Abstract
Background
Gastric cancer is the fourth most common cancer and highly prevalent in South Korea. As one of the predictors of gastric cancer, we focused on health utilization patterns and expenditures, as the surrogate variables of health conditions. This nested case-control study aimed to identify the association between health expenditure trajectory and incidence of gastric cancer.
Methods
Data from the National Health Insurance Service Senior Cohort of South Korea were used. Individuals diagnosed with gastric cancer (N = 14,873) were matched to a non-diagnosed group (N = 44,619) in a 1:3 ratio using a nested case-control design. A latent class trajectory analysis was performed to identify the patterns of health expenditure among the matched participants. Furthermore, conditional logistic regression analysis was conducted to examine the relationship between healthcare expenditure trajectories and gastric cancer incidence.
Results
Seven distinct health expenditure trajectories for five years were identified; consistently lowest (13.8%), rapidly increasing (5.9%), gradually increasing (13.8%), consistently second-highest (21.4%), middle-low (18.8%), gradually decreasing (13.1%), and consistently highest (13.2%). Compared to the middle-low group, individuals in the rapidly increasing [odds ratio (OR) = 2.11, 95% confidence interval (CI); 1.94–2.30], consistently lowest (OR = 1.40, 95% CI; 1.30–1.51), and gradually increasing (OR = 1.26, 95% CI; 1.17–1.35) groups exhibited a higher risk of developing gastric cancer.
Conclusions
Our findings suggest that health expenditure trajectories are predictors of gastric cancer. Potential risk groups can be identified by monitoring health expenditures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Gastric cancer is highly prevalent worldwide [1], with South Korea reporting the highest number of incidences [2, 3]. In 2020, gastric cancer was ranked as the fourth most common cancer in South Korea, after thyroid, lung, and colorectal cancers [2]. Data from the Korean Statistical Information Service (KOSIS) revealed that gastric cancer accounted for approximately 10.8% of all cancers in South Korea, ranking second in incidence among men, with an age-standardized incidence rate of 76.2 per 100,000 individuals [2]. This rate was twice as high in men than in women (31.6%). Despite a gradual decline in the incidence rate of gastric cancer between 2010 and 2020, South Korea still has the highest incidence rate of gastric cancer among mens compared to 185 other countries [2, 3].
The increasing prevalence of cancer imposes a substantial economic burden on patients, families, health systems, and society as a whole [4,5,6]. A previous study conducted in 2014 on the economic burden of gastric cancer in patients reported a total cost of US $557,571 considering both direct and indirect expenses [7]. Other studies on cancer treatments have shown that the cost of cancer treatment is higher owing to repeated hospitalizations, numerous outpatient visits, laboratory services, advanced diagnostic tests, chemotherapy, expensive medications, surgeries, and radiotherapy, among other essential services [8, 9]. Consequently, there is a growing demand for more proactive approaches to effectively treat cancer with fewer side effects, highlighting the significance of accurate and rapid gastric cancer screening [10, 11].
Gastric cancer is a multifactorial disease influenced by various demographic characteristics, diet, lifestyle, genetic predisposition, family history, medical conditions, and infections [12, 13]. Age, sex, socioeconomic status, smoking status, diet, obesity, physical activity, and Helicobacter pylori infection have been associated with gastric cancer. Smoking status, high salt intake, and H. pylori infection are considered modifiable factors [12,13,14,15,16,17,18,19]. Although upper gastrointestinal endoscopy is necessary to assess the risk of gastric cancer, it has potential risks and entails high screening costs [11, 20]. For example, one study found that individuals who underwent gastrointestinal endoscopy reported a 0.13% adverse complication rate and a 0.004% mortality rate [21]. Therefore, gastrointestinal endoscopy has been proposed for high-risk subgroups [22].
In 1999, South Korea implemented a national screening program for gastric cancer, which recommends biennial upper endoscopy or upper gastrointestinal series for individuals aged ≥ 40 years [23]. The “high-risk group” is defined based on age (≥ 40 years), family history of gastric cancer, a previous diagnosis of precancerous conditions, such as atrophic gastritis and intestinal metaplasia, Helicobacter pylori (H. pylori) infection, and chronic conditions, such as pernicious anemia and gastric ulcers.
The observed decrease in the incidence of gastric cancer in South Korea between 2010 and 2020 can be attributed to several factors. For instance, the widespread implementation of a national endoscopic screening program [23], which has led to the early detection and treatment of precancerous lesions. Additionally, efforts to eradicate H. pylori [24], a known risk factor for gastric cancer, have contributed to this decline. Widespread H. pylori screening and eradication programs have been in place in South Korea since the early 2000s. Studies have shown that H. pylori eradication can reduce the risk of gastric cancer by approximately 50%. Other factors that may have influenced this trend include improvements in lifestyle and dietary habits [25], and enhanced sanitation and living conditions [26].
Several studies have primarily focused on health expenditures related to end-of-life care and those incurred after a cancer diagnosis [27,28,29]. However, these studies have mainly focused on the financial burden on patients, families, health systems, and society following cancer occurrence. Given the availability of accurate and rapid screening methods for gastric cancer, such as gastrointestinal endoscopy [30], the most effective strategy is to develop a prediction model that can identify high-risk subgroups by analyzing the patterns prior to the onset of gastric cancer.
This study focused on health expenditure patterns. Using Andersen’s behavioral model of health services utilization, health utilization, and expenditures were determined based on predisposing, enabling, and need factors [31]. Although personal preferences and other predisposing and enabling factors may over- or underestimate health expenditure, previous research has shown that health expenditure is associated with health conditions [32,33,34]. Previous research has also examined the association between health expenditures and cancer incidence and found that higher health expenditures are associated with increased cancer incidence [35]. However, this approach may overlook the patterns of longitudinal health expenditure changes before the onset of gastric cancer. Because the gastrointestinal carcinogenic process typically spans 5–15 years [36], it is imperative to examine the potential impact of longitudinal health expenditure patterns. Whereas a single event can lead to a sudden surge in health expenditures in a particular year, it may not be indicative of the patterns associated with gastric cancer incidence. This underscores the importance of examining health expenditure patterns over time before gastric cancer occurrence. This study utilized data from the National Health Insurance Service (NHIS) Senior Cohort in South Korea and identified specific health expenditure trajectories preceding the onset of gastric cancer, and examined the associations of these trajectories with gastric cancer incidence using a nested case-control study design to address this gap.
Methods
Data and study population
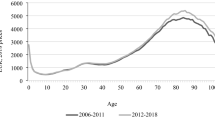
This study used data from the NHIS Senior Cohort of South Korea. The NHIS covers approximately 97% of all Korean citizens and the remaining 3% are covered by Medical Aid [37]. Consequently, the NHIS collects data on the use of medical services by all citizens and stores them anonymously. The NHIS senior cohort data comprised a randomly selected sample stratified based on various criteria, such as sex, age, and insurance premium quantile, representing approximately 8% of South Korean individuals aged ≥ 60 years in 2008 (approximately 510,000 individuals). Moreover, since 2009, the NHIS senior cohort has added 8% older adults who turn 60 each year, resulting in approximately 540,000 older adults between 2009 and 2019. Overall, approximately 1,057,784 older adults participated in the cohort study between 2002 and 2019 [38]. The dataset included information on each individual’s health status, healthcare utilization, and sociodemographic characteristics such as sex, age, and region of residence [38].
This study used data from 2008 to 2019 and included 761,917 individuals aged 60 years or older at baseline between 2008 and 2014. Study participants with a history of cancer (N = 94,260), those on Medical Aid (N = 33,697), and those who died from non-incident gastric cancer during the study period (N = 132,342) were excluded. After excluding 442,126 participants who did not meet the inclusion criteria, 59,492 were included in the analysis (Fig. 1).
Variables
Outcome measure
The primary outcome measure in this study was gastric cancer incidence. Gastric cancer was classified based on the principal diagnosis between 2008 and 2019, using the International Statistical Classification of Diseases, 10th revision (ICD-10; code C16).
Independent variables
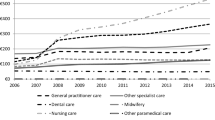
The independent variable used in this study was health expenditure. Health expenditures included all expenses related to medical services incurred before the diagnosis of gastric cancer. This included outpatient and inpatient medical services, except for oriental medicine, dental services, and out-of-hospital prescriptions To account for the annually increasing inflation, health expenditures were calculated using a conversion index applied to health expense calculations [39]. In South Korea, the annual rate of increase is determined by negotiations between the NHIS and provider associations [39]. All health expenditures at different timepoints were calculated using an annual conversion index based on the last data point of the study (2019). The annual conversion index rates used to calculate health expenditures are presented in Supplementary Table 1. Individual health expenditures from 1 to 5 years prior to the diagnosis of gastric cancer were aggregated in units of six months and divided into 20 groups according to the percentiles (Supplementary Table 2). For participants with no incidence of gastric cancer, health expenditures were calculated based on the date of diagnosis of the matched patient with gastric cancer. Seven health expenditure trajectories were identified based on the health expenditure patterns of the segmented health expenditure groups 1–5 years gastric cancer diagnosis. The seven types of health expenditure trajectories over 5 years were categorized based on the following patterns: “consistently lowest,” “rapidly increasing,” “gradually increasing,” “consistently second-highest,” “middle-low,” “gradually decreasing,” and “consistently highest’’ (Fig. 2).
Covariates
The covariates included sociodemographic factors, underlying health conditions, health behaviors, and pre-existing conditions. Sociodemographic factors included sex (men, women), age (60–64, 65–69, 70–74, 75–79, and > 80 years), income (quartile), and region of residence (Seoul, Gyeonggi, metropolitan, rural). Underlying health conditions included disability and the Charlson comorbidity index (CCI). Disability was categorized as non-disabled and registered under Korea’s Disability Registration system [40]. The CCI was calculated according to Quan’s updated criteria and categorized as 0, 1, 2, > 3 [41]. Sociodemographic factors and underlying health conditions were assessed at baseline. Health behaviors included smoking status (no answer (N/A), never, former, current) and alcohol consumption status (N/A, no, yes). Preexisting conditions included eight symptoms associated with gastric cancer, which were identified based on the Korean Standard Classification of Symptoms (KCD). These symptoms included abnormal weight loss (R10.49), dysphagia (R13), dyspepsia/gastro-esophageal reflux disease (K21, K30), hematemesis/melaena (K92.1), H. pylori infection (B98,0), diabetes mellitus (E10-E14), and pneumonia (J12-J18) [42,43,44,45,46,47,48]. The presence of these symptoms was confirmed from baseline until cancer diagnosis.
Statistical analysis
The study was conducted in four steps. First, the gastric cancer diagnosed (cases) and non-diagnosed (controls) groups were matched in a 1:3 ratio according to the nested case-control (NCC) method, which involved the selection of participants (controls) with similar characteristics upon the event incidence [49]. Matching was performed according to sex, age, and income level upon gastric cancer diagnosis. The study design is shown in Supplementary Fig. 1. Second, a latent class trajectory model (LCTM) analysis was conducted to identify health expenditure patterns among the matched participants. LCTM is an analytical method that clusters latent classes based on changes in the dependent variable over time and is suitable for categorical variables [50, 51]. The number of clusters in the latent class was determined by the goodness of fit and pattern proportion of the model. For model fit, we considered the lowest value based on the Akaike information criterion (AIC) and Bayesian information criterion (BIC). At the same time, we examined whether any cluster group had a proportion of < 5%. Third, conditional logistic regression was performed for matched data analysis to investigate the relationship between healthcare expenditure trajectories and gastric cancer incidence. Fourth, a sensitivity analysis was conducted to enhance the robustness of the study’s results. The sensitivity analysis comprised two parts: (a) interesting variable change and (b) subgroup analysis. For the interesting variable change, the data was analyzed by dividing the health expenditures one year before gastric cancer diagnosis, five years before diagnosis, and the average health expenditures from one to five years into quintiles. In the subgroup analysis, participants were categorized into below-median and above-median income groups. The statistical significance of the regression analysis was determined using a 95% confidence interval (CI) of the odds ratio (OR), where a lower bound > 1 was considered significant. All analyses were performed in 2023 using SAS (version 9.4, SAS Institute, Cary, NC, USA) and R (version 3.3.1, R Foundation for Statistical Computing).
Results
LCTM analysis was performed to identify the health expenditure trajectory before the incidence of gastric cancer. The LCTM analysis confirmed the model fit and proportion of each pattern (Table 1). Although class 8 showed the best model fit, its proportion was < 5%. Therefore, class 7, which satisfied both the model fit and proportion criteria, was determined as the final model.
Table 2 shows the general characteristics of the study sample. A total of 59,492 older Korean individuals (14,873 cases and 44,619 controls) were included in this study. The study sample displayed the following general characteristics; most had high health expenditure (54.3%), were men (68.4%), were under 65 years of age (42.2%), belonged to the highest income group (31.8%), resided in rural areas (36.9%), were non-disabled (88.3%), had a CCI score of 0 (63.1%), had never smoked (51.2%), and did not drink alcohol (55.6%). Additionally, 49.9% of the older adults had diabetes mellitus, 18.7% had pneumonia, and 83.3% experienced dyspepsia/gastro-esophageal reflux disease. Other pre-existing conditions were reported by < 5% of the study participants.
The frequency of gastric cancer incidence for each variable is presented in Table 2. Based on the type of health expenditure trajectory, the incidence of gastric cancer was noted in the following order: rapidly increasing (N = 1,251; 35.5%), consistently highest (N = 2,341; 29.8%), gradually increasing (N = 2,264; 27.6%), and consistently second-highest (N = 3,339; 26.2%). The incidence of gastric cancer was higher in groups with consistently higher or increasing health expenditure before the incidence of gastric cancer than in other groups (p < 0.001). With regard to sex, age, and income, the diagnosed and non-diagnosed gastric cancer groups were matched at a ratio of 1:3 using the NCC method. In addition, the incidence of gastric cancer was higher in rural areas (p < 0.001), among those with disabilities (p < 0.001), those with a higher CCI score (p < 0.001), and those who currently smoked (p < 0.001). Furthermore, individuals with pre-existing conditions had a higher incidence of gastric cancer than those without (p < 0.001).
We performed a conditional logistic regression analysis to investigate the association between health expenditure trajectory type and gastric cancer incidence (Table 3). The results indicated that compared to the middle-low group, individuals in the consistently lowest group had an increased OR of 1.40 (95% CI; 1.30–1.51), whereas those in the rapidly increasing and gradually increasing groups had ORs of 2.11 (95% CI; 1.94–2.30) and 1.26 (95% CI; 1.17–1.35), respectively. However, the consistently second highest, gradually decreasing, and consistently highest groups showed no significant difference. Furthermore, we found that certain regions had higher ORs for gastric cancer incidence, with metropolitan and rural areas showing ORs of 1.09 (95% CI; 1.03–1.16) and 1.24 (95% CI; 1.18–1.31), respectively, compared to Seoul. Additionally, the presence of a disability, higher CCI score, former or current smoker status, and pre-existing conditions were associated with a higher OR for gastric cancer incidence. Particularly, pre-existing conditions had higher ORs for gastric cancer incidence; abnormal weight loss (OR = 1.42, 95% CI; 1.21–1.68), dysphagia (OR = 2.04, 95% CI; 1.76–2.36), dyspepsia/gastro-esophageal reflux disease (OR = 2.53, 95% CI; 2.36–2.70), hematemesis (OR = 5.16, 95% CI; 3.91–6.80), melena (OR = 5.13, 95% CI; 4.66–5.65), H. pylori infection (OR = 3.28, 95% CI; 2.90–3.71), diabetes mellitus (OR = 1.38, 95% CI; 1.33–1.44), and pneumonia (OR = 1.30, 95% CI; 1.24–1.37), compared to that in individuals without pre-existing conditions.
The results of the sensitivity analysis are presented in Table 4. In the analysis of interesting variable change, participants were divided into groups based on their health expenditure one year and five years before gastric cancer diagnosis. For the one-year health expenditure group analysis, compared to the middle group, individuals in the lowest group had increased ORs of 1.42 (95% CI; 1.33–1.51), while those in the middle-low groups had ORs of 1.11 (95% CI; 1.04–1.18). In the analysis of the five-year health expenditure group, compared to the middle group, individuals in the lowest group had increased ORs of 1.10 (95% CI; 1.04–1.17), whereas those in the highest groups had ORs of 1.44 (95% CI; 1.35–1.53). In the analysis of the one–five-year average health expenditure group, compared to the middle group, individuals in the lowest group had increased ORs of 1.15 (95% CI; 1.07–1.23), while those in the highest groups had ORs of 1.22 (95% CI; 1.15–1.30). For each subgroup, health expenditure trajectory groups were determined based on health expenditures from one to five years before gastric cancer diagnosis. The classification of health expenditure trajectory groups was based on criteria such as AIC, BIC, and ensuring that no cluster group had a proportion of less than 5% (Supplementary Tables 3 and Supplementary Fig. 2). In the conditional logistic analysis of the below-median income group, compared to the middle-low group, individuals in the consistently lowest group had increased ORs of 1.38 (95% CI; 1.23–1.53), while those in the rapidly and gradually increasing groups had ORs of 2.06 (95% CI; 1.82–2.34) and 1.18 (95% CI, 1.06–1.31), respectively. For the conditional logistic analysis of the above-median income group, the results showed that individuals in the consistently lowest income group had increased ORs of 1.30 (95% CI; 1.16–1.45) compared to the middle-low group. Additionally, those in the rapidly and gradually increasing groups had ORs of 2.18 (95% CI; 1.92–2.47) and 1.31 (95% CI, 1.19–1.45), respectively. The gradually increasing group had an OR of 1.15 (95% CI; 1.03–1.28).
Discussion
To the best of our knowledge, this is the first study to predict an association between health expenditure trajectories and the incidence of gastric cancer. In South Korea, there is only one mandatory social health insurance [52], so it is a good environment to conduct research on health expenditure and health utilization. The primary objectives of this study were to identify specific health expenditure trajectories preceding the onset of gastric cancer and to examine the associations between these trajectories and gastric cancer incidence using an NCC study design. The findings revealed that individuals in the rapidly increasing (OR = 2.11, 95% CI; 1.94–2.30), consistently lowest (OR = 1.40, 95% CI; 1.30–1.51), and gradually increasing (OR = 1.26, 95% CI; 1.17–1.35) groups had a higher risk of developing gastric cancer.
The sensitivity analysis results confirmed the short and long-term association between gastric cancer diagnosis and average health expenditures before diagnosis. The result of the lowest group was the same as that of the consistently lowest trajectory group. The highest group in five-year average health expenditure was significant because some increasing trajectory groups were included in the highest group. This indicates that the increasing trajectories were not able to be captured in the sensitivity analysis from the traditional perspective. It demonstrated the importance of considering the trajectory context. Furthermore, subgroup analyses based on median income levels also demonstrated that consistently low or increasing health expenditures before gastric cancer diagnosis were significantly associated with the diagnosis of gastric cancer. In the health equity and accessibility perspectives, the health expenditures can differ from the income group, but the sensitivity results showed the robustness of our hypothesis. These results provide valuable information for identifying high-risk patients most likely to benefit from gastrointestinal endoscopy.
Health expenditure represents the utilization of healthcare services to meet health demands, categorized as need-based, unnecessary, avoidable, or supplier-induced demands [53]. This study’s results demonstrated various combinations of demand aspects. The consistently highest group may reflect need-based utilization or overuse (such as unnecessary or supplier-induced demands) [54]. The consistently lowest group represents health conditions or the underused and unmet needs that may be attributed to awareness, choice, or access [55]. Both overuse and underuse can be detrimental to patients [54, 56], but underuse can lead to serious health problems, including increased cancer incidence. Thus, the consistently lowest group presents a higher risk than the consistently highest group. The rapidly and gradually increasing groups also showed a high risk of developing gastric cancer. These increasing trends indicate a change that can be attributed to needs-based utilization. Initially, it may involve unnecessary or supplier-induced demands; however, owing to its association with cancer incidence, it ultimately becomes need-based and avoidable.
Gastric cancer prediction models are understudied regarding their ability to identify high-risk populations that can benefit from gastrointestinal endoscopy. Although a few studies have been conducted to predict cancer incidence using claims data, most have overlooked health expenditure patterns. For example, Yeh et al. utilized epidemiological factors, clinical history, and the results of clinical examinations (blood tests, genetic analysis, and imaging results) to predict lung cancer incidence [57]. Similarly, Taninaga et al. used longitudinal medical check-up data (biological characteristics, H. pylori infection status, endoscopic findings, and blood test results) to predict gastric cancer incidence [11]. Our findings suggest that monitoring health expenditure can serve as an indicator for identifying specific risk groups that can be targeted with interventions. However, further research is required to thoroughly explore and validate the predictive potential of health expenditure patterns for gastric cancer.
The incidence of gastric cancer was higher in rural areas and among individuals with disabilities than in other areas and among those without disabilities, which is consistent with the results of previous studies [58, 59]. Song et al. reported that rural areas have a relatively higher incidence of gastric cancer compared with urban areas [58]. They also found a high incidence of gastric cancer in coastal cities and southern provinces, possibly because of higher consumption of highly salted seafood. Evidence suggests that high salt intake may directly stimulate the gastric mucosa or have a synergistic effect with H. pylori infection, leading to gastric cancer. Similar to our findings, Kim et al. (2020) reported that individuals with disabilities tend to be diagnosed at a later stage, particularly those with severe disabilities [60]. Individuals with disabilities are diagnosed with gastric cancer at a later stage, receive inadequate treatment, and have a higher risk of mortality than those without disabilities [59, 60]. Previous research has shown that individuals with disabilities fall within the national free cancer-screening service policy in South Korea [61]. Although this study focused on the incidence of gastric cancer, disability status appeared to be related to the entire cancer control continuum.
This study found that participants with pre-existing conditions and higher CCI scores had a greater incidence of gastric cancer, which is consistent with previous studies indicating that participants with comorbidities or pre-existing conditions have a greater risk of cancer incidence [62, 63]. Hoang et al. (2020) examined the association between comorbidity risk score strata and cancer incidence and observed a dose-dependent relationship between them [63]. In a large population-based prospective study of 405,878 Taiwanese participants, Tu et al. (2018) found a significantly increased risk of incident cancer for eight diseases and markers individually, with adjusted hazard ratios ranging from 1.07 to 1.44 [62]. Although many studies have investigated the effect of comorbidity scores on overall cancer incidence, to the best of our knowledge, this study is the first to examine the association between CCI scores and gastric cancer incidence in South Korea.
Despite its significance, this study had several limitations that should be acknowledged when interpreting the findings. First, although LCTM offers the advantage of grouping by patterns of change in health expenditure over time, a major limitation is the inability to account for factors that influence these patterns. Therefore, future studies should consider a methodology that accounts for the factors affecting the change patterns. Second, there is a possibility of a mismatch between the recorded diagnostic codes and the actual hospital diagnoses. However, it is important to note that a policy has been implemented since September 2005 in South Korea to reduce the copayment for cancer patients, resulting in a 5% decrease in out-of-pocket expenditure [60]. Therefore, all cancer patients are assigned special incidence codes when they receive healthcare services, minimizing the likelihood of code mismatches. Hence, we believe that the code mismatch rate is low. Third, we could not include information related to health status or screening history owing to the characteristics of the claims data. We incorporated the CCI score as a variable reflecting the patient’s underlying health status to compensate for this limitation. Although this design was useful for investigating the associations in a population sample, it has limitations regarding its broader applicability. Since the categorization of health expenditure is data-driven, it is important to recognize that our classifications may not fully capture the health expenditure patterns of the general population. To address concerns regarding generalizability, we conducted sensitivity analyses comparing the characteristics of our nested case-control sample with the overall cohort and general population data.
Conclusion
This study suggests that individuals in the rapidly increasing, consistently lowest, and gradually increasing groups had a higher risk of developing gastric cancer. Health expenditure patterns can help identify high-risk populations; therefore, monitoring these trajectories is important.
This results can be used to guide the high-risk populations to take cancer screenings based on the analysis of health utilization records by NHIS. Alternatively, individuals can assess their cancer risk and take secondary preventive action by using the My Data platform, which allows them to download their health utilization records, including health expenditures in Korea [64].
Data availability
Data for this study are public secondary data, and they can be accessed through the following NHIS website by submitting an application form and paying a fee: https://nhiss.nhis.or.kr/bd/ab/bdaba000eng.do.
Abbreviations
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- ICD-10:
-
International Statistical Classification of Diseases, 10th revision
- KCD:
-
Korean Standard Classification of Symptoms
- KOSIS:
-
Korean Statistical Information Service
- LCTM:
-
Latent class trajectory model
- NHIS:
-
National Health Insurance Service
- NCC:
-
Nested case-control
- OR:
-
Odds ratio
References
Balakrishnan M, George R, Sharma A, et al. Changing trends in stomach cancer throughout the world. Curr Gastroenterol Rep. 2017;19:1–10. https://doi.org/10.1007/s11894-017-0575-8.
Korean Statistical Information Service (KOSIS). Cancer incident cases and incidence rates by site(24 items) and sex. 2023. https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117N_A00022&vw_cd=MT_ETITLE&list_id=F_35&scrId=&language=en&seqNo=⟨_mode=en&obj_var_id=&itm_id=&conn_path=MT_ETITLE&path=%252Feng%252FstatisticsList%252FstatisticsListIndex.do.
Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, Matsuda T, et al. The current and future incidence and mortality of gastric cancer in 185 countries, 2020–40: a population-based modelling study. EClinicalMedicine. 2022;47. https://doi.org/10.1016/j.eclinm.2022.101404.
Piroozi B, Zarei B, Ghaderi B, Safari H, Moradi G, Rezaei S, et al. Catastrophic health expenditure and its determinants in households with gastrointestinal cancer patients: evidence from new health system reform in Iran. Int J Hum Rights Healthc. 2019;12(4):249–57. https://doi.org/10.1108/IJHRH-01-2019-0008.
Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14(12):1165–74. https://doi.org/10.1016/S1470-2045(13)70442-X.
Rahmani H, Asiabar AS, Niakan S, Hashemi SY, Faramarzi A, Manuchehri S, et al. Burden of esophageal cancer in Iran during 1995–2015: review of findings from the Global Burden of Disease studies. Med J Islam Repub Iran. 2018;32:55. https://doi.org/10.14196/mjiri.32.55.
Nguyen TXT, Han M, Oh J-K. The economic burden of cancers attributable to smoking in Korea, 2014. Tob Induc Dis. 2019;17. https://doi.org/10.18332/tid/102673.
Barr RD, Feeny D, Furlong W. Economic evaluation of treatments for cancer in childhood. Eur J Cancer. 2004;40(9):1335–45. https://doi.org/10.1016/j.ejca.2004.01.033.
Doshmangir L, Hasanpoor E, Abou Jaoude GJ, Eshtiagh B, Haghparast-Bidgoli H. Incidence of catastrophic health expenditure and its determinants in cancer patients: a systematic review and meta-analysis. Appl Health Econ Health Policy. 2021;19:839–55. https://doi.org/10.1007/s40258-021-00672-2.
Fitzgerald RC, Antoniou AC, Fruk L, Rosenfeld N. The future of early cancer detection. Nat Med. 2022;28(4):666–77. https://doi.org/10.1038/s41591-022-01746-x.
Taninaga J, Nishiyama Y, Fujibayashi K, Gunji T, Sasabe N, Iijima K, et al. Prediction of future gastric cancer risk using a machine learning algorithm and comprehensive medical check-up data: a case-control study. Sci Rep. 2019;9(1):12384. https://doi.org/10.1038/s41598-019-48769-y.
Cancer IAfRo. IARC monographs on the evaluation of carcinogenic risks to humans. Polychlorinated dibenzo-para-dioxins and polychlorinated dibenzofurans. 1997.
Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev. 2014;23(5):700–13. https://doi.org/10.1158/1055-9965.EPI-13-1057.
Kamangar F. Socio-economic health inequalities: ever-lasting facts or amenable to change? Int J Prev Med. 2013;4(6):621.
Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999;896(1):3–15. https://doi.org/10.1111/j.1749-6632.1999.tb08101.x.
Wiseman M. The second world cancer research fund/american institute for cancer research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: nutrition society and BAPEN Medical Symposium on ‘nutrition support in cancer therapy’. Proc Nutr Soc. 2008;67(3):253–6. https://doi.org/10.1017/S002966510800712X.
Tsugane S, Sasazuki S, Kobayashi M, Sasaki S. Salt and salted food intake and subsequent risk of gastric cancer among middle-aged Japanese men and women. Br J Cancer. 2004;90(1):128–x34. https://doi.org/10.1038/sj.bjc.6601511.
Singh S, Varayil JE, Devanna S, Murad MH, Iyer PG. Physical activity is associated with reduced risk of gastric cancer: a systematic review and meta-analysis. Cancer Prev Res. 2014;7(1):12–22. https://doi.org/10.1158/1940-6207.CAPR-13-0282.
Tsugane S, Sasazuki S. Diet and the risk of gastric cancer: review of epidemiological evidence. Gastric Cancer. 2007;10(2):75–83. https://doi.org/10.1007/s10120-007-0420-0.
Kim GH, Liang PS, Bang SJ, Hwang JH. Screening and surveillance for gastric cancer in the United States: is it needed? Gastrointest Endosc. 2016;84(1):18–28. https://doi.org/10.1016/j.gie.2016.02.028.
Silvis SE, Nebel O, Rogers G, Sugawa C, Mandelstam P. Endoscopic complications. Results of the 1974 American Society for Gastrointestinal Endoscopy Survey. JAMA. 1976;235(9):928–30. https://doi.org/10.1001/jama.1976.03260350032023.
Evans JA, Chandrasekhara V, Chathadi KV, Decker GA, Early DS, Fisher DA, et al. The role of endoscopy in the management of premalignant and malignant conditions of the stomach. Gastrointest Endosc. 2015;82(1):1–8. https://doi.org/10.1016/j.gie.2015.03.1967.
Jun JK, Choi KS, Lee HY, Suh M, Park B, Song SH, et al. Effectiveness of the Korean National Cancer Screening Program in reducing gastric Cancer Mortality. Gastroenterology. 2017;152(6):1319–e13287. https://doi.org/10.1053/j.gastro.2017.01.029.
Lee YC, Chiang TH, Chou CK, Tu YK, Liao WC, Wu MS, et al. Association between Helicobacter pylori Eradication and Gastric Cancer incidence: a systematic review and Meta-analysis. Gastroenterology. 2016;150(5):1113–e11245. https://doi.org/10.1053/j.gastro.2016.01.028.
Kim HJ, Chang WK, Kim MK, Lee SS, Choi BY. Dietary factors and gastric cancer in Korea: a case-control study. Int J Cancer. 2002;97(4):531–5. https://doi.org/10.1002/ijc.10111.
Lim SH, Kwon JW, Kim N, Kim GH, Kang JM, Park MJ, et al. Prevalence and risk factors of Helicobacter pylori infection in Korea: nationwide multicenter study over 13 years. BMC Gastroenterol. 2013;13:104. https://doi.org/10.1186/1471-230X-13-104.
Walker SL, Williams JS, Lu K, Dawson AZ, Egede LE. Trends in Healthcare expenditures among adults in the United States by Cancer diagnosis status, 2008–2016: a cross-sectional study. Cancer Epidem Biomar. 2022;31(8):1661–8. https://doi.org/10.1158/1055-9965.EPI-21-0575.
Han KT, Kim W, Kim S. Disparities in healthcare expenditures according to economic status in cancer patients undergoing end-of-life care. BMC Cancer. 2022;22(1):303. https://doi.org/10.1186/s12885-022-09373-y.
Morishima T, Lee J, Otsubo T, Imanaka Y. Association of healthcare expenditures with aggressive versus palliative care for cancer patients at the end of life: a cross-sectional study using claims data in Japan. Int J Qual Health Care. 2014;26(1):79–86. https://doi.org/10.1093/intqhc/mzt081.
Tan YK, Fielding JW. Early diagnosis of early gastric cancer. Eur J Gastroenterol Hepatol. 2006;18(8):821–9.
Mareike L, Jana T, Eva MB. Application of Andersen’s behavioural model of health services use: a scoping review with a focus on qualitative health services research. BMJ Open. 2021;11(5):e045018. https://doi.org/10.1136/bmjopen-2020-045018.
DeSalvo KB, Jones TM, Peabody J, McDonald J, Fihn S, Fan V, et al. Health Care Expenditure Prediction with a single item, self-rated Health measure. Med Care. 2009;47(4):440–7.
Novignon J, Olakojo SA, Nonvignon J. The effects of public and private health care expenditure on health status in sub-saharan Africa: new evidence from panel data analysis. Health Econ Rev. 2012;2(1):22. https://doi.org/10.1186/2191-1991-2-22.
Gallet CA, Doucouliagos H. The impact of healthcare spending on health outcomes: a meta-regression analysis. Soc sci med. 2017;179:9–17. https://doi.org/10.1016/j.socscimed.2017.02.024.
Ades F, Senterre C, De Azambuja E, Sullivan R, Popescu R, Parent F, et al. Discrepancies in cancer incidence and mortality and its relationship to health expenditure in the 27 European Union member states. Ann Oncol. 2013;24(11):2897–902. https://doi.org/10.1093/annonc/mdt352.
Murakami K, Matsubara H. Chronology of gastrointestinal cancer. Surg Today. 2018;48(4):365–. https://doi.org/10.1007/s00595-017-1574-y. 70.
National Health Insurance Service (NHIS). Population Coverage. 2023. https://www.nhis.or.kr/english/wbheaa02400m01.do
National Health Insurance Service (NHIS). Sample Research DB: Details of DB and cost (Elderly). 2023. https://nhiss.nhis.or.kr/bd/ab/bdaba022Oeng.do#
World Health Organization (WHO). Republic of Korea health system review. 2015. (Vol. 5, No. 4). https://iris.who.int/bitstream/handle/10665/208215/9789290617105_eng.pdf
Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with hispanic populations in the United States. Soc sci med. 2009;69(7):983–91. https://doi.org/10.1016/j.socscimed.2009.05.011.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. https://doi.org/10.1093/aje/kwq433.
Choi JM, Kim SG, Kim J, Han SJ, Park JY, Oh S, et al. Clinical implications of pre-existing adenoma in endoscopically resected early gastric cancers. PLoS ONE. 2017;12(5):e0178419. https://doi.org/10.1371/journal.pone.0178419.
Koyama N, Katayanagi S, Kawachi S. Pre-existing interstitial lung disease as a risk factor for pneumonitis associated with ramucirumab and paclitaxel in patients with gastric cancer: the impact of usual interstitial pneumonia. PLoS ONE. 2018;13(6):e0198886. https://doi.org/10.1371/journal.pone.0198886.
Liu K, Zhou Y. Correlation of autoimmune pancreatitis and risk of gastric cancer in east Asian population. Am J Gastroenterol. 2022;117(9):1539. https://doi.org/10.14309/ajg.0000000000001789.
Miyagawa K, Kumamoto K, Shinohara N, Watanabe T, Kumei S, Yoneda A, et al. Autoimmune pancreatitis with gastric Cancer: some IgG4-related diseases May be paraneoplastic syndrome. Intern Med. 2022;61(14):2155–60. https://doi.org/10.2169/internalmedicine.8590-21.
Quiroga M, Shephard EA, Mounce LT, Carney M, Hamilton WT, Price SJ. Quantifying the impact of pre-existing conditions on the stage of oesophagogastric cancer at diagnosis: a primary care cohort study using electronic medical records. Fam Pract. 2021;38(4):425–31. https://doi.org/10.1093/fampra/cmaa132.
Shiokawa M, Kodama Y, Yoshimura K, Kawanami C, Mimura J, Yamashita Y, et al. Risk of cancer in patients with autoimmune pancreatitis. Am J Gastroenterol. 2013;108(4):610–7. https://doi.org/10.1038/ajg.2012.465.
Yoon JM, Son KY, Eom CS, Durrance D, Park SM. Pre-existing diabetes mellitus increases the risk of gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19(6):936. https://doi.org/10.3748/wjg.v19.i6.936.
Gordis L. Epidemiology e-book. Elsevier Health Sciences; 2013.
Shin HS, Seo B. Latent class model for mixed variables with applications to text data. Korean J Appl Stat. 2019;32(6):837–49. https://doi.org/10.5351/KJAS.2019.32.6.837.
Lennon H, Kelly S, Sperrin M, Buchan I, Cross AJ, Leitzmann M, et al. Framework to construct and interpret latent class trajectory modelling. BMJ open. 2018;8(7):e020683. https://doi.org/10.1136/bmjopen-2017-020683.
Kwon S. Thirty years of national health insurance in South Korea: lessons for achieving universal health care coverage. Health Policy Plan. 2009;24(1):63–71. https://doi.org/10.1093/heapol/czn037.
Santana IR, Mason A, Gutacker N, Kasteridis P, Santos R, Rice N. Need, demand, supply in health care: working definitions, and their implications for defining access. Health Econ Policy Law. 2023;18(1):1–13. https://doi.org/10.1017/S1744133121000293.
Brownlee S, Chalkidou K, Doust J, Elshaug AG, Glasziou P, Heath I, et al. Evidence for overuse of medical services around the world. Lancet. 2017;390(10090):156–68. https://doi.org/10.1016/S0140-6736(16)32585-5.
Allin S, Grignon M, Le Grand J. Subjective unmet need and utilization of health care services in Canada: what are the equity implications? Soc sci med. 2010;70(3):465–72. https://doi.org/10.1016/j.socscimed.2009.10.027.
Glasziou P, Straus S, Brownlee S, Trevena L, Dans L, Guyatt G, et al. Evidence for underuse of effective medical services around the world. Lancet. 2017;390(10090):169–77. https://doi.org/10.1016/S0140-6736(16)30946-1.
Yeh MCH, Wang YH, Yang HC, Bai KJ, Wang HH, Li YCJ. Artificial intelligence–based prediction of lung cancer risk using nonimaging electronic medical records: deep learning approach. J Med Internet Res. 2021;23(8):e26256. https://doi.org/10.2196/26256.
Song HN, Go SI, Lee WS, Kim Y, Choi HJ, Lee US, et al. Population-based Regional Cancer incidence in Korea: comparison between Urban and Rural areas. Cancer Res Treat. 2016;48(2):789–97. https://doi.org/10.4143/crt.2015.062.
Lee WR, Han KT, Choi M, Park S, Kim W. Impact of disability status on mortality in patients with gastric Cancer: a nationwide study focusing on Regional disparities. Healthc (Basel). 2023;11(5). https://doi.org/10.3390/healthcare11050641.
Kim HW, Shin DW, Yeob KE, Cho IY, Kim SY, Park SM, et al. Disparities in the diagnosis and treatment of gastric Cancer in relation to disabilities. Clin Transl Gastroenterol. 2020;11(10):e00242. https://doi.org/10.14309/ctg.0000000000000242.
Kim Y, Shin DW, Kim HW, Jung JH, Han K, Cho IY, et al. Disparities in gastric cancer screening among people with disabilities: a national registry-linkage study in South Korea. Gastric Cancer. 2020;23(3):497–509. https://doi.org/10.1007/s10120-019-01017-8.
Tu H, Wen CP, Tsai SP, Chow WH, Wen C, Ye Y, et al. Cancer risk associated with chronic diseases and disease markers: prospective cohort study. BMJ. 2018;360:k134. https://doi.org/10.1136/bmj.k134.
Hoang T, Lee J, Kim J. Comorbidity Risk Score in Association with Cancer incidence: results from a Cancer Screenee Cohort. Cancers (Basel). 2020;12(7). https://doi.org/10.3390/cancers12071834.
Choi W, Chun JW, Lee SJ, Chang SH, Kim DJ, Choi IY. Development of a MyData platform based on the personal health record data sharing system in Korea. Appl Sci. 2021;11(17):8208. https://doi.org/10.3390/app11178208.
Acknowledgements
None.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2022R1F1A1074383).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Woo-Ri Lee, Ki-Bong Yoo, and Minjee Lee. All authors wrote the first draft of the manuscript and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted using secondary data with anonymized and encrypted personal information. Therefore, Informed consent was not required from the study participants and the requirement for ethical approval was waived by the Institutional Review Board of Yonsei University, South Korea (1041849-202211-SB-206-01) as a review exemption study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, WR., Yoo, KB., Noh, JW. et al. Health expenditure trajectory and gastric cancer incidence in the National Health Insurance Senior Cohort: a nested case-control study. BMC Health Serv Res 24, 1076 (2024). https://doi.org/10.1186/s12913-024-11494-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11494-y