Abstract
Background
The transition to the “test-and-treat” policy in Nepal in 2017, coupled with the rapid initiation of antiretroviral therapy (ART) in 2020, necessitates an in-depth understanding of factors influencing ART initiation and retention. This study investigates these factors from the perspectives of healthcare providers, families/communities, and people living with HIV (PLHIV).
Methods
Employing a qualitative design, in-depth interviews were conducted with 24 ART clients and 26 healthcare providers across different provinces of Nepal. A comprehensive interview guide facilitated the exploration of experiences and perceptions. Interviews were transcribed verbatim, and thematic analysis was applied to distill key insights. Guided by a socio-ecological model, interviews were analyzed to identify the barriers and facilitators to ART initiation and continuation at the individual, family/community, and health system levels.
Results
Facilitators and barriers were identified at three levels. Individual-level facilitators included fear of death, perceived health benefits, knowledge about HIV/ART, confidentiality, and financial support. Barriers encompassed concerns about lifelong medication, side effects, denial of HIV status, fear of disclosure, and financial constraints. At the family/community level, support from family and community health workers facilitated ART adherence, while social stigma and discrimination posed barriers. The health system’s role was dual; the provision of free treatment, a client tracking system and a robust drug supply chain were facilitators, whereas logistical challenges and service accessibility during the COVID-19 pandemic were notable barriers.
Conclusions
This study highlights the various factors that influence ART initiation and retention in Nepal during the test-and-treat era. Tailored interventions should focus on increasing awareness about HIV and ART, strengthening healthcare systems, ensuring availability of medications, and providing accessible treatment during service disruptions. Furthermore, these interventions should encourage supportive environments at the individual, community, and healthcare system levels. Taking this holistic approach is essential for effectively implementing ART and achieving long-term health outcomes in light of changing public health policies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The early initiation of Antiretroviral Therapy (ART) has demonstrated positive impacts on various epidemiological aspects of HIV and AIDS, particularly longer survival time, enhanced immune reconstitution, and reduced mortality rates due to improved time to viral suppression and better health outcomes [1, 2]. Research in low-income countries also found benefits for less onward transmission [3]. These findings prompted the World Health Organization (WHO) to introduce the “test-and-treat” strategy in 2015, which recommends rapid initiation of ART for all people living with HIV (PLHIV) within 7 days of HIV confirmation, regardless of their immunological or clinical status [4, 5]. Nepal has implemented its National HIV Strategic Plan for the years 2021–2026 to address the HIV epidemic [6]. This strategic plan serves as Nepal’s guideline to achieve 95-95-95 targets, i.e. 95% of people living with HIV to be aware of their status, 95% of those diagnosed to be on sustained antiretroviral therapy, and 95% of those on treatment to have viral suppression. To reach this goal, in February 2017, the government of Nepal implemented the “Test-and-Treat” strategy across all 84 ART sites in the country [7]. Consequently, there was a 17% increase in the number of PLHIV initiating ART, rising from 13,069 PLHIV on ART in December 2016 to 15,260 in December 2017 [8]. However, achieving high levels of viral suppression through engagement in ART care remains crucial for reducing HIV-related mortality and morbidity among PLHIV [9]. Similarly, adherence to treatment plays a crucial role in preventing viral resistance, comorbid conditions, and mortality [10, 11].
There are currently 85 HIV treatment centers in 61 districts in Nepal that provide free ART to all PLHIV, as the burden of HIV is primarily concentrated in these areas. The HIV epidemic shows higher prevalence in four specific regions—Kathmandu Valley, Pokhara, Highway districts, and Sudurpaschim Province—necessitating increased access to testing and treatment. Therefore, all these districts have access to ART centers. However, in the remaining 16 districts, where HIV is not prevalent, HIV screening is available up to birthing centers. These 16 districts are included within the antiretroviral dispensing sites network. Thus, if any PLHIV seek services, they will be linked to ART centers, and medications will be transferred to the appropriate district. Sub-centers for dispensing antiretroviral have been strategically placed within local health facilities to enhance access for PLHIV. These efforts were coordinated with ART, community, and home-based care providers. The community-based ART dispensing centers operate under the differentiated service delivery model, specifically catering to men who have sex with men (MSM) and transgender populations, with 26 centers currently operational nationwide.
Most of the HIV treatment services are offered in government hospitals and primary health centers, with only three community-based ART centers managed by communities. Government-owned ART centers operate with funding from the Government of Nepal’s budget. Each center has a dedicated ART counselor responsible for providing counseling, treatment, and monitoring—including antiretroviral side effects, viral load, and treatment adherence—as well as care, support services, and managing all records and reports. The ART dispensing centers function with the existing human resources of the health facility. The national program provides training, distance guidance, and support, working in close collaboration with ART centers for pill distribution and record-keeping. However, NGO-run or community-based dispensing centers are supported by donors; for example, PEPFAR, as they provide services to MSM and transgender populations. There are no private health facilities that provide ART in Nepal.
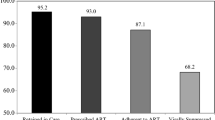
In addition, to enhance treatment accessibility, there are 45 antiretroviral dispensing sites in the country, targeting key populations and individuals residing in remote hilly and mountainous areas. Antiretroviral medications are procured and supplied by the Nepalese government, with the exception of cases supported by donors in instances of delayed procurement or insufficient funds. The distribution of antiretroviral drugs from the central level to provincial health facilities is overseen by the federal government. Treatment coverage, the proportion of people living with HIV who are receiving antiretroviral treatment, has more than doubled, increasing from 32% in 2016 to 78% in 2022 [8]. However, despite this progress, achieving the 95-95-95 targets in Nepal by 2022 has been uneven: 92% of the estimated total PLHIV who are aware of their HIV status (the first 95), 84% of total PLHIV who are aware of their status and are on ART (the second 95), whereas only 72% of total PLHIV on ART have achieved a suppressed viral load (the third 95 target) [8].
ART adherence is a dynamic and intricate behavior that is influenced by socio-economic and cultural factors [12]. Previous studies conducted in Nepal have identified various barriers to treatment initiation and retention, including stigma, discrimination, concerns about confidentiality breaches, unfavorable behavior exhibited by clinical staff, financial constraints, long travel times to the ART centers, inadequate knowledge about ART regimens, and fear of adverse effects [13,14,15,16]. However, these studies were conducted prior to the implementation of the test-and-treat strategy, hence there may be additional or different barriers and facilitators following its implementation as ART is initiated earlier than before. Concerns have been raised about the capacity of healthcare systems to meet the needs of a larger number of new patients, as well as concerns about the availability of ART medication given historical supply chain issues [17] and viral load testing capacity including reagents and cartridges [17]. Others point to the already limited availability of HIV test kits for diagnosing and confirming new positive tests [18]. Furthermore, there are ethical concerns about coercion and the increased possibility for drug resistance among those who start ART early under the test-and-treat strategy but who later struggle with adherence [19]. This issue is exacerbated by the limited treatment options within various drug classes, especially during the transition from first-line to second-line therapy in Nepal. The sole practical alternatives involve utilizing combinations, either two Nucleoside Reverse Transcriptase Inhibitors (2NRTIs) in conjunction with boosted Protease Inhibitors (PIs) or two Nucleoside Reverse Transcriptase Inhibitors (2NRTIs) in conjunction with Integrase Strand Transfer Inhibitors (INSTIs). There are no viable choices for incorporating CCR5 antagonists or fusion inhibitors in Nepal. Lost to follow up was also observed in trials of rapid ART [20].
An assessment of ART initiation and adherence barriers in the era of test-and-treat rollout in Nepal is needed to determine risks and benefits of this new policy implementation. We conducted a qualitative study to explore the barriers and facilitators to ART initiation and retention among PLHIV eligible for ART, from the perspectives of both PLHIV and health care providers, under the test-and-treat policy in Nepal.
Methods
Study design
We employed a descriptive design utilizing qualitative methods to obtain detailed descriptions of the facilitators and barriers to ART initiation and continuation following the implementation of the test-and-treat Strategy in Nepal. Key informant interviews were conducted with health care providers and PLHIV who were on ART.
Study participants
The study included two groups of participants: (a) health care providers; and (b) PLHIV registered at ART centers in Nepal. Recruitment was carried out using a purposive sampling approach [21]. A total of 50 participants were purposively selected from 22 ART sites located in 19 districts across five provinces (Sudurpaschim, Karnali, Lumbini, Bagmati, and Koshi).
Health care providers
Eligible health care providers were those from one of 26 health care centers offering HIV care at ART centers in Nepal. The participants represented diverse genders and came from rural and urban centers, as well as hills (West rukum, Kalikot, Salyan, Dailekh, Doti, Accham, Lalitpur, Dhankuta, Illam, Kathmandu, Dadeldhura), terai (Kapilvastu, Rupandehi, Kailali, Kanchanpur, Rapti, Udayapur, Sunsari), and mountain regions (Darchula, Sakhuwasabha). ART centers with high and low retention rates were also included. The participants were approached during their ART data monitoring meetings and workshops held in four districts in various parts of Nepal (Nepalgunj, Dhangadhi, Bhadrapur, and Kathmandu districts). The main purpose of ART data monitoring meetings and workshops was to align the priorities of all stakeholders to strengthen the national recording and reporting system for the HIV program. Workshop goal was to integrate all recording tools—from prevention programs, testing, treatment, to care and support services—into the DHIS2 tracker system. Additionally, these workshops were organized to update participants on the latest developments in the information system and instruct them on how to utilize various features more effectively. A 10-minute information session was conducted during each meeting, and interested participants provided written informed consent. Additionally, interviews were conducted with laboratory experts from major viral load testing sites in Nepal. The major viral load testing sites in Nepal include the National Public Health Laboratory and Sukraraj Tropical and Infectious Disease Hospital, both located in Kathmandu, the capital city. Other significant sites are Bir Hospital in Kathmandu, Seti Provincial Hospital in Sudurpaschim Province, Pokhara Academy of Health Sciences in Gandaki Province, and Koshi Hospital in Koshi Province.
PLHIV on ART
Eligible participants were individuals who were 18 years of age or older, diagnosed with HIV by an HIV clinical provider, and registered for HIV treatment and care at ART centers. We included 24 PLHIV representing all genders, residing in urban and rural settings, terai, hills, and mountain regions, and from all key population categories. We collaborated with health care providers who participated in our study to reach out to PLHIV as potential participants. The health care providers informed the potential participants about the study and obtained consent to share their phone numbers with the research team. The interested participants were contacted by the research team, and informed consent was obtained. For those participants without formal education, witnessed informed consent was facilitated by the interviewer.
This study was approved by the ethical review board of the Nepal Health Research Council, Kathmandu (REF no. 410/2021). We provided Nepalese Rupee 350 as compensation for transportation and communication costs to all the study participants.
Data collection tools and techniques
The research team underwent an intensive three-day training on qualitative interviews, in-depth probing techniques, and ethical considerations. Trained qualitative interviewers with experience in qualitative research conducted interviews with participants in the Nepali language. The interviews took place either in person, virtually (via Zoom or Teams), or over the telephone, using an open-ended pretested interview guide from August 2021 to November 2021. We maintained privacy and safety of the participants during all interviews. In-person interviews took place in secluded and confidential rooms, prioritizing participants’ comfort and confidentiality. For online and telephone interviews, participants and interviewers were in their respective private rooms. All interviews were audio-recorded and ranged in duration from 40 min to an hour. We stored audio-records as de-identified in a password-protected laptops, only accessible to researchers.
The interview guide [see Additional file 1] examined the facilitators and barriers to ART initiation and continuation during the test-and-treat era, based on the Health Belief Model [22] and the health system building blocks [23]. The Health Belief Model allowed us to examine individuals’ perceptions and attitudes towards ART, including their understanding of the severity of HIV and AIDS, their susceptibility to the complications of discontinuation of ART, and the perceived benefits and barriers to ART. On the other hand, the WHO health system building blocks provided a framework to examine the broader health system level factors affecting ART access and adherence within the domains of six building blocks: healthcare financing, service delivery, human resources, information systems, medical products and technologies, and governance. The interview guide for PLHIV used included 9 components: demographic characteristics, HIV knowledge, perceived benefits of early initiation and continuation of ART, perceived severity, perceived susceptibility, perceived barriers, cues to action, environmental factors of ART centers, and self-efficacy. The health care provider interview guide used the WHO health system building blocks and consisted of nine sections: demographic characteristics, general service, knowledge and attitude, service delivery, medical supplies, human resources, information system, leadership, and health financing. An iterative process was employed, with discussions held after each interview to provide suggestions for future interviews. Subsequent interviews developed deeper into themes emerging from earlier interviews. Data collection continued until data saturation was reached, meaning that no new information was obtained from the participants [24].
Data analysis
All interviews were transcribed verbatim, and the transcripts were reviewed by the interviewer and a trained research assistant for accuracy against the audio-recordings. Thematic analysis [25] was utilized for data analysis. This process involved becoming familiar with the data, generating initial codes, identifying themes, reviewing themes, defining and naming themes, and producing the report. The research team developed a hierarchical codebook by synthesizing codes derived directly from the data (inductive) and from the interview guides (deductive). The inductive aspect captured insights and patterns emerging from the data itself, and deductive aspect ensured that the the key themes outlined in the interview guides were systematically captured in the data. This integrated method allowed us for comprehensive coding. After coding the initial transcripts, the four researchers involved, along with the senior researchers, met to compare the labels they had applied and agreed upon the set of codes to be applied to all subsequent transcripts. The codes were then categorized broadly, and grouped together under common themes which were reviewed and defined. The themes, categories, codes, and relevant quotes were translated into English. An example of emergent theme categories and codes can be found in Table 1.
The analysis and conceptualization of the data were guided by socio-ecological systems theory to aid in understanding the interplay between HIV clients and their environment [26]. After organizing the data into matrices and synthesizing them into broader themes, those specifically concerning ART initiation and adherence were integrated into a socio-ecological framework to better illustrate the findings (Fig. 1).
Results
Characteristics of the participants
Additional file 2 presents the characteristics of participants. Out of 26 health care providers, 57.7% were male, with a mean age of 30.6 ± 5.2 years. Most health care providers (61.5%) had an educational background as health assistants or nurses. Approximately 80.8% of the health care providers were ART counselors, and 11.5% were lab technicians and technologists, with a median job experience of 4 years in the ART center. Among the 24 PLHIV, 58.0% were female, and the mean age was 38 ± 11 years. The median duration of ART treatment was 3 years. The majority of PLHIV (41.7%) had completed secondary education. Half of the PLHIV (50.0%) were involved in agriculture.
Facilitators and barriers to ART initiation and continuation
Health care providers and PLHIV identified a range of individual, family/community, and health system level facilitators that supported the implementation of Test-and-Treat (Fig. 1).
Individual level
Facilitators
-
(a)
Fear of death: Some health care providers and many PLHIV mentioned the fear of dying due to complications from AIDS as a motivating factor to initiate and continue ART. Additionally, some PLHIV also reported that witnessing the deaths of relatives and neighbors who were PLHIV motivated them to start ART.
“There have been some sad incidents here. Two people with HIV have died because they weren’t careful, and one of them was a retired army brother. He used to drink a lot and not pay attention.”-A 34-year-old male PLHIV.
A healthcare provider described a cycle in which PLHIV become lost to follow up only to return to care upon realizing their health was declining.
“Some clients didn’t take their medicine for a year, but when their health got worse, they realized the health consequences of not continuing the drugs and returned back to the ART clinic to get their medicine…”-A 27-year-old female health care provider.
-
(b)
Health benefits: Some health care providers stated that the PLHIV were motivated to continue ART after experiencing health benefits such as reduced symptoms of diarrhea and fever. Most of the PLHIV pointed out that their health improved after starting medications. Some PLHIV who had joined at a later stage of HIV reported having suffered devastating effects of the virus on their bodies and recalled vivid illnesses and experiences. The rapid improvement in health that they experienced after initiating ART strengthened their trust in the medication. Both PLHIV and health care providers shared that the benefits of starting ART were feeling better, increased appetite, weight gain, and longer life expectancy. Some reported that PLHIV were no longer bedridden, regained their strength, and were able to return to their work. These benefits encouraged them to continue taking their medications.
“Doctor said that having medicines would help to alleviate fever…later when I came here, I felt relieved to a certain extent…not having medicines seems to aggravate symptoms, when I don’t take medicines for 10–15 days, I feel sick, I get a fever, lack of appetite. etc.”-A 27-year-old male PLHIV.
“After starting medicines, my body felt relieved, earlier it used to feel heavy, couldn’t wake up in the morning, sometimes there was headache, sometimes fever, …after I started medication, my body now feels light/relieved” -A 35-year-old female PLHIV.
-
(c)
Knowledge: Many PLHIV explained the health benefits of initiating and continuing ART treatment. Some of PLHIV and health care providers mentioned knowledge about preventing HIV transmission to their partners and opportunistic infections for themselves as the main reasons to start ART early. Many PLHIV also indicated that having a good knowledge of HIV and ART leads to better ART retention.
“For instance, there are husband and wife, one gets positive for HIV while another gets negative …we have to convince the husband that the disease won’t transmit to his wife if he takes the medicine…when we tell him about his wife’s safety, he agrees right away to take the medicine.”-A 30-year-old male health care provider.
-
(d)
Confidentiality: A health care provider stated that maintaining confidentiality motivates ART initiation and continuation, noting that the dissemination of medicine through general health centers, where other health services are also offered, reduces the chances of disclosure. Some PLHIV mentioned that they sought ART services at the center because they were assured of the center’s commitment to maintaining their anonymity and privacy.
“If counselors keep and maintain the anonymity of each client, then clients will be driven to attend sessions and take their medicine on a consistent basis. There are few clients engaged as sex workers here, and because we do not reveal their identities, they regularly attend the ART clinic.” -A 30-year-old male health care provider.
-
(e)
Financial support: Some health care providers and PLHIV mentioned financial support for treatment as a motivating factor to initiate and continue ART. Several PLHIV believed that financial hardship would not be a barrier to initiating and continuing ART because they were financially supported. Two health care providers also stated that the provision of travel costs to the ART center was one of the main motivators for PLHIV to continue ART.
“I don’t believe that any of us need to experience any kind of financial stress as the center has helped us in every possible way… when we run into any issues, the health care staff offer us financial support such as transportation costs, lodging, and food.“-A 28-year-old male PLHIV.
Barriers
-
(a)
Denial of HIV status: Some health care providers and PLHIV felt that denial about HIV diagnosis was a major reason for individuals declining ART. Some health care providers noted that some PLHIV experience mental shock and instability upon learning their positive status, associating it with death, which hinders them from making informed decisions about medication. The social stigma surrounding HIV also reinforces this denial. While others do not feel ill and therefore do not find it necessary to take medications.
“Clients think they’re fine (clinically well) and refuse taking the medicine. Few clients don’t have any symptoms at first, so they don’t want to start ART.” -A 41-year-old male program coordinator.
-
(b)
Perspective on lifelong ART and side-effects: Some health care providers and PLHIV expressed concerns about starting a medication that needs to be taken every day for the rest of their lives. Some PLHIV reported avoiding initiating ART or waiting until they were severely ill before starting. They were hesitant about the test-and-treat approach or rapid ART initiation due to the prospect of lifelong medication.
“Taking medicine for the rest of your life is not easy. Most of the time, we just take Cetamol (antipyretics or analgesics) for a few days and leave it at that. In our case, we have to take this HIV medicine for the rest of our lives, and some people forget to take it every day. This could be one reason why people stop taking the medicine”- A 22-year-old female PLHIV.
Most PLHIV reported experiencing unexpected and unbearable side effects upon ART initiation, such as body itching, dizziness, vomiting, insomnia, fever, and allergies. These side effects compelled them to stop taking the medicine for a certain duration. Health care providers also highlighted concerns about side effects as a major obstacle to initiating ART. They emphasized that PLHIV fear the potential harmful effects and that some PLHIV have discontinued ART due to side-effects. Initiating and continuing ART was especially difficult in children, who were hesitant to take drugs and sometimes vomited as soon as they swallowed a pill.
During the first three months of taking antiretroviral medication, I experienced side effects such as vomiting, lack of appetite, and bodily pains… I was unable to wake up in the morning due to headaches and discomfort, however after three to four months, the side effects subsided. -A 35-year-old female PLHIV.
-
(c)
Fear of disclosure and internalized HIV stigma: Many healthcare providers and PLHIV felt that stigma related to HIV diagnosis and taking ART inhibits them from disclosing their HIV status to their partners, and families. This discourages them from initiating ART or obtaining monthly refills. Some PLHIVs even preferred to travel to another city or district to collect ART to avoid disclosure, which resulted in missed appointments and refills due to other financial and access barriers. PLHIV refrained from disclosing their status due to feeling of shame and fear of hatred, discrimination, and social isolation. One PLHIV explained that her partner pressured her not to disclose her HIV status to other family members due to these fears. The feeling of shame and social discrimination was associated with engaging in HIV risk behaviors, such as multiple sexual partners and drug abuse, which are stigmatized in society.
“My spouse forced me not to inform my parents… he also threatened that if I tell my parents about my HIV status, he would leave me… so I haven’t informed my parents because I’m ashamed, and I’m afraid they will hate me….”A 35-year-old female PLHIV.
-
(d)
Lack of information and competing priorities: Inadequate awareness and understanding about the importance of being in care were barriers to ART initiation. Both health care providers and PLHIV cited a lack of understanding about HIV and ART as a significant barrier to starting and maintaining ART. Some PLHIV explained that they were unaware of the new national policy to start HIV treatment as soon as possible after receiving a positive diagnosis, which left them confused and hesitant.
“I think one of the reasons for not initiating antiretroviral medicine is due to lack of awareness about treatment benefits among ART clients … Health centers are also unable to effectively raise awareness about this.” -A 34-year-old male PLHIV.
A female PLHIV claimed that her husband refused to take the antiretroviral drugs even after knowing his status, stating that:
“My husband refused to take the medicine.…. I told my husband that we should go there (in the ART center) and seek treatment. But he said he didn’t want to live any longer and that if I wanted to, I could go by myself.” -A 35-year-old female PLHIV.
Some health care providers and PLHIV reported forgetting to take medications due to being busy, being away from home, experiencing stress, consuming alcohol, or having to attend family or community events.
“People forget to carry their medications with them…. I, too, was once so preoccupied with work that I neglected to take my medication regularly. There are some people who drink alcohol and forget to take their medication.” - A 27-year-old male PLHIV.
A few health care providers mentioned denial or discontinuation of ART due to involvement with faith healers (Dhami, Jhakri).
“There are some clients who believe in Dhami/jhakri…. there is a female client in ward 10 who still refuses to take the antiretroviral medication. The client feels as though something is stuck in her throat while taking the medication, and she also practices and believes in traditional healing practices. We have counseled her numerous times to take the medication, but she continues to refuse.”-A 30-year-old female health care provider.
-
(e)
Seasonal Migration, transportation cost and limits of multi-month dispensation policy: Poor financial status contributed to lower access due to transportation costs, interrupted access due to seasonal migration to India, and inadequate communication with health care providers. This directly affected the initiation and continuation of ART, despite the medication being available free of cost. Many health care providers and PLHIV expressed financial hardship and migration as an underlying cause for not initiating or discontinuing ART. Additionally, PLHIV from low socioeconomic backgrounds are engaged in farming, which provides them with limited cash flow and a high workload, making it challenging for them to visit ART centers for refills.
“Some clients are not willing to come to visit ART centers to receive the medicine due to lack of money for transportation… and, these clients only intake the medicine if it is brought to their homes by the center or community and home-based care providers.” A 29-year-old female health care provider.
“There are many HIV-positive migrant workers in India from our area… we cannot provide them medication for more than three months at a time. As they must go to work, we cannot compel them to stay here for medication consumption; hence, it is difficult for us to ensure that the client adheres to medication.” - A 23-year-old female health care provider.
Family and community level
Facilitators
-
(a)
Family support: Some health personnel and many PLHIV emphasized the importance of family support. Family support played a significant role in two distinct ways. First, the acceptance of PLHIV’s HIV status by their family members helped them gain confidence and combat stigma. Second, family members provided care during illness, obtained medication refills when the PLHIV were busy, and reminded them to take their antiretrovirals daily.
“The support and care of my family has been important in maintaining my excellent health today.” -A 40-year-old male PLHIV.
-
(b)
Community health workers’ support: Some health care providers reported that the PLHIV are followed up by community health care workers, supported by non-governmental organizations, to encourage them to continue ART. Community health workers track PLHIV who fail to show up for their medication. Workers from community and home-based care programs visit the homes of the PLHIV who have missed their medication and provide counseling, emphasizing the consequences of non-adherence.
“We have a community and home-based care team responsible for following up with clients at the community level. We actively search for clients who have been lost to follow up and visit their homes to provide further counseling” -A 23-year-old female health care provider.
Barriers
-
(a)
Anticipated and experienced stigma: Some health care providers mentioned that PLHIV experience shame and fear of being associated with HIV and its risk factors, such as having multiple sex partners and drug use. This fear keeps some PLHIV from attending clinics, particularly stand-alone ART centers. Stigma leads to PLHIV avoiding interactions within the community. Some PLHIV also avoid taking medications at work due to the fear of their co-workers witnessing it.
“People won’t let us go to the temple if they find out we’re taking HIV medication. We can only share about our situation to health personnel… we cannot tell the rest of society about it.” - A 52-year-old male PLHIV.
“Social stigma in this community has caused me a lot of trouble. People don’t look directly at my face, they don’t want to walk, sit, or eat with me… it seems that most people have a negative impression of me. That’s why I’m not getting the medicine from the center near my home “-A 23-year-old female PLHIV.
Most PLHIV mentioned experiencing some form of discrimination and HIV-related stigma, which had a negative impact on them. Health care providers also observed that discrimination by society was one of the reasons for loss to follow up. A few PLHIV also shared their experiences of discrimination by hospital medical staff.
“Sometimes, doctors treat us differently in the hospital. We go to the hospital like any other patient, but when they find out we have HIV, they ignore us… Then we have to go to the ART center, where the counselor will tell us which doctors to see.” -A 22-year-old female PLHIV.
-
(b)
Lack of family support: Health professionals, as well as a few PLHIV, noted that PLHIV without family support are more likely to either not to initiate ART or discontinue it. Conflicts within families due to the positive HIV status of a family member has been a major problem for PLHIV, with some even indicating that family members forced them to discontinue ART. A female client mentioned that her husband left her after learning about her HIV status, resulting in a delay in ART initiation.
“From the very first day, I wanted to take the medication, but my spouse never supported it. I repeatedly asked him to go to the health facility and take the medication, but he refused…I had a baby with me, and back then, I couldn’t go by myself. Even now, after my spouse’s death, I still lack family support.” -A 35-year-old female PLHIV.
Health system level
Facilitators
-
(a)
Free services: Many health care providers mentioned the availability of free testing for HIV and viral load and treatment services as well as government health insurance for PLHIV, which positively influenced ART initiation and continuation. The availability of health insurance allowed PLHIV to receive free services, including lab testing and treatment for other health issues. PLHIV also expressed satisfaction with the financial support provided (such as travel incentives) provided for viral load testing.
‘We provide free lab test services, and almost all HIV programs and services are freely available in our center.”- A 32-year-old male senior medical technologist.
“There are many financial incentives that encourage ART clients to begin their medication. One significant factor is the free distribution of antiretroviral medicine from our center. While the cost of the medicine is considerable, the Nepal government covers it at no charge. Additionally, numerous health insurance benefits are now available for clients, which could serve as further motivation for them to adhere to their medication regimen.” – A 33-year old female health care provider.
-
(b)
Uninterrupted drug supply: Many health care providers emphasized the importance of ART supply management, including bi-monthly reporting to the federal government on medicine stock, timely delivery of medicine based on reporting, and replenishment of medicines from other nearby ART centers. These practices facilitate the maintenance of medicine stock at ART centers. The uninterrupted supply of ART throughout the year helps build trust with PLHIV. The supply chain requires special attention, especially during the monsoon season when roads can become disrupted, and when PLHIV are transferred to a specific ART center.
“Even when we are out of stock, we continue to give medicine to our clients. We coordinate with the federal government during stockouts as well as seek assistance from other ART sites when medication is in short supply.”- A 30-year-old male health care provider.
-
(c)
Human resources availability: Most health care providers indicated the availability of sufficient and trained/skilled human resources at the ART centers to deliver the services to PLHIV. Most of the PLHIV appreciated the health care providers` behavior and attitude and expressed feeling encouraged and motivated to continue HIV services due to the supportive nature of some health care providers.
“The health care providers are very nice to us. They smile and talk to us every time, which I really liked. Each and every health care provider at the clinic counsels us with extremely kind demeanors.” -A 35-year-old female PLHIV.
-
(d)
Monitoring PLHIV through electronic medical record system using District Health Information Software version 2 (DHIS2) tracker:
Health care providers reported the utilization of systematic reporting and recording via the DHIS2 tracker, which facilitated the tracking and timely follow-up of PLHIV, thereby enhancing operational efficiency. Additionally, the DHIS2 tracker simplified the process for staff to monitor and coordinate follow-ups with PLHIV according to their individual schedules. The most significant advantage of employing tracker line list reports was the ability to readily identify PLHIV who were underperforming in terms of missed appointments, unsuppressed viral loads, and other critical metrics, a task that was challenging with paper-based registers. Furthermore, the DHIS2 Tracker also streamlined the process of downloading lists of PLHIV on ART and identifying those eligible for viral load sample collection.
“Diverse community-led organizations in our area offer outreach services, including care, support, and community-based home care, to PLHIV in need. The DHIS2 Tracker information system facilitates the identification and extraction of data regarding PLHIV on ART, categorizing them based on their adherence and retention rates. We share this information with community-led organizations to assist in re-engaging clients who have been lost to follow-up in HIV treatment programs.”A 28-year-old male health care provider.
“The DHIS2 Tracker, an electronic system, significantly enhances our ability to manage PLHIV on ART effectively on a daily basis. It allows for streamlined analysis, access, and management of patients’ clinical appointments scheduled for the day, the following day, or within the week. Furthermore, it enables the efficient downloading and sorting of files to prioritize eligible PLHIV on ART for viral load testing during sample collection days, a process that would otherwise take hours or days with paper-based registers.”A 30-year-old female health care provider.
-
(e)
Monitoring and Supervision: The integration of both in-person and virtual supportive supervision and monitoring, as reported by a majority of service providers, is facilitated by health workers at the federal level, provincial teams, and other groups. This approach has significantly aided healthcare providers in enhancing service quality. Notably, it has been instrumental in tracking clients who are lost to follow-up and ensuring their re-enrollment into the treatment programs. Furthermore, it has enabled health facilities to effectively monitor and manage the treatment outcomes of PLHIV.
“We receive an Excel sheet on a monthly or bi-monthly basis from higher authorities, including federal and provincial level health workers. This sheet includes the client codes of PLHIV on ART, detailing their status and suggested actions. For example, it provides a list of PLHIV who are lost to follow-up or those eligible for viral load testing but have not yet been tested. This systematic reminder and support enable us to utilize available resources more effectively to enhance retention and prioritize PLHIV for the necessary services.“A 30-year-old male health care provider.
During the last monitoring and supervision visit, we discussed how to bring loss to follow up clients to the ART centers and also regarding testing strategy in the rural areas. -A 30-year-old male health care provider.
Barriers
-
(a)
Geographic Accessibility: The geography of Nepal posed a significant challenges to the ability of PLHIV to reach ART centers, which was highlighted by both PLHIV and health care providers. Some health care providers mentioned poor transportation facilities, long distances to ART clinics, and bad road conditions during the rainy season as key barriers to service accessibility, especially in remote hilly and mountain areas. Most PLHIV reported having to travel for more than an hour to reach the ART center, which is further complicated by expensive travel costs.
“Clients in these (remote) outlying areas find it difficult to travel to the ART center because of its rural location. It’s difficult to serve our clients since no local organizations work together with us there…. The lack of road accessibility in rural areas makes it harder for us to bring the clients to the ART center.” - A 33-year-old female health care provider.
-
(b)
Workforce training needs: Many health care providers identified insufficient human resources as a major barrier to efficient service provision. In addition, some health care providers mentioned being overburdened with other tasks in the health center, hindering proper counseling. They frequently expressed the need for additional refresher training in clinical management, counseling, logistics, recording/reporting, and viral load testing. Some of them also cited the transfer or expiration of the working period of trained health care providers as a barrier.
“Main problem is the transfer of the trained staff. Because of federalization, our trained staff got transferred. Previously, whenever I was not available, he used to handle everything. But now that he has been transferred, the position is empty… In this way, there is a shortage of adequately trained staff…” -A 33-year-old female health care provider.
-
(c)
Lack of effective implementation of Multi Month Dispensing (MMD), dispensing antiretroviral drug for 3–6 months: Some health care providers emphasized that the lack of effective MMD implementation, resulting from delays in ART supply or inadequate stock at ART centers, required PLHIV to make monthly visits to the ART center and incur frequent transportation and time costs. This posed a barrier, especially for those who live far away, have a farming background, or are seasonal migrant workers.
“Since most of our clients go to India for work. We cannot provide them with medicine for 5–6 months at once, and we cannot even ask them not to go to their work. They need to work to feed themselves. Because of that, it’s a bit difficult…” -A 23-year-old female health care provider.
-
(d)
COVID-19 interruptions: The COVID-19 pandemic had multiple impacts on HIV services. Some health care providers mentioned interruptions in the supply of medicines, regular training schedules, and a decrease in supervision visits due to travel restrictions imposed during the pandemic. Especially in the initial days, some PLHIV were unable to visit ART centers to refill their medicines, which also hampered testing of viral load. A few health care providers stressed that nationwide shelter-in-place disrupted public transportation, impeding PLHIV’s access to ART sites during the early period of the pandemic. However, in later months, some health care providers mentioned that antiretroviral drugs were delivered to PLHIV`s homes by counselors and community health professionals.
“Due to lockdown, clients did not receive the medicine for a few months. … Later, with the support of the community care center and local police, we were able to deliver the medicines even during the lockdown period.” -A 30-year-old male health care provider.
“Following the COVID-19 pandemic, our clients completely stopped visiting the facility to receive the medicines… staff used to be present at the facility, but clients didn’t come…”- A 28-year-old male health care provider.
Additionally, COVID-19 interrupted the supply of viral load testing reagents and the collection and transfer of samples, resulting in a decrease in viral load tests.
-
(e)
Challenges to test viral load regularly: Several challenges were noted for conducting regular viral load testing. Laboratory technicians mentioned a lack of trained staff at the laboratory, delays in receiving electronic data from ART centres, delays in receiving viral load reagents, and reduced viral load testing due to COVID-19.
“Sometimes, we don’t receive reagents on time since it is supplied from outside. Last time during COVID-19, it took four to five months for us to receive the reagents.” -A 31-year-old female health care provider.
“There are instances when we have reagents on hand but we are unable to perform tests because the machine has broken down. In addition, we are unable to fix the machine on our own and have to wait for a qualified technician. And administrative hold-ups also create difficulties for engineers to proceed. These delays sometimes lead to testing delays.” -A 31-year-old female health care provider.
Discussion
We aimed to understand the barriers and facilitators that influence the initiation and/or retention of ART in PLHIV in Nepal following the implementation of the test-and-treat strategy. At the individual PLHIV level, we identified fear of death, health benefits, knowledge, confidentiality, and financial support as major facilitators, while denial, side effects, fear of disclosure and internalized HIV stigma, competing priorities, and financial hardship were identified as major barriers to ART retention. At the family level, support from family and community health providers motivated PLHIV to remain in treatment, whereas anticipated and experienced stigma were considered as the major barriers to retention. At the health system level, free services, uninterrupted drug supply, availability of human resources, the DHIS2 recording and tracking system, and monitoring and supervision contributed to the ART retention of PLHIV. However, inaccessibility, insufficient human resources, inadequate multi-month dispensing policy and drug supply, and challenges in viral load testing were reported as major barriers.
Our finding revealed that PLHIV’s motivation to initiate and continue treatment was positively influenced by a better understanding of the health benefits of ART. Increased knowledge about HIV reduces fear and ignorance, enabling individuals to consistently start and continue their medication [27]. Moreover, this finding aligns with studies demonstrating the role of health literacy in improving health outcomes among PLHIV [28, 29]. Our findings suggest the need for strengthening the government efforts to strengthen PLHIV’s understanding and motivation for ART. These efforts may include providing structured support for peer educators, expanding training programs to reach a wider spectrum of healthcare professionals, and strengthening outreach to underserved communities.
The beneficial effects of treatment with improved health also served as a motivator for ART continuation in other settings [30, 31]. In our study, PLHIV were motivated to visit ART centers and begin treatment due to the confidentiality maintained by health care personnel. The identification of appropriate behavior and confidentiality as contributing factors to ART continuation among PLHIV is supported by similar studies conducted in resource-limited settings [32,33,34,35]. Confidentiality fosters trust between PLHIV and health care providers while also addressing stigma, social discrimination, and fear of disclosure.
Similar to our study, fear of disclosing one’s HIV infection status was commonly reported as a barrier by respondents and has been previously documented in research conducted in low- and middle- income countries [13, 36]. A systematic review conducted to examine barriers to ART adherence in developed and developing nations, reported that PLHIV who do not disclose their status to their family members or peers experience worse treatment outcomes compared to those who disclose [31].
One of the main reasons for delaying or discontinuing ART initiation among PLHIV was the fear of lifelong commitment to drug adherence and potential drug side effects. The experience of side effects contributed to non-adherence, and this finding is supported by several studies conducted in both high-income and low-income countries [13, 31, 36, 37].
We identified financial constraints as the primary contributing factor to ART initiation and continuation, which interacted with the affordability of ART clinic visits and pushing migration. Although antiretroviral drugs were provided for free in Nepal, costs associated with ART such as transportation, prescriptions, and diagnostic tests were identified as barriers to initiating and continuing ART. This finding is consistent with other studies conducted in Nepal [37, 38]. PLHIV highlighted inadequate job opportunities leading to emigration, which negatively affected adherence to ART. Migration is commonly cited as a reason for non-retention in low-resource settings [39,40,41] due to difficulties in accessing treatment without proper identification, paperwork, and lack of interest among migrant workers [42, 43]. In our setting, the lack of dispensing ART for more than three months was a major barrier to ART engagement for those who were migrant workers. Nutritional support and financial incentives have shown to improve ART continuation [44]. Interventions to address the need for large supplies of ART for migrants may also be needed.
Financial and psychological support from family members are key enablers of ART initiation and retention. Various global studies have documented that family support increases the likelihood of PLHIV maintaining optimal adherence [13, 36, 45, 46]. A meta-analysis found that PLHIVs from cohesive families are nearly twice as likely to continue ART compared to those who do not have cohesive families [47]. Disclosure of HIV status to partners and the general population has been shown to improve access to HIV prevention and treatment programs, as PLHIV receive higher family and social support and experience less anxiety [48, 49].
In low-resource-constrained settings, the reliance on community health workers (CHWs) for HIV care continues to grow [50, 51]. Our findings also revealed good adherence to medication through tracking and monitoring systems implemented by health workers. In Nepal, different organization extends home-based care package for PLHIV through community health workers, including accompanied referral and support for direction to seek services, drugs refilling, positive prevention, and other healthcare- related support [52]. The community-based home services through CHW is valued and appreciated in Nepal [53].
As highlighted in our study, the health-seeking behaviours of PLHIV were influenced by social stigma and discrimination. This phenomenon is observed worldwide, as shown in the findings from the United States [53,54,55], Asia [56,57,58], sub-Saharan Africa [59,60,61], and Europe [62].
Previous studies have shown significant levels of stigma and discrimination are prevalent among PLHIV and Key populations in Nepal [13, 63,64,65,66,67]. Despite ongoing efforts to reduce stigma and discrimination, these are still major barriers to access HIV related information and services [68].
Moreover, we found that PLHIV feared being shunned by their family, friends, and the general public. This fear may arise from the negative attitudes towards HIV due to its mode of transmission, which is associated with socially disapproving behaviors such as having multiple sex partners or using illicit injectable drugs. To address this challenge, a multi-faceted intervention that includes information provision, skill-building, counseling, and facilitating interaction between PLHIV and the community holds the potential to reduce stigma and improve ART adherence and continuation of care [69,70,71]. Stakeholders, governmental, and non-governmental organizations should work collectively to mitigate the negative impacts of HIV-related social stigma and discrimination. While HIV interventions in Nepal are predominantly funded by external sources, incorporating local cultural perspectives into policy and program is essential for effectively addressing HIV-related stigma within the Nepali context.
A functional health system plays a crucial role in facilitating ART initiation and continuation in multiple ways. Firstly, uninterrupted drug supply to PLHIV was identified as a facilitator, likely due to the establishment of trust and confidence in the availability of drugs when needed. A systematic review conducted in developed and developing nations identified irregular drug supply as one of the barriers to continuing ART [31]. Secondly, Many PLHIV expressed feeling encouraged and motivated to continue accessing HIV services due to the supportive nature of certain health care providers. Adherence to treatment improves when PLHIV have a strong connection with their healthcare providers and trust in their expertise [72]. Thirdly, an e-register based information system known as the HIV Care and ART Tracking System (DHIS2 Tracker, mHealth and biometric) offered opportunities to monitor PLHIV’s treatment progress in real-time, identify poor-performing and clinically well PLHIV and take immediate action [73]. Previous studies from Bangladesh [74] and Jamaica [75] have also highlighted DHIS2 as an effective monitoring tool for a country’s health system.
A major barrier was the poor access to ART centers due to long travel distances, challenging terrain, lack of transportation services in rural areas, and the further deterioration of road conditions especially during the rainy season. The issues of long travel distances and a lack of transportation services were also highlighted in another study conducted in Nepal [13]. Several studies globally have also documented that travel time and access to treatment centers pose barriers to ART adherence [31, 56, 76]. Our study participants were concerned about the increasing transportation expenses associated with collecting antiretroviral drugs, which aligns with similar findings from qualitative research conducted in Nepal [13]. Service providers expressed concerns about PLHIV’s ability to consistently refill their ART prescriptions on a monthly basis. To address this challenge, MMD has emerged as a key modality of service delivery, providing ART supplies for a period of 3 to 6 months to the PLHIV who have suppressed viral load VL, have no side effects, have no opportunistic infections, and are not pregnant [77]. MMD is important because it reduces the frequency of clinic visits, thereby decreasing the burden on healthcare facilities and patients. A revised guideline in Nepal advocates for multi-month dispensing, allowing eligible and stable PLHIV to receive three to six months of antiretroviral prescriptions, and up to 12 months for migrant workers [78]. However, routine implementation faced challenges in timely and adequate procurement of antiretroviral drugs in Nepal [79].
Access to HIV treatment was further hindered by systemic issues, such as a high turnover of trained human resources. The availability and deployment of qualified health care providers were crucial facilitators, while the lack of qualified providers posed significant barriers, consistent with findings from other studies [80].
Our study also sheds light on the negative impacts of the COVID-19 pandemic on the delivery of ART services, including delays in receiving medication, supervision, monitoring, and a decrease in the number of visits from PLHIV. Similar disruptions in ART services during the COVID-19 pandemic have been observed in Pakistan [56], China [81] and Uganda [82]. Various reports have highlighted disruptions in the delivery of ART services and the diversion of the resources to control the pandemic, resulting in reduced activities of the national HIV programs [8, 83]. However, National Centre for AIDS and STD Control (NCASC) in Nepal addressed these challenges by disseminating the 2020 HIV Testing and Treatment Guidelines during COVID-19 in May 2020, introducing Dolutegravir (DTG) as the first-line drug for all PLHIV and advocating for rapid ART initiation [84]. Additionally, home delivery services were established to ensure uninterrupted access to antiretroviral drugs for PLHIV, while those who inject drugs received opioid substitution therapy services at home during nationwide shelter-in-place orders. Furthermore, personal protective equipment was distributed to health workers involved in HIV response. Despite these efforts, our study results showed significant implementation gaps, indicating the need for continued vigilance and adaptation to ensure the sustained delivery of ART services and support for PLHIV in emergency situations.
Routine viral load monitoring, along with appropriate interventions based on the viral load results, has been documented to improve treatment results of second-line ART, reduce morbidity and mortality, and decrease ART resistance [85, 86]. Health care providers faced challenges in viral load testing due to a lack of trained personnel, delays in reporting, and insufficient funding to provide the tests for free to PLHIV. Similarly, several studies have highlighted limited access to viral load testing in many low- and middle-income countries due to financial, logistical, and human resource constraints in national AIDS control programs [4, 87]. Without the ability to measure viral loads tracking treatment progress and achieving national HIV targets in Nepal would be challenging. Additionally, the country has formulated a standard service package for the national HIV program [52]. However, to date, various implementing partners have not been able to standardize services or provide the minimum recommended service packages to key populations, particularly regarding geographical coverage and the limited resources available. Ensuring the effective implementation of the prioritized activities within the HIV standard service package for key populations, including nationwide coverage, will address the challenges related to the early initiation of ART and ensure high retention rates in treatment.
This is the first qualitative study to explore the facilitators and barriers to ART initiation and treatment following the implementation of the test-and-treat strategy in Nepal. A primary strength of the study was the inclusion of both PLHIV and health care providers across the nation, allowing for a comprehensive understanding of perspectives. We employed purposive sampling to select PLHIV with diverse demographic characteristics and medication adherence behaviors, as well as health care providers with extensive expertise, ensuring a range of opinions on the topic. Rigorous qualitative data analysis was conducted, addressing the concerns through coding and thematic analysis to ensure the reliability of the collected data. However, the study had some limitations. Some interviews were conducted via phone, which may have resulted in the loss of non-verbal cues. All information obtained from the interviews were self-reported and not cross-checked or validated. Nevertheless, the qualitative data collectors were experienced interviewers trained in qualitative data collection. Furthermore, the study participants were limited to HIV care providers and recipients, potentially overlooking policy-level factors influencing ART initiation and retention. Interviewing planners and policymakers could have provided more comprehensive insights into these factors. Future research should include these stakeholders to capture the full spectrum of socio-ecological determinants better.
Conclusions
This study has identified the complex web of factors that affect the initiation and retention of PLHIV in care. These factors operate and interact at multiple levels, including personal perceptions, societal attitudes and health-system infrastructure. At the individual level, psychological barriers such as denial, side effects, fear of stigma, lack of information, and competing priorities deter PLHIV from initiating and continuing ART. Conversely, factors such as knowledge, confidentiality, and financial support facilitate ART initiation and continuation. The influence of family and community was acknowledged. Social stigma and discrimination create additional concerns for PLHIV leading to reluctance to seek care. Furthermore, the health facility’s capacity is closely linked to PLHIV care. Free services, consistent drug supply, adequate human resources, DHIS2 tracking system, and monitoring contribute access and continuity of PLHIV care. Challenges such as financial and logistical constraints to multi-month dispensation and issues with viral load testing should be addressed. To achieve the overarching national HIV program goals, future interventions need to address these barriers at all levels in collaboration with relevant stakeholders. Tailored strategies targeting experiences and needs of the PLHIV community are essential. By addressing these multidimensional aspects of initiation and retention in care, we can make significant strides towards improving HIV treatment outcomes.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 2NRTIs:
-
Two nucleoside reverse transcriptase inhibitors
- AIDS:
-
Acquired immunodeficiency syndrome
- ART:
-
Antiretroviral therapy
- COVID-19:
-
Coronavirus disease 2019
- HIV:
-
Human immunodeficiency virus
- INSTIs:
-
Integrase strand transfer inhibitors
- NA:
-
Not applicable
- PCL:
-
Proficiency certificate level
- PI:
-
Protease inhibitors
- PLHIV:
-
People living with HIV
- SD:
-
Standard deviation
- WHO:
-
World Health Organization
References
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Mfinanga S, Chanda D, Kivuyo SL, Guinness L, Bottomley C, Simms V, et al. Cryptococcal meningitis screening and community-based early adherence support in people with advanced HIV infection starting antiretroviral therapy in Tanzania and Zambia: an open-label, randomised controlled trial. Lancet. 2015;385(9983):2173–82.
Boyd M, Boffito M, Castagna A, Estrada V. Rapid initiation of antiretroviral therapy at HIV diagnosis: definition, process, knowledge gaps. HIV Med. 2019;20(S1):3–11.
WHO. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach, 2nd ed. [cited 2023 Jul 4]. https://www.who.int/publications-detail-redirect/9789241549684.
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
National HIV. Strategic Plan 2021–2026. Government of Nepal Minsitry of Health and Population National Centre for AIDS and STD Control Teku, Kathmandu.
NCASC, National HIV. Testing and Treatment Guidelines 2017. 2017 [cited 2023 Jul 4]. https://ncasc.gov.np/publications/234.
National Centre for AIDS & STD Control (NCASC). Factsheet 33rd World AIDS Day 2020. [cited 2023 Jul 4]. https://ncasc.gov.np/wad-2020.
WHO. Viral suppression for HIV treatment success and prevention of sexual transmission of HIV. [cited 2023 Jul 4]. https://www.who.int/news/item/20-07-2018-viral-suppression-for-hiv-treatment-success-and-prevention-of-sexual-transmission-of-hiv.
Abadiga M, Hasen T, Mosisa G, Abdisa E. Adherence to antiretroviral therapy and associated factors among human immunodeficiency virus positive patients accessing treatment at Nekemte referral hospital, west Ethiopia, 2019. PLoS ONE. 2020;15(5):e0232703.
Aghaei A, Mohraz M, Shamshirband S. Effects of media, interpersonal communication and religious attitudes on HIV-related stigma in Tehran, Iran. Inf Med Unlocked. 2020;18:100291.
Castro A. Adherence to antiretroviral therapy: merging the clinical and social course of AIDS. PLoS Med. 2005;2(12):e338.
Wasti SP, Simkhada P, Randall J, Freeman JV, Van Teijlingen E. Barriers to and facilitators of antiretroviral therapy adherence in Nepal: a qualitative study. J Health Popul Nutr. 2013;30(4):410–9.
Koirala S, Deuba K, Nampaisan O, Marrone G, Ekström AM, CAT-S group. Facilitators and barriers for retention in HIV care between testing and treatment in Asia-A study in Bangladesh, Indonesia, Lao, Nepal, Pakistan, Philippines and Vietnam. PLoS ONE. 2017;12(5):e0176914.
Zhou J, Tanuma J, Chaiwarith R, Lee CKC, Law MG, Kumarasamy N, et al. Loss to Followup in HIV-Infected patients from Asia-Pacific Region: results from TAHOD. AIDS Res Treat. 2012;2012:1–10.
Bam K, Rajbhandari RM, Karmacharya DB, Dixit SM. Strengthening adherence to anti retroviral therapy (ART) monitoring and support: operation research to identify barriers and facilitators in Nepal. BMC Health Serv Res. 2015;15:188.
Bigna JJR, Plottel CS, Koulla-Shiro S. Challenges in initiating antiretroviral therapy for all HIV-infected people regardless of CD4 cell count. Infect Dis Poverty. 2016;5(1):85.
Meka AFZ, Billong SC, Diallo I, Tiemtore OW, Bongwong B, Nguefack-Tsague G. Challenges and barriers to HIV service uptake and delivery along the HIV care cascade in Cameroon. Pan Afr Med J. 2020;36:37.
Kulkarni SP, Shah KR, Sarma KV, Mahajan AP. Clinical uncertainties, health service challenges, and ethical complexities of HIV test-and-treat: a systematic review. Am J Public Health. 2013;103(6):e14–23.
Ford N, Migone C, Calmy A, Kerschberger B, Kanters S, Nsanzimana S, et al. Benefits and risks of rapid initiation of antiretroviral therapy. AIDS. 2018;32(1):17–23.
Rebecca Robinson. Purposive Sampling | SpringerLink. [cited 2023 Jul 4]. https://springerlink.bibliotecabuap.elogim.com/referenceworkentry/10.1007/978-94-007-0753-5_2337.
Rosenstock IM. Historical origins of the Health Belief Model. Health Educ Monogr. 1974;2(4):328–35.
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. World Health Organization; 2010 [cited 2023 Jul 4]. xii, 92 p. https://apps.who.int/iris/handle/10665/258734.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2017;27(4):591–608.
Peterson BL. Thematic Analysis/Interpretive Thematic Analysis. In: Matthes J, Davis CS, Potter RF, editors. The International Encyclopedia of Communication Research Methods. 1st ed. Wiley; 2017 [cited 2023 Jul 4]. pp. 1–9. https://onlinelibrary.wiley.com/doi/https://doi.org/10.1002/9781118901731.iecrm0249.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
Obermeyer CM, Osborn M. The utilization of testing and counseling for HIV: a review of the social and behavioral evidence. Am J Public Health. 2007;97(10):1762–74.
Wawrzyniak AJ, Ownby RL, McCoy K, Waldrop-Valverde D. Health literacy: impact on the health of HIV-infected individuals. Curr HIV/AIDS Rep. 2013;10(4):295–304.
Zhai Y, Isadore KM, Parker L, Sandberg J. Responding to the HIV Health Literacy Needs of Clients in Substance Use Treatment: the role of Universal PrEP Education in HIV Health and Prevention. Int J Environ Res Public Health. 2023;20(19):6893.
Patel S, Baxi RK, Patel SN, Golin CE, Mehta M, Bakshi H, et al. Perceptions regarding barriers and facilitators to combination antiretroviral therapy adherence among people living with HIV/AIDS in Gujarat, India: a qualitative study. Indian J Sexually Transmitted Dis AIDS. 2012;33(2):107.
Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing Nation patient-reported barriers and facilitators. Attaran A, editor. PLoS Med. 2006;3(11):e438.
Mbonye AK, Hansen KS, Wamono F, Magnussen P. Increasing access to prevention of mother-to-child transmission of HIV services through the private sector in Uganda. Sex Transm Infect. 2009;85(7):534–9.
Parkhurst J. Understanding determinants of health service use from a systems perspective. J Health Serv Res Policy. 2008;13(2):122–3.
Shaikh BT, Haran D, Hatcher J. Where do they go, whom do they consult, and why? Health-seeking behaviors in the northern areas of Pakistan. Qual Health Res. 2008;18(6):747–55.
Shaikh BT, Hatcher J. Health seeking behaviour and health service utilization in Pakistan: challenging the policy makers. J Public Health (Oxf). 2005;27(1):49–54.
Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM, Bimirew MA, Kassie DM. Barriers and Facilitators of Adherence to Antiretroviral Drug Therapy and Retention in Care among Adult HIV-Positive Patients: A Qualitative Study from Ethiopia. Thorne C, editor. PLoS ONE. 2014;9(5):e97353.
Wasti SP, van Teijlingen E, Simkhada P, Randall J, Baxter S, Kirkpatrick P, et al. Factors influencing adherence to antiretroviral treatment in Asian developing countries: a systematic review. Trop Med Int Health. 2012;17(1):71–81.
Poudel AN, Newlands D, Simkhada P. The economic burden of HIV/AIDS on individuals and households in Nepal: a quantitative study. BMC Health Serv Res. 2017;17(1):76.
Bygrave H, Kranzer K, Hilderbrand K, Whittall J, Jouquet G, Goemaere E et al. JJ Miranda editor 2010 Trends in loss to Follow-Up among migrant workers on antiretroviral therapy in a community cohort in Lesotho. PLoS ONE 5 10 e13198.
Saether ST, Chawphrae U, Zaw MM, Keizer C, Wolffers I. Migrants’ access to antiretroviral therapy in Thailand: migrants’ access to antiretroviral therapy in Thailand. Tropical Med Int Health. 2007;12(8):999–1008.
Lima V, Fernandes K, Rachlis B, Druyts E, Montaner J, Hogg R. Migration adversely affects antiretroviral adherence in a population-based cohort of HIV/AIDS patients. Soc Sci Med. 2009;68(6):1044–9.
Sarode S, Naik NM, Soletti AB. Assessment of Healthcare Utilisation among Nepali Migrants Living with HIV/AIDS in Mumbai, India.
Sarode S, Ubale P, Soletti AB. Specification of Policy for the Barriers to Care and Treatment of Nepali Migrants Living with HIV/AIDS in India. In Review; 2022 Feb [cited 2023 Jul 12]. https://www.researchsquare.com/article/rs-1358799/v1.
Chaiyachati KH, Ogbuoji O, Price M, Suthar AB, Negussie EK, Bärnighausen T. Interventions to improve adherence to antiretroviral therapy: a rapid systematic review. AIDS. 2014;28:S187–204.
Kuznetsova AV, Meylakhs AY, Amirkhanian YA, Kelly JA, Yakovlev AA, Musatov VB, et al. Barriers and facilitators of HIV Care Engagement: results of a qualitative study in St. Petersburg, Russia. AIDS Behav. 2016;20(10):2433–43.
Mao L, Buchanan A, Wong HTH, Persson A. Beyond mere pill taking: SMS reminders for HIV treatment adherence delivered to mobile phones of clients in a community support network in Australia. Health Soc Care Community. 2018;26(4):486–94.
DiMatteo MR. Social Support and Patient Adherence to Medical Treatment: a Meta-analysis. Health Psychol. 2004;23(2):207–18.
C M. L K, D F, G H, L D. Disclosure of HIV status and its consequences. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 1999 Dec [cited 2023 Jul 12];89(12). https://pubmed.ncbi.nlm.nih.gov/10678182/.
UNAIDS. Counselling and HIV/AIDS. 1997.
Community and Home-Based Care in Nepal. Findings and Recommendations from a National Program Review.pdf. https://www.fhi360.org/sites/default/files/media/documents/Community%20and%20Home-Based%20Care%20in%20Nepal,%20Findings%20and%20Recommendations%20from%20a%20National%20Program%20Review.pdf.
Busza J, Dauya E, Bandason T, Simms V, Chikwari CD, Makamba M, et al. The role of community health workers in improving HIV treatment outcomes in children: lessons learned from the ZENITH trial in Zimbabwe. Health Policy Plann. 2018;33(3):328–34.
HIV standard service package for key populations ministry of health. and Population National Centre for AIDS and STD Control Teku, Kathmandu, Nepal 2020.
Pitasi MA, Chavez PR, DiNenno EA, Jeffries WL, Johnson CH, Demeke H, et al. Stigmatizing attitudes toward people living with HIV among adults and adolescents in the United States. AIDS Behav. 2018;22(12):3887–91.
Yabes JM, Schnarrs PW, Foster LB, Scott PT, Okulicz JF, Hakre S. The 3 levels of HIV stigma in the United States military: perspectives from service members living with HIV. BMC Public Health. 2021;21(1):1399.
Gunn JKL, Rooks-Peck C, Wichser ME, Denard C, McCree DH, Jeffries WL, et al. Effectiveness of HIV Stigma interventions for men who have sex with men (MSM) with and without HIV in the United States: a systematic review and Meta-analyses. AIDS Behav. 2022;26(S1):51–89.
Ahmed A, Dujaili JA, Jabeen M, Umair MM, Chuah LH, Hashmi FK, et al. Barriers and enablers for adherence to antiretroviral therapy among people living with HIV/AIDS in the era of COVID-19: a qualitative study from Pakistan. Front Pharmacol. 2022;12:807446.
Ekstrand ML, Heylen E, Mazur A, Steward WT, Carpenter C, Yadav K, et al. The role of HIV Stigma in ART Adherence and Quality of Life among Rural women living with HIV in India. AIDS Behav. 2018;22(12):3859–68.
Zhang C, Li X, Liu Y, Qiao S, Zhang L, Zhou Y, et al. Stigma against People Living with HIV/AIDS in China: does the Route of infection matter? Yuhua R. Editor PLoS ONE. 2016;11(3):e0151078.
Jones HS, Floyd S, Stangl A, Bond V, Hoddinott G, Pliakas T, et al. Association between HIV stigma and antiretroviral therapy adherence among adults living with HIV: baseline findings from the HPTN 071 (PopART) trial in Zambia and South Africa. Trop Med Int Health. 2020;25(10):1246–60.
Chirambo L, Valeta M, Banda Kamanga TM, Nyondo-Mipando AL. Factors influencing adherence to antiretroviral treatment among adults accessing care from private health facilities in Malawi. BMC Public Health. 2019;19(1):1382.
Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, et al. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. JAIDS J Acquir Immune Defic Syndr. 2003;34(3):281–8.
Nöstlinger C, Rojas Castro D, Platteau T, Dias S, Le Gall J. HIV-Related discrimination in European Health Care settings. AIDS Patient Care STDs. 2014;28(3):155–61.
Subedi B, Timilsina B, Tamrakar APN. Perceived stigma among people living with HIV AIDS in Pokhara, Nepal. HIV. 2019;11:93–103.
Nepal VP, Ross MW. Issues related to HIV stigma in Nepal. Int J Sex Health. 2010;22(1):20–31.
Kohlbrenner V, Deuba K, Karki DK, Marrone G. Perceived Discrimination Is an Independent Risk Factor for Suicidal Ideation among Sexual and Gender Minorities in Nepal. Niederkrotenthaler T, editor. PLoS ONE. 2016;11(7):e0159359.
Storm S, Deuba K, Shrestha R, Pandey LR, Dahal D, Shrestha MK, et al. Social and structural factors associated with depression and suicidality among men who have sex with men and transgender women in Nepal. BMC Psychiatry. 2021;21(1):476.
Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, et al. Stigma reduction interventions in people living with HIV to improve health-related quality of life. Lancet HIV. 2020;7(2):e129–40.
U.S. Agency for International Development. 2023 [cited 2023 Jul 12]. Meeting Targets and Maintaining Epidemic Control (EpiC) | Nepal | Fact Sheet. https://www.usaid.gov/nepal/fact-sheets/ho-epic.
Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16:18734.
Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16:18640.
Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS Stigma: what have we learned? AIDS Educ Prev. 2003;15(1):49–69.
Lewis MP, Colbert A, Erlen J, Meyers M. A qualitative study of persons who are 100% adherent to antiretroviral therapy. AIDS Care. 2006;18(2):140–8.
Chikwado DHIS. 2023 [cited 2023 Jul 12]. Nepal employs DHIS2 Tracker for improved data and results in its national HIV program. https://dhis2.org/nepal-hiv-tracker/.
Begum T, Khan SM, Adamou B, Ferdous J, Parvez MM, Islam MS, et al. Perceptions and experiences with district health information system software to collect and utilize health data in Bangladesh: a qualitative exploratory study. BMC Health Serv Res. 2020;20(1):465.
Tazhmoye V, Crawford CA, Dosunmu, Kimalie F, Parchment. Using the District Health Information Software 2 as a Think-Tank Strategy for HIV and Syphilis Prevention in Jamaica. Journal of Interdisciplinary Research and Innovations. [cited 2023 Jul 12]; https://www.researchpublish.com/papers/using-the-district-health-information-software-2-as-a-think-tank-strategy-for-hiv-and-syphilis-prevention-in-jamaica.
Posse M, Meheus F, Van Asten H, Van Der Ven A, Baltussen R. Barriers to access to antiretroviral treatment in developing countries: a review: barriers to ART in developing countries. Tropical Med Int Health. 2008;13(7):904–13.
A rapid assessment. Of multi-month dispensing of antiretroviral treatment and pre-exposure prophylaxis the Asia-Pacific region final report August 2020 UNAIDS Regional Office For Asia And The Pacific.
NCASC, National. HIV testing and treatment guidelines. 2020. http://ncasc.gov.np/uploaded/Banner/National-HIV-Testing-Guidelines-May-10-2020-WEB-Version.pdf.
LINKAGES NEPAL Summary of Achievements October. 2016 – September 2020. https://www.fhi360.org/sites/default/files/media/documents/resource-linkages-nepal-achievements-summary.pdf.
Colvin CJ, Konopka S, Chalker JC, Jonas E, Albertini J, Amzel A et al. A Systematic Review of Health System Barriers and Enablers for Antiretroviral Therapy (ART) for HIV-Infected Pregnant and Postpartum Women. Fischer G, editor. PLoS ONE. 2014;9(10):e108150.
Guo W, Weng HL, Bai H, Liu J, Wei XN, Zhou K, et al. [Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(5):662–6.
Linnemayr S, Jennings Mayo-Wilson L, Saya U, Wagner Z, MacCarthy S, Walukaga S, et al. HIV Care experiences during the COVID-19 pandemic: mixed-methods telephone interviews with clinic-enrolled HIV-Infected adults in Uganda. AIDS Behav. 2021;25(1):28–39.
ITPC Global. [cited 2023 Jul 12]. Impacts of COVID-19 on women living with HIV who use drugs in Nepal. https://itpcglobal.org/blog/resource/impacts-of-covid-19-on-women-living-with-hiv-who-use-drugs-in-nepal/.
Government of Nepal Ministry of Health and Population National Centre for AIDS &. STD Control Impact of COVID-19 Pandemic on National HIV Programme in Nepal. 2020.
Piot P, Quinn TC. Response to the AIDS pandemic — A Global Health Model. N Engl J Med. 2013;368(23):2210–8.
Sollis KA, Smit PW, Fiscus S, Ford N, Vitoria M, Essajee S et al. Systematic Review of the Performance of HIV Viral Load Technologies on Plasma Samples. Gray CM, editor. PLoS ONE. 2014;9(2):e85869.
Lecher S, Williams J, Fonjungo PN, Kim AA, Ellenberger D, Zhang G, et al. Progress with Scale-Up of HIV viral load monitoring — seven sub-saharan African countries, January 2015–June 2016. MMWR Morb Mortal Wkly Rep. 2016;65(47):1332–5.
Acknowledgements
The authors would like to thank the study participants and health facilities for their kind support to carry out this study.
Funding
Funding for this study was provided by the national grant of The Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
AS and KD conceived and designed the study. AS, LP, SS, NJ, BHK, and KD contributed to data collection, data management and data analysis. AS, LP and KD drafted the first version of manuscript with inputs from PS, RK, LRP, MBK and EW. All authors contributed substantially to manuscript drafting and revision, and approved submission of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Institutional Review Board of Nepal Health Research Council has approved the study. All participants provided informed consent prior to study participation. Permission was also obtained to digitally record all interviews. All procedures performed in studies involving human participants were in accordance with the ethical standards of the 2019 National Ethical Guidelines for Health Research in Nepal and with the 1964 Helsinki declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shrestha, A., Poudel, L., Shrestha, S. et al. Multilevel determinants of antiretroviral therapy initiation and retention in the test-and-treat era of Nepal: a qualitative study. BMC Health Serv Res 24, 927 (2024). https://doi.org/10.1186/s12913-024-11311-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11311-6