Abstract
This study aimed to compare the findings of plain radiography and computed tomography (CT) of foot and ankle in patients submitted to the emergency department with high-energy foot and ankle trauma, to demonstrate if missing fractures on plain radiographs will significantly alter the treatment plan considered for each patient based on the findings of each imaging modality. We retrospectively observed standard radiological foot and ankle x-rays and CT scans in patients who presented to our center from April 2019 to June 2020 with a history of foot and ankle trauma with either loss of consciousness, a history of high-energy trauma, or clinical presentation disproportionate to plain radiographic findings. We investigated the number of fractures of each bone detected on plain radiographs and CT scans and the treatments based on each modality’s findings in patients admitted to our center. Sixty-five out of 163 (39.87%) included in our study had at least one missed fracture on plain radiography that was detected on CT. Thirty-one (19%) patients had normal radiography despite actually having fractures. In 38 (23.31%) patients CT changed the treatment plan decided by our surgeons (P < 0.001). The two imaging modalities had a moderate agreement for detecting foot and ankle fractures overall (κ = 0.432). The failure to detect fractures in patients with high-energy trauma can significantly impact treatment effectiveness. Integrating CT scans into the diagnostic process can lead to changes in treatment planning and ultimately improve patient outcomes.
Level of clinical evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Foot and ankle trauma, encompassing a wide range of injuries, can significantly impact a person’s mobility and overall quality of life. Fractures of the foot are the most frequently missed fractures in adult patients presenting to the emergency department [1, 2]. To evaluate patients with foot and ankle trauma, initial imaging typically involves three-view plain radiography, including anteroposterior (AP), mortise, and lateral views [3, 4]. However, certain fractures, such as osteochondral talar dome fractures, small avulsion fractures of the mid- or hindfoot, and those involving the posterior malleolus, are often missed on plain radiographs [5,6,7]. Specific management plannings such as open reduction for trimalleolar fractures, which are commonly missed by plain radiography, are needed for perfect reduction of different fracture types [8]. Failure to do so can lead to complications such as avascular necrosis of the talus bone, development of post-traumatic osteoarthritis, and ankle instability; thus significantly affecting the patient’s quality of life and the average cost per patient [9,10,11,12]. Complementary imaging techniques, such as computed tomography (CT) and magnetic resonance imaging (MRI), are commonly used to plan surgical interventions and identify occult fractures and soft tissue injuries not visible on plain radiographs. However, routine utilization of CT and MRI in foot and ankle trauma cases remains uncommon [13].
While CT imaging offers advantages in diagnostic precision, the question arises as to whether it leads to discrepancies in treatment planning compared to plain radiographic findings.
This study aims to evaluate and compare the differences in treatment planning based on CT and plain radiographic findings in patients with either high energy foot and ankle trauma, patients unable to localize or describe their pain or those with pain in their foot and ankle after trauma disproportionate to the X-ray findings. By conducting a comprehensive analysis, we aim to gain insights into the potential variations in treatment planning resulting from differing imaging modalities.
Methodology
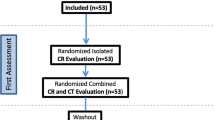
Study Design
This study evaluated treatment planning discrepancies between CT and plain radiographic findings in patients with foot and ankle trauma. A retrospective study design was employed as part of a medical student thesis to analyze data collected from patients admitted to Imam Khomeini Hospital between April 2019 and June 2020. This study was performed thesis of one the authors. Patient data were collected retrospectively from the hospital’s picture archiving and communication system (PACS) without direct patient contact. Ethical approval for the study was obtained from the research ethics committees of the Imam Khomeini Hospital complex.
Inclusion criteria
All patients with a documented history of foot and ankle trauma admitted to the hospital during the specified timeframe were included in the study. The trauma had to occur within the past 24 h and fall into one of the following categories: high-energy trauma, falling from a height, trauma accompanied by loss of consciousness, or trauma with pain or swelling disproportionate to plain radiographic findings. The age range for inclusion was set between 15 and 85 years old. Furthermore, a full medical history, including a comprehensive list of reported abnormalities on radiographs, as well as the treatment plan submitted in the PACS, were recorded.
Exclusion criteria
Patients who did not undergo either plain radiographs or CT scans of the foot or ankle, or did not have consent to take part in this study were excluded. In addition, patients with a history of surgical intervention of foot and ankle, poor general medical conditions, and nonambulatory states were not considered eligible for this study.
Imaging evaluation
Both plain radiographs and CT scans were evaluated for abnormalities, specifically focusing on fractures of the medial, lateral, and posterior malleolus, calcaneus, talus, cuboid, cuneiform, metatarsal, and distal tibial fractures. Two experienced orthopedic surgeons with a minimum of 6 years of practical experience simultaneously reviewed the imaging records. A senior radiologist also reviewed the imaging records. The final decision about the number of fractures was made according to the comments of all three reviewers. The orthopedic surgeons mutually determined the managing plan concluded from each imaging modality based on the findings of plain radiography and CT scans. The patients included in the evaluation were selected randomly. CT scans were considered the gold standard in this study for comparison with plain radiographic findings.
Statistical analysis
The recorded data, including the number and type of pathologies detected by CT and plain radiography, as well as the treatment planning based on the findings of each modality, were analyzed using the statistical package for the social sciences (SPSS) V. 26.0 program.
Quantitative variables were reported as frequency (%). The McNemar’s test was used to assess the relationship between two dichotomous variables of if plain radiography has missed a fracture (yes or no) and the treatment plan has changed (yes or no). A significance level of P < 0.05 was set for all statistical tests.
Cohen’s kappa value was calculated to determine the degree of agreement between CT and plain radiography in detecting foot and ankle fractures. The interpretation of the kappa value was categorized as follows: no agreement for values ≤ 0, none to slight agreement from 0.01 to 0.2, fair agreement from 0.21 to 0.4, moderate agreement from 0.41 to 0.6, substantial agreement from 0.61 to 0.8, and almost perfect agreement from 0.81 to 1.0 [14].
Results
A total of 163 patients with a history of foot and ankle trauma were included in the study, with a mean age of 40 (range 15–85) years. Among the patients, 41 (25.2%) were females and 122 (74.8%) were males. Conventional radiography failed to detect at least one fracture in 65 patients (39.87%), which was subsequently identified on CT scan. Of these 65 patients, 55 (33.74%) had one undetected fracture on plain radiographs, 8 (4.9%) had two undetected fractures, and 2 (1.22%) had three undetected fractures (Table 1.) Additionally, CT scans revealed at least one fracture in 31 patients (19%) with normal findings on conventional radiographs (Fig. 1).
A 29 year-old male presenting with a history of motor vehicle accident with complaint of foot and ankle swelling and pain. The plain radiography seems normal (1–3), but with a closer look at the patient’s CT, fractures of the cuboid (4), 4th metatarsal (5), and comminuted fracture of talus (6,7) can be detected (red arrows). This patient has to be managed operatively based on CT findings
Based on the initial conventional radiographic findings, 84 patients (51.53%) were initially planned for surgical management. However, this number increased to 93 patients (57%) after performing CT scans. In total, 38 patients (23.31%) had a change in their treatment plan following the CT scan.
The agreement between CT and plain radiography in detecting foot and ankle fractures varied across different fracture sites. The agreement was slight for cuneiform (κ = 0.000), fair for talus (κ = 0.333), cuboid (κ = 0.242), and navicular (κ = 0.351), and moderate for posterior malleolar (κ = 0.589), trimalleolar (κ = 0.548), and distal tibial (κ = 0.531) fractures. The overall agreement between CT and plain radiography in detecting foot and ankle fractures, as measured by the kappa value, was interpreted as moderate (κ = 0.432) (Table 2).
Discussion
Evaluating treatment planning discrepancies between CT and plain radiographic findings in patients with foot and ankle trauma is crucial for accurate diagnosis and appropriate management. According to our study’s findings, CT may significantly impact treatment planning in emergency department patients who present with foot and ankle trauma.
Our results demonstrated several important findings. A significant number of fractures were missed by conventional radiography in patients with foot and ankle injuries, with 39.87% of patients having at least one fracture that CT scans could only detect. This result highlights the limitations of plain radiographs in accurately diagnosing fractures in this patient population.
While plain radiography showed high sensitivity (90%) in diagnosing fractures of the distal fibula, medial malleolus, and lateral malleolus, it exhibited lower sensitivity for midfoot bones (12.5%), talus fractures (21.43%), distal tibia fractures (45.83%), posterior malleolar (50%) fractures, and missed all of the cuneiform fractures. Moreover, we identified that even in cases where conventional radiographs appeared normal, CT scans could detect fractures in 19% of patients. These findings support the existing literature highlighting the limited sensitivity of plain radiography in detecting complex foot and ankle fractures, emphasizing the need for additional imaging modalities such as CT for accurate diagnosis [15,16,17,18]. CT can also significantly accelerate fracture detection in trauma settings (P < 0.001) [19]. Therefore, CT may be appropriate to be used routinely in multiple trauma patients suspected of having foot or ankle injuries.
Importantly, our study revealed that including CT scans significantly altered 38 out of 163 cases (23.31%). The alteration may involve the change from nonoperative to operative treatment or a different surgical procedure. In a study conducted by Black et al. on the role of CT in the surgical planning of 600 patients with ankle fractures, it was demonstrated that in 146 cases (24.3%), the surgical management was altered after performing CT [20]. Similarly, another study investigated the use of CT versus plain radiography in surgical planning for ankle fractures; revealing that 24% of patients experienced a modification in their operative management following the addition of CT imaging [6].
In our study, only 1 out of 7 cuboid fractures was detected by plain radiography (κ = 0.242). It has been confirmed in previous studies that plain radiography is often insufficient in diagnosing cuboid fractures due to overlying adjacent midfoot bones. However, these fractures frequently happen along with other foot and ankle fractures in trauma settings and surgical treatment is seldom required due to their extra-articular nature [21, 22].
Posterior malleolus (κ = 0.589), trimalleolar (κ = 0.548), and distal tibial (κ = 0.572) fractures were amongst the most frequently overlooked fractures by plain radiography in ankle regions. In Szymanski’s study, nearly 40% of malleolar pathologies were missed solely based on plain radiography [23]. A similar result has been reported in Donohoe’s study where the management plan and approaches for posterior malleolar fractures were significantly altered after undergoing CT scans. Operative treatment was considered in 84% of cases based on plain radiography, while this number increased to 92% after addition of CT scans [24, 25]. It is suggested in some studies that the decision to operate on the posterior malleolus fractures depends on the fragment size, and plain radiography cannot estimate the size accurately. Larger fragments, with different suggested cut-off sizes, are generally recommended for the operative management [26, 27]. On the contrary, other studies emphasize the importance of additional factors such as articular congruence and ankle stability as indications for surgical intervention. This suggests a more comprehensive approach to treatment decision-making. Furthermore, the impact of factors such as fellowship training and years of surgical practice on the surgical approach was also highlighted [26]. However, based on our data, we could not identify the specific factors influencing surgeons’ decision-making in managing posterior malleolar and trimalleolar fractures.
Our study found an almost perfect agreement between CT and plain radiography for lateral malleolar (κ = 0.937) and medial malleolar (κ = 0.937) fractures. This is in contrast with Jubel’s study in which they reported a sensitivity of 0% for detection of multifragmentary fractures of lateral malleolus. They suggested a routine use of CT for detection of complex ankle fractures, such as multifragmentary fractures of lateral malleolus, in elderly population. However, similar to our findings, the sensitivity of plain radiography was considered to be acceptable (96.8%) for detection of medial malleolar fractures [25].
Our findings suggest that plain radiography could only detect 3 out of 14 (21.43%) talar fractures with a fair agreement (κ = 0.333) with CT. Unless they are nondisplaced, operative management is recommended for talus fractures. Inadequate management of talar fractures can lead to complications such as posttraumatic arthrosis, ankle axial misalignment, and avascular necrosis [28]. Surgical fixation is necessary for large, intraarticular, and comminuted fractures. Conservative treatment using cast immobilization for such fractures has been associated with a higher incidence of chronic pain and nonunion [29]. To detect even minimal displacement in talar fractures and effectively plan management, CT is essential. By identifying subtle fractures and enabling appropriate interventions, CT reduces the need for future reconstructive surgeries [17, 30].
Navicular fractures were detected in only 2 out of 9 (22.22%) patients by plain radiography and there was a fair agreement between CT and plain radiography (κ = 351). These fractures often happen in addition to other fractures of foot and ankle. Other studies also suggest that detection of these fractures is difficult by plain radiography due to their shapes and the overlying adjacent midfoot bones [22]. It is important not to miss these fractures since the navicular bone’s blood supply is poor, which makes it more prone to nonunion [31].
The management of fractures of the metatarsals depends largely on their stability and the amount of displacement. In our study, plain radiography successfully identified 17 out of 25 (68%) metatarsal fractures. Non-operative management of fractures of the proximal shaft of the fifth metatarsal bone (known as Jones fracture) is associated with non- or delayed union.
Conversely, nonoperative approaches are preferred for avulsions of the fifth metatarsal base [32]. Therefore, an accurate diagnosis of the fracture type is necessary for planning the appropriate treatment.
In this retrospective study, we aimed to assess the differences in treatment planning based on these two imaging modalities and explore the implications for patient care.
Despite these findings, plain radiography remains widely employed as the primary imaging modality in trauma patients due to its cost-effectiveness, lower radiation exposure, and widespread availability [33, 34]. However, delaying the diagnosis and treatment of fractures can result in unfavorable outcomes. Various studies have shown that the risk of infection following a delayed treatment of a closed ankle fracture increases significantly, in some studies by six times. Additionally, a delay in treatment has been associated with longer periods of postoperative immobilization, extended hospital stays, and increased average costs for patients [12, 35]. It is important to acknowledge some limitations of our study. Firstly, the retrospective design may have introduced selection bias and limited our ability to control for confounding factors.
Additionally, our study did not provide specific data on the differences in morbidity, cost, and length of hospital stay based on the timing of diagnosis, type of imaging modality and the respective radiation exposure, and treatment. Further prospective research with a larger patient size is necessary to thoroughly evaluate these aspects.
Conclusion
In conclusion, our study highlights the significance of evaluating treatment planning discrepancies between CT and plain radiographic findings in patients with foot and ankle trauma. Failure to detect foot and ankle fractures in patients with high-energy trauma can significantly prevent patients from receiving appropriate treatment. Incorporating CT scans into the diagnostic workup can change treatment planning and improve patient outcomes.
.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Amin S, et al. Trends in fracture incidence: a Population-based study over 20 years. J Bone Miner Res. 2014;29(3):581–9.
Mattijssen-Horstink L, et al. Radiologic discrepancies in diagnosis of fractures in a Dutch teaching emergency department: a retrospective analysis. Scand J Trauma Resusc Emerg Med. 2020;28(1):38.
Bancroft LW, et al. ACR appropriateness Criteria Acute Trauma to the Foot. J Am Coll Radiol. 2015;12(6):575–81.
Russo A, et al. Ankle fracture: radiographic approach according to the Lauge-Hansen classification. Musculoskelet Surg. 2013;97(Suppl 2):S155–60.
Goost H, et al. Fractures of the Ankle Joint. Deutsches Aerzteblatt Online; 2014.
Leung KH, et al. Preoperative radiography versus computed tomography for surgical planning for ankle fractures. J Orthop Surg (Hong Kong). 2016;24(2):158–62.
Pinto A, et al. Traumatic fractures in adults: missed diagnosis on plain radiographs in the Emergency Department. Acta Biomed. 2018;89(1–s):111–23.
Goost H, et al. Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int. 2014;111(21):377–88.
Haskell A. Natural history of avascular necrosis in the Talus: when to operate. Foot Ankle Clin. 2019;24(1):35–45.
Yaradilmis YU. The mid-term effects on Quality of Life and Foot functions following Pilon fracture. Turkish Journal of Trauma and Emergency Surgery; 2020.
Pehlivanoglu T et al. Long-term clinical and radiographic outcomes following Surgical Treatment for Ankle Fracture-Dislocations: do poor radiographic outcomes always matter? J Am Podiatr Med Assoc, 2024: p. 1–26.
Pilskog K, et al. Association of delayed surgery for ankle fractures and patient-reported outcomes. Volume 43. Foot & Ankle International; 2022. pp. 762–71. 6.
Barile A, et al. Emergency and trauma of the ankle. Semin Musculoskelet Radiol. 2017;21(3):282–9.
McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–82.
Magid D, et al. Adult ankle fractures: comparison of plain films and interactive two- and three-dimensional CT scans. AJR Am J Roentgenol. 1990;154(5):1017–23.
Haraguchi N, et al. Pathoanatomy of posterior malleolar fractures of the ankle. J Bone Joint Surg Am. 2006;88(5):1085–92.
Buza JA, Leucht P. Fractures of the talus: current concepts and new developments. Foot Ankle Surg. 2018;24(4):282–90.
Angoules AG, et al. Update on diagnosis and management of cuboid fractures. World J Orthop. 2019;10(2):71–80.
Fitschen-Oestern S, et al. Missed foot fractures in multiple trauma patients. BMC Musculoskelet Disord. 2019;20(1):121.
Black EM, et al. Role of preoperative computed tomography scans in operative planning for malleolar ankle fractures. Foot Ankle Int. 2013;34(5):697–704.
Pountos I, Panteli M, Giannoudis PV. Cuboid injuries. Indian J Orthop. 2018;52(3):297–303.
Bradshaw C-DL. Navicular and cuboid fractures. Clin Podiatr Med Surg. 2024;41(3):425–35.
Szymański T, Zdanowicz U. Comparison of routine computed tomography and plain X-ray imaging for malleolar fractures-how much do we miss? Foot Ankle Surg. 2022;28(2):263–8.
Donohoe S, et al. Impact of computed tomography on Operative Planning for Ankle fractures involving the posterior Malleolus. Foot Ankle Int. 2017;38(12):1337–42.
Jubel A, et al. [Conventional X-Rays of Ankle Joint fractures in older patients are not always predictive]. Z Orthop Unfall. 2017;155(1):45–51.
Gardner MJ, et al. Surgeon practices regarding operative treatment of posterior malleolus fractures. Foot Ankle Int. 2011;32(4):385–93.
Odak S, et al. Management of posterior malleolar fractures: a systematic review. J Foot Ankle Surg. 2016;55(1):140–5.
Vallier HA. Fractures of the Talus: state of the art. J Orthop Trauma. 2015;29(9):385–92.
Wijers O, et al. Lateral process fracture of the Talus: a Case Series and Review of the literature. J Foot Ankle Surg. 2020;59(1):136–41.
Lee C, et al. Talus fractures: evaluation and treatment. J Am Acad Orthop Surg. 2020;28(20):e878–87.
Kiel J, Kaiser K. Stress Reaction and Fractures, in StatPearls. 2022, StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC.: Treasure Island (FL).
Rammelt S, Heineck J, Zwipp H. Metatarsal fractures. Injury. 2004;35(Suppl 2):Sb77–86.
Richter M, et al. Chopart joint fracture-dislocation: initial open reduction provides better outcome than closed reduction. Foot Ankle Int. 2004;25(5):340–8.
Ritter J, et al. Radiology: imaging trauma patients in a deployed setting. Mil Med. 2018;183(suppl2):60–4.
Schepers T, et al. The timing of ankle fracture surgery and the effect on infectious complications; a case series and systematic review of the literature. Int Orthop. 2013;37(3):489–94.
Funding
This study did not receive any funds for conducting or publication.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: SHKAnalysis and interpretation of data: NR, SMMProvision of study material or patients: SHK, TACollection, assembly, possession of raw data (doing experiments) : NB, TAStatistical analysis: NR, IMOCritical revision of the article for important intellectual content: NMFinal approval of the study: SHK, NB, SMMGuarantee of integrity of the entire study: SHK.
Corresponding author
Ethics declarations
Consent for publication
The authors all agree for submission and publication of the manuscript.
Ethics approval and consent to participate
The project was approved by the ethics committee of our university(Tehran university of medical sciences). Written informed consent was obtained from all the participants.
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kalantar, S.H., Bagheri, N., Milan, N. et al. Evaluation of treatment planning discrepancies: CT versus plain radiographic findings in patients with foot and ankle trauma. BMC Res Notes 17, 238 (2024). https://doi.org/10.1186/s13104-024-06902-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-024-06902-9