Abstract
Background
This systematic literature review explored the general characteristics, validation, and reliability of pediatric simulation-based education (P-SBE).
Methods
A literature search was conducted between May 23 and 28 using the PRISMA guidelines, which covered databases such as MEDLINE, EMBASE, CINAHL, and Cochrane Library. In the third selection process, the original texts of 142 studies were selected, and 98 documents were included in the final content analysis.
Results
A total of 109 papers have been published in the ten years since 2011. Most of the study designs were experimental studies, including RCT with 76 articles. Among the typologies of simulation, advanced patient simulation was the most common (92), and high-fidelity simulation was the second most common (75). There were 29 compatibility levels and professional levels, with 59 scenarios related to emergency interventions and 19 scenarios related to communication feasibility and decision making. Regarding the effect variable, 65 studies confirmed that skills were the most common. However, validity of the scenarios and effect variables was not verified in 56.1% and 67.3% of studies, respectively.
Conclusion
Based on these findings, simulation based-education (SBE) is an effective educational method that can improve the proficiency and competence of medical professionals dealing with child. Learning through simulation provides an immersive environment in which learners interact with the presented patient scenario and make decisions, actively learning the attitudes, knowledge, and skills necessary for medical providers. In the future, it is expected that such research on SBE will be actively followed up and verified for its validity and reliability.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Rationale for the study
Simulation-based education (SBE) is not a technology, but a learner-centered pedagogical method based on learning theories [1]. The greatest benefit of SBE is that it enables repeated training in a safe environment resembling an actual hospital setting [2]. For example, students can experience cases in which they cannot be directly involved in a clinical setting, such as providing care for a psychiatric patient exhibiting dangerous behaviors or end-of-life care for patients and their families [1]. Moreover, training that requires a more realistic setting, such as dissection, can be performed using immersive virtual reality [3]. As shown here, SBE can be designed with the desired scenario contents based on the learning objectives, and patient information and simulators can be varied to provide different SBE [1].
Simulation-based education helps nursing students to establish their professional identity by experiencing the roles of a nurse in advance [4], and question and-answer sessions and discussions with the instructor during debriefing after the training allows students to engage in self-reflection, through which they can integrate their learned materials and translate them into practice [5]. Due to these benefits, SBE supplements clinical practicum across all topics. Recently, it’s especially advised for situations where students can’t directly interact, like pediatric vaccinations, asthma treatments, and mother-infant cases [1].
As a result of the coronavirus disease 2019 (COVID-19) pandemic that struck the world in 2019, clinical practicum was either suspended or stopped for patient and student safety, and students expressed anxiety about potentially contracting the infection from patients or other students during clinical practicum [6], further highlighting the need for SBE. Moreover, pediatric nursing clinical practicum is very challenging in the Republic of Korea (ROK) compared with other clinical practicums. The ROK is one of the countries with the lowest fertility rates, and it has the most quickly declining cumulative birth rate and total fertility rate among 37 organization for economic cooperation and development (OECD) countries, with an average annual drop of 3.1%. In addition, the number of neonates has dropped dramatically from 490,000 to 2012 to 260,000 in 2021 [7]. Moreover, the number of high-risk neonates vulnerable to infection and injury is on the rise, from 18,232 to 1995 to 30,462 in 2015 [7], which further hinders students from encountering divers even if clinical practicum courses are offered.
A systematic review of studies that conducted a cost analysis for SBE reported that the most common topic—following surgery cases—was pediatrics and obstetrics and gynecology, and that most studies were conducted in low-income countries, with common topics being neonatal and maternal health care, such as “Helping Babies Breathe” (HBB) and “Essential Newborn Care” (ENC) [2]. As shown here, pediatric health is a very important topic of SBE not only in countries with low fertility rates but also in low-income countries. Providing pediatric nursing clinical practicum is very challenging due to the declining number of newborns, increasing incidence of high-risk births, and high cost associated with SBE.
To address these issues, a growing number of studies have evaluated the effects of SBE; however, the types of SBE studied vary widely, and the validity and reliability of scenarios and contents of SBE have not been adequately evaluated. Furthermore, diverse outcome measures have been used and standardized instruments are lacking [4, 8, 9]. The validity of the simulation was described as the degree to which the simulation accurately represented the target task, and the reliability of the simulation was described as the degree to which simulation education was measured using the same method each time the same participants received education under the same conditions [10]. Because simulation is an educational method that enables nursing educators to facilitate and assess learners’ clinical competencies [1], educators must develop valid and reliable scenarios and assess learners using standardized instruments.
There are several types of simulators available, including standard patients, high-fidelity simulators, low-fidelity simulators, and partial task simulators. Instructors choose the type of simulator based on the objectives of SBE. Consequently, the use of an ineffective simulator may curtail the effectiveness of education [1].
As shown here, past systematic reviews of studies on SBE have primarily conducted technical analyses of educational methods and target populations, with a lack of systematic reviews on the contents of SBE. In this context, we conducted a systematic review to examine the characteristics of pediatric simulation-based education (P-SBE) and evaluate the validity and reliability of the development process. The findings of this study will shed light on the direction of future SBE programs and interventions and establish criteria for validity and reliability evaluations of simulation scenarios and programs.
Research questions
This study was a systematic review of past studies that have developed and evaluated the effects of P-SBE. The findings of this study will be used as criteria for evaluating the validity and reliability of future P-SBE. The specific research questions were as follows:
-
1.
Review the characteristics of studies that developed and evaluated the effects of P-SBE.
-
2.
Identify the characteristics of scenarios used in P-SBE.
-
3.
Evaluate the validity and reliability of the process of developing P-SBE.
-
4.
Evaluate the validity and reliability of instruments used to assess the effects of P-SBE.
Methods
Study design
This study conducted a systematic review of P-SBE, specifically examining the general characteristics of the studies, topics of education, simulation methods, reliability and validity of simulation, and dependent variables. The key question selection, literature selection based on inclusion and exclusion criteria, data extraction, setting of scope of literature search and search databases, quality appraisal, and risk of bias assessment were performed in accordance with the Preferred Reporting Items of Systemic Reviews and Meta-Analysis (PRISMA) 2020 statement [11] and 2022 Cochrane Handbook for Systematic Reviews of Interventions version 6.3 [12], and data were analyzed. We classified the characteristics of literature based on typology, referencing the definition of “Simulation Typologies/Modalities” provided by Palaganas et al. in 2020 [13].
Key questions and selection criteria
The key questions of this study were: “What is the construction of P-SBE?” and “What aspects are assessed in P-SBE?”. The specific inclusion criteria were as follows:1) studies that developed a simulation program or scenario, 2) pediatric scenarios, and 3) health and health care-related scenarios (not necessarily in clinical settings, but including events such as traffic accidents, bee stings, bicycle accidents, daily life shocks, etc., these criteria were included in the third round of literature screening). The exclusion criteria were as follows:1) studies on non-human simulations (even if they are related to pediatrics, studies about the development of simulators, etc., were excluded), 2) non-pediatric scenarios, and 3) studies on non-human simulations (even if they are related to pediatrics, studies about the development of simulators, etc., were excluded). The search strategy was established based on the PICO-SD framework for non-Korean databases: “(simulat* or scenario*) and (pediatric or child or children or baby or newborn or infant or kid*) and (valid* or reliab*).
Literature search and selection process
Two researchers independently performed a literature search. The search was conducted from May 23, 2022, to May 28, 2022. The MEDLINE, EMBASE, CINAHL, and Cochrane Library databases were selected according to the PRISMA statement. An advanced search was performed based on the participants, intervention, comparison, outcome, and study design (PICO-SD) framework. In addition, a search was performed using Google Scholar to include as many gray articles as possible.
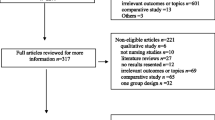
The criteria for the initial screening were set according to the PICO-SD framework. We did not define a specific participant population and included healthcare providers, nurses, and nursing students. As for the intervention, all P-SBE programs were included. The outcome variables were not specified. For the study design, we included all studies that observed effective outcomes after administering an SBE program, and studies that presented data for the validity and reliability of the scenario and instruments. A total of 1,309 studies were selected during the initial screening and 764 duplicates were excluded. In the second round of screening, the titles and abstracts of 545 studies were independently reviewed by three researchers based on the PCIO-SD criteria. In total, 292 studies were excluded. In the third round of screening, the full texts of the selected studies were obtained, and full texts of 253 studies were available. Of these, 111 studies did not meet the inclusion criteria and were excluded. From the resulting 142 studies, 44 were excluded from the content analysis because they were proceedings and did not show the details of the scenarios. Thus, 98 studies were included in the content analysis. Each researcher independently evaluated the quality of the papers using the Mixed Methods Appraisal Tool (MMAT), 2018 [14]. Only papers with moderate-to high-quality ratings were included in the review. Any disagreements among the researchers during this process were resolved by discussion. If the selected studies did not state the detailed study methodology, the researchers described it upon discussion (Fig. 1).
Data analysis
The 98 included studies were written as case reports, and qualitative analysis was performed using Excel 2016 software. The case reports contained information about general characteristics (authors, year, title, and country), study characteristics (study design, participant characteristics, simulator type, scenario topic, scenario reliability, and validity), and outcome characteristics (dependent variables, instruments used to measure dependent variables, and reliability and validity of dependent variables).
Study results
Characteristics of the studies
Table 1 presents the general characteristics of the included studies. A total of 142 studies pertinent to P-SBE were identified. Fifteen (10.6%) were published between 2001 and 2010, and 109 (76.8%) were published in the subsequent ten years, showing a more than seven-fold increase. The greatest number of studies were conducted in the United States (n = 62, 43.7%), followed by Canada (n = 17, 12.0%). Experimental studies, including randomized controlled trials (RCTs), were the most common (n = 76, 53.5%), followed by developmental studies, including simulation development (n = 58, 40.85%). According to simulation typology, advanced patient simulation was the most common (n = 92, 64.8%). Most studies used high-fidelity simulation only (n = 75, 52.8%), followed by video-based simulation, and four studies used VR simulation.
Analysis of simulation scenario contents
A total of 98 studies were included in the analysis of the P-SBE scenario contents (Table 2). The most common target population of P-SBE was medical staff (n = 44, 44.9%), more specifically, there were 37 (37.8%) studies on medical students, medical residents, or medical fellows and seven (7.1%) studies on medical doctors or medical experts. Of the studies conducted on nursing staff, eight (8.2%) studies were conducted on nursing students, and three (3.1%) studies were conducted on registered nurses or experts. Four (4.1%) studies were conducted on children or students, and three (3.1%) studies were conducted on parents. The most common number of scenarios included in the analysis software was one (n = 49, 50.0%), followed by four (n = 13, 13.3%). The proficiency levels were competency (n = 29, 29.6%), proficient (n = 29, 29.6%), and expert (n = 10, 10.2%). Scenario contents included emergency intervention (n = 59, 60.2%), communication ability and decision-making (n = 19, 19.39%), and protection and safety (n = 17, 17.35%). Specific topics included pediatric rescue (n = 37, 37.8%), neonatal rescue (n = 11, 11.2%), and airway management (n = 8, 8.2%). Among the programs developed for children, two studies developed a simulation to enhance the decision-making ability of children with autism spectrum disorder (ASD) [15, 16], and programs developed for students targeted to train rescue competencies [17] and enhance decision-making ability in relation to cigarette smoking [18]. Seventy-two (73.5%) studies had self-developmental scenarios, and 23 (23.5%) had already been published. In terms of validity and reliability evaluation, 48 studies (49.0%) did not test validity, and 55 studies (56.1%) did not test reliability (Table 2). The most common type of validity tested was content validity (n = 10, 10.2%) and the most common type of reliability tested was inter-rater reliability (n = 10, 10.2%) (Table 3).
Outcome variables of simulation program
Of the studies that used one or more outcome variables, most (n = 65, 66.3%) used the skill category as the outcome variable, namely skills, performance, assessment, and communication skills. Twenty-six (26.5%) studies used the attitude category as the outcome variable, namely attitude, confidence, satisfaction, and stress. Seventeen (17.3%) studies have examined this knowledge. Fifty-six studies (57.1%) used one outcome variable and 31 (31.6%) used more than one outcome variable. Sixty-six (67.3%) studies did not test validity, while 50 (51.0%) did not test reliability (Tables 4 and 5).
Discussion
SBE is recognized as an important field in health education [19], and its technology and field are being advanced and expanded at an astonishing pace [19]. In particular, the need for P-SBE is growing because pediatric patients require highly proficient skills, despite limited access by students in clinical settings [20]. In the present study, we conducted a systematic review to identify the characteristics of the P-SBE programs. We also examined the methods of validity and reliability testing in studies that developed the P-SBE programs. We aim to describe these topics based on the general characteristics of the research for discussion.
Navigating through the vast literature, a total of 142 studies on P-SBE were identified. While research in this field was limited prior to 2004 (n = 3, 2.1%), substantial research has been conducted from 2004 to the present (n = 139, 97.9%). In particular, there has been an increase in up to 20 studies since 2011. Simulations were introduced in medical and nursing education in the 1960s when mannequins that enable training of mouth-to-mouth breathing were developed; owing to advances in state-of-the-art technology and artificial intelligence, types of simulations, fields of application, and simulation scenarios have become increasingly similar to real-world situations, allowing for the achievement of special educational objectives [21]. Moreover, according to the IOM recommendation that education for healthcare providers must comprise evidence-based content and that new technology, such as team-based simulations, should be incorporated into the curriculum to provide safer and more effective treatment [22], SBE strategies are anticipated to be further expanded and advanced in the coming years.
Next, by country, there was the most active research in developed countries, including the United States, with 62 (43.7%) studies published in the United States, 17 (12.0%) studies in Canada, and 10 (7.0%) studies in the United Kingdom. This may be attributable to the fact that while national leaders, organizations, and accreditation bodies have spared no support from educators of healthcare providers in transforming the present and have served a central role in simulation education, SBE has advanced primarily around organizations such as the Society for Simulation in Healthcare (SSH) and International Nursing Association for Clinical Simulation and Learning (INACSL), which mostly includes developed countries [23]. In the future, education systems that provide P-SBE to healthcare providers should be expanded to countries with poor supportive networks.
Based on the study design, the most common type of study design was experimental, including RCTs (n = 33, 23.2%) and quasi-experimental studies (n = 18, 12.7%). The prominence of experimental designs emphasizes the scientific accuracy and commitment of the research community in producing evidence-based results in the field of P-SBE. The focus of current research mainly on the development and evaluation of simulation programs is a positive sign. This trend indicates the academic community values ensuring that P-SBE programs are not only innovative but also effective in delivering essential skills to healthcare providers. Even though such designs have been widely adopted, there is a need to consider mixed methods approaches in the future, capable of offering both quantitative data and deeper qualitative insights into learners’ experiences and perceptions. Additional research is necessary to assess not just the effectiveness but also the feasibility, accessibility, and scalability of P-SBE across diverse environments.
By simulation type, 92 studies used an advanced patient simulator and 52.5% used only a high-fidelity simulator. Next, 30 (32.6%) studies used computer-based training and 17 (20.2%) them used video-based simulations. Ten studies used a standardized patient (SP)/participant, and nine (6.3%) of them used an SP. This is because the key to simulation education for healthcare providers, which is defined as skills training, learning, assessment, testing or system, or platform for gaining an understanding of human behavior in a situation or environment that allows them to experience real-world cases [24], is how well it reflects reality, and high-fidelity simulators provide modifiable, realistic responses to the situation and learners’ input. The current level of technology allows high-fidelity simulators to precisely mimic human body functions and provide realistic responses, such as heart and lung sounds, chest movements, and detectable pulses, enabling learners to be integrated into patient scenarios that require their clinical judgment and practice proficiency [25]. Research utilizing VR or other games is rare. Such technology reflects real-world situations and can detect learners’ real-time responses to changes in the situation, but it is rarely used. In particular, the fact that 17 out of 30 (56.7%) studies on computer-based training used video-based simulations shows that this area requires further development.
The target audience for the scenario’s content could be determined through the analysis of the scenario itself. A total of 98 studies were included in the analysis of the content of P-SBE scenarios in Korea and other countries. Of the 44 studies that developed programs for medical staff, 37 (37.8%) were conducted with students, residents, and fellows. Thirteen (13.3%) studies were conducted on medical staff, nursing staff, and other staff, and 12 (12.2%) studies on other staff, including paramedics, lifeguards, and respiratory therapists. Several studies have developed programs for interdisciplinary teams. The core principle of healthcare providers is “First do not harm” [26]. Nevertheless, it has been reported that at least 44,000 (probably 98,000) patients die each year due to preventable errors by healthcare providers [27]. Simulation training enables the development and maintenance of skills in patient safety and quality management of medical services, and can help to acquire non-technical skills development and knowledge, such as communication skills and critical thinking, and to understand conceptual relationships [28] In addition, developing competencies related to interprofessional practice, including effective communication skills and teamwork, was recognized as essential to maximize patient outcomes and improve patient safety [29], confirming that the program was being developed for the team.
In terms of the five-stage model of skill acquisition [30], the most common stage targeted by SBE programs was competency (n = 29, 29.6%) and proficient (n = 29, 29.6%), followed by advanced beginner (n = 21, 21.4%), expert (n = 10, 10.2%), and novice (n = 9, 9.2%). In the 17th century, Dreyfus brothers developed a five-stage model to describe how individuals acquire skills and how experts master them. In other words, more studies have developed simulations designed to promote mastery among individuals at the competent or proficient level, which requires highly advanced and complex skills and experiences in more complex and challenging situations, as opposed to simulations targeting novices learning simple skills.
Subsequently, the scenarios were categorized based on their content. The most common scenario topic was emergency intervention (n = 59, 60.3%), and of these studies, there were 37 studies on pediatric rescue, 11 on neonatal rescue, and 8 on airway management. Another scenario was communication ability and decision making (n = 19, 22.4%), and the most common topic in this category was critical decisions (n = 13). This is in line with the Institute of Medicine (IOM) recommendations that healthcare providers are required to make accurate and critical decisions within a few seconds, even amid incomplete and inaccurate information; for these reasons, they must keep abreast with technological advances and collaborate with other professionals to rescue patients with complex morbidities [27]. Among programs targeting children, two studies developed a simulation program to enhance the decision-making ability of children with ASD, and programs targeting students included programs on resuscitation and decision-making ability during smoking education. These results show that SBE programs for children aim to improve their decision-making abilities. This is because simulation, an adaptive educational technology, provides an immersive environment in which students can interact with a given patient scenario and make their own decisions, through which they gain insight into their decision-making ability [31].
Regarding the reliability and validity of the scenarios, 30 studies (30.6%) tested the validity and 23 (23.5%) tested the reliability of the scenarios. In other words, there were still many studies that did not validate their findings despite the requirement for studies to be published to include evidence for evaluation or intervention, method of realization, reliability and validity, and educational outcomes to enhance the quality of evidence in medical education [32]. Reliability refers to the degree to which consistent measurements are obtained from the same study population. Validity refers to the degree to which something measures what it intends to measure. These crucial concepts underscore the need for more research to undertake such validation processes and reinforce their results, ensuring their applicability as trustworthy studies in a more effective manner.
Finally, in terms of the outcome variables used in the included studies, skills were the most common (n = 28, 28.6%), followed by performance (n = 24, 24.5%), knowledge (n = 17, 17.3%), and confidence (attitude) (n = 12, 12.2%). These results are in line with the recommendations of the (WHO) recommendations to develop standards and guidelines for simulation-based activities and implement simulation-based activities to accelerate the learning process and provide an opportunity for students and professionals to develop their skills and competencies [33].
In our systematic review, we examined the characteristics and development trends of P-SBE. Research in this domain was limited before 2004 but has witnessed significant growth post-2010. We observed that many P-SBE programs utilize high-fidelity simulators and team-based simulations, with emergency interventions being the primary educational topic to nurture rescue competencies. Most of this research has been conducted in developed countries like the United States, Canada, and the United Kingdom. While our results confirm the considerable advancement in P-SBE, many studies have not critically evaluated their validity and reliability. There’s a pressing need for an international protocol for the development of P-SBE, alongside rigorous validation and reliability testing. Furthermore, incorporating virtual reality technology could enhance the learning experience. It’s noteworthy to mention the limitations of our review: potential publication bias due to the focus on published papers, and the exclusion of scenarios where content specifics were not provided.
Conclusion
SBE has become indispensable owing to strengthened patient rights and the growing importance of patient safety. SBE is an educational method that enables pediatric healthcare staff to effectively improve their proficiency and competencies. It provides an immersive environment in which learners can interact with the given patient case scenario and make decisions, and owing to such benefits, it is actively utilized to train attitude, knowledge, and skills in health care providers and other staff. We hope that studies continue to follow up on these programs and evaluate their validity and reliability. Furthermore, there is a need for instruments that enable the categorization of scenarios and simulations based on the objective and learner’s current level and assess their competencies by level.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Aebersold M. Simulation-based learning: no longer a novelty in undergraduate education. Online J Issues Nurs. 2018;23(2):1. https://doi.org/10.3912/OJIN.Vol23No02PPT39.
Hippe DS, Umoren RA, McGee A, Bucher SL, Bresnahan BW. A targeted systematic review of cost analyses for implementation of simulation-based education in healthcare. SAGE Open Med. 2020;8:2050312120913451. : 10.1177/2050312120913451, PMID 32231781.
Hamrol A, Górski F, Grajewski D, Zawadzki P. Virtual 3D atlas of a human body–development of an educational medical software application. Procedia Comput Sci. 2013;25:302–14. https://doi.org/10.1016/j.procs.2013.11.036.
Handeland JA, Prinz A, Ekra EMR, Fossum M. The role of manikins in nursing students’ learning: a systematic review and thematic metasynthesis. Nurse Educ Today. 2021;98:104661. https://doi.org/10.1016/j.nedt.2020.104661. PMID 33298327.
Jeffries PR, Rodgers B, Adamson K. NLN Jeffries simulation theory: brief narrative description. Nurs Educ Perspect. 2015;36(5):292–3. https://doi.org/10.5480/1536-5026-36.5.292. PMID 26521496.
Lim SH. Content analysis on online non-face-to-face adult nursing practice experienced by graduating nursing students in the ontact era. J Korea Acad-Ind Coop Soc. 2021;22(4):195–205.
KOSIS. ; 2021. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_2KAA207_OECD. Accessed on 27 Jan 2023.
Kim J, Park JH, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016;16(1):152. https://doi.org/10.1186/s12909-016-0672-7. PMID 27215280.
Huang J, Tang Y, Tang J, Shi J, Wang H, Xiong T, et al. Educational efficacy of high-fidelity simulation in neonatal resuscitation training: a systematic review and meta-analysis. BMC Med Educ. 2019;19(1):323. https://doi.org/10.1186/s12909-019-1763-z. PMID 31464614.
Lopreiato JO. Healthcare simulation dictionary 2016. Rockville, MD: Agency for Healthcare Research and Quality; 2016.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. https://doi.org/10.1136/bmj.n160. PMID 33781993.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al. Cochrane; updated 2022 Feb [internet]. Cochrane handbook for systematic reviews of interventions. version 6.3 [cited Mar 22 2022]. Available from: http://www.training.cochrane.org/handbook.
Palaganas JC, Ulrich BT, Mancini MEB. Mastering simulation: a handbook for success. Sigma Theta Tau; 2020.
Hong QN, Fabreques S, Bartlett, Boardman F, Cargo M, Dagenais P, et al. The mixed methods appraisal tool (MMAT). Version 2018 for information professionals and researchers. Educ Inf. 2018;34(4):285–91.
Russo-Ponsaran N, McKown C, Johnson J, Russo J, Crossman J, Reife I. Virtual environment for social information processing: assessment of children with and without autism spectrum disorders. Autism Res. 2018;11(2):305–17. https://doi.org/10.1002/aur.1889. PMID 29125691.
Wallace S, Parsons S, Westbury A, White K, White K, Bailey A. Sense of presence and atypical social judgments in immersive virtual environments. Responses of adolescents with autism Spectrum Disorders. Autism. 2010;14(3):199–213. doi: 10.1177/1362361310363283, PMID 20484000.
Khorram-Manesh A, Berlin J, Roseke LL, Aremyr J, Sörensson J, Carlström E. Emergency management and preparedness training for youth (EMPTY): the results of the first swedish pilot study. Disaster Med Public Health Prep. 2018;12(6):685–88. https://doi.org/10.1017/dmp.2017.144. PMID 29446341.
Larsen H, Salemink E, Grond I, Wiers RW, Anderson KG. Validation of a contextualized assessment of smoking behaviour in students. Addict (Abingdon Engl). 2018;113(5):907 – 13. https://doi.org/10.1111/add.14133, PMID 29232482.
Forstrønen A, Johnsgaard T, Brattebø G, Reime MH. Developing facilitator competence in scenario-based medical simulation: presentation and evaluation of a train the trainer course in Bergen, Norway. Nurse Educ Pract. 2020;47:102840. https://doi.org/10.1016/j.nepr.2020.102840, PMID 32745955.
Joseph O. Simulation-based medical education in pediatrics. Acad Pediatr. 2015;15(2):134–042.
Bhandary SP, Lipps JA, Ramadan ME, Jenkins KD, Stoud JM, Papadimos TJ. Scenario development strategies and process for simulation-based education in anesthesiology. Int J Acad Med. 2021;3(1):72–7.
Institute of Medicine. (2011). The future of nursing: Leading change, advancing health. Washington, DC: The National Academies Press. Retrieved from http://www.nationalacademies.org/hmd/Reports/2010/The-Futre-of-Nursing-Leading-Change-Advancing-Health.aspx. Accessed on 27 Jan 2023.
Sittner BJ, Aebersold ML, Paige JB, Graham LL, Schram AP, Decker SI, et al. INACSL Standards of best practice for Simulation: past, Present, and Future. Nurs Educ Perspect. 2015;36(5):294–8. https://doi.org/10.5480/15-1670.
SSH. (Society for Simulation in Healthcare). Healthcare simulation dictionary.
Lioce L, Maddux G, Goddard N, Fogle I, Gunter S, Schroer B. Application of 3D printing in the development of training simulations for nursing students. International Workshop on Innovative Simulation for Healthcare; 2020. p. 7–12. CAL-TEK Srl. https://doi.org/10.46354/i3m.2020.iwish.002.
Smith CM. Origin and uses of primum non nocere—above all, do no harm! J Clin Pharmacol. 2005;45(4):371–7. https://doi.org/10.1177/0091270004273680. PMID 15778417.
Institute of Medicine. To err is human: building a safer health system, Washington DC. The National Academies Press; 2000. Available from: https://www.nap.edu/catalog/7928/to-err-is-human-building-a-safer-health-system. Accessed on 27 Jan 2023.
Cato M, Lasater K, Durham CF. NLN-Jeffries Project: expanding the student construct. Clin Simul Nurs. 2012;8(8):e413. https://doi.org/10.1016/j.ecns.2012.07.083.
Browning DM, Comeau M, Kishimoto S, Varrin P, Ward E, Rider EA et al. Parents and interprofessional learning in pediatrics: integrating personhood and practice. J Interprof Care. 2011;25(2):152-3. https://doi.org/10.3109/13561820.2010.505351, PMID 21043555.
Dreyfus SE, Dreyfus HL. A five-stage model of the mental activities involved in directed skill acquisition. California Univ Berkeley operations research center; 1980.
Lineberry M, Dev P, Lane HC, Talbot TB. Learner-adaptive educational technology for simulation in healthcare: foundations and opportunities. Simul Healthc. 2018;13(3S Suppl 1):S21-7. https://doi.org/10.1097/SIH.0000000000000274, PMID 29346223.
Reed D, Price EG, Windish DM, Wright SM, Gozu A, Hsu EB et al. Challenges in systematic reviews of educational intervention studies. Ann Intern Med. 2005;142(12 Pt 2)(12_Part_2):1080-9. https://doi.org/10.7326/0003-4819-142-12_part_2-200506211-00008, PMID 15968033.
World Health Organization. (2013). Transforming and scaling up health professions’ education and training: World Health Organization guidelines 2013. Retrieved from https://appswho.int/iris/bitstream/handle/10665/93635/9789241506502_end.pdf?sequence=1. Accessed on 27 Jan 2023.
Abraham G, Fehr J, Ahmad F, Jeffe DB, Copper T, Yu F et al. Emergency information forms for children with medical complexity: A simulation study. Pediatrics. 2016;138(2). https://doi.org/10.1542/peds.2016-0847, PMID 27436504.
Adeyinka A, Chahin N, Bochankova T, Caprusso F, Pinto R, Pierre L. Video versus mannequin training as a teaching tool for pediatric advanced airway management. Crit Care Med. 2013;1:A116.
Adler MD, Trainor JL, Siddall VJ, McGaghie WC. Development and evaluation of high-fidelity simulation case scenarios for pediatric resident education. Ambul Pediatr. 2007;7(2):182-6. https://doi.org/10.1016/j.ambp.2006.12.005, PMID 17368414.
Appelbaum N, Clarke J, Feather C, Franklin B, Sinha R, Pratt P et al. Medication errors during simulated paediatric resuscitations: A prospective, observational human reliability analysis. BMJ Open. 2019;9(11):e032686. https://doi.org/10.1136/bmjopen-2019-032686, PMID 31772103.
Aye S, Mohd Azhar MN, Ab Rahman MR. Lessons learned from adolescent aged simulated patients in undergraduate adolescent medicine curriculum: NDUM experience. Eur J Educ Sci. 2014;1:381–96.
Bigelow KM, Lutzker JR. Training parents reported for or at risk for child abuse and neglect to identify and treat their children’s illnesses. J Fam Violence. 2000;15(4):311–30. https://doi.org/10.1023/A:1007550028684.
Brett-Fleegler MB, Vinci RJ, Weiner DL, Harris SK, Shih MC, Kleinman ME. A simulator-based tool that assesses pediatric resident resuscitation competency. Pediatrics. 2008;121(3):e597-603. https://doi.org/10.1542/peds.2005-1259, PMID 18283069.
Brown KM, Mudd SS, Hunt EA, Perretta JS, Shilkofski NA, Diddle JW, et al. A multi-institutional simulation Boot Camp for pediatric cardiac critical care nurse practitioners. Pediatr Crit Care Med. 2018;19(6):564–71. doi: 10.1097/PCC.0000000000001532, PMID 29533354.
Brubacher SP, Powell M, Skouteris H, Guadagno B. The effects of e-simulation interview training on teachers’ use of open-ended questions. Child Abuse Negl. 2015;43:95–103. doi: 10.1016/j.chiabu.2015.02.004, PMID 25703802.
Burns TL, DeBaun MR, Boulet JR, Murray GM, Murray DJ, Fehr JJ. Acute care of pediatric patients with sickle cell disease: a simulation performance assessment. Pediatr Blood Cancer. 2013;60(9):1492-8. https://doi.org/10.1002/pbc.24558, PMID 23633232.
Byars D, Evans D, Lo B, Brodsky R, Walker L. Comparison of standard direct laryngoscopy versus pediatric king LT-D in a simulated difficult pediatric airway. Acad Emerg Med. 2010;1:194.
Chitkara R, Rajani AK, Oehlert JW, Lee HC, Epi MS, Halamek LP. The accuracy of human senses in the detection of neonatal heart rate during standardized simulated resuscitation: implications for delivery of care, training and technology design. Resuscitation. 2013;84(3):369 – 72. https://doi.org/10.1016/j.resuscitation.2012.07.035, PMID 22925993.
Chiu C-J. Development and validation of performance assessment tools for interprofessional communication and teamwork (PACT). ProQuest LLC; 2014.
Cicero MX, Brown L, Overly F, Yarzebski J, Meckler G, Fuchs S et al. Creation and Delphi-method refinement of pediatric disaster triage simulations. Prehosp Emerg Care. 2014;18(2):282-9. https://doi.org/10.3109/10903127.2013.856505, PMID 24401167.
Cordero L, Hart BJ, Hardin R, Mahan JD, Nankervis CA. Deliberate practice improves pediatric residents’ skills and team behaviors during simulated neonatal resuscitation. Clin Pediatr. 2013;52(8):747–52. doi: 10.1177/0009922813488646, PMID 23671270.
Cordova E, Al-Rousan T, Castillo-Angeles M, Aftab S, Nelson BD. Effect of low-cost interventions on the retention of knowledge and skills following Helping Babies Breathe training. Int J Gynaecol Obstet. 2018;142(2):248 – 54. https://doi.org/10.1002/ijgo.12512, PMID 29687893.
Costa LCSD, Avelino CCV, Freitas LA, Agostinho AAM, Andrade MBT, Goyatá SLT. Undergraduates performance on vaccine administration in simulated scenario. Rev Bras Enferm. 2019;72(2):345 – 53. https://doi.org/10.1590/0034-7167-2018-0486, PMID 31017195.
da Costa Brasil G, Ribeiro LM, Mazzo A, Guimarães dos Santos Almeida R, Martins JCA, Fonseca LMM et al. Use of the design and self-confidence scales in the assessment of maternal-child realistic simulation. Utilización Escalas Diseño Autoconfianza Eval Simulación Realista Matern-Infant. 2018;4:117 – 26.
do Nascimento Targino A, da Silva AP, Leitão FNC, Zangirolami-Raimundo J, de Oliveira Echeimberg J, Raimundo RD. Simulador de baixo custo para procedimentos de desengasgo e reanimação cardiopulmonar em lactentes, low cost simulator for cardiopulmonary unobstructed and reunion procedures in infants. Vol. 31; 2021. p. I–VIII.
Donoghue A, Nishisaki A, Sutton R, Hales R, Boulet J. Reliability and validity of a scoring instrument for clinical performance during Pediatric advanced life support simulation scenarios. Resuscitation. 2010;81(3):331-6. doi: 10.1016/j.resuscitation.2009.11.011, PMID 20047787.
Donoghue A, Ventre K, Boulet J, Brett-Fleegler M, Nishisaki A, Overly F, et al. Design, implementation, and psychometric analysis of a scoring instrument for simulated pediatric resuscitation: a report from the Express pediatric investigators. Simul Healthc. 2011;6(2):71–7. https://doi.org/10.1097/SIH.0b013e31820c44da. PMID 21358564.
Dorsey JK, Gocey J, Murrell K, Rinderer-Rand H, Hall C, Myers JH. Medical student response to an interactive patient simulation program used to supplement child abuse education. Child Abuse Negl. 1996;20(10):973 – 77. https://doi.org/10.1016/0145-2134(96)00086-5, PMID 8902294.
Edler AA, Chen M, Honkanen A, Hackel A, Golianu B. Affordable simulation for small-scale training and assessment. Simul Healthc. 2010;5(2):112–5. https://doi.org/10.1097/SIH.0b013e3181c76332. PMID 20661010.
Edwards E, Kessler C, Cherne N, Dissinger E, Shames A. Human factors engineering validation study for a novel 0.1-mg epinephrine auto-injector. Allergy Asthma Proc. 2018;39(6):461-5. https://doi.org/10.2500/aap.2018.39.4171.
Everett TC, McKinnon RJ, Ng E, Kulkarni P, Borges BCR, Letal M, Fleming M, Bould MD. Simulation-based assessment in anesthesia: an international multicentre validation study. Can J Anaesth. 2019;66:1440–49.
Finan E, Bismilla Z, Whyte HE, Leblanc V, McNamara PJ. High-fidelity simulator technology may not be superior to traditional low-fidelity equipment for neonatal resuscitation training. J Perinatol. 2012;32(4):287 – 92. https://doi.org/10.1038/jp.2011.96, PMID 22031045.
Geis GL, Wheeler DS, Bunger A, Militello LG, Taylor RG, Bauer JP et al. A validation argument for a simulation-based training course centered on assessment, recognition, and early management of pediatric sepsis. Simul Healthc. 2018;13(1):16–26. https://doi.org/10.1097/SIH.0000000000000271, PMID 29346221.
Gerard JM, Scalzo AJ, Borgman MA, Watson CM, Byrnes CE, Chang TP, et al. Validity evidence for a serious game to assess performance on critical pediatric emergency medicine scenarios. Simul Healthc. 2018;13(3):168–80. doi: 10.1097/SIH.0000000000000283, PMID 29377865.
Grant EC, Grant VJ, Bhanji F, Duff JP, Cheng A, Lockyer JM. The development and assessment of an evaluation tool for pediatric resident competence in leading simulated pediatric resuscitations. Resuscitation. 2012;83(7):887 – 93. https://doi.org/10.1016/j.resuscitation.2012.01.015, PMID 22286047.
Hall D, de Munter C, Ninis N, Goddard A, Avila H. G72 Simulation training in safeguarding children and adolescents: trainees want it, trainees like it and we need to deliver it. Arch Dis Child. 2015;100;Suppl 3:A30.2-A30. https://doi.org/10.1136/archdischild-2015-308599.71.
Hasselager A, Østergaard D, Kristensen T, Sønderskov C, Bohnstedt C, Lauritsen TLB et al. ”Assessment of laypersons” paediatric basic life support and foreign body airway obstruction management skills: a validity study. Scand J Trauma Resusc Emerg Med. 2018;26(1):73. https://doi.org/10.1186/s13049-018-0544-8, PMID 30189887.
Heimberg E, Schmutz J, Manser T, Eppich W, Keil J, Heinzel O, et al. Using in situ simulation to assess adherence to management guidelines for pediatric septic shock in german childrens hospitals. Pediatr Crit Care Med. 2014;1:176.
Herzberg S, Hansen M, Schoonover A, Skarica B, McNulty J, Harrod T et al. Association between measured teamwork and medical errors: an observational study of prehospital care in the USA. BMJ Open. 2019;9(10):e025314. https://doi.org/10.1136/bmjopen-2018-025314, PMID 31676639.
Hodgkinson R, Hall D, Tomlinson S. Multidisciplinary simulation-based training in managing unexpected child deaths in the emergency department. Arch Dis Child 2019;104;Suppl 2:A253.
Hossino D, Hensley C, Lewis K, Frazier M, Domanico R, Burley M, et al. Evaluating the use of high-fidelity simulators during mock neonatal resuscitation scenarios in trying to improve confidence in residents. SAGE Open Med. 2018;6:2050312118781954. : 10.1177/2050312118781954, PMID 29942511.
House JB, Dooley-Hash S, Kowalenko T, Sikavitsas A, Seeyave DM, Younger JG et al. Prospective comparison of live evaluation and video review in the evaluation of operator performance in a pediatric emergency airway simulation. J Grad Med Educ. 2012;4(3):312-6. https://doi.org/10.4300/JGME-D-11-00123.1, PMID 23997874.
House T, Schwebel DC, Mullins SH, Sutton AJ, Swearingen CJ, Bai S, et al. Video intervention changes parent perception of all-terrain vehicle (ATV) safety for children. Inj Prev. 2016;22(5):328–33. https://doi.org/10.1136/injuryprev-2015-041880. PMID 26850471.
Hoyle JD Jr, Ekblad G, Hover T, Woodwyk A, Brandt R, Fales B et al. Dosing errors made by paramedics during pediatric patient simulations after implementation of a state-wide pediatric drug dosing reference. Prehosp Emerg Care. 2020;24(2):204 – 13. doi: 10.1080/10903127.2019.1619002, PMID 31084508.
Hunt EA, Heine M, Hohenhaus SM, Luo X, Frush KS. Simulated pediatric trauma team management: assessment of an educational intervention. Pediatr Emerg Care. 2007;23(11):796–804. https://doi.org/10.1097/PEC.0b013e31815a0653. PMID 18007210.
Jabbour N, Reihsen T, Payne NR, Finkelstein M, Sweet RM, Sidman JD. Validated assessment tools for pediatric airway endoscopy simulation. Otolaryngol Head Neck Surg. 2012;147(6):1131–5. https://doi.org/10.1177/0194599812459703. PMID 22951432.
John J, Klingborg P. Improving residents’ confidence in leading pediatric codes. J Investig Med. 2019;67(2):425.
Kalaniti K. 52 Simulation-based team-leadership training for neonatal resuscitation: is learning by observation as effective as learning by participation? Paediatr Child Health. 2019;2e21. https://doi.org/10.1093/pch/pxz066.051. 24;Suppl.
Kane SK, Lorant DE. Creation and validation of tool to assess resident competence in neonatal resuscitation. Acad Pediatr. 2019;19(4):394 – 98. https://doi.org/10.1016/j.acap.2018.09.004, PMID 30273690.
Katznelson JH, Wang J, Stevens MW, Mills WA. Improving pediatric preparedness in Critical Access Hospital emergency departments: impact of a longitudinal in situ simulation program. Pediatr Emerg Care. 2018;34(1):17–20. https://doi.org/10.1097/PEC.0000000000001366, PMID 29232353.
Keidan I, Gravenstein D, Berkenstadt H, Ziv A, Shavit I, Sidi A. Supplemental oxygen compromises the use of pulse oximetry for detection of apnea and hypoventilation during sedation in simulated pediatric patients. Pediatrics. 2008;122(2):293-8. https://doi.org/10.1542/peds.2007-2385, PMID 18676546.
Khan EK, Lockspeiser TM, Liptzin DR, Meier M, Baker CD. ”When in Doubt, Change It out”: A Case-Based Simulation for Pediatric Residents Caring for Hospitalized Tracheostomy-Dependent Children. MedEdportal. 2020;16:10994. https://doi.org/10.15766/mep_2374-8265.10994, PMID 33015360.
Kim SJ, Oh J, Kang KA, Kim S. Development and evaluation of simulation-based fever management module for children with febrile convulsion. Nurse Educ Today. 2014;34(6):1005-11. doi: 10.1016/j.nedt.2013.11.008, PMID 24321166.
King G, Shepherd TA, Servais M, Willoughby C, Bolack L, Strachan D et al. Developing authentic clinical simulations for effective listening and communication in pediatric rehabilitation service delivery. Dev Neurorehabil. 2016;19(5):284 – 94. https://doi.org/10.3109/17518423.2014.989461, PMID 25548970.
Kioko M, Kasi N, Gupta A, Khazal S, Pinto R, Adeyinka A, et al. Using high-fidelity simulation to assess the efficacy of the broselow-luten software in the resuscitation of critically ill pediatric patients. Pediatr Crit Care Med. 2010;11(5):664.
Kothari K, Zuger C, Desai N, Leonard J, Alletag M, Balakas A, et al. Effect of repetitive simulation training on emergency medical services team performance in simulated pediatric medical emergencies. AEM Educ Train. 2021;5(3):e10537. https://doi.org/10.1002/aet2.10537. PMID 34099990.
Kurosawa H, Ikeyama T, Achuff P, Perkel M, Watson C, Monachino A et al. A randomized, controlled trial of in situ pediatric advanced life support recertification (”Pediatric Advanced Life Support Reconstructed”) compared with standard pediatric advanced life support recertification for CU frontline providers. Crit Care Med. 2014;42(3):610 – 18. https://doi.org/10.1097/CCM.0000000000000024, PMID 24231759.
Lacour M, Bloudeau L, Combescure C, Haddad K, Hugon F, Suppan L, et al. Impact of a Mobile app on paramedics perceived and physiologic stress response during simulated prehospital pediatric cardiopulmonary resuscitation: study nested within a multicenter randomized controlled trial. JMIR MHealth UHealth. 2021;9(10):e31748. : 10.2196/31748, PMID 34617916.
LaFond CM, Van Hulle Vincent C, Lee S, Corte C, Hershberger PE, Johnson A, et al. Development and validation of a virtual human vignette to compare nurses’ assessment and intervention choices for pain in critically ill children. Simul Healthc. 2015;10(1):14–20. https://doi.org/10.1097/SIH.0000000000000061.
Lammers RL, Byrwa MJ, Fales WD, Hale RA. Simulation-based assessment of paramedic pediatric resuscitation skills. Prehosp Emerg Care. 2009;13(3):345–56. doi: 10.1080/10903120802706161, PMID 19499472.
Lammers RL, Willoughby-Byrwa MJ, Vos DG, Fales WD. Comparison of four methods of paramedic continuing education in the management of pediatric emergencies. Prehosp Emerg Care. 2022;26(4):463 – 75. doi: 10.1080/10903127.2021.1916140, PMID 33872104.
LeBlanc VR, Regehr C, Shlonsky A, Bogo M. Stress responses and decision making in child protection workers faced with high conflict situations. Child Abuse Negl. 2012;36(5):404 – 12. https://doi.org/10.1016/j.chiabu.2012.01.003, PMID 22622225.
Lee MO, Brown LL, Bender J, Machan JT, Overly FL. A medical simulation-based educational intervention for emergency medicine residents in neonatal resuscitation. Acad Emerg Med. 2012;19(5):577 – 85. https://doi.org/10.1111/j.1553-2712.2012.01361.x, PMID 22594362.
Lemke DS, Fielder EK, Hsu DC, Doughty CB. Improved team performance during pediatric resuscitations after rapid cycle deliberate practice compared with traditional debriefing: a pilot study. Pediatr Emerg Care. 2019;35(7):480–86. doi: 10.1097/PEC.0000000000000940, PMID 27741071.
Levy A, Donoghue A, Bailey B, Thompson N, Jamoulle O, Gagnon R et al. External validation of scoring instruments for evaluating pediatric resuscitation. Simul Healthc. 2014;9(6):360-9. https://doi.org/10.1097/SIH.0000000000000052, PMID 25503530.
Levy A, Labrosse M, Donoghue A, Gravel J. Delays and errors among pediatric residents during simulated resuscitation scenarios using PALS algorithms. Acad Emerg Med. 2012;1;Suppl A:S385.
Marlow RD, Wood D, Lyttle MD. Comparing usability of paediatric weight estimation methods. Eur J Emerg Med. 2013;20(3):227.
McBride ME, Waldrop WB, Fehr JJ, Boulet JR, Murray DJ. Simulation in pediatrics: the reliability and validity of a multiscenario assessment. Pediatrics. 2011;128(2):335 – 43. https://doi.org/10.1542/peds.2010-3278, PMID 21746717.
Mema B, Park YS, Kotsakis A. Validity and feasibility evidence of objective structured clinical examination to assess competencies of pediatric critical care trainees. Crit Care Med. 2016;44(5):948–53. doi: 10.1097/CCM.0000000000001604, PMID 26862709.
Nadkarni LD, Roskind CG, Auerbach MA, Calhoun AW, Adler MD, Kessler DO. The development and validation of a concise instrument for formative assessment of team leader performance during simulated pediatric resuscitations. Simul Healthc. 2018;13(2):77–82. https://doi.org/10.1097/SIH.0000000000000267. PMID 29117092.
Neira VM, Bould MD, Nakajima A, Boet S, Barrowman N, Mossdorf P, et al. GIOSAT: a tool to assess CanMEDS competencies during simulated crises. Can J Anaesth. 2013;60(3):280–9. https://doi.org/10.1007/s12630-012-9871-9. PMID 23334779.
Padhya D, Tripathi S, Kashyap R, Alsawas M, Murthy S, Arteaga GM, et al. Training of pediatric critical care providers in developing countries in evidence based medicine utilizing remote simulation sessions. Glob Pediatr Health. 2021;8:2333794X211007473. https://doi.org/10.1177/2333794X211007473. PMID 33997121.
Ponce de Leon CGRM, Silva AK, Ribeiro LM, da Costa Brasil G, del Alamo Guarda LaiseE, Fonseca LMM. Development and validation of clinical cases to be used in maternal-child nursing education. Construcción y validación de casos clínicos para usarlos en la enseñanza de enfermería en el contexto materno-infantil. 2018;4:51–62.
Rovamo L, Mattila MM, Andersson S, Rosenberg P. Assessment of newborn resuscitation skills of physicians with a simulator manikin. Arch Dis Child Fetal Neonatal Ed. 2011;96(5):F383-9. https://doi.org/10.1136/adc.2010.194043, PMID 21242245.
Rowe AK, Onikpo F, Lama M, Deming MS. Evaluating health worker performance in Benin using the simulated client method with real children. Implement Sci. 2012;7:95. https://doi.org/10.1186/1748-5908-7-95, PMID 23043671.
Sadideen H, Wilson D, Moiemen N, Kneebone R. Proposing the burns suite as a novel simulation tool for advancing the delivery of burns education. J Burn Care Res. 2014;35(1):62–71. https://doi.org/10.1097/BCR.0b013e31829b371d. PMID 23877145.
Sadideen H, Wilson D, Moiemen N, Kneebone R. Using ’the burns suite’ as a novel high fidelity simulation tool for interprofessional and teamwork training. J Burn Care Res. 2016;37(4):235–42. doi: 10.1097/BCR.0000000000000262, PMID 26056756.
Sagalowsky ST, Prentiss KA, Vinci RJ. Repetitive simulation is an effective instructional design within a pediatric resident simulation curriculum. BMJ Simul Technol Enhanc Learn. 2018;4(4):179 – 83. https://doi.org/10.1136/bmjstel-2017-000282, PMID 35519013.
da Costa S, Cristina L, Avelino CCV, Aparecida de Freitas L, Aparecida A, Agostinho M, et al. Desempenho de estudantes universitários sobre administração de vacinas em cenário simulado. Rev Bras Enferm. 2019;72:362–70.
Schmutz J, Eppich WJ, Hoffmann F, Heimberg E, Manser T. Five steps to develop checklists for evaluating clinical performance: an integrative approach. Acad Med. 2014;89(7):996–1005. https://doi.org/10.1097/ACM.0000000000000289, PMID 24826862.
Schmutz J, Manser T, Keil J, Heimberg E, Hoffmann F. Structured performance assessment in three pediatric emergency scenarios: a validation study. J Pediatr. 2015;166(6):1498 – 504.e1. https://doi.org/10.1016/j.jpeds.2015.03.015, PMID 25890675.
Sepúlveda Oviedo EH, Bermeo Clavijo LE, Méndez Córdoba LC. OpenModelica-based virtual simulator for the cardiovascular and respiratory physiology of a neonate. J Med Eng Technol. 2022;46(3):179 – 97. doi: 10.1080/03091902.2022.2026500, PMID 35172686.
Seto TL, Tabangin ME, Taylor KK, Josyula S, Vasquez JC, Kamath-Rayne BD. Breaking down the objective structured clinical examination: an evaluation of the helping babies breathe OSCEs. Simul Healthc. 2017;12(4):226–32. doi: 10.1097/SIH.0000000000000224, PMID 28319491.
Shin H, Shim K, Lee Y, Quinn L. Validation of a new assessment tool for a pediatric nursing simulation module. J Nurs Educ. 2014;53(11):623–9. https://doi.org/10.3928/01484834-20141023-04. PMID 25350903.
Siebert JN, Glangetas A, Grange M, Haddad K, Courvoisier DS, Lacroix L. Impact of blended learning on manual defibrillator’s use: A simulation-based randomized trial. Nurs Crit Care. 2022;27(4):501 – 11. https://doi.org/10.1111/nicc.12713, PMID 34519140.
Sigalet E, Donnon T, Grant V. Undergraduate students’ perceptions of and attitudes toward a simulation-based interprofessional curriculum: the KidSIM ATTITUDES questionnaire. Simul Healthc. 2012;7(6):353–58. https://doi.org/10.1097/SIH.0b013e318264499e. PMID 22902608.
Smith KA, Setlhare S, DeCaen A, Donoghue A, Mensinger JL, Zhang B et al. Feasibility and preliminary validity evidence for remote video-based assessment of clinicians in a global health setting. PLOS ONE. 2019;14(8):e0220565. https://doi.org/10.1371/journal.pone.0220565, PMID 31374102.
Teis R, Allen J, Lee N, Kildea S. So you want to conduct a randomised trial? Learnings from a ‘failed’ feasibility study of a Crisis Resource Management prompt during simulated paediatric resuscitation. Australas Emerg Nurs J. 2017;20(1):37–44. https://doi.org/10.1016/j.aenj.2016.12.001, PMID 28042009.
Tobler K, Grant E, Marczinski C. Evaluation of the impact of a simulation-enhanced breaking bad news workshop in pediatrics. Simul Healthc. 2014;9(4):213-9. https://doi.org/10.1097/SIH.0000000000000031, PMID 24787559.
Tofil NM, Lin Y, Zhong J, Peterson DT, White ML, Grant V, et al. Workload of team leaders and team members during a simulated sepsis scenario. Pediatr Crit Care Med. 2017;18(9):e423–7. https://doi.org/10.1097/PCC.0000000000001258. PMID 28654549.
Traynor D, Lydon A, Hickerson KA, Je Sangmo, Nishisaki A. Development of simulation-based assessment for pediatric intensive care nurse orientation. Clin Simul Nurs. 2021;56:37. https://doi.org/10.1016/j.ecns.2021.01.003.
Tsai TC, Harasym PH, Nijssen-Jordan C, Jennett P, Powell G. The quality of a simulation examination using a high-fidelity child manikin. Med Educ. 2003;37;Suppl 1:72 – 8. https://doi.org/10.1046/j.1365-2923.37.s1.3.x, PMID 14641642.
Tyler TR, Franklin AE. Research note—dyadic OSCE subscales: measuring students’ ability to work with parents and LGBTQ children. J Soc Work Educ. 2021;57(4):809–16. https://doi.org/10.1080/10437797.2020.1714523.
Ventre KM, Collingridge DS, DeCarlo D, Schwid HA. Performance of a consensus scoring algorithm for assessing pediatric advanced life support competency using a computer screen-based simulator. Pediatr Crit Care Med. 2009;10(6):623–35. https://doi.org/10.1097/PCC.0b013e3181b00ee4. PMID 19898170.
Walton JL, Dunn DK, Haines NY, Heisler I, Bigham MT, Volsko TA. Ventilator Boot Camp improves the knowledge and skills associated with mechanical ventilator use during interfacility transport of intubated pediatric patients. Respir Care. 2018;63(4):417 – 23. https://doi.org/10.4187/respcare.05951, PMID 29559539.
Watkins SC, de Oliveira Filho GR, Furse CM, Muffly MK, Ramamurthi RJ, Redding AT, et al. Tools for assessing the performance of pediatric perioperative teams during simulated crises: a psychometric analysis of clinician raters’ scores. Simul Healthc. 2021;16(1):20–8. doi: 10.1097/SIH.0000000000000467, PMID 33956763.
Watkins SC, Roberts DA, Boulet JR, McEvoy MD, Weinger MB. Evaluation of a simpler tool to assess nontechnical skills during simulated critical events. Simul Healthc. 2017;12(2):69–75. https://doi.org/10.1097/SIH.0000000000000199, PMID 28704284.
Whalen AM, Boyer D, Nishisaki A. ”Defining competency in neonatal and pediatric bag mask ventilation”, pediatrics. Conference: National Conference on Education. Vol. 144; 2018.
Whalen AM, Merves MH, Kharayat P, Barry JS, Glass KM, Berg RA et al. Validity evidence for a novel, comprehensive bag-mask ventilation assessment tool. J Pediatr. 2022;245:165–171.e13. https://doi.org/10.1016/j.jpeds.2022.02.017, PMID 35181294.
Namba N, Miyake K, Hino S, Itoi S. Examination of a simulated experience program to promote understanding of children with health disorders through remote training. Mejiro J Health Care Sci. 2021;14:51–60.
Acknowledgements
Not applicable.
Funding
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (No. 2021R1A2C1095530).
Author information
Authors and Affiliations
Contributions
KEJ contributed to the idea generation, coordination of research progress, literature screening, description of results section, and creation of tables for the research. KSK contributed to writing the background section, communicating and collecting opinions among authors, conducting literature searches, literature screening, and editing the manuscript. SSS contributed to the literature search, literature screening, writing of the discussion section, and reference formatting. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The Institutional Review Board (IRB) of Gangneung-Wonju National University approved this study under the reference number GWNUIRB-R2022-25 and determined it to be exempt from ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, E., Song, S. & Kim, S. Development of pediatric simulation-based education – a systematic review. BMC Nurs 22, 291 (2023). https://doi.org/10.1186/s12912-023-01458-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-023-01458-8