeoxyglucose(FDG)-positron emission tomography/computed tomography (PET/CT) is a useful and non-invasive method to assess tumor size and glucose metabolic status and is widely used to assess tumor stage and treatment response [10,11,12]. It is very important to evaluate the effectiveness of neoadjuvant immunochemotherapy in NSCLC patients. Misjudgment may lead to wrong decision of next treatment. In particular, there are inconsistencies between CT response assessment criteria and histopathological response in solid tumors. In a meta-analysis, the predictive value of 18F-FDG PET/CT for pathological response after neoadjuvant therapy was significantly higher than that of CT scan in NSCLC patients [13]. In addition, 18F-FDG PET/CT was considered to provide more useful information for assessing the response to immunotherapy of advanced NSCLC in recent research [1, 14, 15]. At present, there are very few studies on 18F-FDG PET/CT in the evaluation of neoadjuvant immunochemotherapy in NSCLC patients. Therefore, the purpose of this study is attempt to evaluate the potential of 18F-FDG PET/CT to assess response to neoadjuvant immunochemotherapy in patients with resectable NSCLC.
Materials and methods
Patients
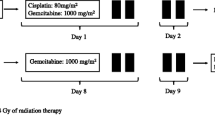
We retrospectively reviewed NSCLC patients underwent 18F-FDG PET/CT at baseline(scan-1) and prior to surgery(scan-2) from January 2019 to June 2022 at our hospital. The inclusion criteria included the following: (1) Patients had histologically or cytologically confirmed NSCLC (stage IA–IIIB, AJCC 8th), with negative driver mutations(EGFR mutation and ALK rearrangement); (2) received 2–3 cycles of intravenous toripalimab (240 mg) or pembrolizumabon(200 mg) IV q 2-3wks added to nab-paclitaxel (100 mg/m2) IV q 2-3wks or pemetrexed (500 mg/m2) IV q 2-3wks plus cisplatin 75mg/m2 IV q 2-3wks before surgical resection 2 wks; (3) neoadjuvant immunochemotherapy was between scan-1 and scan-2 and patients underwent surgery after neoadjuvant therapy. The exclusion criteria included the following: (1) stage IV non-small cell lung cancer; (2) neoadjuvant immunochemotherapy regimen did not meet the inclusion criteria; (3) The patient did not undergo 18F-PET/CT imaging before and after neoadjuvant therapy; (4) The participants were ultimately unable to undergo surgery. Finally, 51 resectable NSCLC patients (6 female and 45 male) with a mean age of 59.80 ± 8.57 years (range: 26–74 years) were enrolled in this study. PET responses were classified using PERCIST criteria [16]. Since this study is retrospective, national laws require neither institutional review board approval nor informed consent.
PET/CT examination
All patients underwent whole-body PET/CT acquisition 60 ± 10 min after injection 18F-FDG by 3.7 MBq/kg. Prior to FDG injection, all patients fasted for at least 6 h. In all cases, the serum glucose concentration met the institutional requirement (≤ 120 mg/dL).
PET/CT scans were performed by Siemens Biograph mCT Flow 64 scanner (Siemens, Erlangen, Germany) which covered the length from the top of skull to the mid-thigh. A low-dose CT scan (120 kV, 35 mA, slice 3 mm) was first performed, and PET acquisition speed was 1.5 mm/s (slice 3 mm, filter: Gaussian, FWHM: 5 mm). A Siemens Biograph mCT Flow 64 scanner PET images were reconstructed using a three-dimensional iterative reconstruction with the time-of-flight algorithm, and the low-dose CT scans were acquired in CARE Dose 4D mode. A Gemini TF scanner PET reconstruction parameters included use of 3D model, and use of ordered-subcohorts expectation maximization(OSEM) method (two iterations, four subcohorts, 128 × 128 pixels of 5.15 mm). Attenuation corrections of the PET images were performed using data from CT imaging.
Image analysis
A Siemens workstation (Syngo.via VB20, MM Oncology) was used for analyzing all images. Two experienced nuclear medicine practitioners reviewed and analyzed the 18F-FDG PET/CT, enhanced CT independently, and any inconsistencies were resolved by consensus.
Volumes of interest (VOIs) were manually drawn for each lesion and the metabolic parameters by lean body mass (SULmax, SULpeak, metabolic tumor volume(MTV), total lesion glycolysis (TLG) and T/N ratio)were automatically calculated. The axial, coronal, and sagittal 18F-FDG PET/CT images were qualitatively analyzed by nuclear medicine physicians. The post-treatment percentage changes of metabolic parameters calculated were recorded. In the case of ΔSULpeak%, the formula is as follows: ΔSULpeak% = ( SULpeak of scan-1-SULpeak of scan-2)/SULpeak of scan-1 × 100%. According to PERCIST, response to the neoadjuvant therapy was defined as (1) complete metabolic response (CMR); (2) partial metabolic response (PMR); (3) progressive metabolic disease (PMD); (4) stable metabolic disease (SMD).
The enhanced CT scan was performed before the start of immunochemotherapy and before surgery, respectively. The primary of lung cancer was evaluated with the solid tumor response evaluation standard (RECIST) 1.1. The criteria were as follows: complete response (CR), the lung lesions disappeared; Partial response (PR), the diameter of the lung lesion decreased by at least 30%; Disease progression (PD): the diameter of lung lesions increases by at least 20% or new lesions appear; Disease stability (SD) is neither CR nor PR or PD.
All histological sections were reviewed by two experienced pathologists in accordance with the guidelines recommended by the International Association for the Study of Lung Cancer (IASLC) for pathological evaluation of resected lung cancer specimens after Neoadjuvant Therapy.MPR defined as 10% or less of viable residual tumour, which was assessed by pathologists who measured the percentage of residual viable tumour in resected primary tumours from each patient after surgery.
Follow-up surveillance
Progression-free survival (PFS) is calculated from the start date of treatment to the date of the first progression (local recurrence or distant metastasis of the tumor) or death from any cause. Overall survival (OS) defined as the time interval from the beginning of induction treatment to death. Evaluate the correlation between metabolic parameters and PFS and OS.
Statistical analysis
Statistical analysis were conducted by using IBM SPSS (Version 22.0, IBM Corporation, New York, USA). All normal distribution data were tested with Kolmogorov-smirnov and homogeneity of variance with Levene test. SULmax, SULpeak, ΔSULmax%, and ΔSULpeak% were approximately normally distributed, while MTV, TLG, T/N ratio,ΔMTV%,ΔTLG% and ΔT/N ratio% were non-normally distributed. The measurment data were described as means ± standard deviation. Independent sample T tests were used to compare SULmax, SULPeak, and their changes with pathological regression, whereas Mann-whitney U tests were used to compare MTV, TLG, and their changes between the two groups. The correlation between metabolic parameters and MPR in primary tumor after neoadjuvant therapy was evaluated by spearmen’s correlation analysis. The value of metabolic parameters for predicting responders were evaluated by receiver operating characteristic(ROC) curve, and area under the ROC curve(AUC) was calulated. The cutoff was determined using the maximum Youden’s method.Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy were calculated. Patients were divided into two categories according to the cutoffs. Kaplan-Meier method and Cox’s Proportional Hazard Model were employed. Statistical significance was set at P < 0.05 .
Results
Patient characteristics
From January 2019 to June 2022, a total of 51 NSCLC patients(45 males and 6 females, the mean age 59.8 ± 8.6 years old)met the requirements for our study. Among 51 enrolled patients, most of them were male (45/51, 88.2%) ,30 patients received toripalimab added to nab-paclitaxel or pemetrexed plus cisplatin, and 21 patients received pembrolizumabon added to nab-paclitaxel or pemetrexed plus cisplatin. 17 patients(17/51,33.3%) received two cycles of immunochemotherapy, and the rest(34/51,66.7%) received three cycles. Squamous cell carcinoma accounted for 70.6%(36/51), and adenocarcinoma accounted for 25.5%(13/51). The clinical information of the 51 patients were summarized in Table 1.
Pathological regression and metabolic parameters
Twenty-five patients(49%, 25/51)pathological regression had achieved MPR, including 21 squamous cell carcinoma and 4 adenocarcinoma, and 18 of these patients achieved pathological complete responses(PCR). Twenty-six patients (51%, 26/51) did not have MPR, but had varying degrees of pathological regression.
Tumour proportion score(TPS), Pathological regression and metabolic parameters of scan-1 and scan-2 after neoadjuvant immunochemotherapy of 51 NSCLC patients were shown in the Supplementary Table S1. There was no statistical significantly between clinical characteristics(gender, age, histology, smoking history, TPS, TNM stage) and MPR. All metabolic parameters of scan-1 had no statistical significant with the degree of pathological regression of lung primary tumor (Table 2). The scan-2 metabolic parameters and the percentage changes of metabolic parameters after neoadjuvant therapy were negatively correlated (p < 0.05) with the tumor regression (Table 3).
The scan-1,scan-2 and the percentage changes of metabolic parameters between MPR and non- MPR were summarized in Table 4. ROC indicated that all of scan-2 metabolic parameters and the percentage changes of metabolic parameters had ability to predict MPR and non-MPR, SULmax and T/N ratio of scan-2 had the best differentiation ability (Table 5). By setting cutoff of SULmax 3.2 and T/N ratio 1.4 of scan-2,the specificity, sensitivity, and accuracy were 84.6%,88.0%,86.3% and 80.8%,88.0% and 84.3%,respectively, with area under curve (AUC) both of 0.94 (p < 0.001).
Association between metabolic response and pathological response
According to PERCIST, the metabolic response were classified as CMR (0%, 0/51), PMR (72.5%, 37/51), SMD (23.5%, 12/51), and PMD (4.0%, 2/51)( Figrue 1) .A typical case is shown in Figrue 2– 4. Of the 37 PMR patients, 25 achieved MPR and 12 achieved non- MPR after neoadjuvant immunochemotherapy (Figrue 5).
A 73-year-old man with squamous cell lung cancer, who had marked metabolic changes on 18F-FDG PET/CT where evaluated as PMR according to PERCIST after three cycles pembrolizumab added to nab-paclitaxel plus cisplatin treatment. (A)The scan-1axial fusion image of lung cancer, SULpeak = 10.0. (B)The scan-2axial fusion image of lung cancer after neoadjuvant therapy, SULpeak = 5.5; ΔSULpeak% = − 45.2%. (C)The surgical pathology showed that MPR was achieved (The residual viable tumor was 5%, less than 10%)
A 54-year-old man with squamous cell lung cancer, who evaluated as SMD according to PERCIST after two cycles toripalimab added to nab-paclitaxel plus cisplatin treatment. (A)The scan-1axial fusion image showed high FDG uptake of nodules in the opening of the left upper lobar bronchus. SULpeak = 9.5. (B)The scan-2axial fusion image of lung cancer after neoadjuvant therapy, SULpeak = 8.7; ΔSULpeak% = − 8.0%. (C)The Resection specimen showed that MPR was not achieved (The residual viable tumor was 80%, more than 10%)
A 53-year-old man with squamous cell lung cancer, who evaluated as PMD according to PERCIST after three cycles toripalimab added to nab-paclitaxel plus cisplatin treatment. (A-B)MIP (maximum intensity projection) image of scan-1 and scan-2, respectively. (C)The scan-1axial fusion image showed high FDG uptake in the left lower lobe near the pulmonary hilum. SULpeak = 10.1; MTV = 25.3; TLG = 150.7. (D)The scan-2 axial fusion image showed that both of ΔMTV% and ΔTLG% were decreased(MTV = 15.2,ΔMTV% = −39.9%; TLG = 100.1,ΔTLG% = − 33.6%), but the SULpeak is higher than that of scan-1(SULpeak = 14.8, ΔSULpeak% = 47.1%). (E) Resection specimen showed this patient had only 15% of pathological regression
The clinical information and all of metabolic parameters of 25 MPR and 12 non-MPR patients were analyzed. The results showed that SULmax, SULpeak, T/N ratio of scan-2 and ΔSULmax%,ΔSULpeak%, ΔT/N ratio were statistically significant for distinguishing MPR from non-MPR(p < 0.001, Table 6). All patients with metabolic SMD and PMD were not acheieved MPR(Figrue 5). Pathology finally revealed that there were 18 patients with no residual lesions (PCR), and the remaining 33 patients had varying degrees of residual lesions.
The clinical information and all of metabolic parameters of 18 PCR and 33 non-PCR patients were analyzed. The results showed that SULmax, SULpeak, MTV, TLG, T/N ratio of scan-2 and ΔSULmax%, ΔSULpeak%, ΔMTV%, ΔTLG%,ΔT/N ratio were statistically significant for distinguishing PCR from non-PCR(p < 0.005, Table 7).
Morphologic (RECIST 1.1) vs. metabolic (PERCIST) criteria
In a total of 51 patients, 15 (29.4%) had inconsistent tumor response evaluation, and 36 (70.6%) were consistent. When the PERCIST criteria was adopted, the tumor response of 8(53.3%) patients was upgraded, and that of 7 (46.7%) patients was degraded (Table 6). Of 15 patients with SD, 7 (46.7%) were reclassified in PMR, while 2 were reclassified in PMD by PERCIST criteria. There was no residual tumor in the primary lung cancer of 18 patients after surgery. These patients were all PMR according to the PERCIST criteria, while four patients were SD according to the RECIST 1.1 criteria.The sensitivity, specificity and accuracy of MRP as the gold standard for diagnosis were 100%, 53.8%, 76.5% and 88%,42.3%,64.7% by PERCIST and RECIST 1.1 criteria, with no statistical significance (P>0.05).
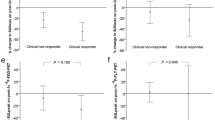
Survival results analysis
The median follow-up was 16 months (95%CI, 14 to 19 months). Using univariate cox regression analysis,ΔSULmax%,ΔSULpeak%, ΔMTV%, ΔTLG%,ΔT/N ratio% from primary lung cancer were associated with PFS (Supplementary Table S2). Among the five univariate factors, ΔMTV% had maximum AUC for predicting responders. Patients were divided into ΔMTV%-defined responders and ΔMTV%-defined non-responders according to the cutoff (ΔMTV%<-70% as responders and ΔMTV%≥70% as non-responders). Kaplan meier curves showed ΔMTV%-defined responders demonstrate statistically better PFS than ΔMTV%-defined non-responders(Figrue 6).
Discussion
With the accumulation of convincing evidence, neoadjuvant immunochemotherapy demonstrates remarkable effectiveness in NSCLC without EGFR/ALK alterations, which has been gradually applied in clinical practice. Traditional imaging evaluation criteria are based on morphological changes [17, 18]. Recent clinical trials and retrospective clinical studies have shown no relationship between treatment response assessed by CT images and MPR [15, 19, 20], while 18F-FDG PET/CT reflects the changes of tumor metabolism level, which is more suitable for systematic evaluation and monitoring of therapeutic effects [21,22,23]. This has been demonstrated in both neoadjuvant chemotherapy and immunotherapy for NSCLC [1, 24,25,26,27]. The lack of reliable predictive imaging markers to evaluate neoadjuvant immunochemotherapy response is a problem that needs to be solved.To date, little is known about the efficacy of 18F-FDG PET/CT to predict response to neoadjuvant immunochemotherapy in patients with resectable NSCLC. In our study, we explored the potential value of 18F-FDG PET/CT in predicting MPR of neoadjuvant immunochemotherapy.
MPR is a commonly used alternative predictor of survival in patients with resectable NSCLC receiving neoadjuvant therapy, both in clinical trials and in the real-world [28, 29]. In our retrospective clinical studies, Nearly half of(49.0%,25/51) the patients achieved MPR after neoadjuvant therapy, which is consistent with previous studies [7]. According to the clinical stage, all NSCLC patients with stage I–III received two-three cycles of immunochemotherapy. We observed more squamous-cell carcinoma patients achieving MPR than adenocarcinoma in our study(84% vs. 16%).In the real world, the majority of male smokers with negative driver mutations, so patients with locally advanced squamous cell carcinoma are more likely than patients with adenocarcinoma to receive neoadjuvant immunochemotherapy. The results of our study have more guiding significance for clinical treatment.
There was a statistically significant association between tumor metabolic parameters on 18F-FDG PET/CT and the expression of PD1/PD-L1 in resected tumor specimens.Previous studies have shown that changes in metabolic activity are associated with tumor response [30, 31]. How to select the appropriate time point for 18F-FDG PET/CT evaluation, and how to evaluate the relationship between the metabolic parameters and the degree of pathological response, these data are worthy of our attention. All patients in our study had some extent degrees of pathological remission after neoadjuvant immunochemotherapy. The scan-2 metabolic parameters and the percentage changes of metabolic parameters of 18F-FDG PET/CT after neoadjuvant immunochemotherapy were negatively correlated with the MPR(p < 0.05) in our research.Unfortunately, the metabolic parameters of tumor on baseline did not correlate with MPR. Previous studies have shown that 18F-FDG PET/CT is an effective methods of monitoring immunotherapy. Our findings suggest that efficacy evaluation should be performed after 2–3 cycles of immunochemotherapy, and SULmax and T/N ratio of scan-2 were the best metabolic parameters to predict MPR. The specificity, sensitivity, and accuracy were 84.6%,88.0%,86.3% and 80.8%,88.0% and 84.3%,respectively.The SULpeak, MTV, TLG of scan-2and all the percentage changes of the metabolic parameters also showed good prediction capabilities to distinguish patients with MPR. Our study showed that 18F-FDG PET/CT can help to determine the population who can benefit from neoadjuvant immunochemotherapy followed by radical surgery. Although the PERCIST criteria were evaluated using SULpeak, our study showed that SULmax was more closely associated with MPR.Compared with SULpeak, SULmax reflects the most metabolically active part of the tumor and is easier to measure in patients after neoadjuvant therapy, especially when the residual lesions are small after treatment [16, 32, 33].
According to PERCIST criteria, 37 patients achieved PMR and 25 of them with MPR.All of SMD and PMD patients with non-MPR. Encouragingly, 18 patients’ primary tumor achieved PCR.This result reflects the real situation of NSCLC patients after neoadjuvant immunochemotherapy in clinical practice. We analyzed all of metabolic parameters of these 37 patients and found that SULmax, SULpeak, T/N ratio of scan-2 and ΔSULmax%,ΔSULpeak%, ΔT/N ratio could help distinguish patients with MPR from non-MPR(p < 0.001). The lower the SULmax, SULpeak and T/N ratio of scan-2, the easier the MPR of the primary lesion was to achieve after treatment. This result may suggest that preoperative 18F-FDG PET/CT is important to evaluate the efficacy of neoadjuvant immunochemotherapy.
We compared PERCIST and RECIST 1.1 criteria to evaluate the response of patients after immunochemotherapy treatment. Of the 15 patients classified as SD according to RECIST 1.1, 6 patients were reclassified as PMR according to PERCIST criteria, 2 patients were reclassified as PMD. More importantly, four patients with no tumor residue were evaluated for PMR by PERCIST and SD by RECIST 1.1. Such changes emphasize that metabolic changes can be detected earlier than morphological changes. SUVmax is the most commonly used metabolic PET/CT parameter, which is based on single pixel value, so cannot well represent the change of FDG uptake distribution in tumor and the overall metabolic state of tumor. Previous studies have proved that volume-based metabolic parameters are significant for the prognosis of primary tumors [34]. Our study demonstrated that ΔSULmax%,ΔSULpeak%, ΔMTV%, ΔTLG%,ΔT/N ratio% from primary lung cancer were associated with PFS, and ΔMTV% was most closely related to PFS. Interestingly, these metabolic parameters were also correlated with patients achieving PCR. Therefore, we recommend measuring ΔMTV% to predict pathological complete response and PFS in NSCLC patients. The metabolic parameter MTV has been used to predict the outcome of NSCLC treatments, including pre-operative [35], chemoradiotherapy [36], chemotherapy [37], and targeted therapy [38].Because there were no death events in all patients, the correlation between OS and metabolic parameters was not studied.
Lopci et al. reported a direct association between the metabolic parameters of 18F-FDG PET/CT and the expression of PD-L1 and PD-1 in NSCLC patients [7, 15, 39, 40]. Some studies have shown that even NSCLC patients who have low or negative expression of PD-L1 may benefit from neoadjuvant immunotherapy combined chemotherapy. Our results suggest that patients with tumor PD-L1 expression level of 1% or more than or those with PD-L1 expression level of less than 1% had different degrees of pathological remission. There was no statistical significance between the expression degree of TPS and MPR. These results may suggest that the implementation of neoadjuvant immunochemotherapy may not depend on the expression level of TPS.
Although some studies have reported that neoadjuvant immunotherapy plus chemotherapy has a better effect on NSLCL than chemotherapy alone, there are few reports on 18F-FDG PET/CT immunotherapy plus chemotherapy. Previous studies have reported that the antitumor activity of immunotherapy is related to the activation of T cells against cancer cells. Therefore, inflammatory changes secondary to the aggregation of macrophages, neutrophils, and lymphocytes may lead to false positive results. In our patients, there were no false positive results due to changes in immune-related inflammation.In our case, there were 4 patients with reduction in the size of tumor on preoperative 18F-FDG PET/CT, but metabolism increased instead. Final pathology confirmed that none of the four patients achieved MPR. This result confirms 18F-FDG PET/CT can predict MPR to neoadjuvant immunochemotherapy in resectable non-small cell lung cancer.
Several limitations must be considered in this study. First of all, the retrospective nature of this study may have introduced potential selection and verification biases. Secondly, Most of patients in our study were squamous-cell carcinoma, and only a small proportion were adenocarcinom, which may have biased the results of this study.Thirdly, The observation duration was relatively short after surgery, we did not evaluate clinical endpoints such as disease-free and overall surviva.Hence, large-scale and multicenter study need to be conducted in the future.
Conclusion
In our study, SULmax and T/N ratio of post-treatment were found to be effective in predicting MPR in NSCLC patients who receiving neoadjuvant immunochemotherapy. Meanwhile, metabolic parameters after treatment were closely related to patients’ PFS, especially ΔTLG%. The metabolic parameters of 18F-FDG PET/CT may be a promising method to assess treatment response from neoadjuvant immunochemotherapy before surgical resection.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- 18F:
-
Fluorine-18
- FDG:
-
Fluorodeoxyglucose
- PET:
-
Positron emission tomography
- CT:
-
Computed tomography
- NSCLC:
-
Non-small cell lung cancer
- SULmax:
-
Maximum standardized uptake value of lean body mass
- SULpeak:
-
Peak standardized uptake value of lean body mass
- MTV:
-
Metabolic tumor volume
- TLG:
-
Total lesion glycolysis
- T/N ratio:
-
Tumor-to- normal liver tissue
- ΔSULmax%:
-
(baseline SULmax-post SULmax)/baseline SULmax × 100%
- ΔSULpeak%:
-
(baseline SULpeak-post SULpeak)/baseline SULpeak × 100%
- ΔMTV%:
-
(baseline MTV-post MTV)/baseline MTV × 100%
- ΔTLG%:
-
(baseline TLG-post TLG)/baseline TLG × 100%
- ΔT/N ratio%:
-
(baseline T/N-post T/N)/baseline T/N × 100%
- MPR:
-
Major pathological response
- PCR:
-
Pathological complete response
- VOI:
-
Volume of Interest
- MIP:
-
Maximum intensity projection
- CMR:
-
Complete metabolic response
- PMR:
-
Partial metabolic response
- PMD:
-
Progressive metabolic disease
- SMD:
-
Stable metabolic disease
- CR:
-
Complete response
- PR:
-
Partial response
- PD:
-
Progression disease
- SD:
-
Stable disease
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
References
Kaira K, Higuchi T, Naruse I, Arisaka Y, Tokue A, Altan B, Suda S, Mogi A, Shimizu K, Sunaga N, et al. Metabolic activity by (18)F-FDG-PET/CT is predictive of early response after nivolumab in previously treated NSCLC. Eur J Nucl Med Mol Imaging. 2018;45(1):56–66.
Nasim F, Sabath BF, Eapen GA. Lung Cancer. Med Clin North Am. 2019;103(3):463–73.
Franzi S, Mattioni G, Rijavec E, Croci GA, Tosi D. Neoadjuvant Chemo-Immunotherapy for locally Advanced Non-small-cell Lung Cancer: a review of the literature. J Clin Med 2022, 11(9).
Wei SC, Duffy CR, Allison JP. Fundamental mechanisms of Immune Checkpoint Blockade Therapy. Cancer Discov. 2018;8(9):1069–86.
Bracci L, Schiavoni G, Sistigu A, Belardelli F. Immune-based mechanisms of cytotoxic chemotherapy: implications for the design of novel and rationale-based combined treatments against cancer. Cell Death Differ. 2014;21(1):15–25.
Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, Domine M, Clingan P, Hochmair MJ, Powell SF, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-small-cell Lung Cancer. N Engl J Med. 2018;378(22):2078–92.
Forde PM, Spicer J, Lu S, Provencio M, Mitsudomi T, Awad MM, Felip E, Broderick SR, Brahmer JR, Swanson SJ, et al. Neoadjuvant Nivolumab plus Chemotherapy in Resectable Lung Cancer. N Engl J Med. 2022;386(21):1973–85.
Paz-Ares L, Luft A, Vicente D, Tafreshi A, Gumus M, Mazieres J, Hermes B, Cay Senler F, Csoszi T, Fulop A, et al. Pembrolizumab plus Chemotherapy for squamous non-small-cell Lung Cancer. N Engl J Med. 2018;379(21):2040–51.
Zhu K, Su D, Wang J, Cheng Z, Chin Y, Chen L, Chan C, Zhang R, Gao T, Ben X, et al. Predictive value of baseline metabolic tumor volume for non-small-cell lung cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Front Oncol. 2022;12:951557.
Zhang L, Huang EH, Wu J, Li J, Hou Q, Li L, Dai C, Deng C, Yang J. Clinical utility of [(18)F]FDG PET/CT in the assessment of mediastinal lymph node disease after neoadjuvant chemoimmunotherapy for non-small cell lung cancer. Eur Radiol. 2023;33(12):8564–72.
Yang M, Li X, Cai C, Liu C, Ma M, Qu W, Zhong S, Zheng E, Zhu H, Jin F, et al. [(18)F]FDG PET-CT radiomics signature to predict pathological complete response to neoadjuvant chemoimmunotherapy in non-small cell lung cancer: a multicenter study. Eur Radiol. 2024;34(7):4352–63.
Wang SY, Shiau YC, Hsu CX. Comments on dynamic (18) F-FDG PET/CT can predict the major pathological response to neoadjuvant immunotherapy in non-small cell lung cancer. Thorac Cancer. 2022;13(24):3513–4.
Zhang C, Liu J, Tong J, Sun X, Song S, Huang G. 18F-FDG-PET evaluation of pathological tumour response to neoadjuvant therapy in patients with NSCLC. Nucl Med Commun. 2013;34(1):71–7.
Tao X, Li N, Wu N, He J, Ying J, Gao S, Wang S, Wang J, Wang Z, Ling Y, et al. The efficiency of (18)F-FDG PET-CT for predicting the major pathologic response to the neoadjuvant PD-1 blockade in resectable non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2020;47(5):1209–19.
Provencio M, Nadal E, Insa A, Garcia-Campelo MR, Casal-Rubio J, Domine M, Majem M, Rodriguez-Abreu D, Martinez-Marti A, De Castro Carpeno J, et al. Neoadjuvant chemotherapy and nivolumab in resectable non-small-cell lung cancer (NADIM): an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol. 2020;21(11):1413–22.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(Suppl 1):S122–50.
Katz SI, Hammer M, Bagley SJ, Aggarwal C, Bauml JM, Thompson JC, Nachiappan AC, Simone CB 2nd, Langer CJ. Radiologic pseudoprogression during Anti-PD-1 therapy for Advanced Non-small Cell Lung Cancer. J Thorac Oncol. 2018;13(7):978–86.
Kim EY, Kim YS, Park I, Ahn HK, Lee HY, Kim JH. Radiologic presentation of non-small cell lung cancer treated with anti-PD-1 therapy. J Thorac Dis. 2018;10(Suppl 33):S3930–2.
Zhao ZR, Yang CP, Chen S, Yu H, Lin YB, Lin YB, Qi H, Jin JT, Lian SS, Wang YZ, et al. Phase 2 trial of neoadjuvant toripalimab with chemotherapy for resectable stage III non-small-cell lung cancer. Oncoimmunology. 2021;10(1):1996000.
Amaria RN, Menzies AM, Burton EM, Scolyer RA, Tetzlaff MT, Antdbacka R, Ariyan C, Bassett R, Carter B, Daud A, et al. Neoadjuvant systemic therapy in melanoma: recommendations of the International Neoadjuvant Melanoma Consortium. Lancet Oncol. 2019;20(7):e378–89.
Weber WA, Figlin R. Monitoring cancer treatment with PET/CT: does it make a difference? J Nucl Med. 2007;48:s36–44.
Kaira K, Ichiki Y, Imai H, Kawasaki T, Hashimoto K, Kuji I, Kagamu H. Potential predictors of the pathologic response after neoadjuvant chemoimmunotherapy in resectable non-small cell lung cancer: a narrative review. Transl Lung Cancer Res. 2024;13(5):1137–49.
Liu J, Dong M, Sun X, Li W, Xing L, Yu J. Prognostic value of 18F-FDG PET/CT in Surgical Non-small Cell Lung Cancer: a Meta-analysis. PLoS ONE. 2016;11(1):e0146195.
Bepler G, Sommers KE, Cantor A, Li X, Sharma A, Williams C, Chiappori A, Haura E, Antonia S, Tanvetyanon T, et al. Clinical efficacy and predictive molecular markers of neoadjuvant gemcitabine and pemetrexed in resectable non-small cell lung cancer. J Thorac Oncol. 2008;3(10):1112–8.
Hicks RJ. Role of 18F-FDG PET in assessment of response in non-small cell lung cancer. J Nucl Med. 2009;50(Suppl 1):S31–42.
Burger IA, Casanova R, Steiger S, Husmann L, Stolzmann P, Huellner MW, Curioni A, Hillinger S, Schmidtlein CR, Soltermann A. 18F-FDG PET/CT of Non-small Cell Lung Carcinoma under Neoadjuvant Chemotherapy: background-based adaptive-volume Metrics Outperform TLG and MTV in Predicting histopathologic response. J Nucl Med. 2016;57(6):849–54.
Takada K, Toyokawa G, Yoneshima Y, Tanaka K, Okamoto I, Shimokawa M, Wakasu S, Haro A, Osoegawa A, Tagawa T, et al. (18)F-FDG uptake in PET/CT is a potential predictive biomarker of response to anti-PD-1 antibody therapy in non-small cell lung cancer. Sci Rep. 2019;9(1):13362.
Chen ZY, Fu R, Tan XY, Yan LX, Tang WF, Qiu ZB, Qi YF, Li YF, Hou QY, Wu YL, et al. Dynamic (18) F-FDG PET/CT can predict the major pathological response to neoadjuvant immunotherapy in non-small cell lung cancer. Thorac Cancer. 2022;13(17):2524–31.
Cascone T, William WN Jr., Weissferdt A, Leung CH, Lin HY, Pataer A, Godoy MCB, Carter BW, Federico L, Reuben A, et al. Neoadjuvant nivolumab or nivolumab plus ipilimumab in operable non-small cell lung cancer: the phase 2 randomized NEOSTAR trial. Nat Med. 2021;27(3):504–14.
Na F, Wang J, Li C, Deng L, Xue J, Lu Y. Primary tumor standardized uptake value measured on F18-Fluorodeoxyglucose positron emission tomography is of prediction value for survival and local control in non-small-cell lung cancer receiving radiotherapy: meta-analysis. J Thorac Oncol. 2014;9(6):834–42.
Yossi S, Krhili S, Muratet JP, Septans AL, Campion L, Denis F. Early assessment of metabolic response by 18F-FDG PET during concomitant radiochemotherapy of non-small cell lung carcinoma is associated with survival: a retrospective single-center study. Clin Nucl Med. 2015;40(4):e215–221.
Sun T, Huang S, Jiang Y, Yuan H, Wu J, Liu C, Zhang X, Tang Y, Ben X, Tang J, et al. Dynamic alteration in SULmax predicts early pathological tumor response and short-term prognosis in non-small cell lung cancer treated with neoadjuvant immunochemotherapy. Front Bioeng Biotechnol. 2022;10:1010672.
Lodge MA, Chaudhry MA, Wahl RL. Noise considerations for PET quantification using maximum and peak standardized uptake value. J Nucl Med. 2012;53(7):1041–7.
Lopci E, Toschi L, Grizzi F, Rahal D, Olivari L, Castino GF, Marchetti S, Cortese N, Qehajaj D, Pistillo D, et al. Correlation of metabolic information on FDG-PET with tissue expression of immune markers in patients with non-small cell lung cancer (NSCLC) who are candidates for upfront surgery. Eur J Nucl Med Mol Imaging. 2016;43(11):1954–61.
Liao S, Penney BC, Wroblewski K, Zhang H, Simon CA, Kampalath R, Shih MC, Shimada N, Chen S, Salgia R, et al. Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39(1):27–38.
Liao S, Penney BC, Zhang H, Suzuki K, Pu Y. Prognostic value of the quantitative metabolic volumetric measurement on 18F-FDG PET/CT in Stage IV nonsurgical small-cell lung cancer. Acad Radiol. 2012;19(1):69–77.
Chin AL, Kumar KA, Guo HH, Maxim PG, Wakelee H, Neal JW, Diehn M, Loo BW Jr., Gensheimer MF. Prognostic value of pretreatment FDG-PET parameters in high-dose image-guided Radiotherapy for Oligometastatic Non-small-cell Lung Cancer. Clin Lung Cancer. 2018;19(5):e581–8.
Winther-Larsen A, Fledelius J, Sorensen BS, Meldgaard P. Metabolic tumor burden as marker of outcome in advanced EGFR wild-type NSCLC patients treated with erlotinib. Lung Cancer. 2016;94:81–7.
Bott MJ, Yang SC, Park BJ, Adusumilli PS, Rusch VW, Isbell JM, Downey RJ, Brahmer JR, Battafarano R, Bush E, et al. Initial results of pulmonary resection after neoadjuvant nivolumab in patients with resectable non-small cell lung cancer. J Thorac Cardiovasc Surg. 2019;158(1):269–76.
Gao S, Li N, Gao S, Xue Q, Ying J, Wang S, Tao X, Zhao J, Mao Y, Wang B, et al. Neoadjuvant PD-1 inhibitor (Sintilimab) in NSCLC. J Thorac Oncol. 2020;15(5):816–26.
Funding
This work was financially supported by the National Natural Science Foundation (No.81871387, 82171980) and Beijing Natural Science Foundation (No.7202027).
Author information
Authors and Affiliations
Contributions
R.G, P.Y, Z.Y and N.L were involved in the conception and design of the study. R.G, F.W, X.M and H.S were involved in the collection and analysis of data. R.G, P.Y and N.L wrote and revised the manuscript. All authors reviewed and approved the final manuscript. Z.Y and N.L were the principal investigator. All authors provided critical feedback and helped shape the research, analysis, and manuscript, and discussed the results. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical approval
As the present analysis has merely a retrospective character, neither Institutional Review Board approval nor informed consent was required by national law.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, R., Yan, W., Wang, F. et al. The utility of 18F-FDG PET/CT for predicting the pathological response and prognosis to neoadjuvant immunochemotherapy in resectable non-small-cell lung cancer. Cancer Imaging 24, 120 (2024). https://doi.org/10.1186/s40644-024-00772-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40644-024-00772-x