Abstract
Background
The United States has lost many lives to COVID-19. The role of social capital and collective action has been previously explored in the context of COVID-19. The current study specifically investigates the role of social trust at the county level and COVID-19 mortality in the US, hypothesizing that counties with higher social trust will have lower COVID-19 mortality rates.
Methods
We used cross-sectional data from the General Social Survey (GSS). We collected COVID-19 mortality data from the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University until October 31, 2021. We obtained county characteristics from the 2019 American Community Survey and supplemented this data source with additional publicly available county-level data, such as measures of income inequality and political leanings. We measured social trust as a single item from the GSS and calculated mean social trust in a county by pooling responses from 2002 to 2018. We then modeled the relationship between mean social trust and COVID-19 mortality.
Results
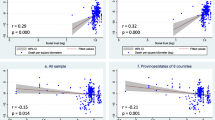
Results indicate that counties with higher social trust have lower COVID-19 mortality rates. Higher values of mean social trust at the county level are associated with a decrease in COVID-19 mortality (b= -0.25, p-value < 0.001), after adjustment for confounding. The direction of association is consistent in a sensitivity analysis.
Conclusions
Our findings underscore the importance of investment in social capital and social trust. We believe these findings can be applied beyond the COVID-19 pandemic, as they demonstrate the potential for social trust as a method for emergency preparedness.
Similar content being viewed by others
Introduction
The COVID-19 pandemic claimed many lives in the United States, both in terms of deaths directly attributable to COVID-19 and excess deaths indirectly attributable to COVID-19 [1, 2]. While scientific advancements, such as the development of vaccines and rapid testing, are conducive to substantially reducing COVID-19 mortality rates, psychosocial factors also play a role in pandemic preparedness and infectious disease burden. The COVID-19 pandemic highlighted the importance of collectivist actions for disease prevention. Public health measures to prevent COVID-19 infections relied on group collectivism, consisting of both group- and individual-level precautions. Group-level measures acting at the policy level can consist of mechanisms such as enforcing a mask mandate, stay-at-home guidelines, and requiring a COVID-19 test or proof of vaccination before travel. Individual-level actions to protect themselves and others from COVID-19 include, but are not limited to, methods such as: getting vaccinated against COVID-19, wearing a mask in high-risk spaces, physical distancing, and testing for COVID-19 when sick.
Researchers explored the role of various dimensions of social capital on COVID-19 mortality, with some inconsistent findings. For example, time-series analyses in 84 countries, including countries in world regions such as the Middle East, Africa, North and South America, and others, suggest that countries lacking in some measures of social capital experienced more COVID-19 deaths [3]. Similarly, research conducted in the US suggests that higher levels of social capital are protective against COVID-19 infection and mortality [4]. However, additional work demonstrated that specific dimensions of social capital were either positively (community attachment and social trust) or negatively (family bond and security) associated with COVID-19 deaths [5].
These studies point towards a need for investigating and focusing on specific dimensions of social capital. Our study specifically considers social trust, a component of social capital facilitating resource-sharing [6, 7], essential for collectivist action within a community or network group [6]. Whether a society has high levels of interpersonal trust is related to how it can engage in collective action [8, 9] and can increase willingness to support public health measures and services [10,11,12]. This is exemplified by work conducted in a Canadian setting that emphasizes the importance of collectivist action by indicating that collectivism is associated with abiding by stay-at-home ordinances [13].
The role of interpersonal trust, specifically in the context of the COVID-19 pandemic, has been explored globally. Some findings suggest that higher interpersonal social trust is associated with higher COVID-19 mortality rates, through a pathway involving more social interactions [3, 5]. This is in contrast to a global study finding that higher interpersonal trust and government trust are associated with lower COVID-19 infection rates [14]. Data from Sweden suggest that non-compliance with COVID-19 public health measures is associated with lower social trust; [15] this is in line with studies in the global context, which find higher interpersonal trust to be associated with increased compliance with COVID-19 public health measures, such as vaccine coverage [14, 16, 17]. A cross-national analysis found that, while a higher level of social trust may result in a shorter duration to the first outbreak due to more cohesive social relationships and lower risk perception, social trust may facilitate cooperation and compliance to neutralize COVID-19 [18].
The complex interplay of interpersonal and institutional trust further complicates the relationship between social trust and COVID-19 deaths. The role of institutional and interpersonal trust are both underscored as drivers of COVID-19, with interpersonal trust invoked as a leverage point for participation in mitigation policies such as decreased outdoor activity [19]. Scholars further highlighted the importance of political trust by examining the role of partisanship in compliance with COVID-19 mitigation policies, finding that Republican-leaning areas complied less than those leaning Democrat; [17] they further suggest that social capital is protective in mitigating COVID-19 cases in liberal counties but a risk factor in conservative areas [20]. Researchers described the interaction of political and interpersonal trust in complying with social distancing measures, noting inconsistent findings over time [21].
There is precedence to believe that social trust influences outcomes during the COVID-19 pandemic, potentially through collectivist action. In light of conflicting findings, this study explores the role of social trust in COVID-19 deaths at the state level in the United States. We hypothesize that areas with a higher social trust will have lower COVID-19 mortality rates.
Methods
Participants and recruitment
Data are from the National Opinion Research Council (NORC) General Social Survey (GSS), a nationally representative panel survey within the United States. Using multi-stage area probability sampling, participants are recruited for the GSS every two years (with some exceptions) from 1972 to 2018 [22]. Detailed information concerning sampling methods is available elsewhere [22]. This cross-sectional analysis pooled data from the 2002–2018 surveys, capturing a total of 19,712 participants. We conducted sensitivity analyses restricted to pooling data from the 2016–2018 GSS to determine whether this impacted variability in our effect estimate.
All statistical analyses were conducted in R using R-Studio. The data were filtered to include counties with at least more than one observation.
Exposure: social trust
We defined social trust through a survey question asking participants whether “Generally speaking, would you say that most people can be trusted or that you can’t be too careful in dealing with people?”. Response categories included ‘most people can be trusted,’ ‘can’t be too careful,’ or ‘it depends’ [23]. We calculated the intraclass coefficient (ICC) to explore clustering at the county level in the GSS data. We found an ICC of 0.22, indicating clustering was a concern; as such, we averaged the measure of social trust to the county level, allowing social trust to be interpreted as the mean level of social trust per county. The mean social trust in a county was calculated by assigning levels of social trust the following numeric values: 0 = ‘can’t be too careful,’ 0.5 = ‘it depends,’ 1.0 = ‘most people can be trusted.’ We pooled data from 2002 to 2018 to estimate mean social trust in a county; we conducted sensitivity analyses restricting to 2016–2018, to test the stability of the measure of mean social trust and its effect on COVID-19 mortality.
Outcome: COVID-19 mortality
We used data from the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University to amass information on COVID-19 cases and deaths [24]. COVID-19 deaths at the county level were counted up until October 31, 2021. The death rate per 1000 individuals was calculated by dividing the number of deaths in a county by the total population of the county and multiplying this value by 1000.
Covariates
Using information from the 2019 American Community Survey (ACS) [25], we adjusted for county characteristics, including average household size and population density. We also adjusted for county-level sociodemographic characteristics, including median age, percentage of the population that is white, median income, and percentage of the population that is insured. We adjusted for income inequality using an index for income inequality available from the 2020 County Health Rankings & Roadmaps (CHRR) [26] and the proportion of Republican voters, from the 2020 election results [27]. All data were harmonized at the county level through the Federal Information Processing Standards (FIPS) codes [28].
Statistical analysis
We first performed bivariate analyses to investigate the relationship of each covariate with the outcome, COVID-19 mortality. To test the relationship between these mean social trust in a county and the county’s death rate, we fit a Generalized Linear Model (GLM) with a Gaussian family using the ‘glm’ function, controlling for median income (per $10,000 increase), median age (per 10-year increase), percentage insurance, percentage of residents who were white, percentage of residents that voted republican, population density of the county per square mile (per 100 people), and inequality. The dependent variable in the model was the death rate and the primary explanatory variable was mean social trust. The model was weighted using survey weights [29]. All models were adjusted for a priori hypothesized confounders of the relationship between social trust and COVID-19 deaths. We removed participants with missing data or who lived in counties with missing data from our analyses. Due to missingness, 10,963 observations were analyzed from 2002 to 2018, with participants representing 374 counties.
Results
Descriptive statistics
Table 1 contains descriptive statistics for participants from the pooled 2002–2018 General Social Survey. The analytic sample included 10,963 participant responses. Of these participants, 61.8% reported distrusting others, with 33.0% reporting that they trust others. Respondents were predominantly female (55.4%), White (76.4%), and currently married (45.7%). Most participants were either in the middle class (42.4%) or working class (45.7%).
Table 2 contains descriptive statistics for county-level characteristics. On average, counties had a median age of 39, were 74% white, with 48% of the county voting Republican.
Multivariable models
After adjustment for appropriate county-level confounders, our results indicate that counties with higher levels of social trust, as measured in the pooled 2002–2018 data, had lower COVID-19 mortality (Table 3). We report our sensitivity analysis, restricted to 2016–2018 data for calculating mean social trust, in Table S1. Broadly, analyses show that this restriction in years of data in calculating mean social trust did not change our conclusions regarding the association between social trust and COVID-19 mortality; however, the effect estimate is stronger (Table S1).
Discussion
This paper explores the role of social trust in COVID-19 mortality. Our results indicate that counties with higher levels of social trust have lower COVID-19 mortality rates. We believe that findings from this study highlight the importance of investment in building social capital and trust beyond the COVID-19 pandemic. Previous research details the importance of collectivism and social capital in mitigating the harmful effects of pandemics, such as Ebola [30, 31], and other natural disasters [32]. Further investigations should explore how investment in social trust could be used as a method of emergency preparedness for future pandemics and widespread crises.
Social capital is a protective factor in various health-related outcomes; [33] it follows that social trust, a component of social capital, is also associated with health-related outcomes across societal contexts. Prior work shows that social trust is associated with all-cause mortality within the U.S., hypothesized to operate biologically through stress and the hypothalamic-pituitary-adrenal (HPA) axis [23]. A small study (N = 20) conducted in Japan with males ages 19–23 found that people who reported higher levels of interpersonal trust had lower levels of cortisol, a chemical associated with stress responses [34]. A similar study in the same context found higher social trust, as a function of social capital highly related to income inequality, to be associated with lower mortality, including all-cause mortality, coronary heart disease, malignant neoplasms, and infant mortality [35]. Community-level social trust among adults in Korea is associated with a lower risk of death from all causes, cardiovascular disease, and cancers [36].
People who are socially disconnected, or, lonely, tend to have lower levels of social trust [37]. Loneliness is associated with increased risk of mortality [38, 39] and adverse health outcomes, including but not limited to psychiatric disorders [40] and cardiovascular diseases [41]. As briefly described above, the mechanism of action is hypothesized to operate through allostatic load and the HPA axis; [23] thus, people who are lonely tend to have higher levels of inflammation [42]. The relationship between loneliness, social trust, inflammation, and adverse health outcomes could suggest that people with a lower degree of social trust were more susceptible to COVID-19 disease. This is bolstered by findings suggesting that inflammation as a result of chronic stress acts synergistically with inflammation from COVID-19 to produce poor health outcomes [43]. Lastly, recent research suggests that lower social cohesion is associated with a lower antibody response from COVID-19 [44], emphasizing this link between social and physical health.
To better understand the importance of the association between social trust and mortality, we must first outline the landscape of social trust within the U.S. Levels of social trust were already decreasing in the U.S. prior to the COVID-19 pandemic. A survey conducted by the Pew Research Center found that 79% of U.S. adults believe they have little confidence in each other (a measure of interpersonal trust), with 58% reporting that it is important to improve levels of confidence between U.S. adults [45]. Research indicates that, historically, levels of social trust vary widely within the U.S.; a higher lack of social trust correlates with greater age-adjusted mortality rates at the state level [35, 46]. Income inequality, a relevant component when discussing income gradients in COVID-19 deaths, is also correlated with a lack of social trust, wherein greater income inequality is associated with lower levels of social trust [35].
The COVID-19 pandemic impacted two facets of social trust: neighborhood and generalized trust. A study with Canadian data conducted during the pandemic delineates distinct trajectories of social trust and found that trust either decreased, increased, or remained stable [47]. Socioeconomic position interacted with social trust to lead to discrepancies in trajectories, with increases in trust observed among people in a higher socioeconomic position and decreases among people in a lower socioeconomic position [47]. Complicating this relationship is data from Sweden, which indicates greater non-compliance in public health measures among people in higher socioeconomic positions [15]. The income gradient in COVID-19 mortality has been well established across various contexts, with higher mortality rates in lower income groups and among people with higher sociodemographic risk factors [48, 49]. Further, counties with greater income inequalities in the United States had higher COVID-19 mortality [50, 51]. While data originated from different countries, these findings suggest a potential mechanism wherein non-compliance with public health measures in conjunction with lower mortality, both in higher socioeconomic groups, may be driving lower social trust among people in lower socioeconomic positions. Future research should delineate the relationship between income inequality and social trust within the US.
This analysis has important limitations to consider. This is a cross-sectional analysis, and social trust was measured at a single point in time for each participant; as such, it is not possible to conclude whether COVID-19 increased or decreased social trust. It is feasible that levels of social trust varied between the time when responses were collected and the onset of the COVID-19 pandemic. Additionally, it is feasible that people who are socially connected versus disconnected contracted COVID-19 at different time points throughout the pandemic. A time series analysis is warranted in future studies, to further our understanding of trajectories of COVID-19 infection and mortality across the spectrum of social trust. While we included a priori hypothesized confounders, we cannot eliminate nor rule out unmeasured or residual confounding. Lastly, measures of social trust are likely not generalizable at the county level and are subject to change over time. Future work should investigate social trust in differing contexts and at multiple levels of social organization, given regional variations in social trust [52]. Exploring social trust across countries in different world regions is important for understanding the complexity of the relationship between social trust and COVID-19 outcomes; while there is a dearth in the literature concerning social trust in low- and middle-income countries [53], examining social trust and COVID-19 outcomes within low- and middle-income countries would also help to inform how investment in building social trust could prevent future pandemics.
Conclusions
Using data from the pooled 2002–2018 General Social Survey, we find that higher mean social trust is associated with lower COVID-19 mortality. A complex interaction between non-compliance with public health measures in conjunction with income inequality could explain our results. We believe these findings highlight the importance of social trust as a means of emergency preparedness. Further exploration into the investment of social trust within communities as a prevention measure for future pandemics is warranted.
Data availability
This study uses secondary data publicly available from: the National Opinion Research Council General Social Survey (GSS) (https://gss.norc.org/Get-The-Data); the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (https://coronavirus.jhu.edu/map.html); the American Community Survey (https://www.census.gov/programs-surveys/acs); the County Health Rankings & Roadmaps (CHRR) (https://www.countyhealthrankings.org); and, the 2020 US presidential election results, available from GitHub (https://github.com/tonmcg/US_County_Level_Election_Results_08-20). The authors do not own nor control these datasets.
References
Centers for Disease Control and Prevention (CDC). COVID-19 Mortality Overview: Provisional Death Counts for Coronavirus Disease 2019 (COVID-19). https://www.cdc.gov/nchs/covid19/mortality-overview.htm. Published 2022. Accessed Oct 24, 2022.
Centers for Disease Control and Prevention (CDC). Excess Deaths Associated with COVID-19. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm. Published 2022. Accessed Oct 24, 2022.
Elgar FJ, Stefaniak A, Wohl MJA. The trouble with trust: time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc Sci Med. 2020;263:113365.
Makridis CA, Wu C. How social capital helps communities weather the COVID-19 pandemic. PLoS ONE. 2021;16(1):e0245135.
Imbulana Arachchi J, Managi S. The role of social capital in COVID-19 deaths. BMC Public Health. 2021;21(1):434.
Kawachi I, Berkman LF. Social Epidemiology. Social Capital, Social Cohesion, and Health. Oxford University Press; 2015.
Harpham T, Grant E, Thomas E. Measuring social capital within health surveys: key issues. Health Policy Plan. 2002;17(1):106–11.
Putnam RD, Leonardi R, Nanetti RY. Making Democracy Work: Civic traditions in modern Italy. Princeton University Press; 1994.
Coleman JS. Social Capital in the creation of Human Capital. Am J Sociol. 1988;94:S95–120.
Kim D, Kawachi I. U.S. state-level social capital and health-related quality of life: multilevel evidence of main, mediating, and modifying effects. Ann Epidemiol. 2007;17(4):258–69.
Kim D, Baum CF, Ganz ML, Subramanian SV, Kawachi I. The contextual effects of social capital on health: a cross-national instrumental variable analysis. Soc Sci Med. 2011;73(12):1689–97.
Habibov N, Cheung A, Auchynnikava A. Does social trust increase willingness to pay taxes to improve public healthcare? Cross-sectional cross-country instrumental variable analysis. Soc Sci Med. 2017;189:25–34.
Card KG. Collectivism, individualism and COVID-19 prevention: a cross sectional study of personality, culture and behavior among canadians. Health Psychol Behav Med. 2022;10(1):415–38.
Bollyky TJ, Hulland EN, Barber RM, et al. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. 2022;399(10334):1489–512.
Nivette A, Ribeaud D, Murray A, et al. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: insights from a longitudinal cohort study. Soc Sci Med. 2021;268:113370.
Siegrist M, Bearth A. Worldviews, trust, and risk perceptions shape public acceptance of COVID-19 public health measures. Proc Natl Acad Sci U S A. 2021;118:24.
Goldstein DAN, Wiedemann J. Who do you trust? The consequences of partisanship and trust for public responsiveness to COVID-19 orders. Perspect Politics. 2022;20(2):412–38.
Min J. Does social trust slow down or speed up the transmission of COVID-19? PLoS ONE. 2020;15(12):e0244273.
Yuan H, Long Q, Huang G, Huang L, Luo S. Different roles of interpersonal trust and institutional trust in COVID-19 pandemic control. Soc Sci Med. 2022;293:114677.
Zhang Z, Liu G, Chen B, Huang K. Social asset or social liability? How partisanship moderates the relationship between social capital and Covid-19 vaccination rates across United States counties. Soc Sci Med. 2022;311:115325.
Woelfert FS, Kunst JR. How political and Social Trust can Impact Social Distancing practices during COVID-19 in unexpected ways. Front Psychol. 2020;11:572966.
The General Social Survey (GSS). GSS Documentation. NORC at the University of Chicago. https://gss.norc.org/get-documentation. Accessed June 7, 2022.
Giordano GN, Mewes J, Miething A. Trust and all-cause mortality: a multilevel study of US General Social Survey data (1978–2010). J Epidemiol Community Health. 2019;73(1):50–5.
Johns Hopkins University Center for Systems Science and Engineering (CSSE). COVID-19 Dashboard. https://coronavirus.jhu.edu/map.html. Updated June 6, 2022. Accessed June 6, 2022.
United States Census Bureau. American Community Survey (ACS). https://www.census.gov/programs-surveys/acs. Accessed Dec 13, 2022.
County Health Rankings & Roadmaps (CHRR). Rankings data & documentation. https://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation. Published 2023. Accessed Aug 9, 2023.
McGovern T. United States General Election Presidential Results by County from 2008 to 2020. https://github.com/tonmcg/US_County_Level_Election_Results_08-20. Published 2020. Accessed Aug 9, 2023.
United States Census Bureau. American National Standards Institute (ANSI) and Federal Information Processing Series. (FIPS) Codes. https://www.census.gov/library/reference/code-lists/ansi.html. Accessed Dec 13, 2022.
Davern M, Bautista R, Freese J, Morgan SL, Smith TW. General Social Survey 2021 Cross-section. Chicago 2021.
Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons from Ebola. Lancet. 2015;385(9980):1910–2.
Blair RA, Morse BS, Tsai LL. Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc Sci Med. 2017;172:89–97.
Hikichi H, Tsuboya T, Aida J, et al. Social capital and cognitive decline in the aftermath of a natural disaster: a natural experiment from the 2011 Great East Japan Earthquake and Tsunami. Lancet Planet Health. 2017;1(3):e105–13.
Rodgers J, Valuev AV, Hswen Y, Subramanian SV. Social capital and physical health: an updated review of the literature for 2007–2018. Soc Sci Med. 2019;236:112360.
Takahashi T, Ikeda K, Ishikawa M et al. Interpersonal trust and social stress-induced cortisol elevation. NeuroReport 2005;16(2).
Kawachi I, Kennedy BP, Lochner K, Prothrow-Stith D. Social capital, income inequality, and mortality. Am J Public Health. 1997;87(9):1491–8.
Choi S, Oh J, Park SM, et al. Association of community level social trust and reciprocity with mortality: a retrospective cohort study. BMC Public Health. 2020;20(1):1793.
Nyqvist F, Victor CR, Forsman AK, Cattan M. The association between social capital and loneliness in different age groups: a population-based study in Western Finland. BMC Public Health. 2016;16(1):542.
House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–5.
Holt-Lunstad J, Smith TB, Layton JB. Social relationships and Mortality Risk: a Meta-analytic review. PLoS Med. 2010;7(7):e1000316.
Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156.
Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart. 2016;102(13):1009–16.
Jaremka LM, Fagundes CP, Peng J, et al. Loneliness promotes inflammation during acute stress. Psychol Sci. 2013;24(7):1089–97.
Lamontagne SJ, Pizzagalli DA, Olmstead MC. Does inflammation link stress to poor COVID-19 outcome? Stress Health. 2021;37(3):401–14.
Stephen G, Siobhán H, Muldoon OT, Whittaker AC. Social cohesion and loneliness are associated with the antibody response to COVID-19 vaccination. Brain Behav Immun. 2022;103:179–85.
Pew Research Center. Trust and Distrust in America. Pew Research Center. https://www.pewresearch.org/politics/2019/07/22/the-state-of-personal-trust/. Published 2019. Updated July 22, 2019. Accessed June 9, 2022.
Lochner K, Kawachi I, Kennedy BP. Social capital: a guide to its measurement. Health Place. 1999;5(4):259–70.
Wu C, Bierman A, Schieman S. Socioeconomic stratification and trajectories of social trust during COVID-19. Soc Sci Res 2022:102750.
Arceo-Gomez EO, Campos-Vazquez RM, Esquivel G, Alcaraz E, Martinez LA, Lopez NG. The income gradient in COVID-19 mortality and hospitalisation: an observational study with social security administrative records in Mexico. Lancet Reg Health – Americas 2022;6.
Karmakar M, Lantz PM, Tipirneni R. Association of Social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462–2036462.
Tan AX, Hinman JA, Abdel Magid HS, Nelson LM, Odden MC. Association between Income Inequality and County-Level COVID-19 cases and deaths in the US. JAMA Netw Open. 2021;4(5):e218799–218799.
Oronce CIA, Scannell CA, Kawachi I, Tsugawa Y. Association between State-Level Income Inequality and COVID-19 cases and mortality in the USA. J Gen Intern Med. 2020;35(9):2791–3.
McKay L, Jennings W, Stoker G. Social ties, trust and the geography of discontent. Camb J Reg Econ Soc. 2024;17(1):17–36.
Agampodi TC, Agampodi SB, Glozier N, Siribaddana S. Measurement of social capital in relation to health in low and middle income countries (LMIC): a systematic review. Soc Sci Med. 2015;128:95–104.
Acknowledgements
We sincerely thank GSS participants for their contributions. All inferences, opinions, and conclusions drawn in this paper are those of the authors, and do not reflect the opinions or policies of the National Opinion Research Council.
Funding
Ms. Marziali is a pre-doctoral fellow supported by NIDA T32DA031099. Dr. Card is supported by a Scholar Award from Michael Smith Health Research BC.
Author information
Authors and Affiliations
Contributions
MEM, KGC, RSH conceptualized and designed the study. KGC, AH analyzed the data. All authors aided in writing, editing, and final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We received IRB approval for secondary data analysis from Simon Fraser University (30002122).
Consent for publication
Not applicable as no individual data appears in this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Marziali, M.E., Hogg, R.S., Hu, A. et al. Social trust and COVID-19 mortality in the United States: lessons in planning for future pandemics using data from the general social survey. BMC Public Health 24, 2323 (2024). https://doi.org/10.1186/s12889-024-19805-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19805-y