Abstract
Background
Ocular siderosis (OS) is a significant cause of visual loss due to retained ferrous intraocular foreign bodies (IOFB). Despite its rarity, OS can lead to severe visual impairment if not promptly diagnosed and treated. This case is notable due to the occult nature of the IOFB, which was undetected by standard imaging modalities, emphasizing the critical role of magnetic resonance imaging (MRI) in such scenarios.
Case presentation
A 51-year-old Caucasian male presented with progressive vision loss in his right eye over 20 days. Best corrected visual acuity (BCVA) was 20/1000 in the right eye and 20/20 in the left eye. Intraocular pressure (IOP) was 9 mmHg in both eyes. Slit-lamp examination revealed a small linear corneal wound and an iris defect in the right eye, along with a cataract featuring brownish deposits on the anterior capsule. The left eye was normal. Fundus examination of the right eye was hindered by media opacities. Ultrasonography showed a flat retina and choroid with no detectable IOFB. Despite a strong clinical suspicion of OS, computed tomography (CT) did not detect any IOFB. MRI subsequently identified an artifact in the inferior sectors of the right eye, indicative of a metallic IOFB. Surgical intervention involved a 23-gauge vitrectomy, phacoemulsification, IOFB removal and silicon oil (SO) tamponade resulting in a fully restored VA of 20/20 and normal IOP one month post-operation. SO was removed 2 months later. The retina remained adherent with no PVR development, and optical coherence tomography (OCT) scans showed a normal macula.
Conclusions
This case underscores the importance of considering OS in patients with unexplained vision loss and history of ocular trauma, even when initial imaging fails to detect an IOFB. MRI proved crucial in identifying the IOFB, highlighting its value in the diagnostic process. Early detection and surgical removal of IOFBs are essential to prevent irreversible visual damage. This case demonstrates that MRI should be employed when CT and ultrasonography are inconclusive, ensuring accurate diagnosis and timely intervention to preserve vision.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Ocular siderosis (OS) is a relatively uncommon cause of vision loss, resulting from a retained ferrous intraocular foreign body (IOFB). IOFBs are present in 8 to 25% of all open globe injuries, and their presence can lead to severe acute complications such as endophthalmitis, or milder chronic conditions like OS, first described in 1890 by Bunge as “siderosis bulbi”. OS is believed to be caused by iron deposition in ocular tissues.
Early symptoms of OS include nyctalopia and decreased colour vision. Gradual vision impairment and progressive visual field loss are late stage symptoms. Common findings in OS patients in the anterior chamber include cataract development, iris heterochromia, pupillary mydriasis, and secondary open angle glaucoma. Additionally, rusty spots may develop on the anterior lens capsule due to iron deposition in epithelial cells, and the lens itself can appear yellowish with cataract formation. In the posterior segment, retinal arteriolar narrowing and sheathing with pigmentary retinal degeneration resembling retinitis pigmentosa are often observed. Optic neuropathy with optic disc swelling or hyperaemia and cystoid macular oedema can also occur.
Diagnosing OS involves both clinical examination and various imaging modalities. Electroretinography (ERG) is used to assess retinal damage due to OS, while fluorescein angiography (FA), electrooculogram (EOG), and visual field testing also provide valuable information.
In the case of a recent ocular injury, preventing OS development is a crucial reason to remove all ferrous IOFBs, aside from the increased risk of infection. If OS has already developed, removing the IOFB remains necessary to prevent further damage. The technical details of the surgery depend on the IOFB’s location and characteristics.
Herein, we report a case of OS due to an occult retained ferrous IOFB. The peculiarity of this case lies in the fact that the foreign body was not identifiable through clinical examination or even with CT.
Case presentation
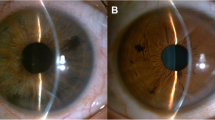
A 51-year-old Caucasian male reporting a progressive vision loss in his right eye in the past 20 days. Two months prior, the patient had a domestic accident while arranging some cooking tools. He sustained a corneal injury, which was sutured at the nearest hospital, with no mention of intraocular foreign bodies. On examination, visual acuity (VA) was 20/1000 in the right eye and 20/20 in the left eye, without any correction. Intraocular pressure (IOP) was 9 mmHg in both eyes. At the slit-lamp examination, in the right eye a small linear corneal wound were visible in temporal periphery, with an iris defect underlying; a cataract with brownish deposit on the anterior capsule was also present. No inflammation signs were found in the anterior chamber. Gonioscopy didn’t reveal any angle abnormalities.
The left eye examination was completely unremarkable. In the right eye, media opacities did not allow to perform a fundus examination, while it was normal in the fellow eye. US examination (Absolu, Quantel Medical, Cournon d’Auvergne, France) in the right eye revealed flat retina and choroid and no IOFBs were detectable (Fig. 1). Given the strong clinical suspicion of OS, an orbital CT was performed, with the aim of finding and localizing a ferrous IOFB. CT did not detect any IOFB (Fig. 2). Subsequently, orbital MRI was done, and an artefact was found in the inferior sectors of the right eye, likely related to metallic chemical shift. A first MRI at 1.5 Tesla was performed. Subsequently, a high-field (3 Tesla) examination was conducted to obtain more detailed information (Fig. 3).
Thus, surgery was aimed to remove the IOFB. The patient’s eye was prepared with povidone-iodine and draped and anaesthesia with retrobulbar block was applied. A complete -gauge vitrectomy was performed. Phacoemulsification was done through a 2.4 mm corneal tunnel. The IOFB was found at level of the inferior pars plana, with no evidence of MRI-induced damage. The IOFB was approximately square in shape, with each side measuring about 2 mm, and it was rather thin. Prior to the IOL implantation, a posterior capsulotomy was created with the vitreous cutter and the IOFB was removed through the corneal tunnel. The IOL was finally implanted in the ciliary sulcus, while the optical zone was luxated posteriorly to the anterior capsulorexis. Given the risk of proliferative vitreoretinopathy (PVR) associated with the presence of the IOFB, we chose silicon oil (SO) tamponade. Sclerotomies and the overlying conjunctiva were then sutured with 8 − 0 resorbable suture.
One month after surgery, BCVA was 20/20 and IOP was 9 mmHg. The IOL was perfectly centred and the retina adherent. OCT scan showed a completely normal macula. Two months after surgery, SO was removed: vision remained stable, with no PVR development.
Written informed consent for publication of his clinical details and clinical images was obtained from the patient.
Discussion and conclusions
OS represents a relatively uncommon and often misunderstood diagnosis and may develop a few days until several years after the trauma. Clinical signs can be highly variable and, despite a thorough ophthalmological evaluation, the IOFB can remain undetected. The interval between ocular trauma and the development of OS may be related to the severity of intraocular toxic reactions. The rate of OS development varies depending on several factors. An irregular roughened IOFB develops OS quicker than a smooth and regular IOFB. Moreover, small IOFBs may completely oxidize, so OS regresses. Additionally, the higher the IOFB iron content, the quicker the OS develops. Regarding IOFB location, OS occurs more rapidly when it is in the vitreous or aqueous humor than when it is encapsulated in tissues with low [1].
OS is thought to be due to the interaction between trivalent iron ions and proteins. Histologically, in the early phase OS shows damage to photoreceptors and RPE cells sparing Bruch’s membrane and the choroid; inner retinal layers are not involved, despite their proximity to the IOFB. [2]. In a following phase, the damage also includes the retinal vessels, with a consequent degeneration of internal retinal layers, supplied only by retinal capillaries. Therefore, in chronic OS, all retinal layers are compromised [3]. Rarely, OS can be caused by an IOFB presumed to not contain free iron, such as stone or steel, or by vitreous haemorrhage [4].
IOFB identification and its subsequent surgical removal are crucial to avoid a poor functional prognosis. A complete ophthalmologic examination is mandatory, with an accurate review of both the anterior and posterior segments. In the case of an undetected IOFB, orbital computed tomography (CT) is considered the gold standard, but ultrasonography (US) can also play an important role. Due to the risk of metallic IOFB movement [5], magnetic resonance imaging (MRI) should be reserved only for patients with suspected ocular injuries not detected by CT, such as subtle open-globe injury due to the non- metallic foreign body [6]. CT provides information about IOFB localization and size, with a sensitivity of 45–65% for IOFBs < 0.06 mm3 and of 100% for IOFBs > 0.06 mm3 [7]. In comparison to CT, MR is more effective in detecting non-magnetic IOFBs, with a sensitivity of 95% [8]. However, it is contraindicated when metallic IOFB is suspected: during MR, metallic IOFB can be moved and cause further damage. Therefore, MR should be reserved only for cases with suspected IOFB not detected by CT. In fact, rarely siderosis can be caused by an IOFB presumed to not contain free iron, such as stone or steel, or by vitreous haemorrhage [4, 9]. In these cases, CT cannot be able to recognize the IOFB and MR should be performed, preferably with high-field MR scans if available. Indeed, this type of foreign body, not identifiable on CT, can affect the magnetic field (and thus be recognized by MRI) but not to the extent that there is a risk of movement and local damage [10].
After OS diagnosis, surgery should be promptly referred for surgery, with the aim to remove the IOFB. Kannan et al. reported a visual improvement occurred in 78% patients following surgery [11]. This is similar to 75% reported by Hope-Ross et al. [12]. The visual potential in eyes with OS may be excellent if the siderotic changes stabilize or improve and if the optic nerve and macula have not been injured.
In conclusion, OS may represents a potential vision-threatening condition, often due to delayed presentation or missed diagnosis: in fact, IOFBs continue to be overlooked and workers at risk should be highly sensitized to wear protective glasses and undergo periodic clinical examination. In the case of any potential IOFB, a CT should be performed as the first step. If negative, MR should be promptly performed in presence of a strong suspect of IOFB or a clinical picture suggestive for OS.
Orbital MR scan of the right ocular bulb: in GRE axial sequence (thickness 3 mm. A), distortion of magnetic field is recognizable in the inferior quadrant of the right eye (arrow). In the 1.5 T T2-weighted sagittal plane (thickness 1 mm, B) an IOFB is clearly detected in the inferior quadrant of the right eye (arrowhead), better recognizable at the 3.0 T T2-weighted sagittal (thickness 1.5 mm, C, arrowhead) and coronal (thinness 2 mm, D, arrowhead) planes. (MR: magnetic resonance; GRE: gradient recalled echo; IOFB: intraocular foreign body)
Data availability
No datasets were generated or analysed during the current study.
References
Ballantyne JF. Siderosis Bulbi. Br J Ophthalmol. 1954;38(12):727–33.
Masciulli L, Anderson DR, Charles S. Experimental ocular siderosis in the squirrel monkey. Am J Ophthalmol. 1972;74(4):638–61.
Shaikh S, Blumenkranz MS. Fluorescein angiographic findings in ocular siderosis. Am J Ophthalmol. 2001;131(1):136–8.
Steel DH, Rosseinsky DR, James CR. Acute retinal toxicity caused by the bimetallic electrochemical action of a galvanized steel intraocular foreign body. Retina. 1998;18(1):77–9.
Ta CN, Bowman RW. Hyphema caused by a metallic intraocular foreign body during magnetic resonance imaging. Am J Ophthalmol. 2000;129(4):533–4.
Rao SK, Nunez D, Gahbauer H. MRI evaluation of an open globe injury. Emerg Radiol. 2003;10(3):144–6.
Chacko JG, Figueroa RE, Johnson MH, Marcus DM, Brooks SE. Detection and localization of steel intraocular foreign bodies using computed tomography. A comparison of helical and conventional axial scanning. Ophthalmology. 1997;104(2):319–23.
Moisseiev E, Last D, Goez D, Barak A, Mardor Y. Magnetic resonance imaging and computed tomography for the detection and characterization of nonmetallic intraocular foreign bodies. Retina. 2015;35(1):82–94.
Casini G, Sartini F, Loiudice P, Benini G, Menchini M. Ocular siderosis: a misdiagnosed cause of visual due to ferrous intraocular foreign bodies-epidemiology, pathogenesis, clinical signs, imaging and available treatment options. Doc Ophthalmol. 2021;142(2):133–52.
Zhang Y, Cheng J, Bai J, Ren C, Zhang Y, Gao X, et al. Tiny ferromagnetic intraocular foreign bodies detected by magnetic resonance imaging: a report of two cases. J Magn Reson Imaging. 2009;29(3):704–7.
Kannan NB, Adenuga OO, Rajan RP, Ramasamy K. Management of ocular siderosis: visual outcome and electroretinographic changes. J Ophthalmol. 2016;2016:7272465.
Hope-Ross M, Mahon GJ, Johnston PB. Ocular siderosis. Eye (Lond). 1993;7(Pt 3):419–25.
Acknowledgements
Not applicable.
Funding
No funds were received for this article.
Author information
Authors and Affiliations
Contributions
MM: conception, design, writing. LR, AB, FBP: imaging acquisition and analysis, manuscript revision. GP: manuscript revision.
Corresponding author
Ethics declarations
Ethical approval
Ethics approval and consent to participate not applicable.
Consent for publication
Written informed consent for publication of his clinical details and clinical images was obtained from the patient. A copy of the consent form is available for review by the Editor of this journal.
Competing interests
the authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mete, M., Romano, L., Beltramello, A. et al. Demystifying the role of magnetic resonance in identifying intraocular foreign bodies: a case of ocular siderosis. BMC Ophthalmol 24, 374 (2024). https://doi.org/10.1186/s12886-024-03649-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-024-03649-6