Abstract
Objective
To identify the epidemiological profile and prognostic factors of open globe injuries that require emergency surgical treatment.
Design
Retrospective cohort study.
Subjects
Patients with OGI who underwent publicly funded emergency surgical treatment in the Federal District from 2014 to 2018.
Methods
Data were collected by reviewing electronic medical records through a questionnaire and tabulated. The statistical analysis was performed in SPSS Statistics 26.0.0.0 (p ≤ 0.05).
Results
A total of 359 records were included, corresponding to 336 eyes of 334 patients (294 males and 40 females). The average age was 32.7 years. The affected eye was the right eye in 165 cases, the left eye in 166 cases, and both eyes in 3 cases. The average time between injury and hospitalization was 75.7 h, and the time between injury and surgery averaged 173.7 h. The injury types were as follows: 197 penetrating; 109 rupture; 19 IOFB; 11 perforating. The injuries were in the following zones: 181 zone I; 82 zone II; 70 zone III. The OTS grades were as follows: 57 were classified as grade 1; 101 were grade 2; 142 were grade 3; 28 were grade 4; and 8 were 5. The most commonly performed surgeries were corneal suture, corneoscleral suture, and evisceration. The most common clinical features were traumatic cataract, herniated iris and hyphema. The following were risk factors for poor prognosis: zone III, time between trauma and surgery > 72 h, rupture injury, retinal detachment, disorganization of the eyeball, endophthalmitis, uveal prolapse, OTS classification 1 or 2, and low initial visual acuity. The following factors predicted a good prognosis: initial VA > 1/200, penetrating injury, OTS 4 and zone II.
Conclusions
The high frequency of many of these factors may explain the high rate of severe visual loss found. Injury localization in zone II was identified as a previously unrecognized protective factor against severe visual loss.
Similar content being viewed by others
Introduction
Ocular globe trauma is associated with several trauma mechanisms and forces involved, generating different types of injuries that are divided into open and closed. Open lesions result from the involvement of the entire thickness of the corneoscleral ocular structure. Closed injuries are those in which the corneoscleral eye structure remains intact [1,2,3,4,5].
The Birmingham Eye Trauma Terminology (BETT) system standardizes the names of mechanical injuries in the eye, connecting terminologies. Thus, open eye trauma is classified as rupture, referring to full-thickness injury of the globe by trauma with a blunt object, and laceration, when there is full-thickness injury of the globe caused by a sharp object. In addition, lacerations are subdivided into penetrating wounds, intraocular foreign bodies (IOFBs) and perforating wounds. The penetrating wound is marked by a simple laceration, whereas the IOFB is when the foreign object retained causes an entrance laceration. The perforating wound shows two full-thickness wounds on the eye structure, showing the entry and exit of the cutting object [6, 7].
Another classification, the Ocular Trauma Score (OTS), estimates the visual prognosis from clinical data such as initial visual acuity (VA), wound location and the relative afferent pupillary defect (DPAR). OTS ranges from 1 (most severe injury and worst prognosis at 6 months of follow-up) to 5 (less severe injury and better prognosis) [8,9,10,11,12].
The reality of the Federal District
The Federal District is a Federative Unit of Brazil that does not have municipalities; it is divided into 31 administrative regions. According to the last demographic census conducted in 2010, the population of the Federal District totaled 2.570.160 people [13].
The Integrated Development Region of the Federal District and Surroundings (RIDE) was ruled by Complementary Laws 94/1998 and 163/2018 to facilitate the articulation of administrative actions between the Union, the States of Goiás, Minas Gerais and the Federal District [14].
In the public network of the Federal District and the surrounding region, all patients who require emergency ophthalmic surgery due to laceration of the eyeball are referred to the Base Hospital of the Federal District by the guidelines of the Urgency and Emergency Protocols of the Federal District Health Department since 2006 [15]. Thus, the results obtained from sampling extracted from this hospital reflect the reality of the RIDE.
Methodology
Outline
This was a retrospective cohort study to determine the epidemiology and prognostic factors of open globe injuries (OGIs) that underwent emergency surgical treatment in a public tertiary hospital in the Federal District from 2014 to 2018.
The data were collected by reviewing electronic medical records and tabulating them in Microsoft® Excel for Mac, version 16.19. The statistical analysis was performed in SPSS Statistics 26.0.0.0 using the chi-square test, Fisher’s exact test and relative risk (RR), with p ≤ 0.05 as the criterion for statistical significance.
The chi-square test was performed for all variables, and those with more than 20% of cells with an expected count < 5 were also subjected to Fisher’s exact test. Those with a total count of 1 have not been tested. Factors for which the chi-square test showed a cell count of less than 5 above 20% were tested separately.
Relative risk was calculated only if the numerator ≠ 0.
Inclusion criteria
Patient victims of traumatic OGI underwent emergency surgical treatment in a public tertiary hospital in the Federal District, with injury and surgical procedures ranging from 01/01/2014 to 12/31/2018.
Exclusion criteria
Nontraumatic globe injury; traumatic closed globe injury; cases occurring outside the stipulated period; without minimal information in the medical records (mechanism of injury, date of injury, affected eye, date of surgery, initial visual acuity and after surgical procedure, type of surgery performed).
Variables
Independents: the origin (city and state), accident environment (home; work; traffic; others), age group (under 18 years; 18–39 years; 40–59 years; 60 years or older), biological sex (male; female), affected eye (right; left; both), type of injury (penetrating; rupture; IOFB; perforating), initial visual acuity (≥ 20/40; 20/50 to 20/200; 19/200 to 1/200; luminous perception (LP) or hand movement (HM); absence of light perception (ALP)), last visual acuity registered in the medical record after surgery (≥ 20/40; 20/50 to 20/200; 19/200 to 1/200; LP or HM; ALP), relative afferent pupillary defect (absent; present; not registered – NR), injury zone (zones: I – restricted to the cornea and limbus; II – from the limbus to 5 mm of surrounding sclera; and III – more than 5 mm from the limbus in the posterior direction along the sclera), time elapsed until hospitalization (≤12 h; > 12 to ≤24 h; > 24 to ≤72 h; > 72 h), time elapsed between trauma and surgery (≤12 h; > 12 to ≤24 h; > 24 to ≤72 h; > 72 h), surgery performed, associated clinical characteristics and calculation of OTS (1 to 5).
Dependent: visual loss, which was categorized as mild (last VA ≥ 20/200) or severe (last VA < 20/200).
Visual acuity was measured with a Snellen chart.
Results
A total of 781 records of urgent/emergency ophthalmologic surgeries were identified during the research period (2014 to 2018). Inclusion and exclusion criteria were applied (Fig. 1).
The final sample consisted of 359 records of surgeries, referring to 336 eyes and 334 patients, that were included in this study. Three patients had OGI in both eyes, but in one case, surgery was required in only one eye, since the lesion in the other eye was self-sealing and was treated conservatively. Twenty-three records were reoperations.
Demographic evaluation
The following origin distribution was found: 202 (60.48%) Federal District, 94 (28.14%) Goiás, 17 (5.09%) Bahia, 17 (5.09%) Minas Gerais, 1 (0.30%) Pernambuco, 1 (0.30%) São Paulo and 2 (0.60%) NR. A total of 291 patients came from RIDE.
In the Federal District, the most common origins were Planaltina (31 patients), Ceilândia (23), Sobradinho (20 patients), Gama (17), Samambaia (16) and Brasília (14).
Epidemiological evaluation
We found 294 (88.0%) males and 40 (12.0%) females in the records.
The average age was 32.74 years old, with extremes of 3 and 80 years and a median of 33 years. By age group, 84 patients (25.1%) were 18 years or younger, 131 (39.2%) were between 19 and 39 years, 94 (28.1%) were between 40 and 59 years and 25 (7.5%) were 60 years or older.
Regarding the injury environment, in 265 (79.3%) NRs, 29 (8.7%) occurred in traffic, 17 (5.1%) at work, 16 (4.8) %) at home, and 7 (2.1%) at other locations.
Analyzing the number of patients, 165 (49.4%) had the right eye affected, 166 (49.7%) had the left eye affected and 3 (0.9%) had both eyes affected. Two of the three bilateral cases occurred in traffic accidents.
The average time between injury and hospitalization was 75.7 h, but the median was 9 h. The average time between injury and surgery was 173.7 h, and the median was 72 h.
Regarding the frequency of the type of injury, 197 (58.6%) were penetrating, 109 (32.4%) were ruptures, 19 (5.7%) were IOFBs and 11 (3.3%) were perforating.
Regarding the afferent pupillary defect, the result was unreported in 314 cases (93.5%), negative in 16 (4.8%), and positive in 6 (1.8%).
As for the zone of the injury, 181 (53.9%) were zone I, 82 (24.4%) were zone II, 70 (20.8%) were zone III and 3 (0.9%) NR.
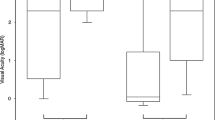
The initial VA values had the following frequencies: 66 (19.6%) ALP; 178 (53.0%) luminous perception (LP) or hand movement (HM); 52 (15.5%) between 1/200 and 19/200; 34 (10.1%) between 20/200 and 20/50; and 6 (1.8%) with 20/40 or more.
Regarding final VA, the average time between surgery and measurement was 223 days, and the results were as follows: 114 (33.9%) ALP; 96 (28.6%) LP or HM; 58 (17.3%) between 1/200 and 19/200; 36 (10.7%) between 20/200 and 20/50; and 32 (9.5%) with 20/40 or more.
Table 1 describes the performed procedures in descending order of frequency, and Table 2 describes the associated clinical characteristics, whether pre-existing or after the trauma.
When analyzing the distribution according to OTS grade, 57 (17,0%) are classified as 1, 101 (30.1%) as 2, 142 (42.3%) as 3, 28 (8.3%) as 4 and 8 (2.4%) as 5.
Visual loss and associated factors
After treatment, 137 (40.8%) of the eyes maintained their VA, 96 (28.6%) worsened and 103 (30.7%) improved. Of the total number of records, 68 (20.2%) presented mild loss, and 268 (79.8%) presented severe loss.
Table 3 shows the results of the association tests between the independent variables and visual loss and the relative risk of severe visual loss.
For biological sex, age group, DPAR and injury-to-hospitalization time, the tests showed no significant association with visual loss.
The types of injuries were tested one by one. Severe visual loss was shown to be significantly increased in rupture (p = 0.019) and penetrating trauma (p = 0.002). The perforating and IOFB types showed no association with visual loss.
Table 2 shows the correlation between associated clinical characteristics and visual loss. Retinal detachment, disorganization of the eyeball, endophthalmitis and uveal prolapse were shown to be statistically related to visual loss.
In the evaluation of the injury zone, a significant association with visual loss was noted by the chi-square test (p < 0.001), but this occurred only for zones II and III. Zone II was a protective factor, and zone III was a risk factor. Zone I showed no significant difference in severe and mild visual loss.
The OTS classification showed a statistical association with visual loss (p < 0.001). Subgroups 1 and 2 were risk factors, and subgroup 4 was a protective factor for severe visual loss. Subgroups 3 and 5 showed no significant difference.
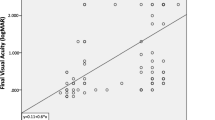
The chi-square test between initial VA and visual loss showed that there was a significant association (p < 0.001). The ALP and LP/HM subgroups had an increased risk of severe visual loss, and patients with an initial VA ≥1/200 had a reduced risk.
Regarding injury-to-surgery time, the subgroups “≤12 h”, “> 12 to ≤ 24 h” and “> 24 to ≤ 72 h” showed no significant association with severe visual loss. The “> 72 h” subgroup had a significant association, increasing in the probability of severe visual loss.
Discussion
OGI is a widely studied topic; however, there are few statistical data on its epidemiology in the Federal District [16, 17].
Rohr et al. (2016) identified the profile of pediatric globe injury in children under 15 who attended the Base Hospital in the Federal District between June 2012 and January 2013, of which only 20% had OGI (n = 103) [7]. Vieira (2007) outlined the profile of 2844 patients treated during September 2003 at the same hospital, identifying that 62% of the patients were male, 17% were from other states, and 30% of the patients were due to eye injury [18]. None of the two studies had the same focus as the present study, but they indicate the high frequency of eye injury in DF.
In the five years included in the survey, practically 70% of urgent/emergency ophthalmologic surgeries in the public network of the Federal District were due to eye injury, with the majority of these types of injuries being open (86.26%), which had an average of 93 cases per year. This corresponds to an incidence of 3.6/100,000 inhabitants, considering the DF population in the 2010 census. This result is in line with other publications that point to a higher frequency of surgery in OGI [19,20,21,22,23]. A Chinese study (n = 2009) in the period from 2010 to 2014 attributed 70.7% of eye injuries to OGI [22]. A ten-year study (2005–2014) in New Zealand including OGI that underwent surgical repair calculated an average incidence rate of 2.8/100,000 inhabitants, another in Turkey (2009–2013) found 3.5/100,000 per year and one in Israel (1996–2005) 3.1/100,000 inhabitants [24,25,26]. Compared to the New Zealand and Israel study, the incidence in DF was higher but very similar to that found in Turkey.
For every 10 cases, 4 were from other states, mainly Goiás. This represents almost twice as much as that found in a previous study at the same hospital that evaluated emergency room visits [18]. In 87.1% of the cases, the patients came from the RIDE.
There was an evident predominance in men, 88% of cases. These data are in line with several studies on ocular trauma, whether in general or specifically OGI, with a male frequency ranging from 73.3 to 90% [5, 9, 19,20,21,2,23,24,25, 27,28,29,30,31,32,33,34,35].
Approximately 67% of the patients were between 19 and 59 years old, with an average age of 32.7 years. In the literature, this average ranges from 30 to 38.3 years [5, 20, 35]. The exclusion of records that did not report visual acuity probably led to the exclusion of many neonates and preverbal children, in whom this measure is more difficult or impracticable.
The most affected age group is economically active, generally requiring time off work. In addition to their treatment expenses, these people stop producing. This shows the importance of reducing the time of care and hospitalization [22].
The frequency was similar between the two eyes, and injuries were rarely bilateral; these results were consistent with the findings of several prior studies, where the difference in laterality was no more than 10% [20, 24, 25, 27, 34, 36].
The lack of information about the trauma environment and DPAR in most of the records makes it impossible to correctly assess the distribution of these variables. In the literature, the main accident environments are work, traffic and home [37,38,39].
In Saudi Arabia, a similar study shows a penetrating type in 37.5% of cases; rupture by 32.5%; perforation in 26.7%, and IOFB in 3.3% [32]. In Israel, the frequency was IOFB in 38.1%; rupture by 28.9%; penetration in 27.1% and perforation in 5.9% [26]. In Turkey there is work showing penetration in 75% of cases, rupture in 13%, IOFB in 8%, and perforation in 4% [34]. In Portugal, penetration occurred in 48.9%, rupture at 31.9%, IOFB at 13.2%, and perforation at 2.2% [33]. In New Zealand, 56.4% penetrating; 35.6% rupture; 7.3% IOFB and 0.8% perforation [24]. In an Australian study, globe rupture and penetration were the most common injuries [30]. Except in the Israeli study, there was a tendency for greater involvement of the penetration and rupture types, as we found.
More than half of the lesions affected zone I, consistent with the literature, where it is the most frequently affected zone, between 38.1 and 53% [24,25,26, 32, 34,35,36].
The average time that is taken from trauma to hospital and surgery was above those found in other studies, which was between 4.9 h to 1.3 days and 5 h to 39,9 h, respectively, with 72.8–94.8% of the patients hospitalized within 24 h of the trauma [24, 25, 29, 33, 36, 40]. However, the median is a better evaluation parameter since the variables in question do not present a normal distribution and have extreme values [41]. The median values found were reasonable, but the time to surgery was still above the average of most studies.
Regarding the initial VA, the majority had LP/HM, which is very similar to that found in the literature [24, 25, 28, 31, 35, 40].
The most common final VA was ALP. The literature shows a wide range of variation in these result, with one study reporting that 65.6% had VA ≥ 20/200 and another reporting a predominance of ALP [25, 33]. Rao et al. (2010) showed that after 6 months, 34.8% of the patients had ≥20/70 vision, and the same number had < 20/400 [35]. In Saudi Arabia, 40.8% had vision between 20/200 and 20/50 [32]. In New Zealand, 46% of patients had vision ≥20/40 at the end of treatment [24].
Previous studies have observed VA improvement after treatment in most cases, varying between 55.7 and 58% of patients, while in our records, the majority had parameter maintenance [5, 26, 35].
We found that more than 70% of the traumas were classified as OTS 3 and 2, tending to be of medium to severe severity. A South African study had similar results, with 66.86% in these categories [27]. Ozturk et al. (2019) found a majority in 2 (45.2%) and 1 (33%) [36].
The most performed surgeries, in decreasing order, were corneal suture, corneoscleral suture, evisceration, scleral suture, and anterior chamber washing. There is a convergence that primary repair is the most frequent, followed by evisceration [5, 27].
The main associated clinical characteristics, in decreasing order, were traumatic cataract, iris hernia, hyphema, vitreous prolapse and uveal prolapse. There is a difference in the literature because of the high incidence of traumatic cataracts. Atik et al. (2018) found hyphema, herniated iris, vitreous hemorrhage, eyelid/eyebrow laceration, and traumatic cataracts as the most frequent cataracts [25]. Rao et al. (2010) reported herniated iris, hyphema, traumatic cataract, vitreous hemorrhage and endophthalmitis [35]. In a Saudi Arab study, the main ones were iris lesions, hyphema, vitreous hemorrhage, aphakia, and retinal damage [32].
The severe visual loss found (79.8%) was above that described in the literature. Atik et al. (2018) observed its occurrence in 65.6% of cases in a Turkish hospital [25]. Teixeira et al. (2014), in a Portuguese study, observed 60% after 6 months of trauma [33]. In New Zealand, Israel, and Saudi Arabia, this rate was much lower, 39.3, 40, and 45.9%, respectively [24, 26, 32].
We found a significant association with severe visual loss in lesion in zone III, time between trauma and surgery > 72 h, rupture injury, retinal detachment, disorganization of the eyeball, endophthalmitis, uveal prolapse, OTS classification 1 and 2, initial visual acuity ALP, LP or HM. Such results reaffirm what was found in previous research, which also relate the presence of relative afferent pupillary defect, extensive wound, eyelid laceration, hyphema, damage to the lens, vitreous prolapse and vitreous hemorrhage [5, 6,7,8,9, 27, 42,43,44,45,46]. The high frequency of these characteristics may explain why severe visual loss was found in almost 80% of cases. This also reaffirms the medium to high severity of this type of injury, indicated by the OTS calculation.
Initial VA > 1/200, penetrating injury, OTS 4 and zone II showed an inverse association with severe visual loss. In the literature, only zone II is not described as a protective factor. Other known protective factors are OTS 3, injury in zone I, pediatric age, and injury restricted to the anterior segment [26, 33,34,35].
Knowledge of prognostic factors enables specific and targeted actions aimed at reducing visual loss due to open eye trauma. Most factors are related to the severity and characteristics of the trauma, which could be improved by educational actions and guidance on the use of personal protective equipment in the work environment and in recreational activities [18].
In Brazil, Regulatory Norm number 6 establishes that companies must have their occupational risks estimated by a trained professional and provide all necessary safety equipment to their employees free of charge to avoid work accidents. It is up to the government to encourage and supervise correct compliance with the standard [47].
Another possible prognostic factor that could be modified is the time between trauma and surgery, which should be prioritized so that it occurs before 72 h. For this purpose, the community must be well informed about the points where emergency eye care is available. The Unified Health System is universal and free in Brazil; therefore, financial issues do not represent a problem for the user. Another point that could be improved is the duration of surgery after hospitalization. Surgeries are prioritized to take place according to the severity of the injury and risk of death or loss of function. The long surgical delays demonstrate the high demand for urgent/emergency surgeries, which could be resolved by expanding existing services and opening new care/surgery units. Another option would be the creation of an exclusive ophthalmology service, which would have more agility in performing these surgeries and addressing other ophthalmological urgencies/emergencies [48].
Conclusion
There have been several studies reviewing the epidemiology of open globe injury in different locations; these studies are in agreement that there is a predominance of males, young adults, and patients with low initial VA. The high morbidity of this type of injury emphasizes the importance of the use of personal protective equipment and the adoption of legislative regulations for eye safety, reducing the impact of globe injuries on the community [49,50,51].
Our research came up with similar results found in the literature, but with a greater divergence regarding the time between trauma and hospitalization/surgery, which can be improved, and we found Zone II as a protective factor for severe loss. The high frequency of poor prognosis factors may explain the large severe visual loss in the studied population.
The demographic data generated in this work can help health entities develop assistance strategies for victims of globe injury, as well as education and prevention actions and improvements in ophthalmological services.
Our study is limited by its retrospective nature and the absence of certain data from the medical records evaluated.
Availability of data and materials
Data were collected by reviewing electronic medical records based on the list of ocular emergency surgeries performed in the Hospital de Base do Distrito Federal from 01/01/2014 to 31/12/2018. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pieramici DJ, Au Eong KG, Sternberg P Jr, Marsh MJ. The prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open-globe injuries. J Trauma. 2003;54(4):750–4. https://doi.org/10.1097/01.TA.0000047053.53821.C8 PMID: 12707539.
Cruvinel Isaac DL, Ghanem VC, Nascimento MA, Torigoe M, Kara-José N. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217(6):431–5. https://doi.org/10.1159/000073075 PMID: 14573978.
Entezari M, Rabei HM, Badalabadi MM, Mohebbi M. Visual outcome and ocular survival in open-globe injuries. Injury. 2006;37(7):633–7. https://doi.org/10.1016/j.injury.2006.02.043 PMID: 16769311.
Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye (Lond). 2006;20(12):1336–41. https://doi.org/10.1038/sj.eye.6702099 Epub 2005 Sep 23. PMID: 16179934.
Rofail M, Lee GA, O'Rourke P. Prognostic indicators for open globe injury. Clin Exp Ophthalmol. 2006;34(8):783–6. https://doi.org/10.1111/j.1442-9071.2006.01309.x PMID: 17073902.
Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham eye trauma terminology system (BETT). J Fr Ophtalmol. 2004;27(2):206–10. https://doi.org/10.1016/s0181-5512(04)96122-0 PMID: 15029055.
Gerstenblith AT, Rabinowitz MP. Manual de Doenças Oculares do Wills Eye Hospital. 6 ed. Porto Alegre: ARTMED; 2015. p. 45–49. ISBN 9788582710418.
Rohr JTD, Santos PM, Santos RCR, et al. Profile of pediatric eye trauma at Hospital de Base do Distrito Federal (HBDF), Brasília, Brazil. Rev Assoc Med Bras. 2016;62(4):324–9 ISSN 1806-9282.
Kuhn F, Dante P. Ocular trauma: principles and practice. Thieme Medical Publishers. 1 ed. New York; 2001. p. 3–20. ISBN-10: 1588900754.
Erikitola OO, Shahid SM, Waqar S, Hewick SA. Ocular trauma: classification, management and prognosis. Br J Hosp Med (Lond). 2013;74(7):C108–11. https://doi.org/10.12968/hmed.2013.74.sup7.c108 PMID: 24145639.
Li EY, Chan TC, Liu AT, Yuen HK. Epidemiology of open-globe injuries in Hong Kong. Asia Pac J Ophthalmol (Phila). 2017;6(1):54–8. https://doi.org/10.1097/APO.0000000000000211 PMID: 28161926.
Pieramici DJ, MacCumber MW, Humayun MU, Marsh MJ, de Juan E Jr. Open-globe injury. Update on types of injuries and visual results. Ophthalmology. 1996;103(11):1798–803. https://doi.org/10.1016/s0161-6420(96)30424-7 PMID: 8942873.
IBGE. Instituto Brasileiro de Geografia e Estatística. v4.3.12.2. 2017.
Brasil. Lei complementar n° 94, de 19 de fevereiro de 1998. Autoriza o Poder Executivo a criar a Região Integrada de Desenvolvimento, Brasília, DF, fev, 1998. Available from: < http://www.planalto.gov.br/ccivil_03/leis/lcp/Lcp94.htm>. Accessed: 12/20/2020.
Brasil. Secretaria de Estado de Saúde do Distrito Federal. Protocolos de Urgência e Emergência da SES/DF. 1a. Ed. P. 199. Revisada e ampliada – Brasília: Secretaria de Estado de Saúde do Distrito Federal; 2006. p. 285. Available from: < http://www.saude.df.gov.br/protocolos-aprovados/>. Accessed: 03/10/2020
Soni NG, Bauza AM, Son JH, Langer PD, Zarbin MA, Bhagat N. Open globe ocular trauma: functional outcome of eyes with no light perception at initial presentation. Retina. 2013;33(2):380–6. https://doi.org/10.1097/IAE.0b013e318263cefb PMID: 23026847.
Brackup AB, Carter KD, Nerad JA, Folk JC, Pulido JS. Long-term follow-up of severely injured eyes following globe rupture. Ophthalmic Plast Reconstr Surg. 1991;7(3):194–7. https://doi.org/10.1097/00002341-199109000-00008 PMID: 1911526.
Vieira GM. Um mês em um pronto-socorro de oftalmologia em Brasília TT - Onemonth in aneyeemergencyclinic in Brasilia. Arq Bras Oftalmol. 2007;70(5):797–802 Available from: <https://doi.org/10.1590/S0004-27492007000500013>. Accessed: 03/10/2020.
Cabral LA, Silva TMN, Britto AEGS. Traumas oculares no serviço de urgência da Fundação Banco de Olhos de Goiás TT - Ocular trauma in the emergency department of Goiás Eye Bank Foundation. Rev Bras Oftalmol. 2013;72(6):383–7 Available from: <https://doi.org/10.1590/S0034-72802013000600006>. Acesso em: 10/03/2019.
Bi H, Cui Y, Li Y, Wang X, Zhang J. Clinical characteristics and surgical problems of ruptured globe injury. Curr Ther Res Clin Exp. 2013;74:16–21. https://doi.org/10.1016/j.curtheres.2012.10.002 PMID: 24385006; PMCID: PMC3862203.
Al Mahmoud T, Al Hadhrami SM, Elhanan M, Alshamsi HN, Abu-Zidan FM. Epidemiology of eye injuries in a high-income developing country: An observational study. Medicine (Baltimore). 2019;98(26):e16083. https://doi.org/10.1097/MD.0000000000016083 PMID: 31261521; PMCID: PMC6617434.
Wang W, Zhou Y, Zeng J, Shi M, Chen B. Epidemiology and clinical characteristics of patients hospitalized for ocular trauma in south-Central China. Acta Ophthalmol. 2017;95(6):e503–10. https://doi.org/10.1111/aos.13438 Epub 2017 Mar 30. PMID: 28371405.
Mir TA, Canner JK, Zafar S, Srikumaran D, Friedman DS, Woreta FA. Characteristics of Open Globe Injuries in the United States From 2006 to 2014. JAMA Ophthalmol. 2020;138(3):268–75. https://doi.org/10.1001/jamaophthalmol.2019.5823 PMID: 31971539; PMCID: PMC6990674.
Court JH, Lu LM, Wang N, McGhee CNJ. Visual and ocular morbidity in severe open-globe injuries presenting to a regional eye Centre in New Zealand. Clin Exp Ophthalmol. 2019;47(4):469–77. https://doi.org/10.1111/ceo.13439 Epub 2018 Dec 3. PMID: 30414237.
Atik SS, Ugurlu S, Egrilmez ED. Open globe injury: demographic and clinical features. J Craniofac Surg. 2018;29(3):628–31. https://doi.org/10.1097/SCS.0000000000004156 PMID: 29381601.
Knyazer B, Bilenko N, Levy J, Lifshitz T, Belfair N, Klemperer I, et al. Open globe eye injury characteristics and prognostic factors in southern Israel: a retrospective epidemiologic review of 10 years experience. Isr Med Assoc J. 2013;15(3):158–62. 23662378.
du Toit N, Mustak H, Cook C. Visual outcomes in patients with open globe injuries compared to predicted outcomes using the Ocular Trauma Scoring system. Int J Ophthalmol. 2015;8(6):1229–33. https://doi.org/10.3980/j.issn.2222-3959.2015.06.28 PMID: 26682179; PMCID: PMC4651895.
Aragaki GN, Inada ET, Teixeira MF, et al. Estudo epidemiológico dos traumas oculares graves em um Hospital Universitário de São José do Rio Preto - SP. Arq Bras Oftalmol. 2003;66(4):473–6. https://doi.org/10.1590/S0004-27492003000400014.
Németh O, Bátor G. A 2014 és 2018 között osztályos ellátást igénylő szemsérülések klasszifikációja a Markusovszky Egyetemi Oktatókórházban [The classification of ocular trauma cases between 2014 and 2018 at the in-patient ophthalmological department of the Markusovszky University Teaching Hospital]. Orv Hetil. 2019;160(49):1941–7. https://doi.org/10.1556/650.2019.31572 PMID: 31786937.
Beshay N, Keay L, Dunn H, Kamalden TA, Hoskin AK, Watson SL. The epidemiology of open globe injuries presenting to a tertiary referral eye hospital in Australia. Injury. 2017;48(7):1348–54. https://doi.org/10.1016/j.injury.2017.04.035 Epub 2017 Apr 18. PMID: 28438416.
Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton MP. Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005;59(1):175–8. https://doi.org/10.1097/01.ta.0000173624.37438.d6 PMID: 16096559.
Makhrash MA, Gosadi IM. Open globe eye injury characteristics and prognostic factors in Jazan, Saudi Arabia. Saudi Med J. 2016;37(12):1328–33. https://doi.org/10.15537/smj.2016.12.15545 PMID: 27874147; PMCID: PMC5303770.
Teixeira SM, Bastos RR, Falcão MS, Falcão-Reis FM, Rocha-Sousa AA. Open-globe injuries at an emergency department in Porto, Portugal: clinical features and prognostic factors. Eur J Ophthalmol. 2014;24(6):932–9. https://doi.org/10.5301/ejo.5000471 Epub 2014 Apr 16. PMID: 24744111.
Ustaoglu M, Karapapak M, Tiryaki S, Dirim AB, Olgun A, Duzgun E, et al. Demographic characteristics and visual outcomes of open globe injuries in a tertiary hospital in Istanbul, Turkey. Eur J Trauma Emerg Surg. 2020;46(3):549–56 PMID: 30523359.
Rao LG, Ninan A, Rao KA. Descriptive study on ocular survival, visual outcome and prognostic factors in open globe injuries. Indian J Ophthalmol. 2010;58(4):321–3. https://doi.org/10.4103/0301-4738.64116 PMID: 20534923; PMCID: PMC2907034.
Ozturk T, Cetin Dora G, Ayhan Z, Kaya M, Arikan G, Yaman A. Etiology and Visual Prognosis in Open Globe Injuries: Results of A Tertiary Referral Center in Turkey. Sci Rep. 2019;9(1):17977. https://doi.org/10.1038/s41598-019-54598-w PMID: 31784641; PMCID: PMC6884622.
Cecchetti DFAl, Cecchetti SAP, Nardy ACT, Carvalho SC, Rodrigues MLV, Rocha EM. Perfil clínico e epidemiológico das urgências oculares em pronto-socorro de referência. Arq Bras Oftalmol. 2008;71(5):635–8. https://doi.org/10.1590/S0004-27492008000500005.
Silber PC, Souza LB, Tongu MTS. Perfil epidemiológico do trauma ocular penetrante antes e após o novo código de trânsito. Arq Bras Oftalmol. 2002;65(4):441–4. https://doi.org/10.1590/S0004-27492002000400009.
Weyll M, Silveira RC, Fonseca Júnior NL. Trauma ocular aberto: características de casos atendidos no complexo Hospitalar Padre Bento de Guarulhos. Arq Bras Oftalmol. 2005;68(4):505–10. https://doi.org/10.1590/S0004-27492005000400015.
Hernández DM, Gómez VL. Comparación del Ocular Trauma Score en traumatismo con globo abierto, atendido temprana o tardíamente [Ocular Trauma Score comparison with open globe receiving early or late care attention]. Cir Cir. 2015;83(1):9–14. https://doi.org/10.1016/j.circir.2015.04.017 PMID: 25982602.
Rodrigues CFS, Lima FJC, Barbosa FT. Importância do uso adequado da estatística básica nas pesquisas clínicas. Rev Bras Anestesiol. 2017;67(6):619–25. https://doi.org/10.1016/j.bjane.2017.01.011.
Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115(1):202–9. https://doi.org/10.1016/j.ophtha.2007.04.008 Epub 2007 Jun 27. PMID: 17588667.
Fujikawa A, Mohamed YH, Kinoshita H, et al. Visual outcomes and prognostic factors in open-globe injuries. BMC Ophthalmol. 2018;18(1):138. https://doi.org/10.1186/s12886-018-0804-4 PMID: 29884145; PMCID: PMC5994054.
Soheilian M, Rafati N, Mohebbi MR, et al. Traumatic Endophthalmitis trial research group. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Arch Ophthalmol. 2007;125(4):460–5. https://doi.org/10.1001/archopht.125.4.460 PMID: 17420365.
Essex RW, Yi Q, Charles PG, Allen PJ. Post-traumatic endophthalmitis. Ophthalmology. 2004;111(11):2015–22. https://doi.org/10.1016/j.ophtha.2003.09.041 PMID: 15522366.
Andreoli CM, Andreoli MT, Kloek CE, Ahuero AE, Vavvas D, Durand ML. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol. 2009;147(4):601–8. https://doi.org/10.1016/j.ajo.2008.10.023 Epub 2009 Feb 1. PMID: 19181306.
Brasil. Norma Regulamentadora 6. Portaria do Ministério do Trabalho no 3.214, de 08 de junho de 1978, modificada pela Portaria no 877 DOU 24/10/2018.
Brasil. Lei 8.080, de 19 de setembro de 1990.
Maneschg OA, Volek E, Lohinai Z, et al. Genauigkeit und Relevanz der CT-Volumetrie bei offenen Bulbusverletzungen mit intraokularen Fremdkörpern [Accuracy and relevance of CT volumetry in open ocular injuries with intraocular foreign bodies]. Ophthalmologe. 2015;112(4):359–63. https://doi.org/10.1007/s00347-014-3230-x PMID: 25698591.
Kanoff JM, Turalba AV, Andreoli MT, Andreoli CM. Characteristics and outcomes of work-related open globe injuries. Am J Ophthalmol. 2010;150(2):265–9. https://doi.org/10.1016/j.ajo.2010.02.015 Epub 2010 Jun 3. PMID: 20522411.
Ahn JY, Ryoo HW, Park JB, et al. Epidemiologic characteristics of work-related eye injuries and risk factors associated with severe eye injuries: a registry-based multicentre study. Ophthalmic Epidemiol. 2020;27(2):105–14. https://doi.org/10.1080/09286586.2019.1683868 Epub 2019 Oct 31. PMID: 31672074.
Acknowledgments
Nature Research Editing Service for the English language review.
The study was performed after receiving approval from the Ethics Committee of the Instituto de Gestão Estratégica de Saúde do Distrito Federal (IGESDF) under number 3.565.112, according to Brazilian Resolution no 466/12 and the Declaration of Helsinki; the committee waived the requirement for an informed consent form for participation/publication.
Funding
None.
Author information
Authors and Affiliations
Contributions
Marina B. Peleja, the main author, performed the preliminary project; obtained the ethics committee authorization; participated in the record review, data tabulation, and statistical analyses; and wrote part of the main manuscript and its translation. Felipe B. S. da Cunha and Mariana B. Peleja collaborated in the record review, data collection, data tabulation, and literature review and wrote part of the main manuscript and its translation. Juliana T. D. Rohr is the advisor for the study and has collaborated on and reviewed all parts of the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics and consent to participate
The Ethics Committee granted approval and waived the need for informed consent.
Consent for publication
Not applicable.
Competing interests
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peleja, M.B., da Cunha, F.B.S., Peleja, M.B. et al. Epidemiology and prognosis factors in open globe injuries in the Federal District of Brazil. BMC Ophthalmol 22, 111 (2022). https://doi.org/10.1186/s12886-021-02183-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-021-02183-z