Abstract
Introduction
The majority of maternal and newborn deaths take place during the first few hours and days after birth and thus postnatal contacts should begin as early as possible, especially within the first 24 h, then again within two to three days after delivery. Globally, early postnatal discharge has increased over the past 50 years and currently too. Even if Ethiopia has very low PNC coverage, there is no evidence on who is discharged early. Hence, the aim of this study was to determine the magnitude and the predictors for early postnatal discharge in Ethiopia.
Methods
This study was based on the secondary data analysis using the Ethiopian Demographic and Health survey (EDHS) 2016 data set. The weighted sample of 2,225 delivered mothers were included for the final analysis. The model was best fitted as assessed by Hosmer-Lemeshow test (p value = 0.1988). The variables with P-value ≤ 0.2 in the bi- variable binary logistic regression analysis were included in to the multi-variable binary logistic regression analysis. The Adjusted Odds Ratio (AOR) with 95% confidence interval (95% CI) was computed to assess the strength of association between the outcome and independent variables. The variables with a P-value of less than 0.05 in the multi-variable binary logistic regression analysis were declared as statistically significant predictors of the outcome variable.
Result
The overall magnitude of early discharge was 70.41% (CI: 68.48, 72.30). Residence (rural; AOR: 0.61, 95% CI: 0.46, 0.80), educational status (No education; AOR: 1.87, 95% CI: 1.19, 2.94), religion (Muslim; AOR: 0.69, 95% CI: 0.55, 0.87, Others; AOR: 0.24, 95% CI: 0.10, 0.57), wealth index (Poor; AOR: 0.77; 95% CI: 0.59, 0.99), marital status (Not married; AOR: 0.29; 95% CI: 0.13, 0.67), ANC visits (No ANC visits; AOR: 0.63; 95% CI: 0.46,0.86), parity (3rd parity; AOR: 1.48; 95% CI: 1.03, 2.11), and size of the child (larger size; AOR: 0.63;95% CI: 0.50,0.79, (smaller size; AOR: 0.72; 95% CI: 0.56,0.92) were independent determinants of early discharge.
Conclusion
A substantial proportions of mothers in Ethiopia had been discharged early (before 24 h). Residence, education, wealth index, religion, marital status, ANC follow up, parity and size of the child were predictors of early discharge. Adequate hospital stay should be promoted. Since the early discharge in Ethiopia is very high, home based postnatal visit should be strengthened focusing the identified predictors.
Similar content being viewed by others
Introduction
Duration of postnatal hospital stay has declined rapidly in the past three/ four decades [1]. Globally, there is variation in postnatal length of stay (LoS). In spite of an increase in medical interventions during pregnancy and childbirth, there is a reduction in the LoS in the facility after child birth for women and infants. Many high income counties, such as the United Kingdom, Australia, and Canada, have an average stay of 1.5, 2.8, and 1.7 days, respectively [2]. There is some evidence suggesting that low-risk women and babies are being discharged from 4 to 6 h following birth [3, 4].
Early hospital discharge after child birth generally refers to the postpartum hospital discharge of the mother and newborn within 48 hours [5]. The cut points on the duration on early discharge across countries varies from 12 to 72 hours [6]. Newborns’ and Mothers’ Health Protection Act (NMHPA) of United States government’ in 1996 ensures coverage of a hospital stay for 48 h following vaginal birth for parents [7]. The Spanish Association of Pediatrics also recommended a discharge from the hospital after 48 h following birth for healthy newborns [8]. The World Health Organization (WHO) recommends healthy mothers and newborns to stay and receive care at the facility for at least 24 h following an uncomplicated vaginal delivery at a health facility [9]. Because the majority of maternal and newborn deaths take place during the first few hours and days after birth, postnatal contacts should begin as early as possible in the postnatal period, especially within the first 24 h, then again within two to three days after delivery [10].
The large gap in postnatal care coverage is evident in a recent analysis of Demographic and Health Surveys in 23 African countries. Approximately, one-third of women in sub-Saharan Africa give birth in facilities, and less than 13% receive a postnatal care visit within two days of delivery [10, 11]. Early postnatal care is needed to encourage preventive behaviors and practices, to increase the likelihood that potentially life-threatening complications are detected, referred, and treated as early as possible and to provide the mother with important information on caring for herself and her baby [12].
The adverse outcomes of early discharge includes insufficient time for women and babies to establish breastfeeding [13, 14], delay in the identification and treatment of maternal and infant complications (jaundice, dehydration, infections), increased infant and maternal readmissions within 28 days, decreased maternal confidence due to lack of professional support, less maternal satisfaction with postnatal hospital care, and increased prevalence of maternal depression [14,15,16,17,18]. On the contrary, others suggested that early discharge from health facility creates opportunities for family-centered care, creates greater opportunities for families to bond in their home environment and is a safe and cost-effective way to provide postnatal care [19, 20].
The 2016 EDHS found that among women age 15–49 giving birth, 17% had a postnatal check during the first 2 days after birth. Four in five women (81%) did not receive a postnatal check [21]. Even though global early postnatal discharge has increased over the past 50 years and today, and Ethiopia has very low PNC coverage, there is no evidence on “what proportions of mothers are being discharged early and what are the predictors of early postnatal discharge?” The main objective of this study was determining the magnitude of early postnatal discharge and to identify potential predictors for early postnatal discharge in Ethiopia. The evidence from this study will allow policy makers, program mangers and clinicians to improve quality of postnatal care. It will also give an insight for researchers to investigate some controversial findings.
Methods
Study setting, study design, period
This was a cross-sectional study conducted in Ethiopia based on the fourth Ethiopian demographic and health survey data (EDHS, 2016). The EDHS 2016 was conducted from January 18 to June 27, 2016 [21]. Ethiopia is the second most populous country in Africa which is federally decentralized into ten regions and two city administrations [21] and ithas a total estimated 118,977,453 population [22]. The 2016 EDHS was cross-sectional by design. Secondary data analysis was performed using evidence from the EDHS 2016 data set which is the latest national survey conducted in nine regional states and two administrative cities. The EDHS 2016 was based on 645 enumeration areas.
Data source, study population and sampling
The sample for DHS survey was designed to represent all regions and administrative cities in the country. The survey participants were selected using stratified and two stage sampling methods: enumeration areas (EAs) in the first stage and households in the second stage. Each region was stratified into urban and rural areas. Then probability proportional allocation to sample size was made. For the 2016 DHS, 645 enumeration areas (EAs) were selected. From this, 202 EAs were from urban and 443 were from rural areas. We have used individual record (IR) data set of EDHS 2016 for this study. The data was accessed from measure DHS website (http://www.measuredhs.com) A total of 2,225 weighted mothers who gave birth vaginally were included for the final analysis. All the frequencies and the percentages in the result section were weighted.
The summary of the sampling technique was described as follows (Fig. 1).
Variables and measurements
The outcome variable was early discharge after vaginal birth. It was dichotomized as (yes/no). In EDHS, women who gave birth in health facilities were asked ‘How long after (NAME of the new born) was delivered did you stay there?’ The responses were recorded in hours (if less than a day), days (if less than a week) and weeks (if less than a month). We dichotomized the outcome variable based on the WHO recommendation as early discharge (yes) if length of stay in the health facility was < 24 h and not early discharge (No) if length of stay was ≥ 24 h) [23].
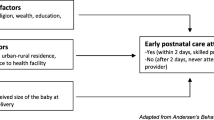
The independent variables were socio-demographic characteristics including the maternal age, educational level, marital status, place of residence, wealth index, religion, and working status and obstetric characteristics like place of delivery, pregnancy type, size of the child, parity, gestational age, wantedness of pregnancy, history of abortion, antenatal care utilization and gestational age.
Wealth index
In the dataset, the categories for wealth index were presented as Poorest, Poorer, Middle, Richer, and Richest [21]. In our study, a new variable was generated which had three categories “Poor”, “Middle” and “Rich” by merging poorest with poorer and richest with richer.
Religion
In the 2016 EDHS, religion had subcategories of Orthodox, Muslim, Protestant, Catholic, traditional followers and others [21]. In our study, the former three were encoded independently and Catholic and traditional religion followers were merged to others category.
Data processing and analysis
This study used the extracted data from EDHS 2016 individual record (IR file) folder. The data extraction and analysis was done using STATA version 14 software. Before analysis, data was cleaned using frequency; listing and sorting to identify any missed values. The time spent at health facility was incomplete for 933 mothers and were excluded. The model fitness was assessed using Hosmer-Lemeshow test. It was best fitted (p value = 0.1988). Variables with p-value ≤ 0.2 in the bi-variable binary logistic regression analysis were included in to the multi-variable binary logistic regression analysis. The Adjusted Odds Ratio (AOR) with 95% confidence interval (95% CI) was computed to determine the association between early discharge and the independent variables. Variables with a P-value of less than 0.05 in the multi variable binary logistic regression analysis were declared as statistically significant predictors of the outcome variable.
Result
Socio-demographic characteristics of mothers
Two thousand two hundred twenty five (2,225) mothers were included in this study. About 30% of mothers were within the age range of 25 to 29 years. More than two third(68.50%) of the mothers were rural residents. The educational status of study participants ranges from 7.3% (higher education) to 41.20% (no education). Nearly half (48.10%) of mothers were orthodox followers. Virtually all (99%) of the mothers were married. Almost half (49.12%) of the mothers were not working (Table 1).
Obstetrics characteristics of mothers
More than half(55.28%) of the mothers had at least 4 antenatal care (ANC) visits. About 68% of the mothers had parity of less than four. Nearly 96% of mothers gave birth in public health facilities. About 92% of the mothers had history of abortion (Table 2).
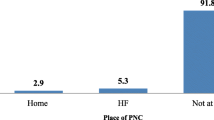
Magnitude of early discharge (ED)
In this study, the overall magnitude of early discharge after childbirth was 70.41% (CI: 68.48, 72.30). However, this magnitude varied across mothers’ characteristics. For example, it was 77.32% in urban and 67.24% in rural. Similarly, the magnitude of early discharge ranged from 66% for primary education to 75% for secondary education. It also varied by marital status (40.95% among not married and 70.80% among married) (Table 1).
ED was 57.43% among mothers who had no ANC visit while it was 71.95% among mothers who had four and more ANC visits. ED also varied by the size of the child. It ranged from 65.03% for larger size to 76.03% for average size of the child (Table 2).
Factors associated with early discharge
Among thirteen independent variables entered in to multivariable analysis, eight variables (residence, education, religion, wealth index, marital status, ANC visit, parity, and size of the child) were statistically and significantly associated with early discharge.
Mothers from the rural area had a 39% reduced risk of early discharge compared to their urban counter parts (rural; AOR: 0.61, 95% CI: 0.46, 0.80). None educated mothers had 1.87 times higher risk of early discharge compared to their higher education counter parts (No education; AOR: 1.87, 95% CI: 1.19, 2.94). Muslim follower mothers had a 31% reduced risk of early discharge compared to their orthodox counter parts (Muslim; AOR: 0.69, 95% CI: 0.55, 0.87). Others religion follower mothers had 76% reduced risk of early discharge compared to their orthodox counter parts (Others; AOR: 0.24, 95% CI: 0.10, 0.57). Mothers who had no ANC visits had a 37% reduced risk of early discharge compared to mothers who had 4 or more ANC visits (No ANC visits; AOR: 0.63; 95% CI: 0.46, 0.86). Para 3 mothers were 1.48 times more likely to be discharged early compared to mothers who were more than Para 3 (3rd parity; AOR: 1.48; 95% CI: 1.03, 2.11). Mothers who gave birth for larger size child had a 37% reduced risk of early discharge compared to mothers who gave birth for average size child (larger size; AOR: 0.63; 95% CI: 0.50,0.79). Mothers who gave birth for smaller size child had 28% reduced risk of early discharge compared to mothers who gave birth for average size child (smaller size; AOR: 0.72; 95% CI: 0.56,0.92). Mothers who were not married had 71% reduced risk of early discharge compared to married mothers (Not married; AOR: 0.29; 95% CI: 0.13, 0.67). Mothers who were in the poor economic class had 23% reduced risk of early discharge compared to the mothers in the rich economic class (Poor; AOR: 0.77; 95% CI: 0.59, 0.99) (Table 3).
Discussion
The primary objective of this study was to determine the magnitude of early discharge (ED) after vaginal delivery in the health facilities and to identify its associated factors.
In our study, the magnitude of ED was 70.41% (CI: 68.48, 72.30). This finding was higher than the study from Ghana [24] in which the 37.6% mothers were discharged within 24 h following birth, Nepal [25] in which early discharge was 61.7% and Beirut [26] in which 64% were discharged early. The observed variation in the magnitude of ED might be due to the difference in the study population. For instance, in our study mothers who gave birth by cesarean section were excluded while they were included in the Nepal, Ghana, and Beirut studies. This is obvious that mothers who gave birth by cesarean section will stay longer in hospital [27]. Generally the highest percentage of early discharge in Ethiopia may be due to the existing facility limitations such as lack of space to stay [28]. As a result, there might be pressure from a health facility to leave early to accommodate other mothers.
The mothers’ residence, educational status, religion, wealth index, marital status, ANC visit, parity, and size of the child were statistically significant determinant factors for early discharge. In our study, mothers from rural and poor economic status stayed longer in health facilities. This finding was supported by other findings from 30 low-and middle-income countries [2]. The possible explanation might be, women in rural areas and who are poor visits health facilities when there is complication. As a result, complicated case takes longer time to recover. But this finding contradicted with the finding in India [29] which stated that women from rural and in the poor economic class stayed shorter due to fear of cost of the services. This difference could be explained by the fact that maternal health services are free of charge in Ethiopia. This contradiction needs further investigation.
Another finding of our study was, women who gave birth for larger and smaller size neonates stayed longer than mothers who gave birth for neonates of average size. This finding was supported by other studies conducted in Ethiopia [30] and south Africa [31] which stated that the length of hospital stay increased proportionally with decreasing birth weight. This might be explained by low birth weight neonates are at risk many complications like hypothermia, apnea, and respiratory distress syndrome [32]. So, mothers with low birth weight neonates may wait longer till their new borns recovered.
In our study non educated mothers stayed shorter duration compared to mothers with higher education. This study was supported by findings from India [33] and Nepal [25] which stated that women who are less educated and come from poor families stayed shorter duration in health facilities. The possible explanation might be non educated mothers are not well informed about the health risks associated with child birth and they lack awareness about the benefit of staying more in the hospital and can’t anticipate further complications [33].
In our study, mothers currently not married stayed longer. This was supported by a study from 92 country [2]. The possible explanation could be not married women have high power of decision on admission and discharge than married women [34].
Limitation and strength
Using a national survey increases the representativeness of the results. However, our findings were based on survey data which may be influenced by recall bias. In addition to this, the EDHS data didn’t include facility and provider as well as family related variables which greatly affects the duration of stay.
Conclusion
Despite the fact that the first 24 h after childbirth provide a golden opportunity to tackle most maternal and neonatal morbidities and mortalities, a very large proportions of mothers in Ethiopia were discharged early (before 24 h). Residence, education, wealth index, religion, marital status, ANC follow up, parity and size of the child at birth were identified as the most significant predictors of early discharge. In addition to institutional delivery promotion, adequate hospital stay should be promoted. Since early discharge in Ethiopia is very high, the postnatal visit in the community should be strengthened focusing the identified predictors. Researchers are expected to further investigate the contradicted finding on rural residency and poor socio economic status. In addition, we would like to recommend researchers to conduct qualitative studies to investigate facility and provider as well as family related variables.
Data availability
The dataset supporting the conclusions of this article is available in the measure DHS website (http://www.measuredhs.com) upon request and the extracted data is available with the corresponding author.
Abbreviations
- AOR:
-
adjusted Odds Ratio
- COR:
-
Crude Odds ratio
- CI:
-
Confidence interval
- EDHS:
-
Ethiopia Demographic and Health Survey
- ED:
-
early discharge
- WHO:
-
World Health Organization
References
Brown S, Small R, Argus B, Davis PG, Krastev A. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database of Systematic Reviews. 2002;(3).
Campbell OM, Cegolon L, Macleod D, Benova L. Length of stay after childbirth in 92 countries and associated factors in 30 low-and middle-income countries: compilation of reported data and a cross-sectional analysis from nationally representative surveys. PLoS Med. 2016;13(3):e1001972.
2015 TRCoMPppcphwroug-icp-pAM.
Knight MKS, Brocklehurst P, Neilson J, Shakespeare J, Kurinczuk J, et al. Saving lives, improving mothers’ care—lessons learned to inform future maternity care from the UK and Ireland Confidential Enquires into maternal deaths and morbidity 2009–2012. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2014.
American Academy of Pediatrics. ACoOaGCotnIK SJ, Papile L, editors. Guidelines for perinatal care (eight ed.). Elk Grove Village, Ill: American Academy of Pediatrics. pp. 347–403.
Benahmed N, San Miguel L, Devos C, Fairon N, Christiaens W. Vaginal delivery: how does early hospital discharge affect mother and child outcomes? A systematic literature review. BMC Pregnancy Childbirth. 2017;17(1):1–14.
Medicare Cf, Services M. Newborns’ and mothers’ Health Protection Act (NMHPA). Centers for Medicare & Medicaid Services website.
Gracia SR, Muñuzuri AP, López ES, Castellanos JLL, Fernández IB, Campillo CWR, et al. Criteria for hospital discharge of the healthy term newborn after delivery. Anales de Pediatría (English Edition). 2017;86(5):289. e1-. e6.
Organization WH. WHO recommendations on postnatal care of the mother and newborn. World Health Organization; 2014.
Warren C, Daly P, Toure L, Mongi P. Postnatal care” in Opportunities for Africa’s Newborns, ed. Joy Lawn and Kate Kerber(Cape Town, South Africa: Partnership for Maternal, Newborn and childhealth, Save the children, UNFPA, UNICEF, USAID, WHO and partners). 2006:80–90.
Chervenak A, McCullough LB, Brent RL, Levene MI, Arabin B. Planned home birth: the professional responsibility response. American Journal of Obstetrics & Gynecology. Volume 208, Issue 1, January, pages 31–38. 2012.
Sines E, Syed U, Wall S, Worley H. Postnatal care: a critical opportunity to save mothers and newborns. Policy Perspect Newborn Health. 2007;1(7).
Gupta P, Malhotra S, Singh DK, Dua T. Length of postnatal stay in healthy newborns and re-hospitalization following their early discharge. Indian J Pediatr. 2006;73(10):897–900.
Britton JR, Britton HL, Beebe SA. Early discharge of the term newborn: a continued dilemma. Pediatrics. 1994;94(3):291–5.
Braveman P, Egerter S, Pearl M, Marchi K, Miller C. Early discharge of newborns and mothers: a critical review of the literature. Pediatrics. 1995;96(4):716–26.
Danielsen B, Castles AG, Damberg CL, Gould JB. Newborn discharge timing and readmissions: California, 1992–1995. Pediatrics. 2000;106(1):31–9.
Lain SJ, Roberts CL, Bowen JR, Nassar N. Early discharge of infants and risk of readmission for jaundice. Pediatrics. 2015;135(2):314–21.
Jones E, Stewart F, Taylor B, Davis PG, Brown SJ. Early postnatal discharge from hospital for healthy mothers and term infants. Cochrane Database of Systematic Reviews. 2021(6).
Waldenström U, Sundelin C, Lindmark G. Early and late discharge after hospital birth. Health of mother and infant in the postpartum period. Ups J Med Sci. 1987;92(3):301–14.
Madden JM, Soumerai SB, Lieu TA, Mandl KD, Zhang F, Ross-Degnan D. Effects of a law against early postpartum discharge on newborn follow-up, adverse events, and HMO expenditures. N Engl J Med. 2002;347(25):2031–8.
Central Statistical Agency - CSA/, Ethiopia ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia: CSA and ICF; 2017.
https://www.worldometers.info/world-population/ethiopia-population/. accessed on december 2021.
Organization WH. WHO recommendations on maternal health: guidelines approved by the WHO Guidelines Review Committee. World Health Organization; 2017.
Essien SK, Chireh B, Melese KG, Essien JKJPGPH. Predictors of prolonged hospitalization after vaginal birth in Ghana: a comparative study. 2022;2(1):e0000100.
Ikeda S, Shibanuma A, Silwal R, Jimba M. Factors associated with the length of stay at health facilities after childbirth among mothers and newborns in Dhading, Nepal: a cross-sectional study. BMJ open. 2021;11(5):e042058.
Farhat R, Rajab M. Length of postnatal hospital stay in healthy newborns and re-hospitalization following early discharge. North Am J Med Sci. 2011;3(3):146.
Nilsson IMS, Kronborg H, Knight CH, Strandberg-Larsen K. Early discharge following birth – what characterises mothers and newborns? Sex Reproductive Healthc. 2017;11:60–8.
Biadgo A, Legesse A, Estifanos AS, Singh K, Mulissa Z, Kiflie A, et al. Quality of maternal and newborn health care in Ethiopia: a cross-sectional study. BMC Health Serv Res. 2021;21(1):1–10.
Kumar P, Dhillon P. Length of stay after childbirth in India: a comparative study of public and private health institutions. BMC Pregnancy Childbirth. 2020;20(1):1–13.
Biru YB, Lemelem GA, Solomon N. Length of stay in health facilities after childbirth and associated maternal and neonatal factors in Ethiopia: a cross-sectional study from a national survey. BMJ open. 2021;11(12):e055327.
Mahovo R, Velaphi S. Duration of hospital stay and factors associated with prolonged hospital stay in very low birth weight infants surviving to hospital discharge. J Pediatr Perinatol Child Health. 2019;3(4):208–20.
Oluwafemi RO, Adesina FP, Hassan AO. Outcomes and Disease Spectrum of LBW Neonates in a Secondary Health Facility. Journal of Healthcare Engineering. 2022;2022.
Kumar P, Dhillon P. Length of stay after childbirth in India: a comparative study of public and private health institutions. BMC Pregnancy Childbirth. 2020;20(1):181.
Butler J, Morgan M. Marital status and hospital use. J Epidemiol Community Health. 1977;31(3):192–8.
Acknowledgements
We want to express our heartfelt thanks to the measure DHS program for allowing access EDHS dataset and authorized us to conduct this research using this data set.
Funding
No funding opportunity.
Author information
Authors and Affiliations
Contributions
This study was done in collaboration between all authors. DAB: conceived the idea for this study and design, participated in the analysis and write-up of the manuscript. YYG, MD, DGB, DS, AMS, WS, DC, AAA, AAK, HBE and MAS: Participated in the data extraction, data analysis, in interpretation of the result, in the manuscript write up and reviewing of the draft manuscript. All authors participated sufficiently in the work and take responsibility for the appropriate portions of the content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics and consent to participate
All procedures of Ethiopian Demographic and health survey were performed based on the international ethical guideline of the DHS program. According to the DHS report, all respondents’ data were anonymized during the collection of the data and it was done based on consent [21]. Since this study was conducted based on EDHS data, which is available by request from the measure DHS website (http://www.measuredhs.com), ethics approval was not required for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bitew, D.A., Diress, M., Gela, Y.Y. et al. Determinants of early discharge after birth among mothers delivered vaginally at health facilities: further analysis of the Ethiopian demographic health survey. BMC Public Health 23, 2128 (2023). https://doi.org/10.1186/s12889-023-16922-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-16922-y