Abstract
Background
Dry powder inhalers (DPIs) rely on both internal resistance and patients’ inspiratory capacity for effective operation. Optimal inspiratory technique is crucial for DPI users. This study assessed the accuracy and repeatability of two available devices, PF810® and In-Check DIAL®, and analyzed their measurement errors and consistency in detecting inspiratory capacity.
Methods
The accuracy and repeatability of peak inspiratory flow (PIF) and forced inspiratory vital capacity (FIVC) against various internal resistances of the two devices were assessed using standard waveforms generated by a breathing simulator. The agreement of PIF measurements between the two devices in healthy volunteers and chronic obstructive pulmonary disease (COPD) patients was analyzed with the intraclass correlation coefficient and Bland–Altman graphical analysis.
Results
PF810® showed great accuracy and repeatability in measuring PIF, except for square waveforms at the lowest flow rate (20 L/min). In-Check DIAL® exhibited poor accuracy against high resistance levels. In scenarios with no resistance, In-Check DIAL® had significantly smaller measurement errors than PF810®, but larger errors against high resistance levels. The two devices showed excellent agreement (ICC > 0.80, P < 0.05), except for healthy volunteers against medium to high resistance (R3-R5) where the ICC was insignificant. Bland–Altman plots indicated small disagreements between the two devices for both healthy volunteers and COPD patients.
Conclusions
In-Check DIAL® exhibited poor accuracy and larger measurement errors than PF810® when detecting PIFs against higher internal resistances. However, its good performance against lower internal resistances, along with its cost-effectiveness and convenience made it appropriate for primary care. PF810® showed good accuracy and repeatability and could detect additional parameters of inspiratory capacity beyond PIF, though required further studies to confirm its clinical benefits.
Similar content being viewed by others
Introduction
Inhalation therapy is the first-line treatment for Chronic Obstructive Pulmonary Disease (COPD) and bronchial asthma (asthma), as recommended by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [1] and the Global Initiative for Asthma (GINA) [2]. Various inhalation devices are available, including pressurized metered-dose inhalers (pMDIs), dry powder inhalers (DPIs), and soft mist inhalers (SMIs). DPIs containing bronchodilators and corticosteroids are commonly used in clinical practice for treating asthma and COPD [3,4,5]. DPIs are recommended for asthma and COPD patients who can achieve a forceful and deep inhalation [1]. DPIs are breath-actuated, relying on the interaction between the device's internal resistance and the patient's sufficient inspiratory capacity, which encompasses specific levels of inspiratory volume, flow rates, and post-inhalation breath-hold time [6, 7]. Meanwhile, the internal resistances of DPIs vary significantly, necessitating different minimum and optimal inspiratory flow rates for effective utilization [8]. Therefore, before selecting appropriate DPIs for patients, it is imperative to evaluate their inspiratory capacity across various internal resistances to mitigate the risk of insufficient lung deposition.
Routine pulmonary function tests mainly assess ventilation function, such as forced expiratory volume in one second (FEV1) and forced vital capacity (FVC). Previous studies have shown a lack of correlation between peak inspiratory flow (PIF) at various device resistance levels and FEV1, FEV1% prediction, or FVC [8,9,10]. More than the severity of airflow limitation, the inspiratory capacity is affected by age, gender, muscle strength, and frailty. Several studies have proved that COPD patients [7, 9, 11,12,13,14] and children with asthma [7, 15] have lower PIFs compared to the healthy adults. Men generally have higher PIFs than women [16], and PIFs tend to decline with age [17]. The inspiratory muscle strength and maximum inspiratory pressures are lower in frail compared to pre-frail and non-frail older adults [18, 19]. Consequently, inspiratory capacity may vary among patients with different conditions, and training can enhance the ability to use inhalers [10]. Evaluating and monitoring inspiratory capacity should be an integral part of disease management.
Patients' inspiratory capacity against internal resistances can be measured and trained by using the In-Check DIAL® with mouthpieces [20, 21] or Multi-Function Spirometer System PF810® [22] (Fig. 1). In-Check DIAL® has been used in previous studies to measure PIFs between 15 and 120 L/min [23,24,25], while PF810® is relatively new in this field. Therefore, this study measured and compared the accuracy, repeatability, and consistency of these two devices. Additionally, their working principles, cost, and application ranges were discussed to determine which device better meets clinical needs.
Methods
Subjects and study design
The subjects were prospectively enrolled for this comparative study. The healthy volunteers and COPD patients were recruited from Zhongshan Hospital, Shanghai Medical College, Fudan University. COPD patients were diagnosed according to the GOLD guidelines [1], with exlusion criterias: patients with other diseases, cognitive disabilities, lack of patient's consent. The healthy volunteers were defined based on clinical investigation and a negative history of any diseases. Demographic characteristics of all participants were collected, and their PIFs against varying levels of resistance were detected through In-Check DIAL® and PF810®. And PIF values detected by In-Check DIAL® and PF810® were compared to assess the consistency between the two devices. The study was approved by the Ethics Committee of Zhongshan Hospital of Fudan University (B2019-142) and all the participants have signed an informed consent.
In order to analyze the in vitro accuracy and repeatability of In-Check DIAL® and PF810®, a breathing simulator was applied to generate specific airflows with fixed inspiratory volumes and flow rates. The PIFs of airflows were measured by In-Check DIAL® and PF810®. The flow volumes, equivalent to forced inspiratory vital capacity (FIVC), were measured by PF810®.
The devices and instruments
In-Check DIAL® (Clement Clarke International, Harlow, UK and Alliance Tech Medical) comprises a resistance generation and a mechanical measurement component to detect the PIF. During the measurement procedure, the resistance generation component was manually adjusted to simulate internal resistances of pMDIs, SMIs, and DPIs, ranging from no resistance (R0) to high resistance (R5) (Supplementary Table S1) [26, 27].
The Multi-Function Spirometer System PF810® (UBREATH, Hangzhou, China), a novel flow sensor-based spirometer, visualizes dynamic real-time inspiratory flow on a flow-time graph and output other parameters reflecting inspiratory capacity (Supplementary Figure S1). The flow sensor inside PF810® was capable of simulating internal resistances from R0 to R5, consistent with In-Check DIAL®.
The breathing simulator (Piston Medical Ltd., Budapest, Hungary) was utilized to simulate patients’ inspiratory efforts with specific flow rates, volumes, and times. The mechanical error of the breathing simulator was less than 0.2%.
Measurement of simulated waveforms
The instructions for using In-Check DIAL® and PF810® were obtained from the respective manufacturer websites and product brochures [20,21,22].
PF810®
Before measurement, the BTPS (body temperature, pressure, water vapor saturated) correction function of PF810® was selected. The software carried by PF810® (Multigunctional Pulmonary Function Testing System v1.1.7) calculated the BTPS correction factor from sensor data and correct the results output of the device. In this way, the PIF and FIVC of airflows generated by the simulator and the participants were BTPS-corrected.Then a certified 3 L syringe (CareFusion Calibration Pump, Germany) was used for calibration. The air outlet of the syringe was connected to PF810®’s filter port with a silicone tube, then volume calibration checks were performed manually using different flow rates between 2 and 12 L/s.
The air outlet of the breathing simulator was connected to PF810®’s filter port using a silicone tube to avoid air leaks. Resistance levels were set via PF810®’s software before operating the simulator to initiate the output of inspiratory waveforms. In this study, C07, C09, C13 inspiratory waveforms from ISO 26782: 2009 international certification, square waveforms with an inspiratory volume of 2 L and flow rates varying from 20 to 100 L/min, and sine waveforms with an inspiratory volume of 3 L and a PIF of 60 L/min were generated using the breathing simulator. The measurement results of the flow rate and volume, equivalent to PIF and FIVC, against different resistance levels were recorded. For each condition, three repetitions were performed.
In-Check DIAL®
The red cursor was reset to the start position before In-Check DIAL® was connected to the simulator's air outlet using a silicone tube. After adjusting the resistance level, the breathing simulator was activated to generate the standard waveforms. The PIF reading, indicated by the position of the red cursor against the scale, was recorded. For each condition, three repetitions were performed.
Measurement of participants' PIFs
After PF810® had completed the BTPS correction and the calibration with the 3 L syringe, In-Check DIAL® and PF810® were both adjusted to the required resistance levels. After connecting the mouthpiece to either the In-Check DIAL® or PF810®, each participant was instructed to (1) sit still, look straight ahead and keep the head vertical; (2) make the mouth close to the mouthpiece; (3) exhale slowly and as completely as possible; (4) inhale deeply and quickly, keep the inhalation as smooth as possible; (5) hold the breath for as long as possible, and then slowly exhale the air in the lungs. Repeat the above maneuvers three times, and the maximum PIF value among three repetitions was recorded before adjusting the device to the next resistance level. Each participant completed PIF measurements at six resistance levels using both devices, with a few minutes of rest scheduled between each inhalation. Additionally, all the participants received detailed instructions on how to use each device from researchers and practiced using them beforehand. Researchers confirmed their proficiency and movements before the actual tests began.
Statistical analysis
The accuracy and repeatability of PF810® and In-Check DIAL® were assessed using three repeated measurements of simulated flows generated by the breathing simulator. The measurement error was defined as the difference between each measured value and the standard value (Vstd). The average error (Verr) was calculated as the mean of the three measurement errors. The reading span (Vspan) was the difference between the maximum and minimum values among the three readings. The accuracy was expressed as the ratio of Verr to Vstd, and the repeatability was determined as the ratio of Vspan to the average measured value. A student t-test was applied to determine whether there was a significant difference (P < 0.05) in measurement error between the two devices.
The agreement of the two devices was assessed using the intraclass correlation coefficient (ICC) and the Bland–Altman graphical analysis. A p-value of less than 0.05 indicated a significant ICC, interpreted as follows: zero to 0.20, poor agreement; 0.21–0.40, fair agreement; 0.41–0.60, moderate agreement; 0.61–0.80, good agreement; 0.81–1.00, excellent agreement [28]. Bland–Altman plots were created based on the average differences between PIFs detected by PF810® and In-Check DIAL®.
SPSS (v26.0) and R (v4.2.0) software were used for statistical analysis.
Results
PF810® presented accuracy less than 10% except measuring the lowest PIFs
According to the international standard ISO 23747: 2015 (Anaesthetic and respiratory equipment), Verr and Vspan of both PIF and FIVC should be less than 10 L/min, and accuracy and repeatability should be less than 10%, to meet the requirements. Supplementary Table S2 indicated that when standard waveform C07, C09, and C13 were measured by PF810®, Verr, Vspan, accuracy, and repeatability of both PIFs and FIVCs all met these criteria.
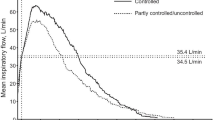
Table 1 presented that when the standard PIF of a square wave was 20 L/min, the accuracy of PIFs measured by PF810® exceeded 10% against resistances R0-R4. It also exceeded 10% against resistance R1 when the standard PIF was 40 L/min. In other conditions, both PIFs and FIVCs of square waves measured by PF810® met the criteria. PF810® also met the criteria for detecting PIFs and FIVCs of sine waves with a volume of 3 L and a peak flow rate of 60 L/min against any resistance level. Figure 2 and Fig. 3 showed the real-time square and sine waveforms measured by PF810® from R0 to R5, which closely matched the waveforms output by the simulator.
The accuracy of In-Check DIAL® exceeded 10% against high internal resistances
Table 2 presented the PIF measurements of simulated waveforms against different resistance levels using In-Check DIAL®. The repeatability of In-Check DIAL® met the criteria except for a fixed flow rate of 20 L/min against resistance R5. The accuracy of measuring certain flow rates (20 and 40 L/min against R0, 60 and 80 L/min against R1, 60–100 L/min against R2) was outside the 10% limit against resistances R0-R2. The accuracy of In-Check DIAL® was above 10% for all flow rates against resistances R3-R5, failing to meet the criteria. The Verr of In-Check DIAL® mostly exceeded 10 L/min against resistances R2-R5, with detected values being lower than the standard values.
The measurement errors between In-Check DIAL® and PF810®
The measurement errors of PF810® and In-Check DIAL® for determining PIFs were compared (Table 3). Against resistance R0, In-Check DIAL® had significantly smaller measurement error than PF810®. Against resistance R1 and R2, with a standard PIF of 20 L/min, In-Check DIAL® also had significantly smaller errors. However, for standard PIFs of 60, 80, or 100 L/min against R1 and R2, In-Check DIAL® had significantly larger errors. Against resistance R3, with standard PIFs from 40 to 100 L/min, In-Check DIAL® also showed significantly larger measurement errors than PF810®. PF810® had notably smaller errors against R4 and R5, regardless of the fixed waveforms' flow rates.
Consistency between In-Check DIAL® and PF810® in measuring participants' PIFs
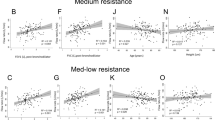
A total of 10 healthy volunteers and 14 COPD patients participated in this study. Table 4 demonstrated that for COPD patients, PF810® and In-Check DIAL® had excellent agreement (> 0.80) from R1 to R5. For healthy volunteers, PF810® and In-Check DIAL® had excellent agreement against R1 (ICC = 0.952, 95% CI: 0.819–0.988, P < 0.001) and R2 (ICC = 0.916, 95% CI: 0.654—0.979, P = 0.001), but the ICC against R3 to R5 was not significant (P > 0.05). From R0 to R5, Bland Altman plots (Fig. 4) all demonstrated small disagreements between PF810® and In-Check DIAL® in PIFs measurement for both healthy volunteers and COPD patients. In COPD patients, the mean difference (In-Check DIAL®—PF810®) was from 2.35 to -6.35 L/s. In healthy volunteers, the mean difference was from 5.50 to -3.00 L/s.
The Bland–Altman plots of participants' PIFs measured by PF810® and In-Check DIAL®.COPD, chronic obstructive pulmonary disease; PIF, peak inspiratory flow; R1, low resistance; R2, medium–low resistance; R3, medium resistance; R4, medium–high resistance; R5, high resistance; Measn, the average difference between the measurement values of In-Check DIAL® and PF810®; SD, standard deviation
PIFs detected by PF810® against R0 exceeded 120 L/min, the upper limit of In-Check DIAL®, so PIFs against resistance R0 were not included in the consistency analysis.
Discussion
To select appropriate DPIs and assist with inhalation training, the device used to evaluate PIF needs to be accurate, repeatable, convenient, and cost-effective. In this study, the accuracy and repeatability of PF810® and In-Check DIAL® were compared based on standard PIFs and FIVCs of different waveforms generated by the breathing simulator for the first time. Their general performance and consistency between PF810® and In-Check DIAL® in detecting PIF against various resistance levels were evaluated for the first time.
Previous studies have shown that many researchers prefer using In-Check DIAL® over other spirometers to measure PIFs because it can measure PIFs against resistance conditions, which more accurately reflects patients’ inspiratory capacity when using DPIs. In-Check DIAL® also assists patients with low PIFs in inhalation training. It has been demonstrated that inhaler technique training using In-Check DIAL® increases patients' PIFs and improves their ability to use DPIs [10]. Accurate measurement of PIFs against resistances was necessary for clinical evaluation and inhalation training. However, few studies have assessed the accuracy of In-Check DIAL®, indicating a need for further evaluation. Barnes found that when In-Check DIAL® was used to detect PIFs at resistant levels of Diskus® or Handihaler®, there was a small mean difference between measurement attempts and a low repeatability limit [29]. Conversely, Broeders proved that In-Check DIAL® could not indicate all patients who did not reach the optimal flow rate [30]. Our research also showed that In-Check DIAL® had low accuracy in measuring PIFs at resistance levels of R3, R4, and R5.
PF810® is a new device in this field and has not been applied in reported research. This study demonstrated good repeatability of PF810®, and its accuracy was also confirmed, except for square waves with extremely low PIF values. Meanwhile, its measurement error against high resistance levels was significantly smaller than that of In-Check DIAL®. Although the Bland–Altman plots showed that PIF measurements of PF810® and In-Check DIAL® were in reasonable agreement for both COPD patients and healthy volunteers, the ICCs indicated inconsistencies against high resistances in healthy volunteers, probabaly due to In-Check DIAL®'s larger measurement error against high internal resistances.
Additionally, since inspiratory flow would be affected by ambient conditions, the device should be able to convert the ambient conditions to physiological ones within the lungs before detecting inspiratory capacity [31]. PF810® included a BTPS correction function, while In-Check DIAL® with simple structure was probably affected by environmental factors.
For a comprehensive evaluation of inhalation techniques, indicators such as breath-holding time, effective inspiratory time and volume were crucial. Excessive flow rate and oral pressure increased the deposition of drugs in the upper respiratory tract due to inertial impaction [32], leading to higher drug deposition in the central respiratory tracts and reduced uniformity of drug distribution throughout the airway [33]. PF810® could measure these parameters and the real-time display of inspiratory flow may aid inhalation training. However, further clinical studies are needed to determine if these technical advantages translate into clinical benefits.
In clinical practice, both cost-effectiveness and safety are important considerations. PF810® was priced at 28, 314 USD, with each disposable mouthpiece costing 4.72 USD. In contrast, In-Check DIAL® costed 37.56 USD, with disposable one-way valved cardboard mouthpieces at 0.42 USD each. Both devices met safety requirements by using replaceable mouthpieces to prevent the transmission of respiratory pathogens. However, due to its high cost, PF810® was more appropriate for specialized hospitals and tertiary hospitals, whereas In-Check DIAL®, being less expensive, smaller, and more convenient, was better suited for use in clinics and at home, where COPD and asthma are commonly treated and managed.
The primary limitation of this study was its small sample size, including only 10 healthy volunteers and 14 COPD patients for comparing the two devices. However, PF810® showed promising advantages in the preliminary study, suggesting further verification. We plan to evaluate the clinical benefits of PF810® in the following studies.
Conclusions
In-Check DIAL® exhibited relatively lower accuracy in detecting PIF against high internal resistances and lacked the capability to measure other indicators of inspiratory capacity. Nevertheless, it was proved to be more cost-effective, convenient, and appropriate for outpatients and primary care settings. PF810®, despite its high cost, exhibited good accuracy and repeatability in measuring multiple parameters. It showed small disagreements with In-Check DIAL®, making it suitable for comprehensive assessments in large hospitals. However, the clinical benefits of PF810® still require substantiation through reliable evidence from clinical trials.
Availability of data and materials
All data generated or analysed during this study are included in the manuscript and supplementary material.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- GOLD:
-
The global initiative for Chronic Obstructive Lung Disease
- GINA:
-
The global initiative for asthma
- pMDIs:
-
Pressurized metered-dose inhalers
- DPIs:
-
Dry powder inhalers
- SMIs:
-
Soft mist inhalers
- R0:
-
No resistance
- R1:
-
Low resistance
- R2:
-
Medium–low resistance
- R3:
-
Medium resistance
- R4:
-
Medium–high resistance
- R5:
-
High resistance
- FEV1 :
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- PIF:
-
Peak inspiratory flow
- FIVC:
-
Forced inspiratory vital capacity
- BTPS:
-
Body temperature, pressure, water vapor saturated
- Vstd :
-
The standard value of airflows' PIFs and FIVCs generated by the breathing simulator
- Verr :
-
The mean of the difference between the measurement and the standard value
- Vspan :
-
The reading span, equivalent to the difference between the maximum and minimum measurement value
- ICC:
-
Intraclass correlation coefficient
References
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease (2023 REPORT). https://goldcopd.org/2023-gold-reports-2/. Accessed 10 Jan 2023.
Global Initiative for asthma. Global Strategy for Asthma Management and Prevention (2021 update). https://ginasthma.org/gina-reports/. Accessed 10 Jan 2023.
Markham A, Jarvis B. Inhaled salmeterol/fluticasone propionate combination: a review of its use in persistent asthma. Drugs. 2000;60(5):1207–33.
Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med. 2003;16(3):249–54.
Pasqua E, Hamblin N, Edwards C, Baker-Glenn C, Hurley C. Developing inhaled drugs for respiratory diseases: A medicinal chemistry perspective. Drug Discov Today. 2022;27(1):134–50.
Sorino C, Negri S, Spanevello A, Visca D, Scichilone N. Inhalation therapy devices for the treatment of obstructive lung diseases: the history of inhalers towards the ideal inhaler. Eur J Intern Med. 2020;75:15–8.
Laube BL, Janssens HM, de Jongh FHC, Devadason SG, Dhand R, Diot P, et al. What the pulmonary specialist should know about the new inhalation therapies. Eur Respir J. 2011;37(6):1308–31.
Ghosh S, Ohar JA, Drummond MB. Peak inspiratory flow rate in chronic obstructive pulmonary disease: implications for dry powder inhalers. J Aerosol Med Pulm Drug Deliv. 2017;30(6):381–7.
Ghosh S, Pleasants RA, Ohar JA, Donohue JF, Drummond MB. Prevalence and factors associated with suboptimal peak inspiratory flow rates in COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:585–95.
Hua JL, Ye XF, Du CL, Xie N, Zhang JQ, Li M, et al. Optimizing inhalation therapy in the aspect of peak inhalation flow rate in patients with chronic obstructive pulmonary disease or asthma. BMC Pulm Med. 2021;21(1):302.
Gosselink R, De Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle training in patients with COPD: what is the evidence? Eur Respir J. 2011;37(2):416–25.
Loh CH, Peters SP, Lovings TM, Ohar JA. Suboptimal inspiratory flow rates are associated with chronic obstructive pulmonary disease and all-cause readmissions. Ann Am Thorac Soc. 2017;14(8):1305–11.
Mahler DA. Peak inspiratory flow rate as a criterion for dry powder inhaler use in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2017;14(7):1103–7.
Mahler DA, Ohar JA, Yun J, Moran EJ, Crater GD. Suboptimal PIFR associated with greater dyspnea in Chronic Obstructive Pulmonary Disease (COPD) [Meeting Abstract]. Am J Respir Crit Care Med. 2019;199:2.
Cooper A, Parker J, Berry M, Wallace R, Ward J, Allan R. Wixela Inhub: dosing performance in vitro and inhaled flow rates in healthy subjects and patients compared with Advair Diskus. J Aerosol Med Pulm Drug Deliv. 2020;33(6):323–41.
Laube BL. In vivo measurements of aerosol dose and distribution: clinical relevance. J Aerosol Med. 1996;9(Suppl 1):S77-91.
Chen HI, Kuo CS. Relationship between respiratory muscle function and age, sex, and other factors. J Appl Physiol (1985). 1989;66(2):943–8.
Pegorari MS, Ruas G, Patrizzi LJ. Relationship between frailty and respiratory function in the community-dwelling elderly. Braz J Phys Ther. 2013;17(1):9–16.
Vidal MB, Pegorari MS, Santos EC, Matos AP, Pinto ACPN, Ohara DG. Respiratory muscle strength for discriminating frailty in community-dwelling elderly: a cross-sectional study. Arch Gerontol Geriatr. 2020;89:104082.
Clement Clarke International. In-Check DIAL® G16: Coaching DPI and pMDI inhaler technique. https://www.haag-streit.com/clement-clarke/products/inhaler-technique/in-check-dial-g16/. Accessed 29 Dec 2023.
Alliance Tech Medical. In-Check™ DIAL G16: Inhaler Technique Training and Assessment Tool. https://alliancetechmedical.com/check-dial-training-device/. Accessed 29 Dec 2023.
e-LinkCare. UBREATH® Multi-Function Spirometer System (PF810). https://www.e-linkcare.com/ubreath-multi-function-spirometer-system-pf810-product/. Accessed 24 Jun 2022.
Mahler DA, Waterman LA, Gifford AH. Prevalence and COPD phenotype for a suboptimal peak inspiratory flow rate against the simulated resistance of the Diskus® dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;26(3):174–9.
Kawamatawong T, Khiawwan S, Pornsuriyasak P. Peak inspiratory flow rate measurement by using In-Check DIAL for the different inhaler devices in elderly with obstructive airway diseases. J Asthma Allergy. 2017;10:17–21.
Sharma G, Mahler DA, Mayorga VM, Deering KL, Harshaw O, Ganapathy V. Prevalence of low peak inspiratory flow rate at discharge in patients hospitalized for COPD exacerbation. Chronic Obstr Pulm Dis. 2017;4(3):217–24.
Ohar JA, Ferguson GT, Mahler DA, Drummond MB, Dhand R, Pleasants RA, et al. Measuring peak inspiratory flow in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2022;17:79–92.
Sanders MJ. Guiding inspiratory flow: development of the In-Check DIAL G16, a tool for improving inhaler technique. Pulm Med. 2017;2017:1495867.
Curvo-Semedo L, Lambregts DM, Maas M, Thywissen T, Mehsen RT, Lammering G, et al. Rectal cancer: assessment of complete response to preoperative combined radiation therapy with chemotherapy–conventional MR volumetry versus diffusion-weighted MR imaging. Radiology. 2011;260(3):734–43.
Barnes CN, Mahler DA, Ohar JA, Lombardi DA, Crater GD. Peak inspiratory flows: defining repeatability limits and a predictive equation for different inhalers. Chest. 2020;158(4):1413–9.
Broeders MEAC, Molema J, Vermue NA, Folgering HTM. In Check dial: accuracy for Diskus and Turbuhaler. Int J Pharm. 2003;252(1–2):275–80.
Sylvester KP, Clayton N, Cliff I, Hepple M, Kendrick A, Kirkby J, et al. ARTP statement on pulmonary function testing 2020. BMJ Open Respir Res. 2020;7(1):e000575.
Cheng YS. Aerosol Deposition in the Extrathoracic Region. Aerosol Sci Technol. 2003;37(8):659–71.
Usmani OS, Biddiscombe MF, Barnes PJ. Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med. 2005;172(12):1497–504.
Acknowledgements
We thank UBREATH (Hangzhou, China) for providing the working principles of PF810®.
Funding
The study is financially funded by 2021 clinical medicine research navigation project of Shanghai Medical College of Fudan University and Science and Technology Commission of Shanghai Municipality (19DZ1920104).
Author information
Authors and Affiliations
Contributions
YW and JZ conceived and designed the study. YW, LL, YG, XL and XY collected the data. YW performed the analysis and wrote the paper. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Authors reporting experiments on humans and/or the use of human tissue samples confirm that all experiments were performed in accordance with relevant guidelines and regulations. This study was approved by the Ethics Committee of Zhongshan Hospital of Fudan University (B2019-142) and all the participants have signed an informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wu, Y., Li, L., Gong, Y. et al. Comparisons between In-Check DIAL® and PF810® in evaluation and training inspiratory capacity for using dry powder inhalers. BMC Pulm Med 24, 380 (2024). https://doi.org/10.1186/s12890-024-03191-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03191-7