Abstract
Background
The emergence of Plasmodium falciparum drug resistance against artemisinin-based combination therapy has threatened malaria control efforts. Since malaria control and elimination plans are dependent on these drugs, they must remain efficacious. However, resistance to these drugs was detected in low-transmission settings and is predicted to emerge in high-transmission settings, including in unspecified areas of Ethiopia. Therefore, this study aimed to assess the therapeutic efficacy and safety of artemether-lumefantrine for the treatment of uncomplicated P. falciparum malaria.
Methods
A single-arm prospective observational study was conducted at Teda Health Centre, Northwest Ethiopia, by following the 2009 World Health Organization efficacy study guidelines from September 2022 to February 2023. Patients with uncomplicated falciparum malaria were conveniently selected and treated with a standard dose of artemether-lumefantrine, along with a single low dose of primaquine. Then clinical and parasitological responses and haemoglobin levels were assessed during the 28-day scheduled follow-up. Blood films were examined and asexual parasites were quantified; axillary temperature was measured; and drug adverse events were assessed throughout the follow-up. Finally, the drug efficacy (adequate clinical and parasitological response) was determined by Kaplan–Meier and per-protocol analyses. The data were analysed using the WHO Excel spreadsheet and SPSS version 25 software.
Results
The success rates of PCR uncorrected and corrected Kaplan–Meier analysis on day 28 were 95.8% (95% CI 87.5–98.6) and 97.3% (95% CI 89.4–99.3), respectively. The per-protocol PCR uncorrected and corrected adequate clinical and parasitological responses were 95.5% (95% CI 87.5–99.1) and 97% (95% CI 89.5–99.6), respectively. On day-3, 97% of study participants were free of asexual parasitaemia, and all of them were fever-free on day-2. All of the gametocyte-positive patients at baseline were found to be negative for gametocytes on day-2. Moreover, the baseline mean hemoglobin of 13.10 g/dl increased slightly on day-14 to 13.27 g/dl but significantly on day-28 to 13.69 g/dl in a paired sample t test. All adverse events reported were mild.
Conclusion
Artemether-lumefantrine continued to be an efficacious and safe drug for the treatment of uncomplicated Plasmodium falciparum malaria at the Teda Health Centre.
Trial registration: unique ID# PACTR202309773069812 at https://pactr.samrc.ac.za on September 1, 2023.
Similar content being viewed by others
Background
Despite decades of clinical research and treatment improvements, Plasmodium parasites still cause millions of cases and hundreds of thousands of deaths worldwide. The malaria burden is disproportionately high in Africa, with 93.6% and 95.4% of global cases and deaths, respectively in 2022. In the same year, Ethiopia reported a substantial increase in malaria cases compared to previous years, with 2.4 million malaria cases, of which 65% were Plasmodium falciparum mono-infections. Ethiopia is one of the main countries contributing to the increase in global malaria cases by 2022 [1].
The mortality and morbidity rates of malaria declined significantly in certain countries including Ethiopia between 2000 and 2015 [2]. Following this, Ethiopia has planned to eliminate the disease by 2030 [3]. Unfortunately, the downward trend has been reversed, and the estimated global case count has been climbing steadily [4]. As demonstrated by Eshetu et al. [5] and by Ewnetu and Lemma [6], malaria is rising substantially in Gondar Zuria, Northwest Ethiopia, which shows that the elimination campaign faces a serious challenge.
Artemether-lumefantrine (AL) has become the first-line drug for treating uncomplicated falciparum malaria in many endemic countries [7] and has been in use in Ethiopia since 2004 [8]. It is recommended to consume with a fatty meal to enhance its absorption. The drug is well tolerated and safer than other anti-malarials, mainly quinine, which is a second-line drug for the treatment of uncomplicated falciparum malaria in Ethiopia [9].
The P. falciparum kelch13 gene (k13) mutation R622I has been validated to cause delayed parasite clearance and partial resistance to artemisinin. In Ethiopia, it was not found to be linked with delayed clearance, but it is expanding [10, 11]. The expansion of k13 mutant variants in Ethiopia, Rwanda, Uganda and Tanzania highlights the threat of artemisinin partial resistance spreading in sub-Saharan Africa (SSA) [11,12,13,14]. If resistant P. falciparum strains spread, eliminating them will become more difficult and expensive. Failure to recognize their emergence early could result in resistant malaria epidemics, which would have overwhelming public health and economic consequences.
Despite AL remaining efficacious in Ethiopia [15], the resistance pattern seen with previous antimalarials suggests that artemisinin partial resistance may emerge in several high-transmission regions of SSA by 2030, as predicted by another study [16]. Consequently, a consistent anti-malarial efficacy monitoring system is vital to ensure the early identification of resistant isolates and tracking changes in resistance patterns [17]. Correspondingly, the World Health Organization (WHO) recommends testing anti-malarial drugs’ efficacy at least once every two years in malaria-endemic settings [18]. As the country moves toward malaria elimination, understanding entrusted drug efficacy and safety is mandatory to evaluate malaria control strategies and interventions. The aim of this study was to assess the therapeutic efficacy and safety of AL for the treatment of uncomplicated P. falciparum malaria.
Methods
Study design and period
An in vivo prospective observational study design, with a single-arm and open-label approach, was implemented from September 12, 2022, to February 8, 2023.
Study area
The study was conducted at Teda Health Centre (THC). The health centre serves more than 20,000 people. It is found in Teda subcity, which is located 29 km away in the Gondar city administration, Amhara National Regional State, Ethiopia. It is located at 11° 20′ 57.93" N latitude and 37° 58′ 42.45" E longitude, 2,200 m above sea level. The annual temperature of the area ranges from 22 °C to 29 °C, with the warmest and coldest months being March and July, respectively, and 1,162 mm of annual rainfall. Teda is located 698 km from Addis Ababa, the capital city of Ethiopia. The estimated population of the subcity is 20,000. The population is perennially infected with malaria, with approximately 20–25% of the total population affected annually. The number of cases rises during the major transmission season from September to December.
Study population
Patients with uncomplicated P. falciparum malaria who met the 2009 WHO eligibility criteria for anti-malarial efficacy study guidelines were enrolled and observed [19].
Inclusion criteria
Eligible individuals ranged from 6 months to 70 years of age and had not undergone malaria treatment in the previous 28 days. They were required to be permanent residents within a 10-km radius from the health centre. Additionally, confirmation of P. falciparum mono-infection through microscopy was necessary, with a parasitaemia level falling between 1,000 and 100,000 asexual forms per microlitre. Prospective participants needed to exhibit an axillary temperature of 37.5 ºCelsius or higher, or have a history of fever within the past 24 h. Moreover, they must able to swallow oral medication and demonstrate compliance with the study protocol.
Exclusion criteria
Individuals presenting complications or danger signs of severe malaria were ineligible for participation, as were those with severe malnutrition, indicated by a body mass index below 18.5 kg/m2 or a z score below -3. Additionally, individuals with known diseases other than malaria, such as typhoid fever, typhus, hepatitis, HIV/AIDS, pneumonia, and tuberculosis, were excluded from the study. The presence of regular medications that could interfere with AL pharmacokinetics, including antiretrovirals, ketoconazole, and rifampicin, rendered individuals ineligible [20]. History of hypersensitivity reactions to AL, pregnancy, lactation, and vomiting twice during drug administration also served as exclusion criteria. These criteria were carefully designed to ensure the safety of participants and the reliability of study outcomes.
Sample size determination
The sample size was computed using a single population proportion formula with a 5% failure rate, a desired precision of 5% and a 95% confidence level. To account for patients who are likely to be lost to follow-up, withdrawal or reinfection, an additional 20% was added to the original sample size [19].
Study participants’ enrollment and data collection procedures
Initially, the presence of at least one P. falciparum parasite for every six white blood cells (WBCs) was used as a preliminary eligibility criterion of parasite density, which matches to approximately 1,000 parasites/μl [19]. Then, a clinical screening was performed at an outpatient department for eligibility. Female patients were also tested for pregnancy when clinically suspected. After a detailed explanation of the study procedure, eligible patients were asked for their consent and/or assent. Finally, an anonymous code number was given to them, their addresses, phone number, Kebele and village were recorded, and they were sent to the laboratory again. There, a capillary blood sample was collected for repeated blood film, hemoglobin and dry blood spot (DBS) tests before the patient started treatment.
Blood film preparation and microscopic examination
A capillary blood sample was collected; blood films were made and stained with 10% and 3% Giemsa stain for 10 min and 30 min, respectively. The 10% Giemsa-stained slides were examined immediately using an oil immersion objective, while the 3% Giemsa-stained slides were sent to the University of Gondar, Medical Parasitology Laboratory, for asexual parasite quantification by highly skilled microscopists. Counting was conducted against 200 WBCs. However, in follow-up smears, when the number of asexual parasites was less than 10 per 200 WBCs, counting was performed against at least 500 WBCs. When > 50% discordant results in parasite density were observed between two microscopists, a third, senior malaria microscope expert examined them. Then, the parasite density was calculated by averaging the two closest counts. The number of asexual parasites per microlitre of blood was determined by dividing the number of asexual parasites by the number of WBCs that were counted and multiplying the result by the estimated number of WBCs (8,000/μl).
The blood films were declared negative after examining the thick blood film, and no asexual parasites were found in 100 high-power fields [19].
Haematocrit determination
Anticoagulated blood collected in a heparin containing capillary tube was centrifuged at 11,000 to 12,000 rpm for 5 min. The resulting value was then read from the scale of a microhaematocrit reader, following the procedure described elsewhere [21].
Anti-malarial treatment
Artemether-lumefantrine (A/L 20 mg/120 mg) [Batch No.: (10): HWE111322; Mfd: (11), 11/2021; Exp: (17): 10/2024] manufactured by Ipca Laboratories Ltd., Kandivali, Mumbai, India, was administered to the patients from the THC. The drug was given the first day at 0 and 8 h and twice daily in the following 2 days, in the morning and early evening, i.e., 8–12 h apart, as recommended by the manufacturer and Ethiopian malaria treatment guidelines. A total of 6 tablets were administered to patients weighing 6–15 kg, 12 tablets to those weighing 16–24 kg, 18 tablets to those weighing 25–34 kg, and 24 tablets to those weighing 35 kg or more [9].
The first and next morning doses were administered under direct supervision at the health centre. The study participants were observed for 30 min after taking the drug to see if they vomited. Patients who vomited during observation were given the same dose and observed for an extra 30 min. For the second daily dose, patients were instructed to take the drug at home under the supervision of their caregivers; a phone call was made to remind them to take the drug on time. There was no provision of any kind food at the health centre. However, patients were advised to take the drug with fatty meals such as milk. Finally, the study participants were instructed not to take any medicines by themselves but rather to come to the health centre if they had any illnesses [19].
Concomitant treatment
Primaquine was coadministered in a single low dose of 0.25 mg/kg [9, 22], at the health centre immediately of taking the first dose of AL. In addition, paracetamol was administered with a standard dose of 15 mg/kg every 6 h to all patients with an axillary temperature of ≥ 38 °C [9, 19].
Rescue treatment
Patients who encountered treatment failure were treated with the second-line treatment oral quinine (10 mg quinine sulfate salt/kg) three times daily for seven days and a single low dose primaquine of 0.25 mg/kg [9].
Follow-up
The follow-up schedule was outlined according to the WHO guidelines. Name, identification code and next scheduled visit dates were printed on an appointment card and given to the study participants. They were advised to come to the THC on days 1, 2, 3, 7, 14, 21, and 28 and any other day if they had any clinical conditions. A reminder of their next schedule was made throughout their visits. When absences on the schedule were encountered, a phone call was made, and they were traced and advised by local health extension workers to complete the follow-up.
Clinical assessment, temperature measurement and blood films were performed throughout the schedule. In addition, haematocrit was performed on days 0, 14 and 28. Moreover, for genotyping, DBS samples were collected when a patient was found to have P. falciparum asexual parasitaemia after day-7. Adverse events that emerged after the taking of the drug were asked about and documented throughout the follow-up [19].
Loss to follow-up
An effort was made to find absent study participants, and no treatment outcome was assigned to the lost patients. Patients who were lost to follow-up but who were subsequently found before day-28 were screened for malaria for their healthcare [19].
Patient discontinuation or protocol violation criteria
Study participants were discontinued from the follow-up when they had withdrawn their consent, vomited twice during day-0 drug administration, developed a Plasmodium vivax infection, or had any other infection that made it difficult to determine the treatment outcome. Additionally, study participants were withdrawn from the study when their PCR results indicated that the treatment failure was caused by a new P. falciparum infection [19].
Molecular genotyping
The DBS was collected on Whatman™ 3MM (CAT No. 3030-6461) filter paper. After the DBSs were dried at room temperature, they were reserved in individual plastic bags with silica gel, protected from direct sunlight, humidity and extreme temperature, and stored at −20 °C until transferred to the Armauer Hansen Research Institute (AHRI). The recurrent P. falciparum parasites that were detected during the follow-up were distinguished between reinfection and recrudescence by comparing the block-3 allelic families of merozoite surface protein-2 gene (msp2). The recrudescence was determined by sharing at least one common allele within 20 base pairs in samples from day 0 and the day of recurrent parasitaemia. Reinfection was determined by the absence of a common allele on either allele of msp2.
DNA extraction
The MagMAX-KingFisher™-Flex DNA extraction and purification principle was applied using MagMAX™ DNA Multi-Sample Ultra 2.0 Kit. The DBS with two spots punched at 6 mm diameter was applied to the deep well on the plate and treated overnight at 56 °C in Proteinase-K (Qiagen) and DNA lysis buffer on an Eppendorf thermomixer according to the manufacturer's procedure [23]. Then, DNA-binding beads were added, centrifuged, and incubated, and absolute isopropanol was added. The beads were bound to the DNA and then immobilized on magnets. Finally, the sample mixture was placed on the KingFisher™ Flex, followed by wash-1 and wash-2 solutions, and run.
The extracted DNA was applied in 1 µl on the device, and then using fiber optic technology with natural surface tension qualities to measure the quality of nucleic acid, shorter channel lengths were used. Quantitative PCR was also performed using Bio-Rad CFX96 Touch Real-Time PCR to confirm the absence of Plasmodium species other than P. falciparum and quantify the parasite density in the cycle of threshold (Ct).
PCR amplification
After the primary PCR using msp2 S2 forward primer and msp2 S3 reverse primer, a separate secondary PCR was followed using family-specific primer pairs. Two microliters of the primary amplicon was used as a template in both separate nested PCRs. For N2 PCRs, allele-specific reverse primers of Primer N5 3D7 and Primer M5 FC27 were used for the 3D7/IC and FC27 allelic families of msp2, respectively. The forward allele-specific Primer S1 tail was used for both alleles PCR following the protocol described elsewhere [24].
Gel electrophoresis
The gel was prepared using agarose powder in Tris–Borate-EDTA buffer, stained with 1% ethidium bromide, and 8 µl of N2 product loaded into the wells. The electrophoresis was run at 90 V and 400 A for 80 min. The Invitrogen 1 kb-plus DNA ladder was used to determine the base-pair size of the PCR product. Finally, a chemiPRO UV scanner was used to capture and read the PCR products [25].
Treatment outcome and safety evaluation criteria
Treatment outcomes were classified on the basis of the assessment of clinical and parasitological outcomes according to the 2009 revised WHO guidelines [19]. Thus, all patients were classified as having Early Treatment Failure (ETF), Late Clinical Failure (LCF), Late Parasitological Failure (LPF) or Adequate Clinical and Parasitological Response (ACPR) as primary treatment outcomes [19].
Early treatment failure
Danger signs or severe malaria on day-1, 2 or 3, in the presence of parasitaemia; parasitaemia on day-2 higher than on day-0, regardless of axillary temperature; parasitaemia on day-3 with axillary temperature ≥ 37.5 °C; or parasitaemia on day-3 ≥ 25% of count on day-0.
Late clinical failure
Danger signs or severe malaria in the presence of parasitaemia on any day between day-4 and day-28; or presence of parasitaemia on any day between day-4 and day-28 with axillary temperature ≥ 37.5 °C in patients who did not previously meet any of the criteria of ETF.
Late parasitological failure
Presence of parasitaemia on any day between day-7 and day-28 with an axillary temperature < 37.5 °C; in patients who did not previously meet any of the criteria for ETF or LCF.
Adequate clinical and parasitological response
Adequate clinical and parasitological response is achieved when there is an absence of parasitaemia on day 28, regardless of axillary temperature, in patients who did not previously meet any of the criteria for ETF, LCF or LPF.
Parasite and fever clearance rates were assessed by the proportion of patients free from asexual parasites and fever, respectively, on days 1, 2 and 3 for the secondary treatment outcomes. In addition, all study participants were asked about previous malaria-related symptoms and drug-related adverse events that occurred after the start of therapy or were present on day-0 and worsened during follow-up. In the case of children, the guardians were asked about any side effects of the drug and the child’s tolerance to treatment.
Data quality control and management
A fresh working solution of Giemsa stain was prepared for each batch of blood smears. Additionally, known positive and negative slides were utilized to assess the quality of the Giemsa stain and to control the microscope quality. The accuracy of the thermometer was tested in a water bath at a known temperature before the study began. Moreover, the average of two capillary tube haematocrit results was used. The weight scale was calibrated daily using a standard weight. All PCR master mixes were prepared in a sterile environment in biosafety cabinets. The PCR techniques and DNA extraction materials were checked for expiration dates and tested using known positive and negative quality control samples. Finally, the data were carefully documented and evaluated, and then entered using a double-entry procedure.
Data processing and analysis
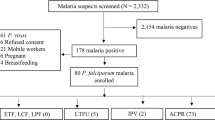
The data were entered and analysed using the WHO Excel worksheet [26] and SPSS version 25. The data were checked for normality using the Shapiro–Wilk test. The data were analysed by per-protocol analysis and Kaplan–Meier survival analysis. A paired sample t test was used to compare the mean haemoglobin levels. The 95% confidence level was used, and a p value of less than 0.05 was considered statistically significant (Fig. 1).
Results
Study participants’ enrollment
A total of 6,019 malaria-suspected patients attending THC were screened during the enrollment period. Of these 2,135 (35.47%) were microscopically positive for malaria. The number of cases of P. falciparum, P. vivax and mixed infection was 942 (44.12%), 1,116 (52.27%) and 77 (3.6%), respectively (Fig. 2).
Baseline characteristics of the study participants
Of the 88 eligible study participants enrolled, most were from the male and adult age groups, with proportions of 61.4% and 63.6%, respectively. The study participants’ mean age was 19.8 years. Seventy-four (84.1%) of those enrolled in the study had an axillary temperature of ≥ 37.5 °C, with a mean of 38.34 °C. The rest, 14 (15.9%), had a history of fever within the previous 24 h. The geometric mean of asexual parasitaemia was 7,402/µl, and the number of study participants with gametocytes was 6 (6.8%). The mean Hgb level was 13.86 mg/dl Table 1.
Treatment outcomes
Of the 88 enrolled study participants, 67 completed the follow-up on their schedule, with three of them having recurrent P. falciparum parasitaemia (Fig. 3).
Primary treatment outcome
The success rates of PCR uncorrected and corrected Kaplan–Meier analyses on day 28 were 95.8% (95% CI 87.5–98.6) and 97.3% (95% CI 89.4–99.3), respectively. Sixty-seven patients completed the follow-up for PP analysis before PCR correction, while 66 patients completed it after PCR correction. Of the properly followed study participants, 64 had an ACPR. The PP PCR-uncorrected and corrected ACPRs were found to be 95.5% and 97%, respectively (Table 2). Three cases of recurrent P. falciparum parasitaemia were found on days 13 and 28. The study participant who had positive parasitaemia on day-13 also had fever and clinical manifestations of malaria. Since the axillary temperature was > 37.5 °C, it formed a PCR uncorrected LCF of 1.5%. The two patients with recurrent parasitaemia had no fever or history of fever in the previous 24 h. Therefore, the uncorrected LPF was 3%. However, after correction, only two of the recurrent parasitaemia confirmed recrudescence, and the remaining new infection was excluded. Therefore, the corrected treatment failures were an LCF of 1.5% and an LPF of 1.5% (Fig. 4).
Secondary treatment outcomes
Parasite clearance
Approximately half of the study participants (48.9%) cleared parasitaemia on day-1. Seventy-five (85.2%) and 86 (97.7%) of 88 study participants cleared parasitaemia on day-2 and day-3, respectively. On day-0, the median parasitaemia was 6,374/µ (1,213–96,661); it decreased 508/µ on day-1, 243/µ on day-2 and 124/µ on day-3.
Fever clearance
For the fever clearance rate, the denominator used was the number of patients having an axillary temperature of ≥ 37.5ºC on day-0, which was 74 (84.1%). The fever cleared in 67 (90.54%) of the patients. All patients were free of fever on day-2 and afterward. The mean axillary temperature of all the study participants improved from the baseline of 38.14 °C (36.7–40.5) to 36.61 (35.60–37.80), 36.44 (35.20–37.20) and 36.70 (36.00–37.30) on day-1, day-2 and day-3, respectively.
Gametocyte clearance
There were only six study participants with gametocytes (6.8%) at baseline. Four were in the 5–15-year-old age group and the remaining two were from the adult group, but no gametocytes were found in the underfive year age group. Two of them had cleared gametocytes on day-1 while the remaining four remained positive. All of the gametocyte-positive cases had cleared gametocytaemia by day-2. No gametocytes were found microscopically thereafter throughout the follow-up, including on the days of the treatment failures.
Genotyping results of recurrent malaria
Three study participants were found to have P. falciparum parasitaemia after the completion of treatment throughout the entire follow-up. The days in which P. falciparum parasites were found were day-13 and day-28. Only one had a fever during the presentation on the unscheduled visit on day-13. Recurrent infections were distinguished as recrudescence or reinfection using the allelic families of msp2. Two of the study participants showed recrudescence since samples from day-0 and the day of recurrent parasitaemia shared at least one common allele within 20 base pairs. However, the remaining was reinfection since it did not show any common allele on either allele of msp2.
Haemoglobin improvement
The mean haemoglobin was 13.10 (SD: 1.29425) on day-0 and 13.27 (SD: 0.96547) on day-14. However, a significant increase was observed on day-28, with the mean haemoglobin rising to 13.69 (SD: 0.9000), as determined by a paired sample t-test, t (63) = -6.061, p = 0.000 (two-tailed) at a 95% confidence interval.
Adverse events
Adverse events that were raised after the initiation of AL treatment or worsened from baseline were reported, with lip dryness (11–15.4%), mouth rash (1.1–18.2%), abdominal pain (2.3–15.9%), dizziness (3.7–9.1%) and coughing (1.1–9.1%) being the most common Table 3.
Discussion
In this study, the PCR-uncorrected and PCR-corrected ACPRs were 95.5% and 97%, respectively, in the per-protocol analysis. Even with extensive utilization, the drug’s therapeutic efficacy is still far from the WHO alarming threat threshold. The results are consistent with an earlier study in southwestern Ethiopia (97.8% corrected ACPR), that was conducted seven years after it had been introduced as a first-line drug [27].
The 97% corrected ACPR is also in agreement with other studies conducted in different transmission settings in Ethiopia: Chewaka 96% [28], Enfranze 95% [29] and consistent with the pooled 98.7% ACPR of the meta-analysis of Ethiopian studies [15]. The minor differences may be due to seasonal variations in the study period. Crompton et al. reported that short-lived naturally acquired humoral responses against P. falciparum antigens became intense after the major malaria transmission season [30]. In addition, the degree of endemicity in the study areas may have contributed to the slight differences. Moreover, the study participants’ age composition, compliance with the study protocol, or fatty meal provision during drug administration might all faintly affect the rates of therapeutic efficacy.
The results of this study indicate the continued success of AL treatment despite the increase in single nucleotide polymorphism mutation prevalence in k13 that was reported in the area located closer to this study site, Northwest Ethiopia [11]. Regardless of the repeated detection of treatment failure in Cambodia [31,32,33], AL was reported to be efficacious in SSA studies [34,35,36,37,38,39].
The consistent success rate of AL in this study and other malaria-endemic SSA countries might be because the populations in these study areas are repeatedly exposed to infectious mosquito bites, allowing them to develop naturally acquired immunity to multiple parasite strains [40, 41]. This background immunity is believed to have a synergistic role with antimalarial drugs and is associated with a lower likelihood of treatment failure [42, 43].
In Ethiopia, k13 mutation was found to be increasing, from 2.4% in 2013/14 [10] to 9.5% after three years [11]. However, a high level of population immunity is believed to boost immune selection in preference to resistant selection. Therefore, it slowed resistance emergence by allowing sensitive lineages to persist at the expense of the expansion of a resistant lineage.
Two study participants experienced recrudescence in the current study, which was confirmed by the block-3 alleles of msp2 in paired samples. They had LCF and LPF and were 16 and 14 years old, respectively. At baseline, their parasite densities were 3,193/µl and 17,972/µl. The former, who had LCF, was found to have positive parasitaemia on day-3, while the latter, who had LPF, cleared parasitaemia on day-2. Since partial resistance to artemether seldom results in treatment failure in the absence of partner drug resistance [44], the presence of parasitaemia on day-13 may be due to the emergence of resistance to lumefantrine. This was explained by an in vitro study in which the efficacious lumefantrine drug boosted artemisinin-killing activity even though parasites have artemisinin resistance with the k13 mutation [45].
Day-3 parasitaemia clearance was 97.7% in this study. This is uneven, with other studies in Ethiopia [11, 46,47,48] and elsewhere [37, 49] reporting complete clearance on day-3. However, it is in agreement with other studies in Ethiopia [28, 29, 50] and elsewhere [39, 51]. One of two day-3 positive parasitaemia patients in this study had a high parasite density at baseline with 93,960/µl parasites, but the other, with a baseline parasitaemia of 3,193/µl developed LCF. It has been identified that a high baseline parasite density influences parasite clearance rates [52]. In contrast, delayed parasite clearance (day-3 parasite-positive rate) can be used as an indicator of artemisinin partial resistance [53, 54].
Likewise, of the patients who were febrile at baseline, 90.5% cleared fever on day-1, and all cleared fever on day-2. This finding is consistent with the studies conducted in Ethiopia [46, 47, 55] and Kenya [37]. This demonstrates the continued reliability of AL with rapid clinical and parasitological resolution.
In this study, the initial gametocyte carriage in six patients was reduced to four on day-1 and all of them cleared on day-2. When compared to prior Ethiopian studies that reported day-3 [28, 50, 56] and day-7 [29, 57] overall clearances, this study's clearance rate is strikingly rapid. The absence of gametocytes after day-1 might be due to the combined gametocidal actions of AL coadministration with primaquine. This is in agreement with the individual meta-analysis that showed an earlier gametocyte clearance rate with day-0 coadministration of AL and primaquine [58].
The mean haemoglobin level increased slightly on day-14 in the current study. On day-28, it increased significantly. The resolution of anaemia and restoration of haemoglobin after treatment were demonstrated by an individual patient data analysis conducted in SSA [59]. The findings of this study are in agreement with the studies conducted in Ethiopia [48, 56, 60].
Artemether-lumefantrine was reported to have the most tolerated anti-malarial effects; in this study, the drug continued its effectiveness with safe tolerance by all age groups of study participants. The most common adverse events reported after initiation of the drug were mouth rash, lip dryness and ulcer, abdominal pain, dizziness and cough. These adverse events are expected since all of them were already mentioned as side effects of the drug [20].
Limitations of the study
The study has some limitations, such as the high rate of loss to follow-up, which challenges the robustness of the findings. Despite attempts to mitigate this, bias may still exist, especially if those lost differ systematically from those who remained, potentially skewing results. Using a single genotyping marker may restrict the accuracy of true treatment failures. Although selected for relevance, incorporating additional markers could enhance understanding of true recrudescence. The haemoglobin measuring tool may introduce errors, as haemoglobin values were derived from haematocrit values.
Conclusion
Despite its limitations, this study demonstrated that AL has continued to be an efficacious drug for uncomplicated P. falciparum malaria treatment with rapid clinical and parasitological resolution and negligible adverse events. It also has a considerable effect on improving the baseline haemoglobin level. However, further investigations are warranted, as the burden of malaria is steadily rising in the study area. For increased awareness and updated evidence, consistent therapeutic efficacy studies are needed.
Availability of data and materials
The individual patients data will be provided with the reasonable request.
Abbreviations
- ACPR:
-
Adequate clinical and parasitological response
- AHRI:
-
Armauer hansen research institute
- AL:
-
Artemether lumefantrine
- ETF:
-
Early treatment failure
- LCF:
-
Late clinical failure
- LPF:
-
Late parasitological failure
- PCR:
-
Polymerase chain reaction
- SSA:
-
Sub Saharan Africa
- THC:
-
Teda Health Centre
- WHO:
-
World Health Organization
References
WHO. World Malaria Report 2023. Geneva: World Health Organization; 2023.
White NJ, Ashley EA. Malaria. In: Loscalzo J, Fauci A, Kasper D, Hauser S, Longo D, Jameson JL, editors. Harrison’s Principles of Internal Medicine. 21st ed. New York: McGraw-Hill Education; 2022.
Federal Republic Ethiopia Ministry of Health. National Malaria Elimination Programme (NMEP); 2021. https://www.mohgovet/en/initiatives-4-col/National_Malaria_Elimination_Program?language_content_entity=en. Accessed 2 Aug 2022.
WHO. World malaria report 2022. Geneva: World Health Organization; 2022.
Eshetu T, Muhamed B, Awol M, Kassa Z, Getu M, Derso A, et al. A retrospective analysis of malaria trends in Maksegnit Health Center over the last seven years, Northwest Ethiopia: 2014–2020. J Parasitol Res. 2022;2022:5170550.
Ewnetu Y, Lemma W. Highland malaria transmission dynamics in space and time before pre-elimination era. Northwest Ethiopia J Epidemiol Glob Health. 2022;12:363–71.
WHO. Guidelines for malaria. Geneva: World Health Organization; 2021.
Federal Republic Ethiopia Ministry of Health. Malaria diagnosis and treatment: a guideline for health workers in Ethiopia. Addis Ababa. 2004
Federal Republic Ethiopia Ministry of Health. National Malaria Guidelines.4th Edn. Addis Ababa, Ethiopia; 2018.
Bayih AG, Getnet G, Alemu A, Getie S, Mohon AN, Pillai DR. A unique Plasmodium falciparum Kelch 13 gene mutation in northwest Ethiopia. Am J Trop Med Hyg. 2016;94:132–5.
Alemayehu AA, Castaneda-Mogollon D, Tesfa H, Getie S, Mohon AN, Balasingam N, et al. Expansion of the Plasmodium falciparum Kelch 13 R622I mutation in Northwest Ethiopia. Res Square. 2021. https://doi.org/10.21203/rs.3.rs-171038/v1.
Stokes BH, Dhingra SK, Rubiano K, Mok S, Straimer J, Gnädig NF, et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. Elife. 2021;10: e66277.
Tumwebaze PK, Conrad MD, Okitwi M, Orena S, Byaruhanga O, Katairo T, et al. Decreased susceptibility of Plasmodium falciparum to both dihydroartemisinin and lumefantrine in northern Uganda. Nat Commun. 2022;13:6353.
Bakari C, Mandara CI, Madebe RA, Seth MD, Ngasala B, Kamugisha E, et al. Trends of Plasmodium falciparum molecular markers associated with resistance to artemisinins and reduced susceptibility to lumefantrine in Mainland Tanzania from 2016 to 2021. Malar J. 2024;23:71.
Abamecha A, Yilma D, Adissu W, Yewhalaw D, Abdissa A. Efficacy and safety of artemether–lumefantrine for treatment of uncomplicated Plasmodium falciparum malaria in Ethiopia: a systematic review and meta-analysis. Malar J. 2021;20:213.
Scott N, Ataide R, Wilson DP, Hellard M, Price RN, Simpson JA, et al. Implications of population-level immunity for the emergence of artemisinin-resistant malaria: a mathematical model. Malar J. 2018;17:279.
Nsanzabana C. Time to scale up molecular surveillance for anti-malarial drug resistance in sub-saharan Africa. Malar J. 2021;20:1–5.
WHO. Artemisinin and artemisinin-based combination therapy resistance: status report. Geneva: World Health Organization; 2016.
WHO. Methods for surveillance of antimalarial drug efficacy. Geneva: World Health Organization; 2009.
Novartis Pharmaceuticals Corporation. COARTEM® (artemether and lumefantrine) tablets, for oral use. 2019.
Mondal H, Lotfollahzadeh S. 2024 Hematocrit. In: StatPearls Publishing [Internet].
WHO. World malaria report 2019. Geneva: World Health Organization; 2019.
Thermo Fisher Scientific. MagMAX™ DNA Multi-Sample Kit. 2016.
Snounou G. Genotyping of Plasmodium spp. nested PCR. Methods Mol Med. 2002;72:103–16.
WWARN. Agarose Gel Electrophoresis of msp1, msp2 and glurp. https://www.iddo.org/procedure/agarose-gel-electrophoresis-msp1-msp2-and-glurp. Accessed 15 Aug 2022.
WHO. Tools for monitoring antimalarial drug efficacy. https://www.who.int/teams/global-malaria-programme/case-management/drug-efficacy-and-resistance/tools-for-monitoring-antimalarial-drug-efficacy. Accessed 15 Aug 2022.
Mekonnen SK, Medhin G, Berhe N, Clouse RM, Aseffa A. Efficacy of artemether–lumefantrine therapy for the treatment of uncomplicated Plasmodium falciparum malaria in Southwestern Ethiopia. Malar J. 2015;14:317.
Abamecha A, Yilma D, Addisu W, El-Abid H, Ibenthal A, Noedl H, et al. Therapeutic efficacy of artemether-lumefantrine in the treatment of uncomplicated Plasmodium falciparum malaria in Chewaka District. Ethiopia Malar J. 2020;19:240.
Getnet G, Fola AA, Alemu A, Getie S, Fuehrer H-P, Noedl H. Therapeutic efficacy of artemether–lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in Enfranze, north-west Ethiopia. Malar J. 2015;14:258.
Crompton PD, Kayala MA, Traore B, Kayentao K, Ongoiba A, Weiss GE, et al. A prospective analysis of the Ab response to Plasmodium falciparum before and after a malaria season by protein microarray. Proc Natl Acad Sci USA. 2010;107:6958–63.
Denis MB, Tsuyuoka R, Lim P, Lindegardh N, Yi P, Top SN, et al. Efficacy of artemether–lumefantrine for the treatment of uncomplicated falciparum malaria in northwest Cambodia. Trop Med Int Health. 2006;11:1800–7.
Song J, Socheat D, Tan B, Seila S, Xu Y, Ou F, et al. Randomized trials of artemisinin-piperaquine, dihydroartemisinin-piperaquine phosphate and artemether-lumefantrine for the treatment of multi-drug resistant falciparum malaria in Cambodia-Thailand border area. Malar J. 2011;10:231.
Peto TJ, Tripura R, Callery JJ, Lek D, Nghia HDT, Nguon C, et al. Triple therapy with artemether–lumefantrine plus amodiaquine versus artemether–lumefantrine alone for artemisinin-resistant, uncomplicated falciparum malaria: an open-label, randomised, multicentre trial. Lancet Infect Dis. 2022;22:867–78.
Konaté A, Barro-Kiki PCM, Angora KE, Bedia-Tanoh AV, Djohan V, Kassi KF, et al. Efficacy and tolerability of artesunate-amodiaquine versus artemether-lumefantrine in the treatment of uncomplicated Plasmodium falciparum malaria at two sentinel sites across Côte d’Ivoire. Ann Parasitol. 2018;64:49–57.
Raman J, Allen E, Workman L, Mabuza A, Swanepoel H, Malatje G, et al. Safety and tolerability of single low-dose primaquine in a low-intensity transmission area in South Africa: an open-label, randomized controlled trial. Malar J. 2019;18:209.
Mhamilawa LE, Ngasala B, Morris U, Kitabi EN, Barnes R, Soe AP, et al. Parasite clearance, cure rate, post-treatment prophylaxis and safety of standard 3-day versus an extended 6-day treatment of artemether–lumefantrine and a single low-dose primaquine for uncomplicated Plasmodium falciparum malaria in Bagamoyo district, Tanzania: a randomized controlled trial. Malar J. 2020;19:216.
Kishoyian G, Njagi EN, Orinda GO, Kimani FT, Thiongo K, Matoke-Muhia D. Efficacy of artemisinin–lumefantrine for treatment of uncomplicated malaria after more than a decade of its use in Kenya. Epidemiol Infect. 2021;149: e27.
Uwimana A, Umulisa N, Venkatesan M, Svigel SS, Zhou Z, Munyaneza T, et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect Dis. 2021;21:1120–8.
Falade CO, Orimadegun AE, Olusola FI, Michael OS, Anjorin OE, Funwei RI, et al. Efficacy and safety of pyronaridine-artesunate versus artemether-lumefantrine in the treatment of acute uncomplicated malaria in children in South-West Nigeria: an open-labelled randomized controlled trial. Malar J. 2023;22:154.
Pinkevych M, Petravic J, Chelimo K, Kazura JW, Moormann AM, Davenport MP. The dynamics of naturally acquired immunity to Plasmodium falciparum infection. PLoS Comput Biol. 2012;8: e1002729.
Barua P, Beeson JG, Maleta K, Ashorn P, Rogerson SJ. The impact of early life exposure to Plasmodium falciparum on the development of naturally acquired immunity to malaria in young Malawian children. Malar J. 2019;18:11.
Djimde AA, Doumbo OK, Traore O, Guindo AB, Kayentao K, Diourte Y, et al. Clearance of drug-resistant parasites as a model for protective immunity in Plasmodium falciparum malaria. Am J Trop Med Hyg. 2003;69:558–63.
Greenhouse B, Slater M, Njama-Meya D, Nzarubara B, Maiteki-Sebuguzi C, Clark TD, et al. Decreasing efficacy of antimalarial combination therapy in Uganda is explained by decreasing host immunity rather than increasing drug resistance. J Infect Dis. 2009;199:758–65.
WHO. Malaria: artemisinin partial resistance. Geneva: World Health Organization; 2022.
Kümpornsin K, Loesbanluechai D, de Cozar C, Kotanan N, Chotivanich K, White NJ, et al. Lumefantrine attenuates Plasmodium falciparum artemisinin resistance during the early ring stage. Int J Parasitol Drugs Drug Resist. 2021;17:186–90.
Tadele G, Jaiteh FK, Oboh M, Oriero E, Dugassa S, Amambua-Ngwa A, et al. Persistence of residual submicroscopic P. falciparum parasitemia following treatment of artemether-lumefantrine in Ethio-Sudan Border Western Ethiopia. Antimicrob Agents Chemother. 2022;66:e00002-22.
Teklemariam M, Assefa A, Kassa M, Mohammed H, Mamo H. Therapeutic efficacy of artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria in a high-transmission area in northwest Ethiopia. PLoS ONE. 2017;12: e0176004.
Gubae K, Mohammed H, Sime H, Hailgiorgis H, Mare AK, Gidey B, et al. Safety and therapeutic efficacy of artemether-lumefantrine in the treatment of uncomplicated Plasmodium falciparum malaria at Shecha health centre, Arba Minch. Ethiopia Malar J. 2023;22:9.
Davlantes E, Dimbu PR, Ferreira CM, Florinda Joao M, Pode D, Félix J, et al. Efficacy and safety of artemether–lumefantrine, artesunate–amodiaquine, and dihydroartemisinin–piperaquine for the treatment of uncomplicated Plasmodium falciparum malaria in three provinces in Angola, 2017. Malar J. 2018;17:144.
Deressa T, Seid ME, Birhan W, Aleka Y, Tebeje BM. In vivo efficacy of artemether–lumefantrine against uncomplicated Plasmodium falciparum malaria in Dembia District. Northwest Ethiopia Ther Clin Risk Manag. 2017;13:201–6.
Wu Y, Soe MT, Aung PL, Zhao L, Zeng W, Menezes L, et al. Efficacy of artemether-lumefantrine for treating uncomplicated Plasmodium falciparum cases and molecular surveillance of drug resistance genes in Western Myanmar. Malar J. 2020;19:304.
Stepniewska K, Ashley E, Lee SJ, Anstey N, Barnes KI, Binh TQ, et al. In vivo parasitological measures of artemisinin susceptibility. J Infect Dis. 2010;201:570–9.
WHO. Global plan for artemisinin resistance containment (GPARC). Geneva: World Health Organization; 2011.
Tun KM, Imwong M, Lwin KM, Win AA, Hlaing TM, Hlaing T, et al. Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. Lancet Infect Dis. 2015;15:415–21.
Tadesse M. Therapeutic efficacy and safety of artemether-lumefantrine plus a single low-dose primaquine for the treatment of uncomplicated Plasmodium falciparum malaria at Maksegnit Health Center, Northwest Ethiopia. Thesis. Bahir Dar University, Ethiopia. 2023.
Wudneh F, Assefa A, Desalegn Nega HM, Solomon H, Kebede T, Woyessa A, et al. Open-label trial on efficacy of artemether/lumefantrine against the uncomplicated Plasmodium falciparum malaria in Metema district. Northwestern Ethiopia Ther Clin Risk Manag. 2016;12:1293.
Ebstie YA, Zeynudin A, Belachew T, Desalegn Z, Suleman S. Assessment of therapeutic efficacy and safety of artemether-lumefantrine (Coartem®) in the treatment of uncomplicated Plasmodium falciparum malaria patients in Bahir Dar district, Northwest Ethiopia: an observational cohort study. Malar J. 2015;14:236.
Stepniewska K, Humphreys GS, Gonçalves BP, Craig E, Gosling R, Guerin PJ, et al. Efficacy of single-dose primaquine with artemisinin combination therapy on Plasmodium falciparum gametocytes and transmission: an individual patient meta-analysis. J Infect Dis. 2022;225:1215–26.
Zwang J, D’Alessandro U, Ndiaye J-L, Djimdé AA, Dorsey G, Mårtensson AA, et al. Haemoglobin changes and risk of anaemia following treatment for uncomplicated falciparum malaria in sub-Saharan Africa. BMC Infect Dis. 2017;17:443.
Assefa A, Kassa M, Tadese G, Mohamed H, Animut A, Mengesha T. Therapeutic efficacy of artemether/lumefantrine (Coartem®) against Plasmodium falciparum in Kersa. South West Ethiopia Parasit Vectors. 2010;3:1.
Acknowledgements
We would like to thank the University of Gondar for financial and material support. We would also like to acknowledge the THC staff for their professional support and the Gondar town health office for providing the required information. Moreover, we would like to thank the study participants. Furthermore, we appreciate the support of Ms Zufan Yiheyis, Dr. Gebeyaw Getnet and Mr. Tegegne Eshetu for their support during data collection, genotyping and data analysis. Finally, we would like to thank the AHRI for assisting in the genotyping and providing technical support.
Funding
This study was fully funded by the University of Gondar.
Author information
Authors and Affiliations
Contributions
Conceived the study, compiled the protocol, designed the experiments, and led data collection: DW, YT, MB, and AA. Microscopy examination and parasite counting: DW, YT, AA, MS, and WA. Performed genotyping: DW, MKB, and AJZ. Analysed the data: DW, YT, MB, and AA. Assisted study implementation: DW, YT, MKB, MW, and ET. Drafted the manuscript and prepared figures: DW. Critically reviewed and contributed to writing: YT.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
A letter of ethical clearance was obtained from the ethical review committee of the School of Biomedical and Laboratory Sciences, College of Medicine and Health Science, University of Gondar (Ref. No. SBLS/398/2022), and written informed consent and/or assent was obtained from all study participants. Verbal consent was also obtained for the pregnancy test. A transport reimbursement was provided to all the study participants. This trial has been registered retrospectively at https://pactr.samrc.ac.za as PACTR202309773069812 on September 1, 2023.
Consent for publication
Not applicable.
Competing interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Woldesenbet, D., Birhanie, M., Abere, A. et al. Therapeutic efficacy and safety of artemether-lumefantrine combination therapy for the treatment of uncomplicated Plasmodium falciparum malaria at Teda Health Centre, Northwest Ethiopia, 2022/23. Malar J 23, 266 (2024). https://doi.org/10.1186/s12936-024-05082-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12936-024-05082-y