Abstract
Background
A 3.0-mm ultrathin bronchoscope (UTB) with a 1.7-mm working channel provides better accessibility to peripheral bronchi. A 4.0-mm thin bronchoscope with a larger 2.0-mm working channel facilitates the use of a guide sheath (GS), ensuring repeated sampling from the same location. The 1.1-mm ultrathin cryoprobe has a smaller diameter, overcoming the limitation of the size of biopsy instruments used with UTB. In this study, we compared the endobronchial ultrasound localization rate and diagnostic yield of peripheral lung lesions by cryobiopsy using UTB and thin bronchoscopy combined with GS.
Methods
We retrospectively evaluated 133 patients with peripheral pulmonary lesions with a diameter less than 30 mm who underwent bronchoscopy with either thin bronchoscope or UTB from May 2019 to May 2023. A 3.0-mm UTB combined with rEBUS was used in the UTB group, whereas a 4.0-mm thin bronchoscope combined with rEBUS and GS was used for the thin bronchoscope group. A 1.1-mm ultrathin cryoprobe was used for cryobiopsy in the two groups.
Results
Among the 133 patients, peripheral pulmonary nodules in 85 subjects were visualized using r-EBUS. The ultrasound localization rate was significantly higher in the UTB group than in the thin bronchoscope group (96.0% vs. 44.6%, respectively; P < 0.001). The diagnostic yield of cryobiopsy specimens from the UTB group was significantly higher compared to the thin bronchoscope group (54.0% vs. 30.1%, respectively; p = 0.006). Univariate analysis demonstrated that the cryobiopsy diagnostic yields of the UTB group were significantly higher for lesions ≤ 20 mm, benign lesions, upper lobe lesions, lesions located lateral one-third from the hilum, and lesions without bronchus sign.
Conclusions
Ultrathin bronchoscopy combined with cryobiopsy has a superior ultrasound localization rate and diagnostic yield compared to a combination of cryobiopsy and thin bronchoscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Lung cancer is characterized by high prevalence globally and is the leading cause of cancer-related deaths [1]. In recent years more and more patients with peripheral pulmonary nodules (PPNs) are successfully diagnosed owing to advances in lung cancer screening through chest computed tomography (CT) scans [2, 3]. Obtaining tissue from PPNs for pathological examination to confirm a diagnosis is crucial due to the potential of malignant transformation [4]. CT-guided transthoracic needle biopsy (CT-TTNB) is a safe and effective method [5]. However, application of this method is limited by exposure to radiation and high rates of complications such as bleeding and pneumothorax. In addition, smaller lesion size is a major risk factor for high complication rates [6]. Bronchoscopy is a promising alternative to CT-TTNB, owing to its high efficacy and safety.
The diagnostic yield of PPNs by bronchoscopy has significantly increased owing to advances in various ancillary technologies such as radial endobronchial ultrasound (rEBUS), virtual bronchoscopic navigation (VBN), electromagnetic navigational bronchoscopy, and ultrathin bronchoscopy [7,8,9,10]. Combining 3.0-mm UTB with rEBUS is effective for PPNs diagnosis [11,12,13]. Studies demonstrated that use of ultrathin bronchoscopy as an adjunctive examination approach for thin bronchoscopy significantly enhances the ultrasound localization rate and the diagnostic yield of PPNs [14, 15]. However, the thin diameter in UTB restricts the size of biopsy instruments, resulting in smaller biopsy specimens compared to traditional forceps biopsy approach. Cryobiopsy facilitates the collection of larger and higher quality specimens compared to forceps biopsy [16]. Previous findings demonstrated that the diagnostic yield of PPNs using rEBUS was significantly higher when the probe was within the lesion rather than adjacent to it [17]. This may be due to the difficulty of forceps biopsy to obtain tissue from the lateral side of the lesions. However, a previous study demonstrated that conducting cryobiopsy with the rEBUS probe positioned adjacent to the lesions exhibits relatively similar diagnostic yields compared to placing the probe within the lesions [18].
Smaller diameter cryoprobes have been developed in recent years [19, 20]. The ultrathin cryoprobes with a 1.1-mm diameter are more flexible than conventional cryoprobes, overcoming the limitations associated with conventional cryoprobes and forceps biopsy. Therefore, our objective was to evaluate the value of ultrathin bronchoscopy in improving the endobronchial ultrasound localization rate and enhancing the cryobiopsy diagnostic yield of PPNs.
Materials and methods
Patients
Patients with unexplained solitary peripheral pulmonary nodules (PPNs) who attended the First Affiliated Hospital of Ningbo University from May 2019 to May 2023 were enrolled into the study. The main inclusion criterion was having a localized pulmonary lesion with the longest diameter < 30 mm under chest computed tomography, which required biopsy for diagnosis. The main exclusion criteria were as follows: subjects with central pulmonary lesions, the target lesions were directly visualized through bronchoscopy, cases lacking a final diagnosis or with incomplete follow-up. A total of 133 subjects were enrolled into the study, with 83 consecutive patients from May 2019 to August 2022 assigned into the thin bronchoscope group, and 50 consecutive patients from September 2022 to May 2023 were assigned into in the UTB group. The UTB technique was implemented in our hospital from September 1, 2022. This study was approved by the ethics committee of the First Affiliated Hospital of Ningbo University (Protocol No. KS20224007).
Procedures
All patients underwent chest CT scan prior to the bronchoscopy examination. All endoscopic procedures were performed by two experienced physicians at the Respiratory Endoscopy Center of the First Affiliated Hospital of Ningbo University. All patients received lidocaine for local anesthesia of the pharynx, and intravenous propofol and fentanyl for general anesthesia. A laryngeal mask airway was used ensure airway patency in the patients.
UTB Group: A 3.0-mm UTB (BF-MP290F; Olympus, Tokyo, Japan) with a 1.7-mm working channel was advanced as close as possible to the target lesion. When the UTB was sufficiently close to the lesion, a 1.4-mm diameter radial endobronchial ultrasound (rEBUS) probe (UM-S20-17 S; Olympus) was inserted through the working channel and advanced towards the lesion. Once the rEBUS probe was positioned as possible as to the center of the lesion, its location would be recorded and the position of the bronchoscope would be maintained. The distance from the entrance of the bronchoscope to the lesion was determined using the rEBUS probe. Subsequently, the probe wasremoved while maintaining the bronchoscope in the exact same position. A marker (stop clip from the K-201 biopsy kit) was applied over the cryoprobe, aligning its length with the measured distance to the lesion. Brush cytology and forceps biopsy were sequentially performed using the K-201 biopsy kit. The brush cytology was performed in duplicates and five replicates were performed for the forceps biopsy. Subsequently, an ultrathin cryoprobe with a 1.1-mm diameter (No. 20402-402; Erbe, Tubingen, Germany) was used for cryobiopsy. Before conducting cryobiopsy for each patient, the operator determined the freezing capacity of the cryoprobe in vitro by estimating the duration required for the wet cryoprobe to form an ice-ball with a diameter of 2–3 mm and this duration was used for performing the cryobiopsy. The freezing time typically lasted 4 s. After freezing, the cryoprobe and bronchoscope were removed together. The specimen was thawed and transferred into a formalin bottle. The target number of specimen was one. After each cryobiopsy, if necessary, the location of the lesion was reconfirmed by the rEBUS probe. Fluoroscopic guidance was not performed during the procedure to minimize radiation exposure. Bronchoalveolar lavage was performed only on the target bronchus for ethical considerations, if the lesion was invisible on the rEBUS image.
Thin Bronchoscope Group: The basic procedure was similar to the UTB group. A 4.0-mm thin bronchoscope (BF-P260F/BF-F260/BF-260; Olympus, Tokyo, Japan) with a 2.0-mm working channel was used. A rEBUS probe with 1.4-mm diameter (UM-S20-17 S; Olympus) and a 1.95-mm guide sheath (GS) were inserted into the working channel when the bronchoscope was sufficiently close to the lesion. The bronchus was selected when the rEBUS was located as close as possible to the center of the lesion. Subsequently, the probe was withdrawn and brushing, forceps biopsy, and cryobiopsy were conducted as described in the UTB group. Only bronchoalveolar lavage was performed for lesions which could not be visualized by rEBUS. Fluoroscopy was not conducted during the entire procedure.
Bleeding is common during cryobiopsy. However, bleeding is effectively controlled by performing the procedure using angioplasty balloon [21, 22], two-scope technique [23, 24] and rigid bronchoscope [25]. These instruments were not used in the present study. A flexible video bronchoscope was used to minimize bleeding. After the bronchoscope and the cryoprobe were withdrawn, another endoscopic operator promptly inserted the flexible video bronchoscope to observe the bleeding status.
Diagnosis
The histological and cytological results were interpreted by experienced pathologists. Histological findings that resulted in a definitive diagnosis (such as malignant and benign tumors, granulomatous inflammation, organizing pneumonia, and fungal infection) were considered diagnostic. Uncertain histological findings, such as non-specific fibrosis and inflammation, were considered non-diagnostic [26, 27]. The final diagnosis was determined based on pathological results, microbiological analysis or clinical follow-up. Benign lesions that could not be diagnosed by pathological or microbiological methods were confirmed radiologically and clinically. All patients with non-diagnostic lesions were followed up for at least 1 year after bronchoscopy to monitor lesion reduction or disappearance.
Endpoints
The primary endpoint in this study was the ultrasonographic localization rate (number of patients with ‘within’ or ‘adjacent to’ the image/total number of patients) and the diagnostic yield of cryobiopsy. The secondary endpoints included the safety and cryobiopsy diagnostic yields based on the nature of the lesion (benign or malignant), lesion size, lesion location, and ultrasonic probe location on the rEBUS image. Bleeding occurrences were graded as follows: 0, no bleeding; 1, mild bleeding that required bronchoscopy suctioning, without other endoscopic procedures; 2, moderate bleeding that required bronchoscopy occlusion-collapse and/or cold saline instillation; 3, severe bleeding leading to hemodynamic or respiratory instability, requiring tamponade, surgical interventions, blood transfusion or admission to the intensive care unit [28].
Statistical analysis
Statistical analysis were performed using the SPSS software version 26 (SPSS Inc., Chicago, Illinois). Categorical variables were analyzed using the Pearson’s chi-square test or Fisher exact test. Continuous variables were analyzed using the Mann-Whitney U test. A p-value < 0.05 was considered significant.
Results
Patients and lesions
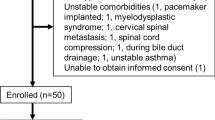
The 168 patients were diagnosed with PPNs through chest CT scans and accepted bronchoscopy examination (Fig. 1). Two patients were excluded from the study due to presence of visible lesions under bronchoscopy, and 33 patients were excluded due to undiagnosed or incomplete follow-up. The remaining 133 patients were included in the study, with 83 patients assigned into the thin bronchoscope group and 50 patients assigned into the UTB group. Baseline characteristics of the patients and lesions were not significantly different between the two groups (Table 1). The bronchoscopy findings and final diagnosis are shown in Table 2.
Ultrasonographic localization rate and diagnostic yields
The location of the rEBUS probe relative to the lesion significantly improved when an UTB was used(P < 0.001; Table 3). The ultrasound localization rates in the thin bronchoscope group and UTB group were 44.6% and 96.0%, respectively. The diagnostic yield of cryobiopsy was significantly higher in the UTB group than in the thin bronchoscope group (54.0% vs. 30.1%, respectively; p = 0.006). The yields of different biopsy methods between the two group were compared, indicating that the UTB group exhibited higher diagnostic yields than the thin bronchoscope group. In the UTB group, the diagnostic yield of cryobiopsy combined with forceps biopsy was higher compared to cryobiopsy alone. However, when comparing the lesions visualized by the rEBUS probe in both groups, there was no statistically significant difference observed in the diagnostic yield obtained through various biopsy methods between the two groups (Table 4). The mean freezing time in the thin bronchoscope group and the UTB group were 4.84 s (range, 3–8 s) and 3.75 s (range, 3–4 s), respectively (p < 0.001). The number of specimens retrieved by cryobiopsy was not significantly different between the groups (a mean of 1.19 in the thin bronchoscope group and 1.15 in the UTB group; p = 0.442).
The diagnostic yields of the cryobiopsy method in the thin bronchoscopy group and UTB group were 30.1% (25 of 83) and 54.0% (27 of 50), respectively (P = 0.006; Table 5). Larger lesions, malignant nature, lesions located in the middle one-third from the hilum, and the presence of bronchus sign were associated with higher diagnostic yield in the two groups. Univariate analysis demonstrated that the diagnostic yields of the UTB group were significantly higher for lesions ≤ 20 mm, benign lesions, upper lobe lesions, lesions located in the lateral one-third from the hilum, and lesions without bronchus signs compared to the diagnostic yields in the thin bronchoscope group. Among the 37 lesions visualized by the rEBUS probe in the thin bronchoscope group, specimens could not be obtained from 13 lesions using forceps biopsy, including 7 benign lesions. Among the 48 lesions visualized by the rEBUS probe in the UTB group, specimens could not be obtained from 7 lesions using forceps biopsy, including 5 benign lesions.
Safety
Adverse events are presented identified in this study in Table 6. The 85 subjects with lesions visualized by the rEBUS probe did not exhibit iatrogenic pneumothorax, procedure-related lung infection, or mortality. There were no statistically significant differences in the number of adverse events between the UTB and thin bronchoscope groups (18 of 48 [37.5%] vs. 20 of 37 [54.1%], respectively;P = 0.128).
Discussion
The UTB has better accessibility and bronchial selectivity compared with the thin bronchoscope. In a previous randomized study, Oki et al. observed that ultrathin bronchoscopy effectively detects more distal bronchi than thin bronchoscopy. The mean segmental bronchial generation detected using UTB, thin bronchoscopy, and VBN were 5.5, 4.4, and 5.1, respectively [13]. These results indicate that UTB is more effective in identifying the bronchial path than using direct vision under the guidance of VBN under direct vision, improving the operability for peripheral small bronchi.
Previous studies reported that the position of rEBUS probe relative to the lesion is an important predictive factor for diagnosing the lesion [29]. Therefore, it is imperative to improve the ultrasound localization rate to reduce non-diagnostic results in cases with “invisible” images that cannot be processed. Using UTB as an adjunct to thin bronchoscopy significantly improves the relative position of the radial ultrasound probe and the diagnostic yield of peripheral pulmonary lesions [14, 15]. Nishii et al. conducted a retrospective study comprising 44 cases that were ‘adjacent to’ and ‘invisible’ under the rEBUS imaging. The location of the rEBUS probe improved significantly to the lesion after replacing thin bronchoscopy with ultrathin bronchoscopy. The results showed that among the 12 patients with ‘adjacent’ images, the rEBUS position was upgraded to ‘within’ images in 8 patients. In addition, among the 32 patients with “invisible” images, the rEBUS images were upgraded in 26 patients [14]. Moreover, Oki et al. conducted a multicenter prospective study comprising 87 patients who had undergone both thin bronchoscopy and ultrathin bronchoscopy. The relative position of the rEBUS probe to the lesion improved significantly when ultrathin bronchoscopy was conducted (P < 0.001).The rates were 44.8% and 82.8% under the thin bronchoscopy and ultrathin bronchoscopy, respectively [15]. In our retrospective study, a significantly higher ultrasound localization rate was observed in the ultrathin bronchoscopy group compared to the thin bronchoscopy group (44.6% vs. 96.0%, respectively; P < 0.001), consistent with previous findings.
The narrow working channel of ultrathin bronchoscopy limits the size of biopsy instruments that can be used and limits the size of specimens can be obtained. The specimen size can be controlled by increasing the freezing time. The sample can be obtained through the bronchoscope as a whole instead of using the working channel. These factors ensure that larger specimens obtained and higher histological quality is achieved when performing cryobiopsy with ultrathin bronchoscopy, ultimately improving the diagnostic yield. Several factors affect the freezing time, including the cryosurgical system (ERBE CA vs. ERBE CA II), the type of freezing gas and the characteristics of the biopsied lung tissue [28]. The cryosurgical system (ERBE CA) and the freezing gas (carbon dioxide) were not changed during this study. The pressure of the carbon dioxide gas is an important factor that affects the freezing time during the cryobiopsy procedure. Therefore, we evaluated the freezing capacity of the cryoprobe before performing the cryobiopsy procedure to estimate the freezing time required to collect sufficient samples. (The freezing time was estimated based on the time it takes for the ice-ball’s diameter to reach 2–3 mm). In this study, we observed that the freezing time in the thin bronchoscope group was significantly longer than in the UTB group. This difference in freezing time can be attributed to the variation in carbon dioxide pressure, resulting in a greater dispersion degree in the freezing time in the thin bronchoscope group. Oki et al. (2023) conducted a prospective study comprising 50 subjects who underwent forceps biopsy and cryobiopsy under the guidance of ultrathin bronchoscopy and rEBUS. The findings showed that feasibility of cryobiopsy was 98%. In addition, the median size of specimens obtained by cryobiopsy was significantly larger than the size obtained by forceps biopsy (7.0 mm2 vs. 1.3 mm2, respectively; P < 0.001). The diagnostic yields of forceps biopsy, cryobiopsy, and a combination of the two methods were 54% (27/50), 62% (31/50), and 74% (37/50), respectively [27]. Kim et al. reported that using a 1.1-mm cryoprobe for transbronchial cryobiopsy of peripheral pulmonary lesions is an effective and reliable method, which is not associated with serious complications. [30]. In summary, cryobiopsy with ultrathin bronchoscopy is a feasible and safe method for diagnosing of small peripheral lung lesions.
Bronchoscopy has varying diagnostic rates depending on the lesion size, lesion characteristics, lobar location of the lesion, lesion location from the hilum and presence of bronchus signs. A previous meta-analysis demonstrated that larger lesions (> 20 mm), presence of bronchus signs, and malignancy were associated with higher diagnostic yields [31]. The findings from a prospective multicenter study demonstrated a correlation between lesions located in non-upper lobes and higher diagnostic yield through multivariate analysis [32]. TAY et al. reported that lesions larger than 20 mm, malignant nature, and lesions located within 50 mm from the hilum are associated with enhancing location rate of rEBUS [33]. A prospective study revealed that the forceps biopsy diagnostic yields of the UTB method for non-upper lobe lesions, lesions located in the peripheral one-third of the lung, benign lesions, lesions > 20 mm, and pleural lesions were significantly higher compared to the use of thin bronchoscopy. Notably, logistic regression analysis demonstrated that these factors were not associated with higher diagnostic yields of UTB [13]. The present findings demonstrated that ultrathin bronchoscopic cryobiopsy has advantages over bronchoscopic fibroscopy, with higher diagnostic yields for smaller lesions, benign lesions, upper lobe lesions, lesions in the lateral one-third from the hilum, and lesions without bronchial sign. This finding partially indicates that cryobiopsy can be used to circumvent the limitation of ultrathin bronchoscopy of the size of the biopsy instruments, improving the diagnostic yields for smaller lesions. In addition, the flexibility of the cryoprobe and the higher ultrasound localization rate of ultrathin bronchoscopy enhance the diagnostic yield of upper lobe lesions.
This study had some limitations. This was a retrospective, single-center study, and experience and skills are essential factors for achieving good diagnostic yield. Therefore, the results may not be generalizable to other inexperienced institutions. In addition, the study had a small sample size. In this study, we observed that the diagnostic yield of the cryobiopsy combined with forceps biopsy was higher than using the cryobiopsy alone in the UTB group. A randomized, prospective study with a larger sample size should be conducted to verify if a combination of cryobiopsy and forceps biopsy has higher diagnostic yields than cryobiopsy alone guided by the ultrathin bronchoscopy. Additionally, the freezing time of transbronchial cryobiopsy is unstandardized. A randomized controlled trial should be conducted to compare the ice-balls of different diameters (such as 2.0 mm vs. 5.0 mm) to determine the diagnostic yield of cryobiopsy. Moreover, we did not perform biopsy on lesions that were invisible with rEBUS due to ethical reasons. This may have affected the number of positive rates. However, previous results have shown that the diagnostic yield of this population is significantly low (17%) [34]. In addition, we did not perform fluoroscopic guidance in the study, which may have limited accessibility of some of the lesions. Furthermore, the 1.95-mm guide sheath (GS) of the K-201 biopsy kit is too large to fit into the 1.7-mm working channel of the UTB. Although the position would be reconfirmed using the rEBUS probe after cryobiopsy, the bronchoscope position may shift after the rEBUS probe is withdrawn without GS in the UTB group. Therefore, it is imperative to perform fluoroscopic guidance for cryobiopsy in the UTB group. Finally, not all final diagnoses were confirmed by pathological results. Although we carefully reviewed and analyzed the clinical data, the final diagnosis of benign or malignant obtained from clinical follow-up may not be entirely accurate.
In conclusion, ultrathin bronchoscopy has higher ultrasound localization rate compared to thin bronchoscopy, as an important predictive factor for diagnosing the lesion, the diagnostic yield of UTB combined with cryobiopsy is significantly higher than the thin bronchoscope group. And ultrathin bronchoscopy with cryobiopsy is not associated with serious complications. Besides, univariate analysis demonstrated that ultrathin bronchoscopy is a more feasible method for examination of smaller lesions, benign lesions, upper lobe lesions, lesions located in the lateral once-third from the hilum, and lesions without bronchus signs.
Data availability
The data that support the findings of the study are not publicly available due to containing information that could compromise privacy of participants. Unidentified data generated or analyzed during this study may be obtained upon reasonable request to the corresponding author.
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48.
de Koning HJ, van der Aalst CM, de Jong PA, Scholten ET, Nackaerts K, Heuvelmans MA, et al. Reduced lung-Cancer mortality with volume CT screening in a Randomized Trial. N Engl J Med. 2020;382(6):503–13.
Lam S, Tammemagi M. Contemporary issues in the implementation of lung cancer screening. Eur Respir Rev. 2021;30(161).
Swensen SJ, Jett JR, Hartman TE, Midthun DE, Mandrekar SJ, Hillman SL, et al. CT screening for lung cancer: five-year prospective experience. Radiology. 2005;235(1):259–65.
Lu CH, Hsiao CH, Chang YC, Lee JM, Shih JY, Wu LA, et al. Percutaneous computed tomography-guided coaxial core biopsy for small pulmonary lesions with ground-glass attenuation. J Thorac Oncol. 2012;7(1):143–50.
Heerink WJ, de Bock GH, de Jonge GJ, Groen HJ, Vliegenthart R, Oudkerk M. Complication rates of CT-guided transthoracic lung biopsy: meta-analysis. Eur Radiol. 2017;27(1):138–48.
Sainz Zuñiga PV, Vakil E, Molina S, Bassett RL Jr., Ost DE. Sensitivity of Radial Endobronchial Ultrasound-guided bronchoscopy for Lung Cancer in patients with Peripheral Pulmonary lesions: an updated Meta-analysis. Chest. 2020;157(4):994–1011.
Miyoshi S, Isobe K, Shimizu H, Sunakawa M, Suzuki A, Sugino K, et al. The utility of virtual bronchoscopy using a computed tomography workstation for conducting conventional bronchoscopy: a retrospective analysis of clinical practice. Respiration. 2019;97(1):52–9.
Folch EE, Pritchett MA, Nead MA, Bowling MR, Murgu SD, Krimsky WS, et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary lesions: one-year results of the prospective, Multicenter NAVIGATE Study. J Thorac Oncol. 2019;14(3):445–58.
Kim SH, Kim J, Pak K, Eom JS. Ultrathin bronchoscopy for the diagnosis of Peripheral Pulmonary lesions: a Meta-analysis. Respiration. 2023;102(1):34–45.
Sumi T, Ikeda T, Sawai T, Shijubou N, Kure K, Yamada Y, et al. Comparison of ultrathin bronchoscopy with conventional bronchoscopy for the diagnosis of peripheral lung lesions without virtual bronchial navigation. Respir Investig. 2020;58(5):376–80.
Oki M, Saka H, Ando M, Asano F, Kurimoto N, Morita K, et al. Ultrathin bronchoscopy with Multimodal Devices for Peripheral Pulmonary lesions. A Randomized Trial. Am J Respir Crit Care Med. 2015;192(4):468–76.
Oki M, Saka H, Asano F, Kitagawa C, Kogure Y, Tsuzuku A, et al. Use of an ultrathin vs thin bronchoscope for Peripheral Pulmonary lesions: a Randomized Trial. Chest. 2019;156(5):954–64.
Nishii Y, Nakamura Y, Fujiwara K, Ito K, Sakaguchi T, Suzuki Y, et al. Use of Ultrathin Bronchoscope on a need basis improves diagnostic yield of difficult-to-Approach Pulmonary lesions. Front Med (Lausanne). 2020;7:588048.
Oki M, Saka H, Himeji D, Imabayashi T, Nishii Y, Ando M. Value of adding ultrathin bronchoscopy to thin bronchoscopy for peripheral pulmonary lesions: a multicentre prospective study. Respirology. 2023;28(2):152–8.
Babiak A, Hetzel J, Krishna G, Fritz P, Moeller P, Balli T, et al. Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration. 2009;78(2):203–8.
Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirology. 2017;22(3):443–53.
Tanaka M, Matsumoto Y, Imabayashi T, Kawahara T, Tsuchida T. Diagnostic value of a new cryoprobe for peripheral pulmonary lesions: a prospective study. BMC Pulm Med. 2022;22(1):226.
Yarmus LB, Semaan RW, Arias SA, Feller-Kopman D, Amador RO, Bösmüller H, et al. A randomized controlled trial of a Novel Sheath Cryoprobe for Bronchoscopic Lung Biopsy in a Porcine Model. Chest. 2016;150(2):329–36.
Franke KJ, Linzenbold W, Nuessle D, Enderle M, Boesmueller H, Nilius G, et al. A New Tool for Transbronchial cryobiopsies in the lung: an experimental feasibility ex vivo study. Respiration. 2016;91(3):228–34.
Echevarria-Uraga JJ, Pérez-Izquierdo J, García-Garai N, Gómez-Jiménez E, Aramburu-Ojembarrena A, Tena-Tudanca L, et al. Usefulness of an angioplasty balloon as selective bronchial blockade device after transbronchial cryobiopsy. Respirology. 2016;21(6):1094–9.
Bian Y, Zhou G, Gao Q, Deng M, Tong R, Xia Y, et al. Assessment of a randomized controlled trial on the safety of pre-placing bronchial balloons in transbronchial lung cryobiopsy for diagnosing interstitial lung disease. Eur J Med Res. 2024;29(1):268.
Cooley J, Balestra R, Aragaki-Nakahodo AA, Caudell Stamper DN, Sriprasart T, Swank Z, et al. Safety of performing transbronchial lung cryobiopsy on hospitalized patients with interstitial lung disease. Respir Med. 2018;140:71–6.
Nakai T, Watanabe T, Kaimi Y, Ogawa K, Matsumoto Y, Sawa K, et al. Safety profile and risk factors for bleeding in transbronchial cryobiopsy using a two-scope technique for peripheral pulmonary lesions. BMC Pulm Med. 2022;22(1):20.
Batra H, Yarmus L. Indications and complications of rigid bronchoscopy. Expert Rev Respir Med. 2018;12(6):509–20.
Oki M, Saka H, Kitagawa C, Kogure Y, Murata N, Adachi T, et al. Randomized study of endobronchial ultrasound-guided transbronchial biopsy: thin bronchoscopic method versus guide sheath method. J Thorac Oncol. 2012;7(3):535–41.
Oki M, Saka H, Kogure Y, Niwa H, Yamada A, Torii A, et al. Ultrathin bronchoscopic cryobiopsy of peripheral pulmonary lesions. Respirology. 2023;28(2):143–51.
Hetzel J, Maldonado F, Ravaglia C, Wells AU, Colby TV, Tomassetti S, et al. Transbronchial cryobiopsies for the diagnosis of diffuse Parenchymal Lung diseases: Expert Statement from the Cryobiopsy Working Group on Safety and Utility and a call for standardization of the Procedure. Respiration. 2018;95(3):188–200.
Yamada N, Yamazaki K, Kurimoto N, Asahina H, Kikuchi E, Shinagawa N, et al. Factors related to diagnostic yield of transbronchial biopsy using endobronchial ultrasonography with a guide sheath in small peripheral pulmonary lesions. Chest. 2007;132(2):603–8.
Kim SH, Mok J, Kim S, Yoo WH, Jo EJ, Kim MH, et al. Clinical outcomes of transbronchial cryobiopsy using a 1.1-mm diameter cryoprobe for peripheral lung lesions - a prospective pilot study. Respir Med. 2023;217:107338.
Nadig TR, Thomas N, Nietert PJ, Lozier J, Tanner NT, Wang Memoli JS, et al. Guided bronchoscopy for the evaluation of Pulmonary lesions: an updated Meta-analysis. Chest. 2023;163(6):1589–98.
Ost DE, Ernst A, Lei X, Kovitz KL, Benzaquen S, Diaz-Mendoza J, et al. Diagnostic Yield and complications of Bronchoscopy for Peripheral Lung lesions. Results of the AQuIRE Registry. Am J Respir Crit Care Med. 2016;193(1):68–77.
Tay JH, Irving L, Antippa P, Steinfort DP. Radial probe endobronchial ultrasound: factors influencing visualization yield of peripheral pulmonary lesions. Respirology. 2013;18(1):185–90.
Oki M, Saka H, Kitagawa C, Kogure Y, Mori K, Kajikawa S. Endobronchial ultrasound-guided transbronchial biopsy using novel thin bronchoscope for diagnosis of peripheral pulmonary lesions. J Thorac Oncol. 2009;4(10):1274–7.
Acknowledgements
We thank all the patients and all members’ contributions to this study.
Funding
Our study is funded by The Affiliated Hospital of Medical School of Ningbo University Youth Talent Cultivation Program (FYQM-LC-202003), Ningbo Social and Scientific Development Fund (2015C50012), Zhejiang Medical and Health Science and Technology Plan Project (2016KYB268), Ningbo Health Youth Technical Key Talents Training Special Project (2020SWSQNGG-05), Zhejiang Provincial Health Science and Technology Plan (2022RC247) and the Natural Science Foundation of Ningbo (2018A610271,2017A610250,2022J232), Clinical Medicine Special Fund Project of Zhejiang Medical Association (2022ZYC-Z31), Special Project on Scientific and Technological Research of COVID-19 Infection Diseases (Normal project No.6), Key Research and development plan of Ningbo City (2023Z179), Zhejiang basic public welfare research project(LGF21C010001).
Author information
Authors and Affiliations
Contributions
ZC and YY equally contributed to the study. ZC: study conception and design; administrative support; data collection, analysis, and interpretation; drafting of the manuscript; and final approval of the version to be published. XS: study conception and design; data collection, analysis, and interpretation; drafting of the manuscript; and final approval of the version to be published. YY: provision of study materials/patients; data collection, analysis, and interpretation; drafting of the manuscript; and final approval of the version to be published. HM: provision of study materials/patients; data collection; drafting of the manuscript; and final approval of the version to be published. SL: provision of study materials/patients; data collection; drafting of the manuscript; and final approval of the version to be published. LZ: provision of study materials/patients; data collection; drafting of the manuscript; and final approval of the version to be published. ZD: data collection, analysis, and interpretation; drafting of the manuscript; and final approval of the version to be published. HC: data collection, analysis, and interpretation; drafting of the manuscript; and final approval of the version to be published. XY: data collection; drafting of the manuscript; and final approval of the version to be published. RX: data collection; drafting of the manuscript; and final approval of the version to be published. DL: data collection; drafting of the manuscript; and final approval of the version to be published. XJ: data collection; and final approval of the version to be published. YZ: data collection; and final approval of the version to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the First Affiliated Hospital of Ningbo University(Ningbo, China; KS20224007; April 1, 2022), and the need for informed consent was waived due to retrospective nature of the study. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Patient consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, X., Chen, H., Li, S. et al. Value of ultrathin bronchoscope in improving the endobronchial ultrasound localization rate and diagnosing peripheral pulmonary nodules by cryobiopsy. BMC Pulm Med 24, 439 (2024). https://doi.org/10.1186/s12890-024-03256-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03256-7