Abstract
Background
Retinal artery occlusion is a vascular entity caused by the temporary blockage of retinal arterioles.
Case presentation
We present the case of a 57-year-old woman a partial visual loss in the right eye due to a cilioretinal artery occlusion. Ophthalmoscopy revealed a focal area of retinal whitening superior to the optic nerve in the right eye, while the left eye was within the limit.
Retinal imaging, in particular optical coherence tomography angiography (OCTA), showed a capillary drop out of the superficial capillary plexus and the corresponding b-scan showed a round hyporeflective grey dot (optical empty) corresponding to the dark grey spot on the enface view at the level of the retinal whitening area.
Conclusion
Although the images did not allow the differentiation between vasospasm or retinal emboli, the OCTA imaging might help to identify and to caught in the act the specific region causing the retinal impairment. Also, the possible formation of small microcavity should be considered in case with branch retinal artery occlusion. The use of this new imaging technology might help to evaluate the efficacy of the therapy in vivo.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Retinal artery occlusion is a vascular entity caused by the temporary blockage of retinal arterioles. The occlusion can affect either the central retinal artery or a branch of this vessel. In this case, patients usually present sectoral visual field defect [1].
The vasospastic syndrome might involve the ocular circulation, especially in patients with migraine, and rarely cause a retinal arteriolar vasospasm [2].However, also minor microvasculature thromboembolic events of the capillary network might produce localized ischemic lesions.
In this case, non-invasive imaging modalities including fundus autofluorescence [3] and optical coherence tomography angiography (OCTA) [4, 5] have provided structural insights and also showed, for the first time in vivo, the vascular alteration into this retinal disease.
Case presentation
A 57-year-old woman presented with visual complaints described as a “foggy area” in the right eye.
There was no history of classic migraine, ocular pain, flashes, recent trauma or visual loss. The past medical history was also negative for any thromboembolic episodes as well as any primary Raynaud’s phenomenon. She was a non-smoker and referred being on a high dietary protein intake in the last few months. Recently, she was diagnosed with high blood pressure and was taking medication as prescribed. Haematological examinations were within the limits excluding the presence of high cholesterol levels.
In both eyes, the optic nerve was normal. There was not relative afferent pupillary defect and full colour vision was within the limits. Her best corrected visual acuity was 20/20 in both eyes. Both of her eyes were quiet with no conjunctival hyperaemia and no anterior chamber inflammation.
Ophthalmoscopy revealed a focal area of retinal whitening superior to the optic nerve consisting with branch retinal artery occlusion. There was no evidence of disc swelling or haemorrhages and examination of her fellow eye was normal. Gentle, prolonged ocular massage was applied.
Optical coherence tomography (OCT) and optical coherence tomography angiography (OCTA) (Heidelberg Engineering, Heidelberg, Germany) images were performed to rule out any other retinal lesions involving the macular area.
On presentation, the OCT b-scan shows a normal macular area in both eyes. Conversely, in the corresponding retinal whitening area, the b-scan showed a small area of retinal nerve fibre layer thickening. In this area, after 4 weeks, the b scan OCT showed a focal zone of retinal nerve fibre layer thinning (Fig. 1). At the same time, the visual complain was completely resolved.
Superiorly to the optic nerve, the ischemic lesion showing corresponding inner nuclear, inner plexiform, ganglion cell, and retinal nerve fibre layer on spectral domain optical coherence tomography (A). Four weeks after initial presentation affected layers revealed thinning and the inner nuclear layer is only partially identifiable (B)
Baseline and follow up of the inner nuclear layers thinning
The OCTA scan showed a capillary drop out of the superficial capillary plexus and the corresponding b-scan showed a round hyporeflective grey dot (optical empty) corresponding to the dark grey spot on the enface view at the level of the retinal whitening area.
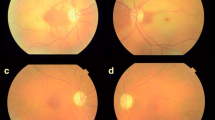
At follow- up, after 4 weeks, the OCTA scan showed a partial recovery of this focal vessel shut down of the superficial capillary plexus indicating an incomplete restoration of blood flow. The hyporeflective grey dot corresponding to the dark grey spot on the enface slab disappeared. Also, the ophthalmoscopy showed that the focal area of retinal whitening was resolved. (Fig. 2).
Portion of the colour fundus image of the right eye revealing one retinal whitish lesion (A), which was resolved after 4 weeks (B). The optical coherence tomography angiography (C) showed a capillary drop out at the level of the superficial capillary plexus, which was partially recovered at 4 weeks (D). At baseline, on the enface slab (E), the greyish area, encompassed between the two large vessel, displayed the dark dot (green circle). On the structural B-scan (F), this corresponded to the small hyporeflective dot within the hyperreflectivity band in the inner retina layers. At the follow up visit, in the corresponding area, only a thinning of the retinal nerve fibre layer is present (G and H)
Baseline and follow up of the optical coherence tomography angiography analysis
An echocardiogram and carotid Doppler sonography were obtained to assess for possible embolic retinitis. While the first examination was unremarkable, the second revealed < 50% stenosis within the right carotid bulb primarily indicating the presence of a cholesterol atherosclerotic plaque.
Discussion and conclusions
Branch artery occlusion can represent the earliest sign of cardiovascular diseases. In the acute phase, the non-perfused or partially perfused retinal area appears white.
It has been already found that the localization of the hyperreflectivity on SD-OCT b-scan can help not only to visualize which retinal layer are involved but also to show the progressive thinning of respective layers the retinal damage with time [6, 7].
This patient who complained of blurred vision in her right eye, with consistent focal OCTA findings, was diagnosed with branch retinal artery occlusion, which can be both associated with either retinal emboli or vasospasm. Very few cases have been described in the literature to date, with limited details regarding the patient history and follow-up.
Today, optical coherence tomography angiography provides the ophthalmologists with the new capability to promptly observe and assess the retinal changes due to the vascular impairment over time.
In patients with severe Raynaud's phenomenon, Salmenson et al. described persistent decrease in retinal capillary flow after cold stimuli, resolved at least 10 min after removal [8]. Furthermore, Ansari Y et showed the OCTA findings in the superficial capillary plexus in a case of sudden onset of peripheral visual deficit secondary to retinal artery spasm in Raynaud’s phenomenon [5]. However, the case presented did not suffer with Raynaud's disease.
On the other hand, small microvasculature thromboembolic events of the capillary network in turn can also cause localized ischemic lesions, limited to particular retinal layers.
In a previous study, the appearance of the thromboembolic plaque, based on their component including collagen I, IV and calcium or cholesteryl esters, showed different emission spectrum [9]; nevertheless, OCTA cases of retinal thromboembolic plaque has not been shown.
In addition, since it is known that there is a threshold of the OCTA system necessary to register blood flow rate [10], it is interesting to speculate, as we shown in a previous study on hyporeflective microaneurysm [11], that the blood flow inside the hyporeflective dot might be turbulent or containing plasma with erythrocytes packed, and therefore not shown using OCTA [12, 13].
Moreover, the contribution of the long-term effects of higher dietary protein intake cannot be totally excluded. A previous study showed the relationship between high protein intake and increased incidence of cardiovascular events [14]. Furthermore, it was found that the prevalence of the metabolic syndrome is higher in a diet with low in carbohydrate and high in protein [15].
Finally, in this case reported, the retinal finding could be interpreted as a microcavity/cyst.
The microvacuolar changes have been already described in the macular area in patients with neurodegenerative diseases including autosomal dominant optic atrophy, multiple sclerosis, ischemic optic neuropathy, glaucoma [16,17,18,19]. This represents the result of swelling from diminished fluid clearance of the inner retina rather than from retinal vessels exudation. Müller cells have been implicated in fluid absorption and their dysfunction might be correlated with formation of micro-lacunae also in case with branch retinal artery occlusion.
In case with branch retinal artery occlusion, the OCTA imaging might help to identify in vivo and to caught in the act the specific region of the retinal impairment.
However, fundus autofluorescence and fluorescein angiography were not performed in this case and this can be considered a limitation of this study. Therefore, further studies are needed to discern between vasospasm as well as thromboembolic plaques, including the differentiation of their component, but also, the possible formation of small microcavity leading to new insights into the pathophysiology of this retinal disease.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- OCTA:
-
Optical coherence tomography angiography
- OCT:
-
Optical coherence tomography
References
Hayreh SS, Podhajsky PA, Zimmerman MB. Branch retinal artery occlusion: natural history of visual outcome. Ophthalmology. 2009;116(1188–94):1188-94.e1-4.
Lewinshtein D, Shevell MI, Rothner AD. Familial retinal migraines. Pediatr Neurol. 2004;30:356–7.
Munk MR, Mirza RG, Jampol LM. Imaging of a cilioretinal artery embolisation. Int J Mol Sci. 2014;15:15734–40.
Bonini Filho MA, Adhi M, de Carlo TE, Ferrara D, Baumal CR, Witkin AJ, Reichel E, Kuehlewein L, Sadda SR, Sarraf D, Duker JS, Waheed NK. Optical coherence tomography angiography in retinal artery occlusion. Retina. 2015;35:2339–46.
Ansari Y, Kale AU, Tallouzi MO, Manna A. Sudden onset peripheral visual deficit secondary to retinal artery spasm in Raynaud's phenomenon. BMJ Case Rep. 2021;14(2):e239954. https://doi.org/10.1136/bcr-2020-239954.
Aleman TS, Tapino PJ, Brucker AJ. Evidence of recurrent microvascular occlusions associated with acute branch retinal artery occlusion demonstrated with spectral-domain optical coherence tomography. Retina. 2012;32:1687–8.
Ritter M, Sacu S, Deák GG, Kircher K, Sayegh RG, Pruente C, Schmidt-Erfurth UM. In vivo identification of alteration of inner neurosensory layers in branch retinal artery occlusion. Br J Ophthalmol. 2012;96:201–7.
Salmenson BD, Reisman J, Sinclair SH, Burge D. Macular capillary hemodynamic changes associated with Raynaud’s phenomenon. Ophthalmology. 1992;99:914–9.
Uchida Y, Uchida Y, Kawai S, Kanamaru R, Sugiyama Y, Tomaru T, Maezawa Y, Kameda N. Detection of vulnerable coronary plaques by color fluorescent angioscopy. JACC Cardiovasc Imaging. 2010;3:398–408.
Seidel G, Aschinger G, Singer C, Herzog SA, Weger M, Haas A, Werkmeister RM, Schmetterer L, Garhöfer G. Estimating retinal blood flow velocities by optical coherence tomography. JAMA Ophthalmol. 2016;134:1104–10.
Parravano M, De Geronimo D, Scarinci F, Querques L, Virgili G, Simonett JM, Varano M, Bandello F, Querques G. Diabetic microaneurysms internal reflectivity on spectral-domain optical coherence tomography and optical coherence tomography angiography detection. Am J Ophthalmol. 2017;179:90–6.
Kadomoto S, Muraoka Y, Uji A, Ooto S, Murakami T, Tsujikawa A. Hemodynamic and structural changes in retinal arterial macroaneurysm after intravitreal anti-vascular endothelial growth factor injection. Am J Ophthalmol Case Rep. 2021;23: 101182.
Kadomoto S, Muraoka Y, Uji A, Tamiya R, Ooto S, Murakami T, Oritani Y, Kawai K, Tsujikawa A. Ultrastructure and hemodynamics of microaneurysms in retinal vein occlusion examined by an offset pinhole adaptive optics scanning light ophthalmoscope. Biomed Opt Express. 2020;11:6078–92.
Halbesma N, Bakker SJ, Jansen DF, Stolk RP, De Zeeuw D, De Jong PE, Gansevoort RT. High protein intake associates with cardiovascular events but not with loss of renal function. J Am Soc Nephrol. 2009;20:1797–804.
Skilton MR, Laville M, Cust AE, Moulin P, Bonnet F. The association between dietary macronutrient intake and the prevalence of the metabolic syndrome. Br J Nutr. 2008;100:400–7.
Eckmann-Hansen C, Bek T, Sander B, Grønskov K, Larsen M. Prevalence of macular microcystoid lacunae in autosomal dominant optic atrophy assessed with adaptive optics. J Neuroophthalmol. 2022. https://doi.org/10.1097/WNO.0000000000001592. Online ahead of print.
Gelfand JM, Nolan R, Schwartz DM, Graves J, Green AJ. Microcystic macular oedema in multiple sclerosis is associated with disease severity. Brain. 2012;135:1786–93.
Wolff B, Azar G, Vasseur V, Sahel JA, Vignal C, Mauget-Faÿsse M. Microcystic changes in the retinal internal nuclear layer associated with optic atrophy: a prospective study. J Ophthalmol. 2014;2014: 395189.
Kisimbi J, Shalchi Z, Mahroo OA, Mhina C, Sanyiwa AJ, Mabey D, Mohamed M, Plant GT. Macular spectral domain optical coherence tomography findings in Tanzanian endemic optic neuropathy. Brain. 2013;136:3418–26.
Acknowledgements
We thank Fondazione Roma (Rome, Italy) for continuous support.
Funding
Italian Ministry of Health provided financial support in the form of Ricerca Corrente funding. The sponsor had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Contributions
Study concept and design: FS and AC; Acquisition of data: FS; Analysis and interpretation of the data: FS, GR and MP; Drafting the manuscript: FS; Critical revision of the manuscript: MP, AC and GR. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent to publish this information was obtained from study participant.
Competing interests
Scarinci, Cacciamani and Ripandelli report no proprietary or financial interest to disclose.
Parravano reports personal fees from Allergan, from Bayer, and from Novartis outside the submitted work. The remaining authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Scarinci, F., Cacciamani, A., Ripandelli, G. et al. Branch retinal artery occlusion caught in the act by an optical coherence tomography angiography image: case report. BMC Ophthalmol 22, 303 (2022). https://doi.org/10.1186/s12886-022-02517-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-022-02517-5