Abstract
Introduction
Healthcare financing systems, dependent on out-of-pocket expenditure(OOPE), impose a heavy burden on those who use the services regularly, such as patients suffering from chronic diseases. High OOPE for health services leads to decreased utilization of the services and/or catastrophic health expenditure, which would significantly impede the achievement of Universal Health coverage.
Objective
We aimed to determine variations in OOPE and factors associated with Catastrophic Health Expenditure (CHE) of households with patients suffering from non-communicable diseases(NCDs) in four districts.
Methods
A survey was conducted among 2344 adult patients having selected NCD/s. Multi-stage stratified cluster sampling selected respondents from 4 districts representing urban, rural, semi-urban, and estate. Data was collected using a validated interviewer-administered questionnaire. Logistic regression identified the predictors of CHE(> 40%). Significance was considered as 0.05.
Results
Common NCDs were hypertension(29.1%), diabetes(26.8.0%), hyperlipidaemia(9.8%) and asthma(8.2%). Only 13% reported complications associated with NCDs. Fifty-six percent(N = 1304) were on regular clinic follow-up, and majority utilized western-medical government hospitals(N = 916,70.2%). There were 252 hospital admissions for chronic-disease management in the past 12 months. Majority(86%) were admitted to government sector hospitals. Most patients incurred nearly SLR 3000 per clinic visit and SLR 3300 per hospital admission. CHE was beyond 40% for 13.5% of the hospital admissions and 6.1% of the regular clinic follow-up. Patients admitted to private sector hospitals had 2.61 times higher CHE than those admitted to government sector hospitals.
Conclusions
Patients with NCDs incurred high OOPE and faced CHE during healthcare seeking in Sri Lanka. The prevalence of NCDs and complications were high among the participants. Patients with chronic conditions incur high OOPE for a single clinic visit and a hospital admission. Patients incur high OOPE on direct medical costs, and district-wise variations were observed. The proportion with more than 40% CHE on monthly clinic care was high. Patients being followed up in the government sector are more likely to have CHE when obtaining healthcare and are more likely to face barriers in obtaining needed health services. The services rendered to patients with chronic conditions warrant a more integrative approach to reduce the burden of costs and related complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Sri Lanka, the burden of non-communicable diseases is growing. Also, there is an increased focus on ensuring that people are protected against financial risks due to accessing care. Universal Health Coverage (UHC), which is one of the overarching objectives of the Sustainable Development Goals, which are to be achieved by 2030, is defined as “attempts to ensure that all people obtain the health services they need without suffering financial hardship when paying for them” [1]. Considering financial protection, no “best financing strategy “fits all countries or situations. Therefore, the challenge is identifying the pitfalls and the most suitable healthcare strategy to achieve UHC [2].
In Sri Lanka, inpatient care is mainly provided through the public sector, and outpatient care through both the public and private sectors. The private sector is sometimes utilized as a substitute for the government sector and sometimes as complementary. The government is the main financier of the health care expenditure, and is universally free of charge at the point of delivery [3]. In 2019 the government was responsible for providing 47.2% of CHE, out of pocket expenditure(OOPE) contributed to 51% of CHE [4]. Sri Lankan households,more than 60% of households incur high OOPE [5]. Evidence suggests that patients incur OOPE expenses when utilizing public and private sector services. In 2021 the budget allocation to health was Sri Lankan Ruppes million 24,500. Voluntary health insurance (VHI) contributes about 5% of total private financing, and the private insurance market has shown considerable growth in recent years [6]. Sri Lanka's healthcare allocations are relatively low compared to other countries in the region, posing challenges in meeting the growing demands for healthcare services and addressing the rising burden of diseases [7].
Non-communicable diseases are diseases that are not transmitted from one person to another. Globally the burden of non-communicable diseases (NCDs) is growing [8]. NCDs are diseases that need continuity of care. Hence the costs incurred due to NCDs are a significant financial burden to people suffering from these diseases. In a time and era where there is an increased focus on ensuring that people are protected against financial risks due to accessing care, addressing NCDs and the associated costs is essential. Especially since escalating NCD costs correlate with the aging of the population with the demographic transition taking place in Sri Lanka, and is projected to rise in the next decade, the country needs to be prepared to face the rising demands [9]. The increasing global prevalence of chronic non-communicable diseases (NCDs), compounded by their chronic nature and the frequent occurrence of multimorbidity, has led to a significant rise in out-of-pocket expenditures (OOPE) for affected individuals, placing a substantial financial burden on households worldwide [10].
Large OOPE for healthcare have been shown to impede healthcare-seeking behavior and drive families towards impoverishment [11]. Therefore, it is crucial to identify the characteristics of persons likely to incur OOPE and diseases and conditions that are most likely to generate large OOPE. In the current context where the country is grappling with a pandemic and an economic crisis, its timely to re-visit and generate this information to ensure the sustainability of the services as the macroeconomic challenges we are currently observing are interrelated with poverty and health.
The OOPE data should be valid, reliable, and up-to-date for policymakers for evidence-informed decision-making. Currently, the OOPE data is generated through the data that are collected through the Household Income and Expenditure Survey (HIES) conducted by the Census and the Statistics Department using the HIES questionnaire [12]. The HIES questionnaire has many components, and one section comprises health. However, it has been observed that the data gathered during the HIES survey does not consider direct non-medical costs or other essential components. Hence the need for a comprehensive tool to assess OOPE data was felt.
Sri Lanka's healthcare system has achieved remarkable success despite limited resources. However, to achieve Universal Health Coverage (UHC), healthcare strategy needs to be reevaluated. This includes revenue raising, pooling, purchasing, and addressing inefficiencies. Evidence-based policymaking is crucial. A review of the literature reveals a need for more recent comprehensive national estimates of Out-Of-Pocket Expenditure (OOPE) by the general population and individuals with chronic conditions. Therefore, the study aims to describe the variation in OOPE by chronic condition/ conditions and factors associated with catastrophic health expenditure of households with patients suffering from selected chronic conditions in four districts in Sri Lanka.
Methods
We conducted a cross-sectional study among male and female adults diagnosed with a selected NCD/s in four Sri Lankan districts. The sample size was computed using an alpha-value of 0.05, an estimated proportion of high OOPE of 40% [7, 13], and an absolute precision of 3.0%, which was subsequently inflated by adding a non-response rate of 15% and since cluster-sampling method was adopted, the effect of clustering was overcome by correcting using a design effect of 2. Therefore, the expected minimum sample size was 2300. Sampling was conducted using stratified cluster smalping. Four districts ( Gampaha, Ampara, Jaffna and Nuwaraeliya) were considered as strata. Sri Lanka has twenty-five administrative districs representing nine provinces. Economic factors and level of urbanization among the districts vary. Four districts to represent four provinces considering, population-size, population density, economic functions such as cost of living, and governance were chosen [14, 15]. Grama Niladari(GN) divisions were stratified by the four districts in the second stage of stratification and were selected based on Probability Proportionate to Size(PPS).
A Grama Niladari(GN) division [16] (government-approved smallest administrative sector) was considered a cluster, and the cluster size was 20. The number of households was identified from 115 clusters identified from four districts of Sri Lanka representing urban (Gampaha), rural (Ampara), semi-urban (Jaffna), and estate (Nuwaraeliya). The claissfication to urban, semi-urban, rural and estate was done based on factors such as populationsize, population density, economic functions, and governance [14]. The selection of process is described in Fig. 1.
An extra cluster was chosen in each group as a backup in case of unforeseen problems with the initial sample. A random geographical point was selected within sampled GN divisions, and this was the starting point for sampling within a cluster. The study unit comprised male and female patients aged 18 years and older, diagnosed with selected NCDs for over three months and regularly receiving treatment for their chronic conditions. Twenty consecutive houses in one direction from this point which consisted a NCD patient were selected and only one adult who was eleigibe to partipate was chosen from one household where Kish grid method to select one NCD patient per household [17]. All eligible households were offered written study information and selected participants consented prior to their recruitment.
The study was conducted from April to August 2022. An interviewer-administered questionnaire (IAQ) was used for data gathering and administered in all three languages (Sinhala, English, and Tamil). The IAQ was developed and validated (judgmental) for the current survey, and pre-tested prior to use among a similar group of participants outside the target study settings, and the questionnaire was further refined based on their feedback and suggestions (Supplement). The questionnaire gathered information on sociodemographics, socioeconomic, healthcare seeking for chronic illnesses, and details on hospital admissions and related costs. Trained data collectors administered the questionnaire. The principal investigator carried out data entry. Statistical analysis was conducted employing the software package STATA Version 14.
Categorical data were expressed as proportions/percentages with 95% confidence intervals.
The total cost of illness for NCDs was calculated from the patient's perspective. It involved adding direct (related to patient care) and direct non-medical costs. Direct costs include medical expenses such as medications, labortarory investigations as well as non-medical costs such as meals, by-stander costs and travel to the hospital. In calculating OOPE, both components (direct medical and direct non-medical costs), were considered. Quantitative data, normally distributed, were summarized in terms of mean and standard deviation(SD) and non-normally distributed as the median and interquartile range(IQR). Following data entry, frequency distribution was examined of each variable, and incompatible entries were identified and corrected by referring to the original questionnaires. The economic burden of the patients suffering from NCDS was assessed using direct medical and non-medical costs incurred by patients due to the disease.
The associations between each contributory factor and high OOPE (categorized into Catastrophic and non-catastrophic) were analyzed using bivariate cross-tabulations. Different definitions and thresholds have been used in the literature to calculate catastrophic health expenditure. Various studies have used different threshold levels. In this particular study, we calculated the occurrence of catastrophic expenditure using the 15% threshold of total expenditure [7, 18,19,20]. The correlates significantly associated with high Catastrophic healthcare expenditure were identified using appropriate tests. Mann Whitney U test was used to compare median OOPE between government sector and private sector follow ups. The correlates significantly associated were used in logistic regression models for multivariate analysis. The odds ratios with confidence intervals were calculated using binary logistic regression to quantify the strength of association between CHE and correlates. General Sir John Kotelawala Defence University Ethics Committee granted the project ethical approval.
Results
The study was conducted among 2344 patients with chronic medical illnesses. Among them, the majority were females(52.8%), aged 30 to 60 years(67.4%), Sinhalese(51.5%), educated GCE O/L or above(69.3%), and married (74.0%) (Table 1). Nearly 41% were employed, and the majority(37.1%) were private sector employees. Only 32.7% of patients had an average monthly income above 60,000 SLR. The median(IQR) distance to any healthcare institution was 5 km(7 km). The mean distance to any healthcare institution in the urban, semi-urban, rural, and estate sectors were 2(SD ± 0.9)km, 5(SD ± 1.6)km, 6(SD ± 2.3)km and 9(SD ± 3.1)km, respectively.
Cosidering proportion of diseases, majority had hypertension (29.1%), followed by diabetes (26.8%), dyslipidemia (9.8%), and asthma (8.2%). Nearly 32% had more than one chronic medical illness, while only 55.6% were on regular clinic follow-ups (Table 2). Nearly 50% (N = 1167) had suffered from NCDs for over five years. Only 12.8% (N = 298) had self-reported NCD complications. Most utilized Western medicines (73.0%) for their chronic medical illnesses. Interestingly, 9.4% spent on religious and cultural activities to cure chronic medical illnesses.
Out of Pocket expenditure for hospital admissions and follow-up visits
Out of Pocket Expenditure (OOPE) was calculated for both follow-up visits and admissions for NCD management. By combining direct medical and direct non-medical costs incurred, the total OOPE was calculated. OOPE was measured in Sri Lankan Rupees (SLR). Sector-wise variations were observed in OOPE for both hospital admissions and follow-up visits. For a regular follow-up an urban, rual estate and semi-urban patient spent a median (IQR) of SLR 3903 (3000), 6564 (2000),5162(1500),and 7224(2750) respectively.
Among the sample, 252 patients(10.7%) had hospital admissions for NCD management. Among them 51.6%(N = 130) were females. Nearly 86%(N = 217) were admitted to government hospitals. During admissions majority(N = 212, 84.1%) incurred direct non-medical OOPE, while 15.9%(N = 40) had both direct medical and non-medical OOPE. None had borne direct medical costs alone. Most patients(N = 159, 63.2%) had a total OOPE of less than 5000 rupees per admission. Patients had spent a median(IQR) of SLR 2750(3500) on medications and 2500 (2300) on laboratory investigations. Patients had spent a median (IQR) of 800(500) rupees per day for meals and 500(800) SLR per day for transport. Only 11.5% of the patients had spent a median(IQR) of 1500(1350) SLR for bystanders per day. The average cost for a hospital admission, it was SLR 3100 (Table 3).
Nearly 25%(N = 572) on regular NCD follow-ups responded to OOPE due to clinic visits. Among them 52.1%(N = 298) were females. Nearly 58%(N = 333) were followed up in the government sector. Diabetes(37.6%), hypertension(31.3%), asthma(8.7%), cancer(8.6%), chronic kidney disease (7.9%) were identified as common NCDs among this subsample. Considering a clinic visit, most(N = 521, 91.1%) incurred only direct medical OOPE, while 4.5%(N = 26) had only direct non-medical OOPE. Interestingly, only 4.4%(N = 25) had direct medical and non-medical OOPE. Most patients(N = 391, 68.4%) had a total OOPE of less than 5000 SLR. The average cost for a clinic visit was SLR 3000 (Table 3). Patients had spent a median (IQR) of 750(500) SLR per day for meals while 2000(2300) SLR per day for transport. Interestingly, 6.3% of patients had spent a median(IQR)of 1350(3500) SLR for investigations, and 6.5% of patients had spent a median(IQR)of 1500(5000) SLR for drugs per routine follow-up visits. When considred common NCDs, cancer had highest OOPE(SLR12000 with 5000–16000 IQR)and highest CHE of 34.3% with 13.7% -75.0% IQR followed by chronic kidney disease (CKD) (OOPE, SLR 7000 with 2375 – 9475 IQR & 11.9% CHE with 4.7%—20.9%), asthma (OOPE, SLR 2500 with 1500 – 3500 IQR & 10.0% CHE with 4.7%—15.0%), diabetes (OOPE, SLR 3000 with 1325 – 5000 IQR & 6.9% CHE with 2.5%—12.5%) and HTN (OOPE SLR 2400 with 1000 – 4500 IQR & 5.8% CE with 2.0%—11.0%).
Catastrophic Health expenditure for hospital admissions and follow-up visits
Catastrophic Health expenditure (CHE) for hospital admissions and follow-up visits were calculated by dividing respective total OOPE by average monthly income. CHE was less than 15% for the majority (N = 167, 66.3%) in hospital admissions as well as for follow-up visits (N = 461, 80.6%) (Table 3). District-wise variations were observed in CHE for both hospital admissions and follow-up visits. OOPE was higher in the private sector compared to the government sector for hospital admissions (SLR 4800 vs. 3000). For regular follow-up visits OOPE was higher in the private sector compared to the government sector (SLR 4700 vs. 2000). A statistically significant difference in OOPE was detected among the private and government sectors for regular follow-up visits(p < 0.001).
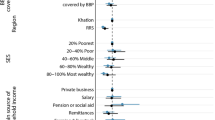
Associated factors for Catastrophic health expenditure for patients with regular clinic visits and hospital admissions
Associated factors for CHE were assessed using binary logistic regression (Enter method), and CHE categorization was done considering 15% as the threshold. Age, sector treated, gender, and income category(SLR 30000 and below, above SLR 30000) were considered independent variables (Table 4). OOPE was not considered an independent variable as it had multicollinearity with monthly income. Factors significantly associated with > 15% CHE for both hospital admissions and regular clinic follw-ups were montly income, presence of complications, and sector treated. The risk for CHE for regular follow-up visits is increased with patients' age, and duration of illness.
Discussion
The present study was conducted among 2344 NCD patients residing in four selected districts in Sri Lanka to represent the urban, rural, semi-urban, and estate sectors. Common NCDs identified were hypertension (29.1%), diabetes (27.0%), hyperlipidemia (9.8%), and asthma (8.2%). Complications associated with NCDs were reported by 13% of the patients. Among the participants, 56% (N = 1304) were on regular clinic follow-up, with the majority (70.2%, N = 916) utilizing government hospitals for Western medical care. Over the past year, 252 hospital admissions for chronic disease management occurred, with the majority (86%) to the government sector hospitals. The average cost for a clinic visit was SLR 3000, while for a hospital admission, it was SLR 3100. Catastrophic health expenditure (CHE) exceeded 40% for 6.1% of hospital admissions and 13.5% of regular clinic follow-ups. Patients admitted to private hospitals faced 2.61 times higher CHE than those admitted to government sector hospitals. To our knowledge, this is the first study in Sri Lanka to comprehensively examine both the disease burden and the economic impact of non-communicable diseases, specifically focusing on the factors that contribute to CHE.
The sector a person lives affects healthcare spending and well-being. The place of residence is correlated with living and working conditions, air and water quality, physical activity, and healthcare access [21]. This cross-sectional study analyzed all activities in managing NCD patients for costing purposes. Cost components were identified and included in a validated interviewer-administered questionnaire, which was pre-tested before use.
NCDs have a long duration and cause complications if left untreated and a major cause of premature death and disability. One of the main goals of Sustainable Development Goals is to “Ensure healthy lives and promote well-being for all at all ages” by 2030. Globally and locally the leading causes of premature deaths are stroke, diabetes, cancer, and respiratory diseases [22] and these were selected for the current study. The study reveals high self-reported NCDs among the participants. We found that the majority had hypertension and diabetes. The high incidence of these NCDs leads to high healthcare costs, limited ability to work through presenteeism, and absenteeism, leading to financial insecurity and slow growth of a country [23]. The curent study provides evidence that NCDs related compications are high among the partipants and alarmingly nearly half of the population are not on regular follw-up.Although NCDs are not curable, with early diagnosis and regular treatment, patinets can live a long life without complications [24]. Public policies and financial protection are crucial to curb NCDs epidemic, along with individual responsibility.
Out-of-pocket payments(OOPE) are defined as any direct payment by households, including payments to health practitioners, pharmaceuticals, therapeutic devices, other goods and services, and informal payments [25]. Chronic conditions often require ongoing medical care, medications, and specialized services, leading to high OOPE. This financial burden can cause CHE, where households are forced to spend a significant portion of their income on healthcare, leading to financial distress and impoverishment. Studies in various settings, including local studies, have emphasized this trend, emphasizing the urgent need for strategies to reduce these economic impacts, especially for vulnerable populations [5, 19, 26]. A substantial proportion of costs in a hospital admissions is for medication, diagnosis, and other non-medical expenditures such as transport, meals, and bystanders. The study shows that private sector hospital admissions cost more. In government hospitals, patients have access to free drugs and laboratory investigations available at the time as part of the public healthcare system. Conversely, in private hospitals, patients are responsible for covering the costs associated with these services. In Sri Lanka only the formal sector employers have social insurance and voluntary health insurance enrollment is low [3]. Hence, private sector healthcare utlization will lead to OOPE. Follow-up costs also depend on finances and the medical facility. Our study confirms a link between income and healthcare expenditure [27]. Another major factor for the tendancy to push people to incure high OOPE leading to CHE when obtaining treatment from a private sector facility could be due to the fact that the private sector aims to maximize profits [27].
The reasons for high OOPE for medications and laboratory investigations could be due to multi morbidity [28] and lack of essential drugs and investigations at the government hospitals leading patients to obtain these at the private sector. The current study shows that patients face significant out-of-pocket expenses and are more likely to experience CHE when suffering from chronic diseases such as cancer, CKD, and asthma. These conditions typically necessitate ongoing, intensive treatment, consisting of frequent healthcare encounters, specialized therapies, and long-term medication. The economic burden of illnesses such as asthma, CKD, and cancer, like other non-communicable diseases, often results in treatment non-compliance, which can lead to disease complications and a diminished quality of life [26]. This may result in a higher occurrence of CHE, with households being compelled to allocate a large portion of their income to healthcare, potentially pushing them into financial hardship or poverty.
Similar to other studies in leterature, current study show that there are sector wise variations of OOPE incurred and in some sectors transport costs were very high [26]. This is despite the avaialabilty of healthcare institutions in close proximity. Patients by-pass smaller institutions to go to larger healthcare institutions for may resons [29]. This study shows that most patients were followed up at government Western healthcare institutions. Patients in Sri Lanka often prefer Western medical care because of its effectiveness, widespread availability, and trust in the system. Healthcare professionals' expertise and formal training reinforce this understanding.Consistent with other studies, OOPE is higher for private hospital admission than public facilities (p < 0.05) [19, 26, 30].
Many disadvantages could occur when health systems rely on OOPE as the predominant revenue source for healthcare; the people may not seek the care they need as treatment-seeking would depend on the ability to pay, or they may suffer severe financial hardship (catastrophic health expenditure) as a result of incurring such payments [2]. The current study showed that considering a hospital admission, 19.4% had bourn > 15% CHE, and considering a clinic follow-up, 33.7% had incurred CHE. In the Sri Lankan setup, people prefer the public sector, which is free of charge, for hospital admission, and the private sector for regular follow-up [27]. Hence the public and private sectors sometimes act as a substitute and sometimes as complimentary to each other. Sri Lankan people often prefer the public sector for hospital admissions due to their faith in the system and the availability of free medical services, including treatments, medications, and diagnostic tests, which significantly reduces their financial burden. However, this decision could vary depending on factors such as affordability, having insurance, type of dweeling/ sector and the type of treatment they need. These differnces have been highlighted in the global literature [19, 31]. If healthcare financing depends on OOPE, its burden would be shifted towards those who use services more, possiblty to low-income earners or people at more risk, where healthcare needs are higher which is shown in the study [21, 32]. This violates fundemnaetals of UHC and is againnst objectives of a health system.If health system does not consit of sound health care financing policies, barriers to quality health care will be created due to high costs and spending. In Sri Lanka, primary health facilities are not well equipped to manage chronic non-communicable diseases (NCDs). The ability for patients to directly obtain tertiary care services without a referral system leads to under-utilization of the primary health care (PHC) facilities and increases the burden at tertiary care levels [33]. Overutilization of tertiary care institutions and underutilization of smaller institutions pose a major threat to the efficiency of the healthcare system. Another issue is that this lack of referral system doesn’t allow comprehensive or continuous care to the patient, which is crucial in NCD care. From a patient’s perspective, continuity of care is necessary to monitor lifestyle risk factors. This places a burden on both the patient and the system [33]. Considering these factors, it is evident that a PHC reform is necessary for Sri Lanka due to changing disease patterns and emerging issues. A well-equipped healthcare facility with trained doctors, essential lab facilities, and a consistent supply of necessary drugs plays a vital role in providing continuous care for chronic illnesses. Additionally, it would significantly alleviates the financial burden on patients. In formulating policies, it is important for policymakers to carefully consider the heterogeneities patient preferences, and the social and commercial determinants of health.
Limitations
This study has limitations. Although the survey was conducted using an IAQ, the data were self-reports; hence there could be information bias. However, the questionnaire was developed and validated prior to use and pre-tested to enhance reliability. Additionally, an interviewer guide was developed, data collectors were trained to minimize inter-observer bias, and the principal investigator was present throughout the data collection process. Finally, selection bias was minimized by adhering to a probability sampling technique in recruiting the respondents and visiting the households twice( if the selected respondent was absent at the time of data collection) before categorizing non-respondents. As is shown in literature the threshold used to define catastrophic payment is arbitrary. We cannot ensure that spending less than this ratio would not lead to CHE, hindering meeting basic needs [19]. In this study, we did not investigate the reasons for people not using healthcare facilities, such as a shortage of doctors, lack of facilities, and the limited ability of smaller clinics to offer services for non-communicable diseases (NCDs). This may be why transportation costs are high. Future studies should explore why people are not using these smaller healthcare facilities more.
Conclusions
The Sri Lankan health sector has achieved impressive health outcomes, but the rising burden of non-communicable diseases such as diabetes and hypertension is concerning. The utilization rate of healthcare services among patients suffering from NCDs is currently comparatively low. Participants in the study showed high proportions of NCDs, leading to significant out-of-pocket expenditures for various reasons. Most sought care in the government sector, yet the direct medical and non-medical costs for NCD care remain high, resulting in catastrophic health expenditures. There were sectoral variances in reasons for incurred OOPE, which should be studied. The presence of heterogeneities of reasons carries important policy implications, and policymakers should consider these factors in addressing this matter. As a lower-middle-income country, Sri Lanka faces challenges in ensuring Universal Health Coverage (UHC) due to limited financial resources. Policymakers must explore financial options like cost-sharing and service delivery reorganization to improve efficiency, equity, and access while protecting patients from high OOPE. Further studies are needed to understand the determinants of multimorbidity and the demand for private-sector care despite a universal public health system.
Abbreviations
- BMI:
-
Body mass index
- NCDs:
-
Non-communicable diseases
- OOPE:
-
Out of Pocket Expenditure
- CHE:
-
Catastrophic health expenditure
- WHO:
-
World Health Organization
- UHC:
-
Universal Health Coverage
References
Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. 2014;11(9): e1001701.
Kutzin J, Yip W, Cashin C. Alternative Financing Strategies for Universal Health Coverage. World Scientific Handbook of Global Health Economics and Public Policy. World Scientific Series in Global Health Economics and Public Policy: WORLD SCIENTIFIC; 2016. p. 267–309.
Rajapaksa L, De Silva P, Abeykoon P, Somatunga L, Sathasivam S, Perera S, Fernando E, De Silva D, Perera A, Perera U, et al. Sri Lanka Health System Review. In.: World Health Organization; 2021.
Global Health Expenditure Database, 2000–2020 [https://apps.who.int/nha/database].
Kumara AS, Samaratunge R. Patterns and determinants of out-of-pocket health care expenditure in Sri Lanka: evidence from household surveys. Health Policy Plan. 2016;31(8):970–83.
Gamage A, Dias T, Amarasiri M, Karunathilake I. The impact of the economic crisis on the Sri Lankan health financing. 2022.
Talking Econmics Sri Lanka’s Health Financing Challenge: Why Smarter Spending is Key. In. Edited by IPS. Colombo Sri Lanka: Institute of policy studies Sri Lanka; 2021.
Gamage AU. Seneviratne RdA: Physical inactivity, and its association with hypertension among employees in the district of Colombo. BMC Public Health. 2021;21(1):2186.
Tackling Non-Communicable Diseases in Sri Lanka [https://www.worldbank.org/en/news/feature/2012/05/16/non-communicable-diseases-sri-lanka].
Sum G, Hone T, Atun R, Millett C, Suhrcke M, Mahal A. Koh GC-H, Lee JT: Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ Glob Health. 2018;3(1):e000505.
Gamage SCA AU, Undurraga E, Fabrizio C, Sridharan S. Determinants of out-of-pocket health care expenditure in Sri Lanka: From Diagnosis to Reforms Journal of College of Community Physicians of Sri Lanka. 2019.
Department of Census and Statistics C. Household Income and Expenditure Survey 2016. In: Edited by Statsitics DoCa. Colombo Dept. of Census and Statsitics. 2016.
Azzani M, Roslani AC, Su TT. Determinants of household catastrophic health expenditure: a systematic review. The Malaysian journal of medical sciences: MJMS. 2019;26(1):15.
Weerarathne Bilesha. Re-Defining Urban Areas in Sri Lanka. In: Working paper seiris 23 Edited by INSTITUTE OF POLICY STUDIES OF SRI LANKA: INSTITUTE OF POLICY STUDIES OF SRI LANKA. 2016.
Gnanapragasam S. A MULTIVARIATE APPROACH TO CLASSIFY THE DISTRICTS OF SRI LANKA BASED ON THE COST OF LIVING. International Journal of Information Research and Review. 2017;4:4128–32.
Engstrom R, Newhouse D, Soundararajan V. Estimating small-area population density in Sri Lanka using surveys and Geo-spatial data. PLoS ONE. 2020;15: e0237063.
McBurney P. On Transferring Statistical Techniques Across Cultures: The Kish Grid. Curr Anthropol. 1988;29(2):323–5.
Rashidian A, Akbari Sari A, Hoseini SM, Soofi M, Ameri H. Comparison of the Thresholds of Households’ Exposure to Catastrophic Health Expenditure in Iran and Brazil, and Selection of the Most Appropriate Threshold. Iran J Public Health. 2018;47(12):1945–52.
Verma VR, Kumar P, Dash U. Assessing the household economic burden of non-communicable diseases in India: evidence from repeated cross-sectional surveys. BMC Public Health. 2021;21(1):881.
Wagstaff A. Doorslaer Ev: Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993–1998. Health Econ. 2003;12(11):921–33.
WHO: The World Health Report. Health Systems Financing: the Path to Universal Coverage. In: Edited by WHO. 2010.
Indoor Mortality and Morbidity Report 2019 [vailable from: https://data.health.gov.lk/dataset/indoor-mortality-and-morbidity-report-2019].
Nagata T, Mori K, Ohtani M, Nagata M, Kajiki S, Fujino Y, Matsuda S, Loeppke R. Total Health-Related Costs Due to Absenteeism, Presenteeism, and Medical and Pharmaceutical Expenses in Japanese Employers. J Occup Environ Med. 2018;60(5):e273–80.
Luna F, Luyckx VA. Why have Non-communicable Diseases been Left Behind? Asian Bioeth Rev. 2020;12(1):5–25.
Jalali FS, Bikineh P, Delavari S. Strategies for reducing out of pocket payments in the health system: a scoping review. Cost Eff Resour Alloc. 2021;19(1):47.
Menon GR, Yadav J, John D. Burden of non-communicable diseases and its associated economic costs in India. Social Sciences & Humanities Open. 2022;5(1): 100256.
Pallegedara A, Grimm M. Demand for private healthcare in a universal public healthcare system: empirical evidence from Sri Lanka. Health Policy Plan. 2017;32(9):1267–84.
Sum G, Hone T, Atun R, Millett C, Suhrcke M, Mahal A, Koh GC, Lee JT. Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ Glob Health. 2018;3(1):e000505.
Karunaratne NP, Kumara GSP, Karunathilake KTGS, Karunathilake GVKM, Kaushalya PGM, Kavinda HWI, Keshala AAM, Ponnamperuma T. Bypassing primary healthcare institutions: Reasons identified by patients’ attending the out-patient department. J Ruhunu Clin Soc. 2019;24(1):16–22.
Khalid F, Raza W, Hotchkiss DR, Soelaeman RH. Health services utilization and out-of-pocket (OOP) expenditures in public and private facilities in Pakistan: an empirical analysis of the 2013–14 OOP health expenditure survey. BMC Health Serv Res. 2021;21(1):178.
Pandey A, Kumar GA, Dandona R, Dandona L. Variations in catastrophic health expenditure across the states of India: 2004 to 2014. PLoS ONE. 2018;13(10): e0205510.
Hanson K, Brikci N, Erlangga D, Alebachew A, De Allegri M, Balabanova D, Blecher M, Cashin C, Esperato A, Hipgrave D, et al. The <em>Lancet Global Health</em> Commission on financing primary health care: putting people at the centre. Lancet Glob Health. 2022;10(5):e715–72.
Rannan-Eliya Ravi P, Elwalagedara Ruwanthi, Abeykoon AB ATPL, Dalpatadu Shanti, Balasundaram Ahalya, Dalpatadu Shanti, Anuranga Chamara, Brearley Lara. An Assessment of the Burden, Issues and Policy Options in Curative Care Services Delivery and Non-communicable Diseases in Sri Lanka. 2010.
Acknowledgements
Funding for this study was provided by the World Bank Primary Health Care System Strengthening Project for Sri Lanka. The funding agency had no role in the design, analysis, or interpretation of data, writing of the report, or the decision to submit the article for publication. The authors were entirely independent of the funding agency in conducting the research.The authors gratefully acknowledge the time and effort given by all the participants to make this study a success.
Data Sharing
The raw data that supported the finding of this study are available from corresponding author, AG, upon a reasonable request. The derived data which was generated in this study and other supplementary study materials, such as study instruments and informed consent form, are publicly available within this article from the date of publication.
Funding
Funding for this research was through World Bank Primary Healthcare Strengthening Project—Small Grants ( PSSP/ SG/ 2019/ 05).
Author information
Authors and Affiliations
Contributions
AG and SS conceived, designed, and managed the study. AG, ND and TG contributed to management of data AG and ND, performed statistical analysis and drafted the manuscript, and AG, ND, TG DA and SS contributed to revising the manuscript’s intellectual content. All authors have access to the data analysed in the study and take responsibility for the integrity of the data and the accuracy of the analysis. All authors read and approved the final version of the manuscript and have agreed to authorship and order of authorship.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed written consent was obtained from all the patients. Ethical clearance for the study was obtained (RP/2020/11) from the Ethical Review Committee of the Faculty of Medicine, General Sir John Kotelawala Defence University, Sri Lanka.
Consent for publication
Not applicable.
Competing interests
The funding agency had no role in the design, analysis, or interpretation of data; writing of the report; or the decision to submit the article for publication. The authors were fully independent of the funding agency in conducting the research. The authors declare that they have no conflicts of interest. All authors have access to the data analyzed in the study and take responsibility for the integrity of the data and accuracy of the analysis.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gamage, A., Darshana, N., Gunasekara, T. et al. Variations in out-of-pocket spending and factors influencing catastrophic health expenditure of households with patients suffering from chronic conditions in four districts in Sri Lanka. BMC Health Serv Res 24, 1055 (2024). https://doi.org/10.1186/s12913-024-11553-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11553-4