Abstract
Introduction
Spinal cysts have traditionally been treated with surgery since it was first described in 1950. However, there have been rare instances where these cysts have resolved on their own without the need for surgical intervention. Here, we discuss the 27th reported case of such spontaneous resolution in the medical literature and delve into the details of this unique case.
Case presentation
This report details a rare case of a 58-year-old Middle Eastern female who suffered from severe radicular and lumbar pain. Radiological study showed the presence of a cyst in the lumbar column. Noninvasive treatment was chosen after ensuring that there were no other symptoms requiring surgery. The patient showed gradual improvement over the course of 12 months, after which the pain completely disappeared.
Discussion
The surgical approach is currently the main treatment for spinal cysts, but spontaneous resolution, despite its rarity, may be worth considering as a preferred therapeutic approach in the future. This avenue has not been thoroughly explored or studied. Due to the etiology of these cysts and their location within mobile joints, a longer period of conservative management including rest and physical therapy may play a pivotal role in promoting natural resolution.
Conclusion
Conservative treatment of cysts should continue for at least 8 months, using painkillers and physical therapy without lumbar bracing. Surgery remains the most effective means of treatment to date. Further research is needed to validate and establish standardized treatment protocols.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
In 1877, Becker was the first to describe synovial cysts, initially identifying them as cysts located in the joints of the lower limb [1]. Later, it was found that they can occur in most of the body’s moving joints. Then, in 1950, Vossschulte and Borger [2] documented the first case of a synovial cyst in the lumbar spine.
Synovial cysts, or ganglion cysts, are fluid-filled sacs that develop in the facet joints of the spinal column as a result of external factors putting pressure on the movable joints in the spine, causing degenerative changes that can lead to the enlargement of the facet joints and the formation of these cysts [3].
Spinal cysts are mostly found in the lumbar and cervical regions, with limited evidence of their occurrence in the thoracic spine. The main treatment approach, as indicated by the majority of medical literature, involves surgical intervention by excising and decompressing [4]. In some cases, spinal fusion might be necessary to stabilize the spine following the removal of the cyst [5]. A recent study by Benito et al. [6] on 657 patients with synovial cysts, comparing the outcomes of different surgical methods, revealed that lumbar decompression and fusion (LDF) were associated with better outcomes, including reduced postoperative back pain and lower rates of cyst recurrence compared with lumbar posterior decompression (LPD).
Alternatively, treatment may include aspiration and steroid injections. Facet joint injections have demonstrated efficacy in offering short-term pain relief for spinal synovial cysts. Nonetheless, their effectiveness tends to diminish over time [7]. Additionally, the aspiration of cysts guided by computed tomography (CT) or fluoroscopy, along with subsequent steroid injection, has produced varying outcomes [8, 9]. Certain studies have indicated increased recurrence or failure rates when employing this method compared with surgical alternatives [9, 10].
In some rare cases, cysts may resolve spontaneously with the use of pain management, physical therapy, and lumbar bracing [11].
This report will elaborate on a unique case of a patient who achieved full recovery from a painful lumbar synovial cyst without the need for any interventional procedures, using only painkillers and physical therapy.
Case presentation
A 58-year-old Middle Eastern female from Syria presented to the neurosurgery department in the sixth month of 2021 with progressive left radicular pain extending to the hip and the lateral posterior side of the thigh and leg, reaching the lateral toes, and back pain in the lumbar region, scoring 10/10 on the numeric pain scale, that had been ongoing for 1 month. The patient had difficulty walking and denied any traumatic events. A review of the patient’s medical history revealed that she had chronic right radicular lumbar pain in 2018 with a normal lumbar magnetic resonance imaging (MRI), which was successfully treated with painkillers for 3 months. In 2020, the same pain recurred, and the MRI was again normal, and she recovered using painkillers once more.
Investigations
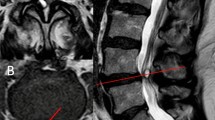
Physical examination revealed normal strength and tendon reflexes in the lower limbs, normal muscle tone in both lower limbs, and a highly positive Lasègue test. Lumbar MRI showed an extradural cystic lesion in the L5–S1 spinal canal, adjacent to the left internal facet joint, with hypointensity in T1-weighted images and slightly hyperintensity in T2-weighted images, consistent with a synovial cyst (Fig. 1).
Differential diagnosis
The primary differential diagnosis considered for the observed lesion was a spinal synovial cyst. The MRI findings showed a significant increase in synovial fluid within the articular facet, with a clear connection between the cyst and the articular facet.
In some cases, an extruded disc fragment may be considered when there is a disc herniation. Nonetheless, protruding disc fragments usually show signal intensity features that mirror those of the original disc and are commonly situated in front, rather than posterior and lateral to the thecal sac.
Meningioma is another differential diagnosis that may present with similar intensity to synovial cysts on MRI. However, meningiomas are typically intradural extramedullary and develop over a longer period. The earlier MRI results excluded this potential diagnosis.
Treatment
The patient did not exhibit any clinical or radiological signs indicating the need for surgery. Therefore, a noninvasive approach was chosen, focusing on pain management with diclofenac potassium 50 mg twice daily and a proton pump inhibitor (PPI) once daily in the morning. Physical therapy was recommended, while orthopedic bracing was not deemed necessary. Clinical re-evaluation was scheduled every 3 months.
Follow-up and outcome
The patient reported gradual but significant improvement in pain over the next 3 months, but the pain remained severe, scoring 7/10 on the pain scale. After 6 months she stopped physical therapy sessions, with 5/10 on the pain scale, and we reduced the dose of pain relievers to once a day or when needed. A total of 9 months after the onset of symptoms, the patient reported a nearly complete absence of pain. A follow-up MRI performed 12 months later showed overgrowth of facets without canal stenosis at L5–S1. The previously observed cyst was nearly no longer present. Since then, the patient has been free of pain or any neurological symptoms (Fig. 2).
Discussion
Spinal cord cysts are often a result of degenerative changes in the spine or repeated minor trauma to the joint surfaces. These issues can cause a build-up of joint fluid and subsequent leakage, leading to the development of synovial cysts, which sometimes may present with severe symptoms indicating appropriate treatment. These cysts are frequently located near the joint surfaces and are particularly prevalent in the most mobile regions of the lumbar spine, such as at the L4–L5 level [3,4,5,6,7,8,9,10,11,12]. In the patient’s medical history, she experienced intermittent lumbar pain attributed to external factors, which aligns with the degenerative etiology of these cysts.
Synovial cysts are consistently located posterolateral to the thecal sac and can cause central or lateral spinal stenosis. Symptoms may include radiculopathy, back pain, sensory deficit, motor deficit, neurogenic claudication, and cauda equine syndrome. These cysts can appear at any level in the spinal column, including the C1–C2 level, but 92% of cases occur in the lumbar spine. The cervical and thoracic spines are less frequently affected, with rates of 6.3% and 1.6%, respectively [12].
The available treatment options for these spinal cysts include interventional treatments, such as surgical procedures with or without spinal instrumental fusion, or aspiration of the cyst along with steroid injections. Noninterventional treatments, such as pain management, physical therapy, and lumbar bracing, may also be considered. Surgical intervention with cyst removal to relieve pressure on the spine is considered the most common procedure for treating these symptomatic cysts in medical literature, as it has shown lower recurrence rates than any other approaches [10, 12]. The type of surgical procedure, whether it involves cyst removal or decompression with or without fusion, remains the best and in most cases the primary treatment for any symptomatic lumbar synovial cyst [13, 14].
The spontaneous resolution of these cysts is very rare in the medical literature, with only 26 cases recorded. Adding our case brings the total number recorded to 27 to date. Chiarella et al. [11] collected data on the spontaneous resolution of spinal cysts, which they referred to as “ganglion cysts.” They suggested noninvasive treatment for at least 6 months including anti-inflammatory drugs and light unloading exercises to control pain and reduce intra-cystic fluid, rest, and lumbar bracing. But they did not mention any specific indication for conservative treatment, and most of the reviewed cases did not mention severe symptoms.
Considering the pathological mechanism of these cysts, as well as the absence of alternative causes for the patient’s pain in the clinical and radiological examinations, a conservative treatment plan was implemented. This involved the administration of painkillers and physical therapy over a period of 3 months. Following this initial treatment, the patient reported a reduction in pain from 10 out of 10 to 7 out of 10 on the pain scale, prompting an extension of the conservative treatment. After 10 months from the onset of symptoms, the patient reported intermittent pain at an intensity of 1 out of 10 on the pain scale. Subsequent MRI scans after 12 months demonstrated a 90% reduction in the size of the cyst, with decreased signal intensity at both T1 and T2. This case illustrates that physical therapy and long rest, which alleviated external pressures on joint surfaces and relieved spinal pressure, facilitated the gradual reabsorption and reduction in cyst size over time.
Lumber bracing is a controversial issue. While lumbar spine stabilizers may offer short-term benefits, they may also lead to muscle weakness in this area, potentially resulting in increased pain and subsequent complications.
Noninvasive treatment methods may hold significant promise for the future, with the potential to reduce the need for surgical intervention, thereby decreasing financial burdens and mitigating potential post-operative complications. However, this case, along with the other 26 cases of spontaneous resolution in the medical literature, does not provide sufficient evidence to consider it as the optimal method for managing spinal synovial cysts. Hopefully, the number of these cases will increase in the future so that a large study on this treatment method can be done.
Conclusion
Cysts are a rare cause of radicular pain, but they can manifest as severe pain, which may perplex the medical practitioner regarding treatment and diagnosis. Surgical treatment is approach the most often availed for treating these cysts. A longer period of conservative treatment can be given a chance, even with severe pain. We propose a conservative approach involving noninvasive therapies for a minimum of 8 months focusing on pain management and physical therapy. Further extensive studies are needed to validate the effectiveness of this method so it could be considered for treatment.
Availability of data and materials
Not applicable.
Abbreviations
- LDF:
-
Lumbar decompression and fusion
- LPD:
-
Lumbar posterior decompression
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Baker WM. On the formation of synovial cysts in the leg in connection with disease of the knee-joint. Clin Orthop Relat Res. 1994;299:2–10.
Vossschulte K, Borger G. Anatomische und funktionelle Untersuchungen über den Bandscheibenprolaps [Anatomic and functional studies of intervertebral disk hernia]. Langenbecks Arch Klin Chir Ver Dtsch Z Chir. 1950;265(3–4):329–55.
Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976). 1995;20(1):80–9. https://doi.org/10.1097/00007632-199501000-00015.
Weiner BK, Torretti J, Stauff M. Microdecompression for lumbar synovial cysts: an independent assessment of long term outcomes. J Orthop Surg Res. 2007;2:5. https://doi.org/10.1186/1749-799X-2-5.
Campbell RJ, Mobbs RJ, Rao PJ, Phan K. Interventions for lumbar synovial facet joint cysts: a comparison of percutaneous, surgical decompression and fusion approaches. World Neurosurg. 2017;98:492–502. https://doi.org/10.1016/j.wneu.2016.11.044.
Benato A, Menna G, Rapisarda A, Polli FM, D’Ercole M, Izzo A, D’Alessandris QG, Montano N. Decompression with or without fusion for lumbar synovial cysts-a systematic review and meta-analysis. J Clin Med. 2023;12(7):2664. https://doi.org/10.3390/jcm12072664.
Christophis P, Asamoto S, Kuchelmeister K, et al. “Juxtafacet cysts”, a misleading name for cystic formations of mobile spine (CYFMOS). Eur Spine J. 2007;16:1499–505. https://doi.org/10.1007/s00586-006-0287-5.
Lutz GE, Shen TC. Fluoroscopically guided aspiration of a symptomatic lumbar zygapophyseal joint cyst: a case report. Arch Phys Med Rehabil. 2002;83(12):1789–91. https://doi.org/10.1053/apmr.2002.34601.
Allen TL, Tatli Y, Lutz GE. Fluoroscopic percutaneous lumbar zygapophyseal joint cyst rupture: a clinical outcome study. Spine J. 2009;9(5):387–95. https://doi.org/10.1016/j.spinee.2008.08.008.
Epstein NE, Agulnick MA. Perspective: operate on lumbar synovial cysts and avoid ineffective percutaneous techniques. Surg Neurol Int. 2024;1(15):65. https://doi.org/10.25259/SNI_95_2024.
Chiarella V, Ramieri A, Giugliano M, Domenicucci M. Rapid spontaneous resolution of lumbar ganglion cysts: a case report. World J Orthop. 2020;11(1):68–75. https://doi.org/10.5312/wjo.v11.i1.68.
Bruder M, Cattani A, Gessler F, Droste C, Setzer M, Seifert V, Marquardt G. Synovial cysts of the spine: long-term follow-up after surgical treatment of 141 cases in a single-center series and comprehensive literature review of 2900 degenerative spinal cysts. J Neurosurg Spine. 2017;27(3):256–67. https://doi.org/10.3171/2016.12.SPINE16756.
Epstein NE, Baisden J. The diagnosis and management of synovial cysts: efficacy of surgery versus cyst aspiration. Surg Neurol Int. 2012;3(Suppl 3):S157–66. https://doi.org/10.4103/2152-7806.98576.
Lalanne LB, Carmona RL, Cirillo Totera JI, Lemos FA, Wilson JTM, Beaulieu Montoya AM. Surgically managed symptomatic intraspinal lumbar facet synovial cyst outcome of surgical treatment with resection and instrumented posterolateral fusion, a case series. BMC Surg. 2022;22(1):277. https://doi.org/10.1186/s12893-022-01712-x.
Acknowledgements
Not applicable.
Funding
None for all authors.
Author information
Authors and Affiliations
Contributions
Mostafa Hassan contributed to writing, editing, data collection, data interpretation and analysis, drafting, and critical revision. Iyas Salman contributed to data collection and editing of the manuscript. Issam Salman was the supervisor and contributed to critical revision and final approval.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hassan, M., Salman, I. & Salman, I. Spontaneous resolution of synovial lumbar cyst presented with severe symptoms: a case report. J Med Case Reports 18, 432 (2024). https://doi.org/10.1186/s13256-024-04762-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-024-04762-2