Abstract
Background
Work-integrated learning (WIL) is a core aspect of allied health education. WIL placements typically focus on developing clinical skills, with broader conceptions of work readiness a secondary consideration. Near-peer mentoring (NPM), where senior students mentor junior students, is one WIL placement model that holds promise for developing students’ work readiness, along with additional benefits for educators and service users. While there is emerging evidence of the benefits of NPM in allied health, a more comprehensive understanding of the design and outcomes of NPM WIL placements for allied health students, their educators and service users is needed.
Methods
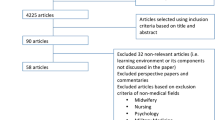
A systematic search of seven electronic databases (CINAHL, ERIC, ProQuest Education, Medline, PsychInfo, EMBASE and Scopus) from 2003 to 2022 was conducted with 4195 records reviewed. Included studies reported on near-peer mentoring between at least one of the identified 11 allied health professionals providing services to real people (i.e. not simulation). Data extracted included pedagogical approaches, type of service model and relationship of peers to each other and educator, objectives for implementing the NPM, and effects for students. Quality appraisal was undertaken using the Standards for Reporting of Qualitative Research (SRQR).
Results
Fourteen studies met the inclusion criteria. The majority were North American in origin, from the disciplines of pharmacy, physiotherapy, psychology and occupational therapy, and used a range of research designs. Four types of placement design were observed from incidental co-location of students and observing outcomes through to deliberate preparation of students and/or educators for their roles in a NPM placement. Outcomes for junior students included lowered anxiety leading to increased confidence and motivation to learn and thus enhanced clinical skills. Senior student outcomes included development of educator skills, increased confidence, and enhanced professional reasoning. Service users and educators also benefited from NPM; however, evidence was sparse in these areas.
Conclusion
The evidence supports near-peer mentoring as a valuable WIL model to support work readiness, and several general pedagogical designs are evident. Future research should design NPM WIL with a greater integration of educational theory and evaluate outcomes beyond satisfaction and self-reported experiences.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
In general, many allied health professionals are considered eligible to directly enter practice upon completion of their degrees (i.e., without any further requirements such as a postgraduate internship or residency). Thus, adequate preparation and subsequent achievement of professional competencies is essential to ensure graduates are ready for the demands of the workplace. ‘Work readiness’ is a multidimensional concept, [1] defined as “the extent to which graduates are perceived to possess the attitudes and attributes that render them prepared or ready for success in the workplace” [[2], p12]. It encompasses both technical or discipline-specific and generic or soft skills [3] that support the use of professional judgement in complex situations [4]. Beyond clinical proficiency, work readiness for allied health professionals includes personal characteristics or social intelligences such as confidence, responsibility, maturity, resilience, flexibility, self-awareness and stress management, and non-technical skills such as effective communication with service users and colleagues, clinical reasoning, interprofessional teamwork, and organisational skills, [5, 6] along with participation in the education of others [5, 6].
Work-integrated learning (WIL) is often identified as an appropriate arena for the development of non-technical capabilities, [1] yet in the health professions, WIL, in the form of individual placements, has traditionally focussed on the development of clinical acumen through service userFootnote 1/client contact [7, 8]. Simultaneously, education providers are forced to deal with capacity limitations in workplace-based learning, and it is recognised that individual apprenticeship models of clinical education are unlikely to be viable in the longer term [7, 8]. Individual apprenticeships also limit opportunities for students to develop teaching skills prior to graduation. This may in turn compound limited placement capacity since graduates must first further develop their skills before becoming placement educators [9]. Presently, the predominance of the apprenticeship model means there is often limited focus on students and educators implementing innovative placement models, and where innovations do occur, these studies are often of poor methodological quality [7, 10, 11]. Evidence for WIL models that support all aspects of work readiness – especially the development of educator skills – is therefore required to ensure that allied health graduates are indeed prepared for practice.
Preparedness for practice, or work readiness has been explored in health professions [12,13,14] generally, with some studies specifically focussing on the unique contribution of WIL [13, 15]. Much of this literature comes from the professions of nursing and medicine and, given that these professions share a common purpose of healthcare service delivery with allied health, findings could be interpreted as being applicable to all health professions. However, even between nursing and medicine, cultural differences in hospital-based teaching and learning practices have been identified, [16] challenging the assumption that WIL placement research findings are applicable across health professions. Attrill et al., [4] argues that generalisation of findings is also impacted by context, since medical and nursing work readiness research is primarily based in hospital settings. This contrasts with allied health professionals who increasingly work in a diversity of practice settings such as disability services, community organisations and private practices in addition to tertiary healthcare. The relative absence of the voice of allied health professionals in health professions educational research to date points to a need for research on WIL models focussing on the development of educator skills involving a range of allied health professions. In this paper, we firstly summarise the pedagogical contribution of one WIL model, near-peer mentoring, investigating the impacts of near-peer mentoring in allied health WIL placements through a systematic review of the literature.
Near-peer mentoring (NPM)
NPM is particularly applicable to workplace-based settings for learning and the development of the associated work readiness skills. Variously referred to as near-peer mentoring, near-peer tutoring, layered learning model, [17] tiered learning or cross-peer assisted learning, [18] it involves students who are one or more academic year levels apart. It is a subset of peer-assisted learning (PAL), which is a well-established educational approach in which students learn from and with each other [19, 20]. This learning occurs in very small groups (1:1 to 1:2 ratios of senior:junior students [19]), with more experienced peer/s also role modelling and reinforcing the learning of less experienced peer/s and in turn learning by teaching [21].
The pedagogical underpinnings of near-peer mentoring in WIL
NPM is broadly considered a pedagogical approach that is aligned with a social constructivist paradigm, whereby knowledge is constructed by individuals from experiences that are integrated into their own understandings, rather than being absolute and transferrable [22, 23]. This combines well in WIL where the context promotes experiential learning; that is, learning in context from authentic experiences and through interaction with others [22]. Important to such learning in WIL is deliberate practice where students have the opportunities for repetition, feedback and reflection to improve their performance [24]. In NPM, these opportunities are enhanced by the availability of peers. Participating in roles of both performer and observer, feedback receiver and feedback provider, also enhances students’ metacognitive awareness and self-regulation [25].
Learning together in NPM, students have opportunities to develop their knowledge, skills, and professional identities within their zone of proximal development (ZPD) where substantial seniority or expertise is not required, and learning can occur with the guidance and support of anyone who is more advanced in the area [26]. Supporting this belief is the idea that students, even of differing levels are both cognitively and socially congruent [27]. They share a similar knowledge base which enables the more advanced student to explain difficult topics or share how they learned a complex technical skill or concept. In relation to social congruence, they have both adopted student roles, sharing similar experiences, problems and demands [28]. NPM also provides opportunities for senior students to fulfil relatively senior roles such as supervision to support development of their educator skills prior to graduation. In the process, junior students may feel more comfortable to be vulnerable for new learning and development, [27] and in NPM, senior students may gain confidence in the extent of their knowledge and skill [15] relative to peers at a level of their own recent experience, as well as reinforcement of knowledge and skill through interaction with others and teaching [15, 21, 29].
Through the process of constructivist and experiential learning in WIL settings, students are developing the knowledge, values, and attitudes of professionals in their field in a process of professional socialisation [30]. In NPM, students have opportunities for exposure to, and internalisation of, the norms and practices of their profession with peers who are more advanced as well as with educators [31]. They also have opportunities to see the process of professional entrustment in progress whereby students are entrusted by educators with increasing levels of independence based on an evaluation of the risk involved considering their knowledge, skill and attributes [32]. Similarly, NPM harnesses the tendency for social comparison as a means for self-evaluation [20] as students progress in their professional socialisation and identity formation. Finally, with senior students, junior students, and/or educators interacting and learning together in the workplace, there is also the opportunity for the formation of communities of practice [33] and consequently the motivation and reward of working towards membership of the profession [34].
Evidence for effectiveness of peer-assisted learning
The use of various forms of PAL in health professions WIL are identified in the literature dating back to the 1980s, [35,36,37] in a number of health professions education systematic reviews [7, 11, 20, 21, 38]. These reviews vary as to who was included (medicine, nursing, or all health professions) and the inclusion or exclusion of a near peer versus same level PAL. Overall, these reviews demonstrate that students benefit from increased opportunities for discussion, reflection, and peer support in PAL models [7, 11] with students in NPM also finding learning from a near peer lower pressure than learning from an educator [15]. Generally, students’ increased confidence also leads to reduced educator supervision needs [7, 11]. Improved outcomes are often noted in collaborative, non-technical, work readiness skills and attributes such as communication, teamwork, time management, and leadership, as well as autonomy and clinical reasoning [10, 11, 15, 38, 39]. Challenges arise when there is perceived competition between students, or students feel that learning from peers competes with their learning from ‘expert’ educators, especially as they approach the end of their placements [7, 11, 15, 39]. When paired with junior students, however, senior students gain confidence and teamwork skills thought to be beneficial in the transition to graduate practitioner [15, 39]. Despite these generally positive outcomes for students identified in previous reviews of PAL, the quality of included studies was criticised, especially since study designs focus on student and educator satisfaction rather than learning, behaviour and/or impact levels [10, 11]. Reviews also do not distinguish the difference in allied health professions contexts from nursing and medical contexts, meaning contextual outcomes and experiences may be neglected [7, 10]. Though research quality has improved over time, even recent reviews across all health professions concluded there is insufficient evidence to recommend any particular placement model [11, 15]. While outcomes evidenced to date are reasonably consistent [7] and align with what may be expected given the theoretical foundations of PAL, there has been limited consideration of such explanations for the outcomes observed in allied health, [10] in contrast to medicine [20] or nursing [40].
In the placement setting, it is also important to consider the benefits and impacts for other stakeholders such as service users, educators and employers. It has been noted that PAL and NPM placement models can be challenging for educators to implement, particularly if students have different learning needs or a student is underperforming or requires support in managing peer relations [11, 15, 38, 39]. Educator training regarding the facilitation of PAL is therefore recommended, [7, 39] though it is also challenging if placement models are prescriptive of PAL activities [15]. On the other hand, educators can find that peer interactions during the placement can decrease the time educators spend in instructing and supervising students and increase the service productivity when accounting for student inputs [10, 38, 39]. Educators may also have opportunities to gain additional skills related to instruction, teamwork, and clinical management [39]. The balance of these challenges and benefits do vary, and findings regarding the time commitments for PAL placements are mixed, [11, 15, 38] which may lead educators to perceive that PAL placements will be time consuming [39]. Organisation is certainly required, including to schedule students together and for advance preparation of the placement, educators, and students, with a degree of tailoring to students’ goals and individual needs [7, 10, 15, 38, 39]. It has also been noted that there is little evidence regarding the impact of PAL and NPM placements on service users, despite the argument that such placements should improve quality and outcomes in healthcare [39].
The evidence gaps for allied health NPM placements
The use of NPM in allied health WIL has the potential to address the quality of learning experiences for students, enhance outcomes for service users, improve educator productivity and increase placement capacity. WIL, like clinical practice, should be based on evidence [39]. The lack of focus on and supporting evidence for the impacts of NPM on allied health service users and educators is perhaps a reason why there has been limited uptake of these placement models. While considerable evidence exists for NPM PAL placement models in medicine and nursing, [39] there is limited evidence beyond 2:1 placement models and insufficient evidence to recommend any specific PAL placement model in allied health [11, 15]. Recent systematic reviews have mostly failed to consider the underlying pedagogies used to inform placement design while recommending that future studies collect further evidence beyond student and/or educator satisfaction to consider outcomes for student learning, behaviour and/or impact [41]. Presently, allied health educators are unable to determine how to effectively design and implement NPM to achieve desired learning outcomes for students. Therefore, this study sought to address the following questions:
-
What are the outcomes of near-peer mentored work integrated learning placements for allied health students, their educators and service users?
-
How are near-peer mentored placements in allied health designed to achieve those outcomes?
Methods
This review was conducted using a systematic approach to literature searching and data analysis. Details of the protocol for this systematic review were registered on PROSPERO (CRD42018102790) [42].
Search strategy
Seven databases were searched: Cumulative Index to Nursing and Allied Health Literature (CINAHL via EBSCO), Educational Resources Information Center (ERIC via EBSCO), Proquest Education (via Proquest), Medline (via OVID SP), PsychInfo (via OVID SP) EMBASE (via OVID SP) and Scopus for English-only sources dated between January 2003 and December 2022. The years 2003 to 2022 were selected to both overlap with an earlier near-peer learning in WIL-specific systematic review [43] while capturing the most recent literature, with the search first undertaken in March 2018, updated in October 2019 and last repeated on 21 November 2022.
Search terms
Previous systematic reviews [10, 18, 44] provided insight into the breadth of search terms needed to capture NPM in work integrated learning placements. Search terms included combinations of the terms student, clinical, education, placement, clerkship, practicum, and professional education; terms to capture peer learning included near-peer, peer-assisted, peer mentoring, cross peer, paired, collaborative or cooperative learning; and allied health related terms. To determine which professions to include in the search, the list published by Allied Health Professions Australia [45] was used with the following professions included: occupational therapy, physiotherapy, speech pathology, social work, pharmacy, dietetics, audiology, podiatry, exercise physiology and paramedicine as well as their various international derivatives (for example, physiotherapy or physical therapy and exercise physiology or exercise science professional). The criteria for inclusion/exclusion is outlined in Table 1.
Screening and selection of studies
Covidence [46] was used to manage the review process (refer to Fig. 1). The first 300 articles (sorted according to title) were independently reviewed by title and abstract by the lead author (MP), with two additional authors (JT and GE) reviewing 50% each. Where differences were identified, all three reviewed the title and abstract together to establish concordance. With agreement reached on the interpretation of the criteria through this process, the team moved to single reviewer screening (MP) with a tendency to include rather than exclude as outlined by Tai et al. [20] Where it was not clear whether to include based on title/abstract, MP consulted with JT and GE and a final decision was made.
Full-text screening of studies found across the three search dates was undertaken on 198 papers independently by a combination of two of MP, GE and JT, with the third screener providing conflict resolution. Of note, is the addition of three papers [47,48,49] found in the final search, being the only ones published after October 2019 that met the inclusion criteria. In total, this process identified 19 papers as potentially meeting all criteria for inclusion in the review. Given the differing nature of the papers, and to ensure that all relevant information was located and reported, MP, GE and JT scrutinised each article in depth. Data extraction was completed separately using a simple data extraction tool [20] with headings aligned to the review questions. Findings were compared and compiled into final descriptions. Through this process a further five studies were excluded as it became evident that these studies did not fully meet the criteria. Specifically, participants were not purposefully paired for the purposes of learning, or minimal research data was presented.
Quality review was then undertaken on the final 14 papers using the Standards for Reporting of Qualitative Research (SRQR), [50] which was designed for holistic judgement as befits a qualitative approach, instead of a quantifying score. Each paper was assessed for quality across 21 standards of the SRQR. Two researchers (MP and GE) applied the SRQR standards separately, deeming the quality of meeting each standard to be high if the majority of elements were adequately described and justified, low if substantial elements were described but not adequately justified, or unclear if substantial elements were not described in adequate detail (refer to Supplementary Material). MP and GE then compared these judgements with the aim of reaching consensus. The overall judgement of the quality of each paper was discussed and agreed to by MP, GE and JT with more weighting placed on the standards relating to methodology than other standards. For most papers, quality was difficult to judge due to insufficient information provided in the articles resulting in many unclear ratings. No papers were excluded based on the quality assessment given the small number of papers overall and the descriptive nature of this review. Instead, study quality was considered when considering the weighting of the evidence.
Results
Description of studies
The final 14 papers, (henceforth called studies; see Table 2) described 12 NPM placement interventions. Two studies were represented by pairs of papers. One of the NPM placement interventions was reported first from the student learner [49] and then educator [47] perspectives. The second study was undertaken with pharmacy students [51] with the design of the NPM intervention and research methods appearing to be replicated in a later comparative study [52, 57] between medical and pharmacy students in the same hospital. Although these studies appear to be paired and each group of authors references the earlier study, for the purposes of the results they are reported as individual studies.
Studies were from the United States (n = 6), Canada (n = 7) and the United Kingdom (n = 1). Disciplines represented included pharmacy, physiotherapy, psychology and occupational therapy, with 12 studies involving students from the same discipline, [6, 9, 17, 47,48,49, 51,52,53,54,55,56] and two pairing related but distinct roles within the same disciplines (e.g., occupational therapy with occupational therapy assistants and physiotherapy students with physiotherapy assistants) [57, 58]. Across the 14 studies, placement lengths varied from four weeks [51] through to nine- to twelve-month programs, [53, 55] with some being part-time only for the junior [6, 9, 53, 56] and/or senior students [6, 53, 55, 56]. Five studies were based in university owned and operated clinics, [6, 9, 53, 55, 56] six in adult hospital settings, [17, 48, 49, 51, 52, 58] one in mixed hospital/community settings [47], and one in a residential aged care setting [54]. One study did not provide sufficient data to determine the placement setting [57].
Studies were also varied in their research design. Six were program evaluations, [6, 17, 53, 55, 57, 58] one mixed methods research, [56] two drew on ethnographic principles, [51, 58] two were case study research, [9, 54] with one of these also utilising action research [54] and three studies used a retrospective design, [47,48,49] being either survey and/or individual semi-structured interviews. Sample sizes ranged vastly for both students (n = 4–130) and educators (n = 1–20). In one study, service users’ experiences (n = 16) were also reported [53].
The aims and objectives of the studies were also heterogenous, with research designs reflecting the variety of positioning of the research in relation to the rationales for including NPM. For example, some studies described placement structures where, due to the curriculum design and resulting overlapping placement across different year groups, near-peer mentoring was already occurring. The focus of these studies was to evaluate what had been ongoing for some time [51] or to explore the value of additional introduced elements [53, 58]. Several studies focused on student and/or educator perspectives of evaluating the introduction of NPM for the first time, with evaluations undertaken on placement completion, [54] within 3 years of graduating, [49] or at times not explicitly reported [47, 48]. Other studies had more specific goals for introducing NPM; for example, to explore whether NPM could assist students in the acquisition of skills required to be effective educators, [47, 48] or to ensure students from differing roles within the same discipline (e.g., physiotherapists and physiotherapy assistants) were better prepared for working collaboratively [57].
Overall, the quality of the papers was difficult to discern and therefore to weight in the evidence when also considering different designs and aims. There were, however, exemplars [6, 9, 52,53,54,55, 57] that adequately described and justified most of the elements for the quality standards pertaining to the methodology and results. Most of the papers had multiple sections scored as ‘unclear’ due to limited reported details about the study, with those deemed of lower quality not providing adequate justification and often not clearly being aligned to a research framework.
Placement design
The catalyst for adoption of a NPM model varied across the studies. Analysis of the placement designs described provided insight into the underpinning educational theories and/or learning strategies utilised. The placement designs could be organised into four main groupings: the first related primarily to co-locating the students and observing outcomes, the second to preparing students to achieve expected learning outcomes, and the third to preparing educators for their role in placement design. The fourth group consisted of retrospective studies of whole student cohorts, where the emphasis was on the student and academic experiences, with no specific information provided about placement design.
Co-location of students
Three studies [53, 54, 58] primarily drew on the theories of collaborative learning and experiential learning [53, 54] to inform placement design. Examples of learning strategies included introducing Grand Rounds to provide better continuity of care and stronger learning experience for students [53] or joint tutorials between related disciplines to discuss interprofessional issues [58]. The underlying premise in these studies was that by co-locating students in a collaborative peer relationship, mutual learning would occur through the sharing of experiences and knowledge, with junior students also learning from observing their senior peers. In these studies, there appeared to be minimal to no preparation of students for their roles as mentor/mentees or even co-learners. While the authors reported that students found the experience satisfying and gained confidence in some skills, [53, 54] it was not clear the degree to which this could be attributed to the near peer relationship as opposed to the placement learning experiences generally. Outcomes from these studies included recommendations related to the need for improved preparation of students, including clarity of senior and junior roles [54].
Deliberate student preparation
Studies in this group [6, 9, 17, 55, 56] included those where the authors deliberately designed their placement models to meet specified student learning outcomes, such as developing senior students’ educator skills with the view that they eventually become formal educators of others, or for fostering interdisciplinary teamwork. Whilst drawing from experiential learning theory, [9, 55] these authors also applied learning theories or models such as cognitive apprenticeship [6] and transformative learning [6] in a layered learning [17] or progressive curricular model [56]. In these five studies, senior and junior students were specifically prepared for their roles. Junior students were primarily prepared for aspects of direct service delivery and in one study also for their role in providing feedback to senior students [9]. Senior students were specifically prepared for their role as educators, mentors or coaches. While the senior students may initially have a greater clinical role (e.g., to model practice behaviours/skills), in some studies [6] this was reduced over time to enable increased opportunity for junior student involvement in service delivery. For all studies in this group, senior students were prepared for their mentoring role during classes occurring in parallel with the placement, [6] or within the placement itself [17, 55, 56]. For the within-placement model, learning experiences were deliberately scaffolded, with ongoing coaching/education sessions and/or educator modelling to support the development of the senior students’ mentoring role. Several of these studies [6, 17, 56] implemented a progressive circular or layered learning model where students experience firstly the junior, then senior role, in the same context. Three of these studies were pro-bono university clinics [6, 9, 56] the other two university managed clinics, either in the academic medical centre [55] or ambulatory clinic in a local hospital [17]. Thus, for students entering the senior role in these studies, some had already experienced being a junior student and were familiar with the placement context, educators and service delivery models.
Compared with the first group, where students were co-located with the aim of learning from each other, studies in this group deliberately designed for specific outcomes. With targeted preparation and some degree of ongoing coaching (either in class or in the placement), a different range of outcomes were reached. For example, students were seen to have a greater degree of confidence in not only their educator skills, but in their clinical skills as well, with one study suggesting the model assisted with readiness for the final placement and postgraduate clinical experience, [17] and another that students demonstrated increased confidence and sense of capability [6]. Students and their educators perceived that students developed clinical skills in communication, problem-solving and clinical reasoning and were able to identify growth both in themselves and junior students, [6, 17, 56] with participants in one study reporting knowledge being reinforced through the instruction of junior peers [17]. In studies where the learning was explicitly scaffolded, where the educators modelled how to educate, and where students rotated through from junior to senior student, the findings suggested that these senior students emerged from the experience feeling confident in the educator skills they had developed, positioning themselves as lifelong learners and being inspired for, and feeling prepared for future educator roles [6, 9, 55, 56].
Deliberate educator preparation
One study incorporating deliberate educator preparation [57] was identified, being otherwise similar to the studies with deliberate student preparation designed to achieve student learning outcomes. This study drew from learning theories such as collaborative learning within a reciprocal peer coaching model. However, the preparation focus in this study was on the educators who were encouraged to use guidelines for collaborative practice to create optimal learning experiences for student pairs. Outcomes of this model were similar to those studies where students were co-located with minimal to no preparation for their educator roles.
Retrospective perspectives
The final and most recent group of studies [47,48,49] had a retrospective approach to investigating the use of NPM placements and did not explicitly state either the educational theory or learning strategies implemented in the original placements. These studies employed survey and semi-structured interview methods to understand student and educator perspectives on past experiences with NPM models of placement. Findings from these three studies reiterated outcomes for students and educators found in the other groups of studies, such as building educator skills, student autonomy and student enjoyment [47,48,49]. Additionally, MacDonald et al. [48] gathered suggestions from educators on strategies to mitigate specific challenges encountered in future implementation of the model.
Observed outcomes
A collation of reported outcomes reported in included studies is reported in Table 3. Outcomes for each stakeholder group are briefly summarised below.
Overall, the NPM model was well received by most students [17, 55]. Many of the studies supported that the model facilitated development in students’ personal growth, skill acquisition and well-being. As discussed above, outcomes varied across the studies, depending on the intent and educational approaches to student placement. Skills such as communication, confidence and collaborative practice were observed to be developed, including reports of student motivation and inspiration for the roles of clinician [9] and educator in the future [6, 48, 49, 56]. Outcomes observed by students and educators were different between senior and junior groups with predominantly positive outcomes reported. A few studies described challenges of the model for students with reports of some anxiety, repetition of information, difficulties managing time, competitiveness and role confusion [48, 52].
Outcomes for educators
Six studies [6, 47, 48, 51, 54, 57] commented specifically on the educator impacts of implementing this model at their sites. Educators further developed their supervision skills and support for each other in this model [54]. Educators also felt rewarded in facilitating this integration of near-peer student placement models with client care [6] and in one study reported the logistical benefits of project-funded relief time from duties to prepare for the placement [57]. Challenges reported for educators included the balancing of different learner needs and time commitment for tasks such as preparation and assessment [47,48,49].
Outcomes for service users
Five studies mentioned an impact on service users and health care delivery, [17, 47, 48, 51, 53] with only one of these [53] including service users as direct participants contributing their own perspectives. None of the impacts on service users were measured; all were reported from the perspectives of participants. In the one study that included service users as participants, those service users did not overtly recognise the students as delivering a service [53]. Students and educators were more positive about the impacts on service users, with participants perceiving the team learning approach in NPM improved service users’ care and progression, [17, 51] and educators feeling the model assisted with continuity of service for service users. [53] It was also reported that more service users were able to be receive a service when senior students were assisting the junior students in the NPM but this was not quantified [51].
Discussion
This review has identified clear benefits for allied health students from participating in NPM placement models, across a modest number of papers. Due to the evaluative rather than comparative nature of the research, it is uncertain whether all of the findings are substantial additional benefits over a traditional placement model. However, it is unlikely that students would enjoy the same development of educator skills without opportunities to practise these in the mentoring role. To be considered work ready, graduates must be able to practice not only service user care, but also other capabilities that are considered core components of professional practice in allied health, such as working collaboratively in teams [4, 59] and participating in the education of students and peers [5, 6]. In alignment with previous reviews, there remains sparse evidence for educator and service user benefits. However, this should not prevent the implementation of NPM, rather, we echo previous recommendations that further investigation and more elaborate reporting of outcomes is required, when NPM is utilised.
Given that the evidence from these studies does not provide a strong basis for implementation of any particular placement model, we now propose and discuss three aspects of intervention design and/or research that would facilitate the generation of higher quality NPM research and implementation.
Design NPM with work readiness in mind
Several studies in the review [53, 54] reported that NPM came about as a by-product of circumstances related to the increased need for placements. This impetus has previously been noted in systematic reviews of same level PAL [5, 10]. Rather than selecting this model to only address placement capacity, we suggest that intentionally designing NPM into the learning experience, as was done in the deliberate student preparation group of interventions, will lead to better outcomes for students. Further, additional to the aim of developing students’ clinical skills, there should be explicit goals to support the development of work readiness attributes [14] including: interpersonal capabilities such as confidence in developing professional relationships; practical wisdom or confidence in making deliberate, effective and appropriate decisions; organisational acumen or the navigation of administrative and cultural elements of the workplace; as well as supporting the development of personal attributes such as resilience, flexibility, adaptability and having a growth mindset for themselves and others [3, 4, 14, 59]. Whilst acknowledging that it is not feasible to design a single placement to address students’ needs to develop the full gamut of work ready attributes, the findings of our review suggest it is possible for a well-designed NPM placement to offer a range of learning opportunities to support the development of work readiness of both senior and junior students.
NPM placements can be designed in a way that ensures experiences exist to scaffold learning, where educators understand the theoretical basis for such approaches. For example, pro-bono university-based clinics can be carefully structured to ensure opportunities for lower-risk service activities by having senior students who are already familiar with the service and placement model support junior students to take responsibility for these activities. Entrustment of lower risk activities to the senior-junior student dyad builds a sense of responsibility in both senior and junior students [32]. It also creates a culture of preparing students for future educator roles, where senior students are supported and expected to develop and exercise educator skills as part of their degree. As reported in some of the studies in this review, acting in an educator role also appears to develop senior students’ sense of clinical competence, professional reasoning, and independent practice [6, 47,48,49, 58]. It appears that with more responsibility for service user care, comes a growing sense of agency by senior students as they move towards being a fully-fledged clinician. Designing for learning moves beyond the co-location models reviewed in this study that, although generating perceptions of safety and collaborative learning, are less intentional in developing students’ educator skills. As has been recommended in same level PAL, [10] achieving these outcomes requires the preparation of both educators and students in the theory and application of NPM education strategies as part of deliberate design for learning.
Evaluate beyond student and/or educator satisfaction
For student outcomes, more elaborate evaluation is needed, beyond Kirkpatrick’s Level 1, satisfaction with education interventions [41]. Future studies could focus on student performance on relevant assessments, and/or tracking students longitudinally to understand what types of future mentoring, leadership and educator roles they engage with as graduates, and how NPM experiences have shaped their educator and professional practice, that is, Kirkpatrick’s Level 4 [41]. Furthermore, teamwork and collaborative capabilities developed in NPM might influence how graduates work in multidisciplinary teams with peers and how they engage in supervision relationships and lifelong learning i.e. Kirkpatrick’s Levels 2 and 3 [41]. While some of these aspects have been revealed through qualitative, open-ended studies included in this review, [9, 51, 55, 56] they should be more systematically investigated across cohorts.
Beyond students, there might be efficiencies in investigating educator and service user outcomes simultaneously, since they overlap. While service user [60] and educator satisfaction is important, additional metrics might usefully focus on occasions of service (how many times a service was utilised), clinician time-use, service staffing profile (where students become integral to the service enabling existing staff to be deployed elsewhere) along with meeting service key performance indicators (KPIs) such as progression along clinical care pathways, and/or waitlist lengths and discharge destination (e.g. rehabilitation, care facility or home). In addition, career progression for educators (such as formal leadership, supervision and educator roles) could also be investigated. Some of these metrics have been examined for allied health placements in general, [61, 62] but not for NPM placements in this review.
Finally, it was apparent that few studies followed any reporting guidelines for qualitative studies, for example using the Standards for Reporting of Qualitative Research (SRQR) [50]. The use of such standards when reporting on studies undertaken not only support high quality publications but may also assist researchers in planning and undertaking higher quality research, the findings of which can be confidently applied in the practice context.
Use learning theories to interpret NPM outcomes
In recommending further research be conducted in this area, we echo recent exhortations to more explicitly adopt and incorporate learning theory within health professions education in both framing the phenomenon or intervention of interest and developing relevant and appropriate research designs [63,64,65]. Authors of the studies identified a number of educational theories that informed the design of the NPM placements including communities of practice (with legitimate peripheral participation [33, 66]), peer learning theories, [26, 67] cognitive apprenticeship, [68] social constructivist [23] and experiential learning [22]. What is not clear from this review is which of these theories are core to the design of NPM placements or which contributes most to which learning outcomes. Further research could assist placement designers to select the most appropriate learning theory or theories to inform the design of their placement models to achieve the desired learning outcomes.
Whilst it can be challenging for researchers, the use of theory and theoretical frameworks in health professions education supports understanding of the mechanics and meaning of complex phenomena such as learning environments, learning relationships and learning outcomes [64, 65]. It also assists educators and WIL placement providers to identify the usefulness, relevance and application of findings from individual studies as they work to implement innovative placement models such as NPM [63, 64]. Conversely, failing to engage with theory in this domain risks the implementation of ineffective education programs that do not meet the goals of placement design, and research that lacks transparency, integrity and rigor [63, 64].
Limitations
This systematic review aimed to examine the design and outcomes of NPM WIL placements for allied health students. The findings presented draw only from peer-reviewed articles published in English with no searching of the grey literature or citation tracking. Thus, we acknowledge that this narrower focus may have excluded studies across the globe and informal reports, particularly where professions may still be establishing, and a paucity of educators may lead to more creative placement models. The search was also restricted from 2003 to 2022, with the aim of capturing studies not found by Burch et al. [43] in their earlier systematic review on the same topic. It is possible that our selection of search teams and databases may have led to some studies being omitted, however the use of a range of professions, along with a broader use of descriptions for the placement model has addressed this potential limitation. Finally, we acknowledge that a degree of individual judgement was exercised when searching the included articles for the educational pedagogy and/or teaching/learning methods. Having multiple authors involved in the screening, data extraction and data analysis, working independently before comparing and clarifying, mitigated this limitation.
Conclusion
There is growing evidence for positive student outcomes of NPM in terms of both satisfaction and opportunities to further develop work ready attributes and characteristics. However, the evidence for educator and service user outcomes remains sparse. Based on the findings of this review, there are two clear actions for universities, their partner site educators and health profession education researchers to consider. Firstly, to continue to use NPM solely as a means of addressing placement shortages is a disservice to health professions education, and this model specifically. If the objectives of a placement are to support students’ development of work-ready attributes and discipline-specific knowledge and skills, then NPM could be the placement model of choice. Secondly, in specifically designing for these outcomes, suitable educational theories should be used to inform the design of both the placement and research to address the evidence gaps. Making careful and deliberate choices in educational and research design and reporting will increase the potential for richer, evidence-based learning experiences for students as well as improved outcomes for educators and service users.
Availability of data and materials
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request.
Notes
Across healthcare, a range of terms are used for the person accessing the service including patient, client, consumer or service user. In this paper, service user will be used.
Abbreviations
- BscPhm:
-
Bachelor of Science in Pharmacy
- NPM:
-
Near-peer mentor/mentoring
- OT:
-
Occupational therapy
- OTA:
-
Occupational Therapy Assistants
- PAL:
-
Peer-assisted learning
- Pharm D:
-
Doctor of Pharmacy
- PT:
-
Physiotherapy or Physical Therapy
- PTA:
-
Physical Therapy Assistants
- WIL:
-
Work Integrated Learning
- ZPD:
-
Zone of Proximal Development
- KPI:
-
Key Performance Indicators
References
Orr P, Forsyth L, Caballero C, Rosenberg C, Walker A. A systematic review of Australian higher education students’ and graduates’ work readiness. High Educ Res Dev. 2023;42(7):1714–31.
Walker A, Campbell K. Work readiness of graduate nurses and the impact on job satisfaction, work engagement and intention to remain. Nurse Educ Today. 2013;33(12):1490–5.
O’Leary N, Cantillon P. Why shouldn’t we do that on placement if we’re doing it in the real world? Differences between undergraduate and graduate identities in speech and language therapy. Adv Health Sci Educ Theory Pract. 2020;25(4):781–97.
Attrill SL, McAllister S, Brebner C. Not too little, not too much: supervisor perceptions of work-readiness of speech-language pathology graduates. Adv Health Sci Educ Theory Pract. 2022;27(1):87–106.
Gazula S, McKenna L, Cooper S, Paliadelis P. A Systematic Review of Reciprocal Peer Tutoring within Tertiary Health Profession Educational Programs. Health Professions Education. 2017;3(2):64–78.
Collins J, Mowder-Tinney JJ. The Apprentice Clinical Instructor (ACI): a mentor/protégé model for Capstone-Integrated Clinical Education (C-ICE). J Phys Therapy Educ. 2012;26(3):33–9.
Briffa C, Porter J. A systematic review of the collaborative clinical education model to inform speech-language pathology practice. Int J Speech Lang Pathol. 2013;15(6):564–74.
Sevenhuysen S, Thorpe J, Barker LA, Keating JL, Molloy EK, Haines T. Education in peer learning for allied health clinical educators: A mixed methods study. Focus on Health Professional Education-a Multidisciplinary J. 2017;18(2):4–18.
Dockter M, Roller J, Eckert J. Preparing physical therapy students for the role of clinical educator: a case study report. Work. 2013;44(3):255–63.
Sevenhuysen S, Thorpe J, Molloy E, Keating J, Haines T. Peer-Assisted Learning in Education of Allied Health Professional Students in the Clinical Setting: A Systematic Review. J Allied Health. 2017;46(1):26–35.
Pope K, Barclay L, Dixon K, Kent F. Models of pre-registration student supervision in allied health: A scoping review. Focus on Health Professional Education-a Multidisciplinary J. 2023;24(2):27–62.
Chesterton P, Chesterton J, Alexanders J. New graduate physiotherapists’ perceived preparedness for clinical practice. A cross-sectional survey. European J Physiotherapy. 2021;25(1):33–42.
Padley J, Boyd S, Jones A, Walters L. Transitioning from university to postgraduate medical training: A narrative review of work readiness of medical graduates. Health Sci Rep. 2021;4(2):e270.
Caballero CL, Walker A, Fuller-Tyszkiewicz M. The Work Readiness Scale (WRS): Developing a measure to assess work readiness in college graduates. Journal of Teaching and Learning for Graduate Employability. 2011;2(1):41–54.
Markowski M, Bower H, Essex R, Yearley C. Peer learning and collaborative placement models in health care: a systematic review and qualitative synthesis of the literature. J Clin Nurs. 2021;30(11–12):1519–41.
Liljedahl M, Bjorck E, Bolander LK. How workplace learning is put into practice: contrasting the medical and nursing contexts from the perspective of teaching and learning regimes. Adv Health Sci Educ Theory Pract. 2023;28(3):811–26.
Kasper B, Brownfield A. Evaluation of a Newly Established Layered Learning Model in an Ambulatory Care Practice Setting. Curr Pharm Teach Learn. 2018;10(7):925–32.
Irvine S, Williams B, McKenna L. How are we assessing near-peer teaching in undergraduate health professional education? A systematic review Nurse Educ Today. 2017;50:42–50.
Olaussen A, Reddy P, Irvine S, Williams B. Peer-assisted learning: time for nomenclature clarification. Med Educ Online. 2016;21:30974.
Tai J, Molloy E, Haines T, Canny B. Same-level peer-assisted learning in medical clinical placements: a narrative systematic review. Med Educ. 2016;50(4):469–84.
Yu TC, Wilson NC, Singh PP, Lemanu DP, Hawken SJ, Hill AG. Medical students-as-teachers: a systematic review of peer-assisted teaching during medical school. Adv Med Educ Pract. 2011;2:157–72.
Yardley S, Teunissen PW, Dornan T. Experiential learning: transforming theory into practice. Med Teach. 2012;34(2):161–4.
Mann KV. Theoretical perspectives in medical education: past experience and future possibilities. Med Educ. 2011;45(1):60–8.
Ericsson KA, Krampe RT, Teschromer C. The Role of Deliberate Practice in the Acquisition of Expert Performance. Psychol Rev. 1993;100(3):363–406.
Medina MS, Castleberry AN, Persky AM. Strategies for Improving Learner Metacognition in Health Professional Education. Am J Pharm Educ. 2017;81(4):78.
Vygotsky LS, Cole M. Mind in Society: The Development of Higher Psychological Processes. Cambridge: United States of America: Harvard University Press; 1978.
Loda T, Erschens R, Loenneker H, Keifenheim KE, Nikendei C, Junne F, et al. Cognitive and social congruence in peer-assisted learning - A scoping review. PLoS ONE. 2019;14(9):e0222224.
Loda T, Erschens R, Nikendei C, Zipfel S, Herrmann-Werner A. Qualitative analysis of cognitive and social congruence in peer-assisted learning - The perspectives of medical students, student tutors and lecturers. Med Educ Online. 2020;25(1):1801306.
Arruzza E. Teaching students to mentor: Near-peer mentoring in undergraduate medical radiation science education. J Med Imaging Radiat Sci. 2023;54(1):23–7.
Howkins EJ, Ewens A. How students experience professional socialisation. Int J Nurs Stud. 1999;36(1):41–9.
McKenna L, Williams B. The hidden curriculum in near-peer learning: An exploratory qualitative study. Nurse Educ Today. 2017;50:77–81.
Bramley AL, McKenna L. Entrustable professional activities in entry-level health professional education: A scoping review. Med Educ. 2021;55(9):1011–32.
Wenger E. Communities of practice: Learning, meaning, and identity. Cambridge, United Kingdom: Cambridge University Press; 1998.
Trede F, Macklin R, Bridges D. Professional identity development: a review of the higher education literature. Stud High Educ. 2012;37(3):365–84.
Byrne C, Mcknight J, Roberts J, Rankin J. Learning Clinical Teaching Skills at the Baccalaureate Level. J Adv Nurs. 1989;14(8):678–85.
Ladyshewsky RK. Enhancing service productivity in acute care inpatient settings using a collaborative clinical education model. Phys Ther. 1995;75(6):503–10.
Tiberius R, Gaiptman B. The Supervisor-Student Ratio: 1:1 versus 1:2. Can J Occup Ther. 2016;52(4):179–83.
Secomb J. A systematic review of peer teaching and learning in clinical education. J Clin Nurs. 2008;17(6):703–16.
Loewen P, Legal M, Gamble A, Shah K, Tkachuk S, Zed P. Learner : preceptor ratios for practice-based learning across health disciplines: a systematic review. Med Educ. 2017;51(2):146–57.
Carey MC, Kent B, Latour JM. Experiences of undergraduate nursing students in peer assisted learning in clinical practice: a qualitative systematic review. JBI Database System Rev Implement Rep. 2018;16(5):1190–219.
Cahapay MB. Kirkpatrick Model: Its Limitations as Used in Higher Education Evaluation. International Journal of Assessment Tools in Education. 2021;8(1):135–44.
Penman M, Evans G, Tai J, Brentnall J, Judd B. Near peer mentoring in allied health clinical education: effects for allied health students, their educators and service users - a systematic review. PROSPERO: International prospective register of systematic reviews. 2018. Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018102790.
Burch C, Guthrie P, Kidd M, Lewis C, Smiler P. Near-peer learning in clincial education: a systematic review. Focus on Health Professional Education: A Multi-Disciplinary J. 2010;11:1–21.
Irvine S, Williams B, McKenna L. Near-peer teaching in undergraduate nurse education: An integrative review. Nurse Educ Today. 2018;70:60–8.
Allied Health Professions Australia. Allied Health Professions 2023. Available from: https://ahpa.com.au/allied-health-professions/.
Covidence systematic review software. Veritas Health Innovation. Available from: https://www.covidence.org. Cited 30 October 2019
Cicinelli E, Leblanc K, Cameron K, Fernandes O, McIntyre C, Bjelajac Mejia A, et al. An analysis of Canadian doctor of pharmacy hospital preceptor experiences in alternative preceptor models. Curr Pharm Teach Learn. 2021;13(4):353–60.
MacDonald M, Thompson AE, Ton J, Mysak T. Strategies to optimize implementation of novel preceptorship models: Peer-assisted learning and near-peer teaching. Curr Pharm Teach Learn. 2020;12(8):945–55.
McIntyre C, Natsheh C, Leblanc K, Fernandes O, Mejia AB, Raman-Wilms L, et al. An Analysis of Canadian Doctor of Pharmacy Student Experiences in Non-Traditional Student-Preceptor Models. Am J Pharm Educ. 2019;83(10):7367.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51.
Leong C, Battistella M, Austin Z. Implementation of a near-peer teaching model in pharmacy education: experiences and challenges. Can J Hosp Pharm. 2012;65(5):394–8.
Sharif-Chan B, Tankala D, Leong C, Austin Z, Battistella M. An Observational Case Study of Near-peer Teaching in Medical and Pharmacy Experiential Training. Am J Pharm Educ. 2016;80(7):114.
Black JD, Bauer KN, Spano GE, Voelkel SA, Palombaro KM. Grand Rounds: A method for improving student learning and client care continuity in a student-run physical therapy pro bono clinic. J Scholar Teach Learn. 2017;17:68–88.
Boniface G, Seymour A, Polglase T, Lawrie C, Clarke M. Exploring the nature of peer and academic supervision on a role-emerging placement. Br J Occup Ther. 2012;75(4):196–201.
Foxwell AA, Kennard BD, Rodgers C, Wolfe KL, Cassedy HF, Thomas A. Developing a Peer Mentorship Program to Increase Competence in Clinical Supervision in Clinical Psychology Doctoral Training Programs. Acad Psychiatry. 2017;41(6):828–32.
Kucharski-Howard J, Babin CJ, Inacio CA, Tsoumas LJ. DPT student perceptions about developing mentoring skills: A progressive model. J Allied Health. 2019;48(2):108–13.
Jelley W, Larocque N, Patterson S. Intradisciplinary clinical education for physiotherapists and physiotherapist assistants: a pilot study. Physiother Can. 2010;62(1):75–80.
Jung B, Salvatori P, Martin A. Intraprofessional fieldwork education: occupational therapy and occupational therapist assistant students learning together. Can J Occup Ther. 2008;75(1):42–50.
O’Brien M, Troy K, Kirkpatrick J. The Allied Health Work Readiness Study: Identifying Personal Characteristics Signalling Work Readiness in Allied Health Students. Internet Journal of Allied Health Sciences and Practice. 2020;18(1):5.
Patterson F, Doig E, Fleming J, Strong J, Birch S, Whitehead M, et al. Student-resourced service delivery of occupational therapy rehabilitation groups: patient, clinician and student perspectives about the ingredients for success. Disabil Rehabil. 2022;44(18):5329–40.
Bourne E, McAllister L, Nagarajan S, Short K. The effect of speech-language pathology students on clinician time use and activity. Int J Speech Lang Pathol. 2019;21(2):163–74.
Bourne E, Short K, McAllister L, Nagarajan S. The quantitative impact of placements on allied health time use and productivity in healthcare facilities: A systematic review with meta-analysis. Focus on Health Professional Education-a Multidisciplinary J. 2019;20(2):8–40.
Rees CE, Monrouxe LV. Theory in medical education research: how do we get there? Med Educ. 2010;44(4):334–9.
Samuel A, Konopasky A, Schuwirth LWT, King SM, Durning SJ. Five Principles for Using Educational Theory: Strategies for Advancing Health Professions Education Research. Acad Med. 2020;95(4):518–22.
Varpio L, Ellaway RH. Shaping our worldviews: a conversation about and of theory. Adv Health Sci Educ Theory Pract. 2021;26(1):339–45.
Lave J, Wenger E. Situated learning: Legitimate peripheral participation: Cambridge, United Kingdom: Cambridge University Press; 1991.
Topping KJ. The effectiveness of peer tutoring in further and higher education: A typology and review of the literature. High Educ. 1996;32(3):321–45.
Lyons K, McLaughlin JE, Khanova J, Roth MT. Cognitive apprenticeship in health sciences education: a qualitative review. Adv Health Sci Educ Theory Pract. 2017;22(3):723–39.
Acknowledgements
The authors acknowledge the valuable feedback provided by Professor Lynn Monrouxe on earlier draft of this manuscript.
Funding
The first author was supported in part by the Special Studies Program of The University of Sydney.
Author information
Authors and Affiliations
Contributions
All authors conceptualised the study, MP performed the database searches, MP, JT and GE completed data extraction and quality review. All authors completed data analysis and interpretation, drafted, edited and finalised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Penman, M., Tai, J., Evans, G. et al. Designing near-peer mentoring for work integrated learning outcomes: a systematic review. BMC Med Educ 24, 937 (2024). https://doi.org/10.1186/s12909-024-05900-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05900-6