Abstract
Background
The objective of this study was to carry out a cost-effectiveness analysis of dapagliflozin, as an add-on therapy to standard of care (SoC), for the treatment of type 2 diabetes mellitus (T2DM) in Spain, based on the results of the DECLARE-TIMI 58 trial.
Methods
A discrete event simulation model (Cardiff T2DM) based on the data observed in the DECLARE-TIMI 58 trial was adapted to the Spanish setting to estimate the costs and health outcomes of treatment with dapagliflozin in patients with T2DM who had or were at risk of atherosclerotic cardiovascular disease. Macrovascular events (hospitalization for heart failure, myocardial infarction, stroke, and unstable angina), end-stage renal disease and cardiovascular and non-cardiovascular mortality were modeled according to the survival equations of the DECLARE-TIMI 58 study. Microvascular events (blindness and ulcers) were estimated based on the risk equations of the UK Prospective Diabetes Study. The analysis was conducted from the Spanish National Health System perspective and the time horizon was 30 years. The results were evaluated in terms of cost per quality-adjusted life year (QALY) gained. Only direct health costs were included, and a 3% discount rate was applied to costs and health outcomes. Univariate and probabilistic sensitivity analyses (PSA) were made to assess the robustness of the results.
Results
In the main analysis, dapagliflozin was a dominant therapeutic option compared with placebo, with greater effectiveness (0.08 QALYs) and lower associated total costs per patient (€ -2,921). The univariate sensitivity analysis and the PSA confirmed the robustness of the results. The PSA showed the probability that dapagliflozin was a dominant alternative compared with placebo was 84.2% and that it was cost-effective of 92.1%, under a willingness-to-pay of € 20,000/QALY gained.
Conclusions
The analysis of data from the DECLARE-TIMI 58 trial shows that dapagliflozin would be a cost-effective option in Spain for the treatment of adult patients with T2DM, as an add-on therapy to SoC, compared with placebo.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Diabetes mellitus (DM) is a chronic disease with a high socioeconomic impact due to its associated morbidity and mortality. Patients with DM have two to three times increased risk of cardiovascular morbidity than the general population [1]. In addition, the direct costs of DM account for between 8% and 13% of total health expenditure by the Spanish National Health System (NHS) and were estimated at € 5,809 million in 2012 [2, 3]. The main conditioning factors are the costs of hospitalization and pharmacological treatment, which account for more than 70% of direct costs (41% and 32%, respectively) [3]. Diabetes complications increase the pharmacological and disease management cost, as well as the risk of hospitalization, and involve significant productivity loss [3].
Type 2 DM (T2DM) accounts for around 90% of all cases of diabetes [4]. In Spain, the prevalence of T2DM is estimated at 13.8%, of which approximately 6% are undiagnosed [5], and the incidence rate is 11.6 cases per 1,000 person-years [6]. T2DM is characterized by hyperglycemia and caused by insufficient secretion of insulin from pancreatic beta cells and insulin resistance [7]. T2DM is often associated with obesity and other modifiable risk factors (sedentary lifestyle, smoking, diet, high blood pressure, dyslipidemia, etc.) that increase the cardiovascular risk and reduce the quality of life [1, 7].
Currently, the management of T2DM requires a multifactorial and individualized approach to control blood glucose and other risk factors [7]. The main recommendation to achieve glycemic control is lifestyle modification (physical activity and diet). However, when it is not sufficient, metformin remains the first choice of treatment for most patients [7].
In uncontrolled patients with T2DM, sodium-glucose cotransporter-2 inhibitors have proven efficacy in achieving sustained glycemic control, providing cardiovascular benefits, and reducing body weight and blood pressure, without increasing the hypoglycemic risk [8]. The DECLARE-TIMI 58 trial evaluated the effects of dapagliflozin on cardiovascular and renal outcomes in 17,160 T2DM patients who had or were at risk for atherosclerotic cardiovascular disease [9]. Participants were randomly assigned to dapagliflozin 10 mg/day or placebo, as an add-on therapy to standard of care (SoC). Treatment with dapagliflozin result in a lower rate of hospitalization for heart failure (HF) and cardiovascular death, and a reduction in the progression of kidney disease, compared with placebo [9].
In Spain, dapagliflozin is reimbursed in adults for the treatment of insufficiently controlled T2DM as an adjunct to diet and exercise as monotherapy when metformin is considered inappropriate due to intolerance, and in addition to other medicinal products for the treatment of T2DM. Dapagliflozin is prescribed by endocrinologists in the hospital setting.
The objective of this study was to evaluate cost-effectiveness of dapagliflozin, as an add-on therapy to SoC, for the treatment of uncontrolled patients with T2DM in Spain, according to the results of the DECLARE-TIMI 58 trial.
Methods
Model structure and type of analysis
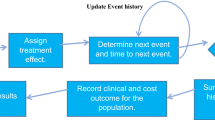
A cost-effectiveness analysis was used to evaluate the use of dapagliflozin, as an add-on therapy to SoC, compared with placebo for the treatment of T2DM from the NHS perspective. This analysis was performed by adapting the Cardiff T2DM Model, a Monte Carlo simulation model with individual fixed time increments that was developed using equations from the United Kingdom Prospective Diabetes Study [10,11,12], and was previously validated to simulate the disease progression of patients with T2DM [13,14,15,16]. This model has recently been updated to include the survival curves observed in the DECLARE-TIMI 58 trial [9, 17] and a module to track the progression of the estimated glomerular filtration rate (eGFR) through stages 2-5 of chronic kidney disease (CKD). Model predictions over a time horizon of 4.2 years were validated to results from the DECLARE-TIMI 58 trial (see Additional file 1). To further validate the model, the structure, main assumptions and inputs were validated with clinical experts to ensure it simulated clinical practice in Spain.
The model simulated the natural history of T2DM in a cohort of 1,000 patients, considering usual Spanish clinical practice, treatment effectiveness and direct healthcare costs. The costs associated with drug acquisition, treatment discontinuation, T2DM-related micro- and macrovascular complications, adverse events (AEs) and severe hypoglycemic events, and the management of CKD were included. Macrovascular events (hospitalization for HF, myocardial infarction, stroke, unstable angina), all-cause mortality and end-stage renal disease (ESRD) were predicted by specific survival curves of each event, which were fitted to Kaplan-Meier data collected over the DECLARE-TIMI 58 trial and extrapolated from 4-year survival curves over the time horizon. Spanish life tables were applied if the age- and gender-specific probability of mortality in the general population exceeded the predicted probability from the survival curves. Microvascular events (blindness and ulcers) were estimated based on UKPDS 82 study risk equations [11].
The simulations were performed individually for each patient in 6-month cycles until the end of the time horizon or death. Considering the mean baseline age of the patients included and their life expectancy in Spain, a time horizon of 30 years was assumed. A 3% discount rate was applied to health costs and outcomes, in accordance with the Spanish recommendations for economic evaluation and budget impact of drugs [18].
The model estimated the economic and clinical consequences, expressed in quality-adjusted life years (QALY), for each therapeutic alternative during the time horizon. The results of the analysis were evaluated in terms of cost per QALY gained, expressed as the incremental cost-effectiveness ratio (ICER).
Treatment alternatives evaluated
According to the DECLARE-TIMI 58 trial, the initial cohort included patients with uncontrolled T2DM who had started treatment with dapagliflozin (10 mg/day) or placebo, as add-on therapy to SoC with metformin, sulphonyl urea, insulin, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 receptor agonists and/or diet [9]. Treatment intensification was not considered, but the model assumed that patients discontinued dapagliflozin at a given annual rate according to the data observed in DECLARE-TIMI 58 trial, and remained on placebo until the end of the time horizon or patient’s death. Additionally, patients discontinued dapagliflozin at an eGFR of 45 ml/min/1.73m2.
Population included and clinical efficacy and safety of treatments
The demographic characteristics and baseline modifiable risk factors of patients with T2DM were obtained from published data from the DECLARE-TIMI 58 trial [9, 17] DAPA-RWE Spain study [19] (Table 1).
The efficacy endpoints were the change in glycated hemoglobin (HbA1c), systolic blood pressure (SBP), body weight and eGFR (Table 2). The efficacy of each treatment on modifiable risk factors was applied in the first year, except for the reduction in eGFR that was applied annually. In subsequent years, the model assumed that the progression of HbA1c and SBP was similar to the data observed in the UKPDS study [10], while the progression of weight was considered to be -0.395 kg for dapagliflozin and -0.353 kg for placebo annually according to the DECLARE-TIMI 58 trial [9]. The annual incidence of AEs (diabetic ketoacidosis, urinary and genital tract infection, acute kidney damage and fractures) and severe hypoglycemia, and the discontinuation rate of each treatment from the DECLARE-TIMI 58 trial were included (Table 2) [9, 21].
Costs
According to the perspective used, only direct healthcare costs were included in the analysis. The costs identified were updated to 2021 values based on the healthcare component of the Spanish consumer price index (Table 3).
Pharmacological costs
Dapagliflozin acquisition cost was calculated from the retail price, including value added tax and applying the deduction according to Royal Decree Law 8/2010 (7.5%) [22]. The annual cost of dapagliflozin treatment was estimated at € 624.37 for the recommended dose of 10 mg/day [23].
Costs of T2DM complications
The costs of managing micro- and macrovascular complications in T2DM were differentiated in the year of incidence according to whether they were fatal or non-fatal events. In patients who survived, annual maintenance costs were considered for all subsequent years up to the end of the time horizon or patient’s death (Table 3). Costs were obtained from the Spanish Minimum Basic Data Set [24] and from published studies in the Spanish setting [25,26,27,28].
Costs of AEs, severe hypoglycemic events and treatment discontinuation
The costs of AEs included the costs associated with urinary tract infections, genital tract infections and fractures, and hospitalization costs for diabetic ketoacidosis and acute kidney damage [24]. The cost of managing urinary and genital tract infections included the cost of a primary care physician visit and treatment with amoxicillin [22, 29], while the cost managing fractures was calculated as the mean cost of a fracture of the hip and pelvis, forearm, and humerus [29].
In terms of hypoglycemic events, only the costs of severe hypoglycemic events were considered. These events were calculated from the unit cost of a severe event [30] and the number of events occurred in each cycle.
The cost of treatment discontinuation for dapagliflozin was also considered, assuming the cost of a primary care physician visit [29] (Table 3).
CKD-related costs
CKD-related costs were included as the model tracks eGFR progression. The annual cost of each disease stage (2-5) was calculated from Spanish studies [31,32,33] (Table 3).
Utilities
The impact of T2DM on health-related quality of life was assessed using utilities and was expressed as QALYs. The baseline utility was 0.800 and was estimated from the European Quality of Life-5 Dimensions questionnaire in an observational study of Spanish T2DM patients [34]. In addition, utility decrements associated with T2DM-related complications, AEs, hypoglycemic events, treatment discontinuation, CKD and body mass index were included (see Additional file 2). Utility values were applied additively and were obtained from published data [35,36,37,38,39,40,41,42] in other settings due to the lack of Spanish data.
Sensitivity analysis
Univariate sensitivity analyses were performed to evaluate the impact of the parameters on the results of the analysis and to validate their robustness. The parameters modified individually were time horizon (20 years and lifetime), discount rate (0% and 5%), mean baseline age (40 and 70 years), and mean baseline eGFR (70 ml/min/1.73m2). These sensitivity analyses were conducted to assess the use of dapagliflozin in different populations (young, older people, with greater renal impairment). When baseline age was varied, time horizon was also modified to simulate the costs and effects proportionally to the base case.
In addition, a probabilistic sensitivity analysis (PSA) was performed, in which the values of all parameters, except patient characteristics, were modified simultaneously in each model run. A cohort of 1,000 patients was simulated over 1,000 runs. A normal distribution was considered for baseline patient characteristics and treatment efficacy, a gamma distribution for costs, and a beta distribution for utilities and probabilities. The analysis assumed a willingness-to-pay (WTP) threshold of € 20,000/QALY gained for Spain [43].
Consolidated Health Economic Evaluation Reporting Standards checklist [44] was applied to ensure a proper reporting of the health economic evaluation (see Additional file 3).
Results
Main analysis
Treatment with dapagliflozin was more effective than placebo, resulting in 0.08 more QALYs per patient (10.96 vs. 10.88). Over a 30-year time horizon, dapagliflozin would prevent 17 macrovascular events (495 vs. 512) in a cohort of 1,000 patients, compared with placebo; 17 hospitalizations for heart failure (123 vs. 140), and 7 microvascular events (124 vs. 131).
The prevention of these complications was mainly thanks to a better disease control, with improvements in all modifiable risk factors (HbA1c, body weight, SBP, eGFR) compared with placebo [9] Additionally, dapagliflozin reduced the risk of complications, such as hospitalization for HF and myocardial infarction.
Cost analysis results show that the total cost per patient was € 56,984 with dapagliflozin and € 59,905 with placebo, saving € 2,921 per patient (Table 4). Therefore, the additional acquisition cost of dapagliflozin (€ 4,985) was fully offset by the lower cost of micro- and macrovascular events (€ -7,908) and severe hypoglycemic events (€ -4).
As a result, dapagliflozin was a dominant therapeutic alternative for the treatment of T2DM, resulting in higher effectiveness and lower overall associated costs than placebo.
Sensitivity analysis
The univariate sensitivity analysis confirmed the robustness of the main analysis. In all scenarios, dapagliflozin was a cost-effective therapeutic option for the treatment of T2DM, considering a WTP threshold of € 20,000/QALY gained (Table 4). A 20-year time horizon and a higher discount rate (5%) reduced slightly the effectiveness of dapagliflozin compared with placebo because long-term benefits of dapagliflozin were not fully captured.
The PSA showed that dapagliflozin was a dominant option compared with placebo in 84.2% of the simulations and was cost-effective in 92.1% of cases at a WTP threshold of € 20,000/QALY gained (Fig. 1).
Discussion
The present cost-effectiveness analysis of dapagliflozin based on the data from the DECLARE-TIMI 58 trial show that dapagliflozin is a dominant option compared with placebo in patients with T2DM who had or were at risk of atherosclerotic cardiovascular disease in Spain. Dapagliflozin resulted in increased effectiveness (0.08 QALY) and lower costs (€ -2,921) in the management of T2DM. Dapagliflozin had a beneficial effect on both glycemic control and the reduction of T2DM-related complications, including progression of CKD and hypoglycemic events.
Our findings are similar to those published in an economic evaluation of dapagliflozin performed in the UK, in which the Cardiff T2DM model was also adapted according to the survival results of the DECLARE-TIMI 58 trial [45]. In that study, dapagliflozin was a dominant alternative compared with placebo, resulting in 0.06 more QALYs and cost-savings of £ 2,552. These results were maintained in the subgroup analysis, which evaluated patients with established cardiovascular disease, multiple risk factors, and prior HF, and highlighted the potential of dapagliflozin to reduce the economic burden of T2DM and its associated complications [45].
In a literature review, two economic evaluations of dapagliflozin for the treatment of T2DM were identified in Spain [25, 46]. In one study, dapagliflozin was compared with DPP-4 inhibitors, both in combination with metformin. In line with our study, the results showed that dapagliflozin was a dominant alternative with higher effectiveness (0.019 QALYs) and lower total costs (€ -42) [25]. In the other study, the combination of dapagliflozin and insulin was compared with the combination of DPP-4 inhibitors and insulin, and insulin alone. Dapagliflozin in combination with insulin was a dominant option (0.168 QALYs; € -51) compared with DPP-4 inhibitors and insulin; and it was cost-effective with an ICER of € 2,159/QALY (0.698 QALY; € +1,508) compared with insulin alone [46]. Thus, dapagliflozin was a therapeutic alternative for intensification treatment in T2DM patients with uncontrolled glycemia, which has greater effectiveness than other available options (such as DPP-4 inhibitors and insulin) without a significant economic impact and even making cost savings.
A possible limitation of the present study is long-term extrapolation of data from short-term clinical trials to model disease progression throughout a patient’s lifetime, although this approach is common in most cost-effectiveness models. In addition, the incidence rate of macrovascular events, mortality and ESRD was estimated using the survival equations from the DECLARE-TIMI 58 trial, instead of established risk equations; and, the incidence rate of microvascular events was calculated based on the UKPDS study risk equations, due to the lack of data from the DECLARE-TIMI 58 trial. However, the incidence rate of events was modeled directly using data from the DECLARE-TIMI 58 trial without the need to use surrogate risk markers [9, 45]. Besides, the Cardiff T2DM model used to simulate the progression of T2DM in this analysis has been validated in previous studies as a tool for conducting economic evaluations of new technologies and making health policy decisions [13,14,15,16].
A further limitation is related to the patient characteristics used in the model. This analysis assumed that patient profile of the Spanish population with T2DM in clinical practice was similar to that of the patients in the DECLARE-TIMI 58 trial, but published evidence shows that around 38% and 51% of patients treated with dapagliflozin in clinical practice met the inclusion criteria for the DECLARE-TIMI 58 trial [19, 47]. However, univariate sensitivity analyses were carried out, in which baseline characteristics (age and eGFR) were modified, and a PSA were also performed to ensure the representativeness of T2DM patients who may be treated with dapagliflozin in real clinical practice. The results confirmed that dapagliflozin was a cost-effective therapeutic alternative. In addition, real-world evidence with dapagliflozin in other European countries confirmed the improvements in glycemic control and the reduction of cardiovascular and T2DM-related complications observed in the DECLARE-TIMI 58 trial [48,49,50,51].
Conclusions
In conclusion, this analysis suggests that dapagliflozin, as add-on therapy to SoC, is a cost-effective alternative compared with placebo for the treatment of T2DM in patients who had or were at risk of atherosclerotic cardiovascular disease in Spain. Dapagliflozin demonstrated to reduce T2DM-related complications and hypoglycemic events and therefore this study highlights its potential to minimize clinical and economic burden of T2DM.
Availability of data and materials
The datasets used and/or analysed during the current study are included in this published article.
Abbreviations
- AEs:
-
Adverse Events
- CKD:
-
Chronic Kidney Disease
- DM:
-
Diabetes Mellitus
- DPP-4:
-
Dipeptidyl Peptidase-4
- eGFR:
-
Estimated Glomerular Filtration Rate
- ESRD:
-
End-Stage Renal Disease
- Hb1Ac:
-
Glycated Hemoglobin
- HF:
-
Heart Failure
- ICER:
-
Incremental Cost-Effectiveness Ratio
- NHS:
-
National Health System
- PSA:
-
Probabilistic Sensitivity Analyses
- QALY:
-
Quality-Adjusted Life Year
- SBP:
-
Systolic Blood Pressure
- SoC:
-
Standard of Care
- T2DM:
-
Type 2 Diabetes Mellitus
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- WTP:
-
Willingness-To-Pay
References
Muñoz Grimaldo M. La enfermera de Primaria y la Diabetes. Guía de la RedGDPS. Epidemiología, prevención y criterios diagnósticos y de control. 2011. http://www.redgdps.org/la-enfermera-de-primaria-y-la-diabetes-20161003. Accessed 21 Jan 2021.
Crespo C, Brosa M, Soria-Juan A, Lopez-Alba A, López-Martínez N, Soria B. Direct cost of diabetes mellitus and its complications in Spain (SECCAID Study: Spain estimated cost Ciberdem-Cabimer in Diabetes). Avances en Diabetología. 2013;29:182–9.
Hidalgo A, Oliva J, Rubio M, Zozaya N, Villoro R, García S. Estudios de coste de la diabetes tipo 2: una revisión de la literatura. 2015. http://gesdoc.isciii.es/gesdoccontroller?action=download&id=26/05/2015-28ff538b32. Accessed 21 Jan 2021.
Ministerio de Sanidad Servicios Sociales e Igualdad. Estrategia en Diabetes del Sistema Nacional de Salud. Madrid; 2012.
Soriguer F, Goday A, Bosch-Comas A, Bordiú E, Calle-Pascual A, Carmena R, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es Study. Diabetologia. 2012;55:88–93.
Rojo-Martínez G, Valdés S, Soriguer F, Vendrell J, Urrutia I, Pérez V, et al. Incidence of diabetes mellitus in Spain as results of the nation-wide cohort di@bet.es study. Scientific Reports. 2020;10:2765.
Fundación redGDPS. Guía de diabetes tipo 2 para clínicos: Recomendaciones de la redGDPS. 2018.
Gomez-Peralta F, Escalada San Martín FJ, Menéndez Torre E, Mata Cases M, Ferrer García JC, Ezkurra Loiola P, et al. Recomendaciones de la Sociedad Española de Diabetes (SED) para el tratamiento farmacológico de la hiperglucemia en la diabetes tipo 2: Actualización 2018. Endocrinología, Diabetes y Nutrición. 2018;65:611–24.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. New England Journal of Medicine. 2019;380:347–57.
Clarke PM, Gray AM, Briggs A, Farmer AJ, Fenn P, Stevens RJ, et al. A model to estimate the lifetime health outcomes of patients with Type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia. 2004;47:1747–59.
Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM. UKPDS Outcomes Model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia. 2013;56:1925–33.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). The Lancet. 1998;352:837–53.
Palmer AJ. Computer Modeling of Diabetes and Its Complications: A Report on the Fifth Mount Hood Challenge Meeting. Value in Health. 2013;16:670–85.
McEwan P, Ward T, Bennett H, Bergenheim K. Validation of the UKPDS 82 risk equations within the Cardiff Diabetes Model. Cost Effectiveness and Resource Allocation. 2015;13:12.
McEwan P, Bennett H, Ward T, Bergenheim K. Refitting of the UKPDS 68 Risk Equations to Contemporary Routine Clinical Practice Data in the UK. PharmacoEconomics. 2015;33:149–61.
McEwan P, Peters JR, Bergenheim K, Currie CJ. Evaluation of the costs and outcomes from changes in risk factors in type 2 diabetes using the Cardiff stochastic simulation cost-utility model (DiabForecaster). Current Medical Research and Opinion. 2006;22:121–9.
Raz I, Mosenzon O, Bonaca MP, Cahn A, Kato ET, Silverman MG, et al. DECLARE-TIMI 58: Participants’ baseline characteristics. Diabetes, Obesity and Metabolism. 2018;20:1102–10.
Ortega Eslava A, Marín Gil R, Fraga Fuentes MD, López-Briz E, Puigventós Latorre F. Guía de evaluación económica e impacto presupuestario en los informes de evaluación de medicamentos. 2016.
Fadini GP, Tentolouris N, Caballero Mateos I, Bellido Castañeda V, Morales Portillo C. A Multinational Real-World Study on the Clinical Characteristics of Patients with Type 2 Diabetes Initiating Dapagliflozin in Southern Europe. Diabetes Therapy. 2020;11:423–36.
Franch Nadal J, Mata Cases M, Mauricio Puente D. Epidemiología y control clínico de la diabetes mellitus tipo 2 y sus comorbilidades en España (estudio e-Control). Medicina Clínica. 2016;147:1–7.
Mosenzon O, Dwyer J, Cahn A, Goodrich E, Murphy S, Rozenberg A, et al. TH-PO1205: Prevention of chronic kidney disease with dapagliflozin: analysis of the DECLARE-TIMI 58 trial. In: ASN Kidney week 2019. 2019.
Consejo General de Colegios Oficiales de Farmacéuticos. Portal Farma. BotPLUS. 2021. https://botplusweb.portalfarma.com/botplus.aspx.
World Health Organization. ATC/DDD Index 2021. WHO Collaborating Centre for Drug Statistics Methodology. 2021. https://www.whocc.no/atc_ddd_index/. Accessed 25 Jan 2021.
Ministerio de Sanidad Consumo y Bienestar Social. Conjunto Mínimo Básico de Datos (CMBD). Registro de Atención Especializada. 2021. http://pestadistico.inteligenciadegestion.msssi.es/. Accessed 26 Jan 2021.
Abad Paniagua EJ, Casado Escribano P, Fernández Rodriguez JM, Morales Escobar FJ, Betegón Nicolás L, Sánchez-Covisa J, et al. Análisis de coste-efectividad de dapagliflozina en comparación con los inhibidores de la DPP4 y otros antidiabéticos orales en el tratamiento de la diabetes mellitus tipo 2 en España. Atención Primaria. 2015;47:505–13.
Abejón Arroyo A, Álaverz Vázquez J, Blasco García C, Bermejo Martínez M, López Casanova P, Cuesta Cuesta J, et al. Coste-Efectividad de un apósito de espuma de poliuretano con TLC-NOSF. Estudio en el tratamiento de las úlceras venosas de pierna. Revista Rol de Enfermería. 2012;35:747–52.
Ministerio de Sanidad Servicios Sociales e Igualdad. Documento Marco sobre Enfermedad Renal Crónica (ERC) dentro de la Estrategia de Abordaje a la Cronicidad en el SNS. 2015.
Cabellero Alcalde C, Calleja Hernández M, Escoda Ruiz L, Espasa Triquell N, Estévez Lucas J, Fraga Rodríguez G, et al. Libro Blanco de la Poliquistosis Renal Autosómica Dominante (PQRAD) en España. 2nd edition. 2016.
Gisbert R, Brosa M. Base de datos de costes sanitarios y ratios coste-efectividad españoles: eSalud. Barelona, Spain; 2020.
Parekh W, Hoskins N, Baker-Knight J, Ramirez de Arellano A, Mezquita Raya P. The Economic Burden of Insulin-Related Hypoglycemia in Spain. Diabetes Therapy. 2017;8:899–913.
Pons R, Torregrosa E, Hernández-Jaras J, García H, Rius A, Calvo C, et al. El coste del tratamiento farmacológico en la enfermedad renal crónica. Nefrología. 2006;26:291–414.
Darbà J, Marsà A. Chronic kidney disease in Spain: analysis of patient characteristics, incidence and direct medical costs (2011–2017). Journal of Medical Economics. 2020;:1–7.
Lorenzo-Sellares V, Pedrosa MI, Santana-Expósito B, García-González Z, Barroso-Montesinos M. Cost analysis and sociocultural profile of kidney patients. Impact of the treatment method. Nefrologia. 2014;34:458–68.
DePablos-Velasco P, Salguero-Chaves E, Mata-Poyo J, DeRivas-Otero B, García-Sánchez R, Viguera-Ester P. Calidad de vida y satisfacción con el tratamiento de sujetos con diabetes tipo 2: resultados en España del estudio PANORAMA. Endocrinología y Nutrición. 2014;61:18–26.
Sullivan PW, Slejko JF, Sculpher MJ, Ghushchyan V. Catalogue of EQ-5D Scores for the United Kingdom. Medical Decision Making. 2011;31:800–4.
Beaudet A, Clegg J, Thuresson P-O, Lloyd A, McEwan P. Review of Utility Values for Economic Modeling in Type 2 Diabetes. Value in Health. 2014;17:462–70.
Clarke P, Gray A, Holman R. Estimating Utility Values for Health States of Type 2 Diabetic Patients Using the EQ-5D (UKPDS 62). Medical Decision Making. 2002;22:340–9.
Barry HC, Ebell MH, Hickner J. Evaluation of suspected urinary tract infection in ambulatory women: a cost-utility analysis of office-based strategies. The Journal of family practice. 1997;44:49–60.
Gorodetskaya I, Zenios S, Mcculloch CE, Bostrom A, Hsu C-Y, Bindman AB, et al. Health-related quality of life and estimates of utility in chronic kidney disease. Kidney International. 2005;68:2801–8.
Lane S, Levy AR, Mukherjee J, Sambrook J, Tildesley H. The impact on utilities of differences in body weight among Canadian patients with type 2 diabetes. Current Medical Research and Opinion. 2014;30:1267–73.
Currie CJ, McEwan P, Peters JR, Patel TC, Dixon S. The Routine Collation of Health Outcomes Data from Hospital Treated Subjects in the Health Outcomes Data Repository (HODaR): Descriptive Analysis from the First 20,000 Subjects. Value in Health. 2005;8:581–90.
Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Economics. 2005;14:217–30.
Vallejo-Torres L, García-Lorenzo B, Rivero-Arias O, Pinto-Prades J, Serrano-Aguilar P. Disposición a pagar de la sociedad española por un Año de Vida Ajustado por Calidad. Santa Cruz de Tenerife: Servicio Canario de la Salud; 2016.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS) Statement. Value in Health. 2013;16:e1–5.
McEwan P, Morgan AR, Boyce R, Bergenheim K, Gause-Nilsson IAM, Bhatt DL, et al. The cost‐effectiveness of dapagliflozin in treating high‐risk patients with type 2 diabetes mellitus: An economic evaluation using data from the DECLARE‐TIMI 58 trial. Diabetes, Obesity and Metabolism. 2020. https://doi.org/10.1111/dom.14308.
Sánchez-Covisa J, Capel M, Schmidt R, Charokopou M, Verheggen BG. The Cost-Effectiveness of Dapagliflozin In Combination With Insulin for the Treatment of Type 2 Diabetes Mellitus (T2dm) In Spain. Value in Health. 2014;17:A350.
Canivell S, Mata-Cases M, Vlacho B, Gratacòs M, Real J, Mauricio D, et al. How Many Patients with Type 2 Diabetes Meet the Inclusion Criteria of the Cardiovascular Outcome Trials with SGLT2 Inhibitors? Estimations from a Population Database in a Mediterranean Area. Journal of Diabetes Research. 2019;2019:1–9.
Norhammar A, Bodegard J, Nyström T, Thuresson M, Rikner K, Nathanson D, et al. Dapagliflozin vs non-SGLT‐2i treatment is associated with lower healthcare costs in type 2 diabetes patients similar to participants in the DECLARE‐TIMI 58 trial: A nationwide observational study. Diabetes, Obesity and Metabolism. 2019;21:2651–9.
Morieri ML, Consoli A, Sesti G, Purrello F, Avogaro A, Fadini GP. Comparative effectiveness of dapagliflozin vs DPP-4 inhibitors on a composite endpoint of HbA1c, body weight and blood pressure reduction in the real world. Diabetes/Metabolism Research and Reviews. 2021;37.
McGurnaghan SJ, Brierley L, Caparrotta TM, McKeigue PM, Blackbourn LAK, Wild SH, et al. The effect of dapagliflozin on glycaemic control and other cardiovascular disease risk factors in type 2 diabetes mellitus: a real-world observational study. Diabetologia. 2019;62:621–32.
Persson F, Nyström T, Jørgensen ME, Carstensen B, Gulseth HL, Thuresson M, et al. Dapagliflozin is associated with lower risk of cardiovascular events and all-cause mortality in people with type 2 diabetes (CVD‐REAL Nordic) when compared with dipeptidyl peptidase‐4 inhibitor therapy: A multinational observational study. Diabetes, Obesity and Metabolism. 2018;20:344–51.
Acknowledgements
Not applicable.
Funding
This study was funded by AstraZeneca Spain. AstraZeneca Spain designed and collected data for the economic evaluation; however, they had no role in data analysis, interpretation of results, or preparation of manuscript.
Author information
Authors and Affiliations
Contributions
FP and EP performed the economic evaluation and drafted the manuscript. CE and CM provided clinical expert opinion on the disease area. All authors discussed the results and commented on the manuscript at all stages. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. Research ethics was not required as the study did not involve human subjects or materials.
Consent for publication
Not applicable.
Competing interests
MC and SS are employed by AstraZeneca Spain. FP and EP are employed by Oblikue Consulting, a consultant company specialized in economic evaluations of health interventions and received financial support from AstraZeneca Spain for the development of this study. CE and CM received an honorarium from the sponsor and participated as independent consultants.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Validation of the results of the model over a time horizon of 4.2 years with the DECLARE-TIMI 58 trial.
Additional file 2:
Utilities and utility decrements used in the model.
Additional file 3:
CHEERS checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Escobar, C., Morales, C., Capel, M. et al. Cost-effectiveness analysis of dapagliflozin for the treatment of type 2 diabetes mellitus in Spain: results of the DECLARE-TIMI 58 study. BMC Health Serv Res 22, 217 (2022). https://doi.org/10.1186/s12913-022-07567-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-07567-5