Abstract
Background
This study aims to examine risk of adverse pregnancy outcomes and mothers’ characteristics in patients with chronic hypertension, gestational hypertension and preeclampsia.
Methods
The study included all births born from women aged 15–45 years, in Lleida, Spain from 2012 to 2018. Pregnancy outcomes were retrieved by regional administrative databases. Logistic regression analysis was used to calculate adjusted odds ratios (OR) (OR 95% CI) for maternal characteristics or neonatal outcomes.
Results
Among 17,177 pregnant women, different types of hypertension present varying risks for both the mother and fetus. There is an increased risk of cesarean section in patients with preeclampsia (OR 2.04, 95% CI: 1.43–2.88). For the newborn, a higher risk of preterm birth is associated with maternal chronic hypertension (OR 3.09, 95% CI: 1.91–4.83) and preeclampsia (OR 5.07, 95% CI: 3.28–7.65). Additionally, there is a higher risk of low birth weight in cases of maternal chronic hypertension (OR 3.2, 95% CI: 2.04–4.88), preeclampsia (OR 5.07, 95% CI: 3.34–7.52), and gestational hypertension (OR 2.72, 95% CI: 1.49–4.68). Furthermore, only newborns of patients with preeclampsia had a higher risk of an Apgar score lower than 7 in the first minute (OR 2.95, 95% CI: 1.45–5.38).
Conclusions
In the study population adjusted for body weight, the different types of hypertension represent different risks in the mother and foetus. These complications were mostly associated with preeclampsia.
Similar content being viewed by others
Introduction
Hypertensive disorders in pregnancy (HDP) are significant contributors to elevated maternal morbidity and mortality rates [1, 2], along with neonatal morbidity [1, 2], as well as neonatal morbidity. HDP refers to gestational hypertension, preeclampsia and eclampsia, chronic hypertension complicated with preeclampsia, and chronic hypertension [3, 4]. According to the International Society for the Study of Hypertension in Pregnancy in 2021, HDP is classified into chronic hypertension, which exists or is diagnosed before 20 weeks’ gestation, and de novo hypertension, which typically occurs from 20 weeks’ gestation onwards. This second one has many manifestations including hypertension alone, known as gestational hypertension; pre-eclampsia (PE), hypertension with proteinuria and maternal organ dysfunction (haematological, liver, renal and neurological) and eclampsia, characterised by seizures [5, 6].
Most guidelines around the world agree on the definition of hypertension in pregnancy, consisting in blood pressure (BP) ≥ 140/90 mmHg. At the same time, there is variability in the threshold for initiating antihypertensive treatment attributable to uncertainty about the maternal benefits of lowering BP and the potential foetal risks from reductions in utero-placental circulation and in utero exposure to drugs [7].
Hypertension in pregnancy is associated with an increased risk of placental abruption, intrauterine growth restriction, preterm birth, renal failure, postpartum haemorrhage, perinatal and maternal death and newborn morbidity [8,9,10]. In this sense, it has been estimated that hypertension during pregnancy is one of the main causes of maternal and foetal morbidity and mortality in the world [11].
Therefore, the aim of this study is to determine the difference in pregnancy outcomes in women with chronic hypertension, gestational hypertension and preeclampsia compared to women with normal pregnancies using populations data.
Materials and methods
Study design and data collection
A retrospective observational cohort study was conducted among pregnant women in the health region of Lleida from 2012 to 2018.
The data of women who had given birth at the Arnau de Vilanova Hospital between January 1st, 2012 and December 31st, 2018 were obtained through the (“Conjunt Minim de Base de Dades”) CMBD database. Data of all the eligible patients assigned to a primary care unit derived from the computerized clinical history database E-CAP of the Catalan Health Institute; and data from Social Security prescriptions obtained from the database of the ServeiCatalà de Salut.
This article is part of the Iler Pregnancy project, a retrospective cohort study conducted in Lleida with the aim of evaluating the prevalence of chronic pathologies in pregnancy (hypothyroidism, depression, diabetes mellitus and obesity) and therapeutic adherence to prescribed drugs [12, 13].
Study population
Women who have had a birth at the Arnau de Vilanova University Hospital in Lleida between January 1st, 2012, and December 31st, 2018, were included in the study. Women who did not belong to Lleida health region were excluded. To evaluate the representativeness of the sample, we calculated the percentage of pregnant women studied compared to the total of pregnant women in the health region of Lleida. Data was obtained from the database of “Instituto Statistics of Catalonia” (Idescat) (Table 1).
Variables recorded
The following variables were recorded: region of origin (Sub Saharan Africa, Latin America, Asia and the Middle East, West Europe, Eastern Europe, and Maghreb) [12]; body mass index (BMI) which is classified according to low weigh (BMI under 18.5 Kg/m2), overweigh (BMI between 25 and 29.9) and obesity (BMI more than 30); number of pregnancy and twin pregnancy; risk during pregnancy; diabetes and mellitus (code O24.9 at CIE-10.); arterial hypertension (code I10-I16 at l’ICD-10); dyslipidemia (code E78 at l’ICD-10); depression (codes F32.0-F32.9, F33.0-F33.3, F33.8, F33.9, F34.1, or F41.2 at l’ICD-10). Other variables taken into account were risk of the pregnancy; duration of the pregnancy (miscarriage, preterm, term, prolonged); caesarean section; birth weight (< 2500 g = underweight, between 2500 g and 3999 g = normal weight, and ≥ 4000 g = macrosomia), 1-minute and 5-minute Apgar score; and preeclampsia.
Data analysis
We performed a descriptive analysis. Based on delivery status, the cohort was divided into four groups: (1) without HDP, (2) chronic hypertension, (3) gestational hypertension, and (4) preeclampsia. Maternal and neonatal characteristics were compared between groups. Continuous variables were expressed as mean and SD and analyzed using ANOVA with post hoc Scheffé test. Ordinal variables were expressed as median and IQR and analyzed using Kruskal–Wallis H test. Categorical variables were expressed as percentages and analyzed using χ² or Fisher’s exact test. Relative risks of HDP phenotypes and outcomes were estimated using multinomial logistic regression. The model-building process was conducted in two blocks: the first included HDP, and the second included covariates (maternal age, BMI, hypothyroidism, maternal diabetes). Adjusted relative risks were expressed as odds ratios (OR) with 95% confidence intervals (95% CI). The “No hypertension” group served as the reference. Superimposed hypertension was excluded from the analysis.
Ethical aspects
This study was approved by the ethics and clinical research committee at the Institut d’Investigació IDIAP Jordi Gol under the code 19/195-P and carried out in accordance with the principles of the Declaration of Helsinki. Information was obtained from electronic medical records stored in the centralized ECAP database and extracted by the Department of Healthcare Evaluation and Research Management. Therefore, it was not necessary to ask participants to sign an informed consent. The variables in the ECAP database were processed anonymously and with full confidentiality guarantees as established by national Spanish law and Regulation 2016/679 of the European Parliament and of the Council on the protection of natural people regarding the processing of personal data, and to the free movement of such data. Ethics committee of (Idiap Jordi Gol i Gurina) waived the need for informed consent due to retrospective observational cohort study.
Results
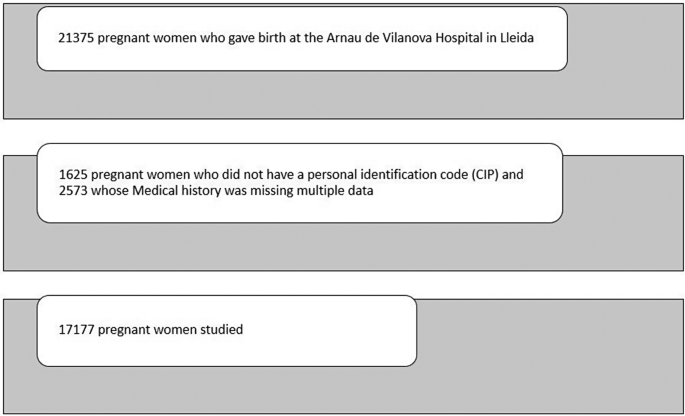
The study was started with a sample of 21,375 women who had given birth at the Arnau de Vilanova Hospital in Lleida between 2012 and 2018 (both included). From this sample, 1625 patients were excluded because they did not have a personal identification code (CIP), and 2573 because multiple data from the clinical history was missing. The final study sample included 17,177 patients (Fig. 1).
Characteristics of the study population
Among the total sample, 533 (3.10%) women had a diagnosis of high blood pressure. 263 (1.53%) pregnant women were diagnosed of chronic hypertension, 111 (0.65%) pregnant women were diagnosed with gestational hypertension and 134 (0.78%) were diagnosed with preeclampsia. Preeclampsia superimposed on chronic hypertension occurred in 25 cases (0.14%).
It was observed that in pregnant women with chronic arterial hypertension (263), the mean age was 33.9 (± 6.00) years, compared to 30.6 (± 5.85) years in the non-hypertensive population. Regarding BMI, 38.4% of patients with chronic hypertension were obese, 44.1% of patients with gestational hypertension, and 26.6% in case of preeclampsia. However, only 14% of non-hypertensive women were obese. Among maternal complications, the percentage of caesarean sections was 28.5% in the case of chronic hypertension, 30.8% in preeclampsia, 23.4% in gestational hypertension compared to 17% in non-hypertensive women. Among the newborn complications, 7.6% in the case of mothers with preeclampsia had an Apgar score lower than 7 in the first minute compared to 2.4% in the case of mothers without hypertension. Respect preterm birth, 18.3% were preterm in the case of chronic hypertension, 24.4% in preeclampsia, 10.7% in gestational hypertension and 5.5% in the case of absence of maternal hypertension. Low birth weight occurred in 17.6% in cases of chronic hypertension, 14.8% in gestational hypertension, 22.9% in preeclampsia and in 5.6% newborns of mothers without hypertension during pregnancy. In the case of chronic hypertension, it was classified as high or very high risk of pregnancy to a greater extent, affecting 31% and 16.3% respectively (Table 2).
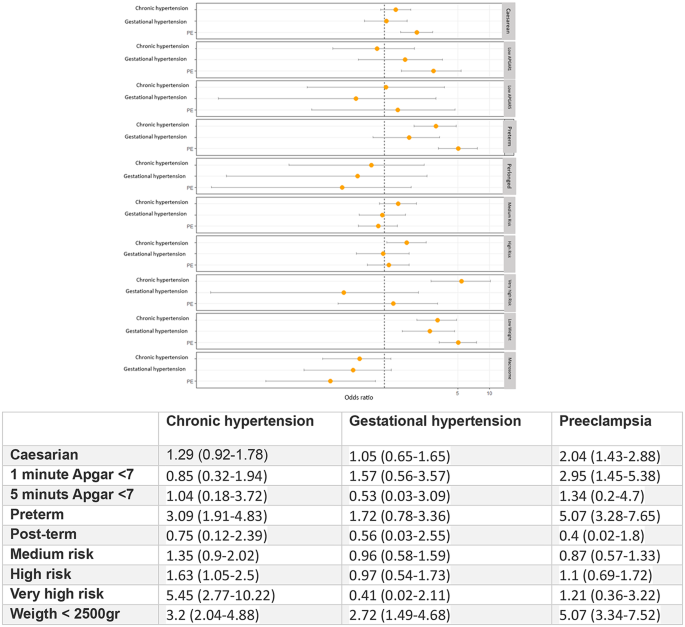
In the multivariate analysis of the different phenotypes of hypertension during pregnancy adjusted for the covariates (maternal age, BMI, hypothyroidism, maternal diabetes) showed statistically significant associations in the risk of cesarean section in patients with preeclampsia (OR 2.04 95% CI: 1.43–2.88). For the newborn, higher risk of preterm birth was associated with maternal chronic hypertension (OR 3.09, 95% CI: 1.91–4.83) or preeclampsia (OR 5.07, 95% CI: 3.28–7.65) and higher risk of low birth weight in case of maternal chronic hypertension (OR 3.2, 95% CI: 2.04–4.88), preeclampsia (OR 5.07, 95% CI: 3.34–7.52) and in the case of gestational hypertension (OR 2.72, 95% CI: 1.49–4.68). On the other hand, only newborns of patients with preeclampsia had higher risk of having an Apgar score lower than 7 in the first minute (OR 2.95, 95% CI: 1.45–5.38). Patients classified as high or very high risk were primarily those who presented chronic hypertension (OR 5.45, 95% CI: 2.77–10.22) and followed by preeclampsia (OR 1.21, 95% CI: 0.36–3.22) (Fig. 2).
Discussion
This study, including 17,177 pregnant women, provides valuable information on the risk factors, prevalence and outcomes of a range of HDP adjusted for body weight, which demonstrates that the different subtypes of hypertension represent different risks to the mother and the foetus. There is an increased risk of caesarean section in patients with preeclampsia (OR 2.04 95% CI: 1.43–2.88). For the newborn, higher risk of preterm birth was associated with maternal chronic hypertension (OR 3.09, 95% CI: 1.91–4.83) or preeclampsia (OR 5.07, 95% CI: 3.28–7.65) and higher risk of low birth weight in case of maternal chronic hypertension (OR 3.2, 95% CI: 2.04–4.88), preeclampsia (OR 5.07, 95% CI: 3.34–7.52) and in the case of gestational hypertension (OR 2.72, 95% CI: 1.49–4.68). On the other hand, only newborns of patients with preeclampsia had higher risk of having an Apgar score lower than 7 in the first minute (OR 2.95, 95% CI: 1.45–5.38). Patients categorized as high or very high risk predominantly include those with chronic hypertension (OR 5.45, 95% CI: 2.77–10.22), followed by those with preeclampsia (OR 1.21, 95% CI: 0.36–3.22).
Analysing risk factors individually, gestational age was significantly higher in patients with chronic hypertension with a median of 33.9 (± 6.19) years of age; being 3 years older in comparison to preeclampsia and non-hypertensive women. BMI average for hypertensive women was 28.8 (± 6.28) and 25.9 (± 5.75) in women with preeclampsia. For the rest of the pregnant women, BMI was 24.8 (± 4.85). In a retrospective cohort study carried out in Southern Spain [14], it was concluded that overweight and obesity increase the risk of suffering from hypertensive disorders during pregnancy; the risk is significantly higher as BMI increases. In multiple population studies it was identified that obesity increases 2 to 4 times the risk of developing preeclampsia [15, 16].
Relationship of chronic hypertension (OR 3.09) and preeclampsia (OR 5.07) with a risk of preterm birth in our study has been observed, as described in other publications. According to Sibai et al., the rates of preterm delivery in a large population of women with chronic hypertension while comparing them with those in a healthy control woman, the overall rates of preterm delivery were significantly higher among women with diabetes mellitus (38%) and hypertension (33.1%) than among control women (13.9%) [17]. An et al., in a prospective cohort study done in China, after adjusting for potential confounders, observed higher levels of preterm birth in women with gestational hypertension 1.04 (95% CI 0.98 to 1.11) and pre-eclampsia 1.39 (95% CI 1.25 to 1.55), respect control women [18]. Other medical publications also showed an increased risk of preterm birth in a population with hypertension during pregnancy [19, 20].
Delivery methods studies demonstrate higher rate of caesarean section in all women with hypertension: 28.5% in chronic hypertension, 23.4% in gestational hypertension and 30.8% in preeclampsia; compared to 17% in women without hypertension in pregnancy. A systematic review and meta-analysis of hypertension and pregnancy outcomes showed a combined incidence of cesarean section of 41.4% (35.5-47.7%) higher than the rate observed in our study [21]. Moreover, high incidence of adverse outcomes, were described. Therefore, patient-level analysis should be conducted to assess the reasons for cesarean section to provide and guarantee clear indication in each instance.
Study results are comparable to another study from a maternity hospital in Brazil [22] that reveals the existence of statistically significant differences between the proportion of c-sections, preterm infants and low birth weight infants for pregnant women with and without hypertensive disorders.
All types of hypertensive disorders were associated with low birth weight. The rate observed for patients with chronic hypertension was 17.6%, 22.9% in patients with preeclampsia, 14.8% in patients with gestational hypertension and 5.6% in women not diagnosed with hypertension.
The study conducted by Fang et al. describes similar results comparing women with and without chronic hypertension; reporting rates of low birth weight among hypertensive mothers for white (16.8%), black (24.4%), and Hispanic (19.5%) populations respectively. Trends were similar for chronic and pregnancy-related hypertension, as well as preeclampsia/eclampsia [23]. The study completed by Wu et al. evaluates the relationship of stage 1 hypertension detected early in gestation (< 20 weeks) and risks of adverse pregnancy outcomes, stratified by pre-pregnancy BMI. Data indicates that women classified at stage 1a (systolic blood pressure 130–134 mm Hg; diastolic BP, 80–84 mm Hg; or both) and stage 1b hypertension (systolic BP, 135–139 mm Hg; diastolic BP, 85–90 mm Hg; or both) show slightly higher but significant rates and risks of gestational diabetes mellitus, preterm birth, and low birth weight (< 2500 g) in both groups compared with normotensive controls [24].
Results of this study show that only newborns of patients with preeclampsia had a higher risk of having an Apgar score lower than 7 in the first minute (OR 3.3). However, this was not observed in other hypertensive disorders, where Apgar score was normalizing at 5 min. In a large Chinese population study both maternal hypertension and preeclampsia increased risks for low Apgar score at 1 min (aRR: 1.20, 95%CI: 1.13–1.27; aRR: 1.53, 95%CI: 1.41–1.67, respectively), and for low Apgar score at 5 min (aRR: 1.30, 95%CI: 1.17–1.45; aRR: 1.70, 95%CI: 1.46–1.99, respectively). The risk for neonatal respiratory disorders increased with severity of maternal hypertension [25]. Moreover, Gu et al. proved that higher diastolic blood pressure was associated with an increased risk of 1-minute Apgar score ≤ 7 when extreme quartiles were compared. However, no significant association was found between systolic blood pressure and 1-minutes or 5-minutes Apgar score ≤ 7, which implies that diastolic blood pressure, has a better prognostic value [26].
Bronfield et al. [27]. found in a retrospective study in 14 US states worse outcomes for both mothers and babies in mothers with preeclampsia or superimposed preeclampsia compared to the non-hypertensive population, the population with chronic hypertension also had a higher risk of childbirth premature birth, respiratory distress, low birth weight compared to women without hypertension, but the risk was lower than that of mothers with preeclampsia and, as a last group, women with gestational hypertension had a somewhat higher risk of complications compared to non-hypertensive women but more similar to the healthy population. These data are similar to those reported in our study.
Limitations
The main limitation of this study if the fact of using a retrospective design based on administrative data, thus reducing important information on both maternal and neonatal outcomes. The effect of different antihypertensive treatments on maternal and perinatal outcomes have not been evaluated.
Adequate blood pressure control can modify these adverse outcomes. Minas et cols. [28] Show that more uncontrollable blood pression patients had superimposed preeclampsia with severe features (54.6% vs. 25.0%; p = 0.01) and preterm delivery (40.9% vs. 10.7%; p = 0.002) than controlled blood pressure patients. The results of CHAP trial [29] and the meta-analysis carried out by Atta et al. [30] suggest the beneficence of pharmacologic treatment of mild chronic hypertension during pregnancy to a blood pressure goal below140/90 mm Hg, which is also supported by the Society for Maternal-Fetal Medicine (SMFM) [31]. Conversely, in our study, we did not analyze the potential complications of eclampsia or HELLP syndrome in a detailed manner, as these conditions are encompassed within the diagnoses of preeclampsia. Furthermore, superimposed preeclampsia was excluded because it involves patients from two distinct groups. Some instances of gestational hypertension may correspond to previously undetected chronic hypertension due to the presence of masked hypertension. This condition has been associated with an increased risk of developing preeclàmpsia [32].
Finally, another limitation to be considered is the lack of socioeconomic data on the population, which may also influence several factors and health outcomes.
Future research
All types of hypertension have been found to be related to adverse events on pregnancy. This study supports the need to further investigate the pathophysiological knowledge of hypertension in pregnancies to improve the preventive and therapeutic approaches.
Conclusions
Hypertension in pregnancy is associated with higher incidence of adverse pregnancy outcomes. The different types of hypertension represent different risks in the mother and foetus. These complications were mostly associated with preeclampsia. This finding should be interpreted within the limitations of the study.
The use of sensitive diagnostic criteria facilitates solid foundation in epidemiological study, general practise, and clinical research. To address hypertension, Public Health interventions are necessary in addition to clinical management that act at different levels to improve lifestyle habits and early diagnosis before and during pregnancy.
Data availability
The data used in this study are only available for the participating researchers, in accordance with current European and national laws. Thus, the distribution of the data is not allowed. However, researchers from public institutions can request data from SIDIAP.
References
1, Boulet SL, Platner M, Joseph NT, Campbell A, Williams R, Stanhope KK, Jamieson DJ. Hypertensive Disorders of Pregnancy, Cesarean Delivery, and Severe Maternal Morbidity in an Urban Safety-Net Population. Am J Epidemiol. 2020;189(12):1502–1511. https://doi.org/10.1093/aje/kwaa135. PMID: 32639535.
Wu P, Chew-Graham CA, Maas AH, Chappell LC, Potts JE, Gulati M, Jordan KP, Mamas MA. Temporal Changes in Hypertensive Disorders of Pregnancy and Impact on Cardiovascular and Obstetric Outcomes. Am J Cardiol. 2020;125(10):1508–1516. doi: 10.1016/j.amjcard.2020.02.029. Epub 2020 Mar 5. PMID: 32273052.
Li F, Qin J, Zhang S, Chen L. Prevalence of hypertensive disorders in pregnancy in China: a systematic review and meta-analysis. Pregnancy Hypertens. 2021;24:13–21. https://doi.org/10.1016/j.preghy.2021.02.001. Epub 2021 Feb 14. PMID: 33626437.
ACOG Practice Bulletin No. 202: Gestational Hypertension and Preeclampsia. Obstet Gynecol. 2019;133(1):1. https://doi.org/10.1097/AOG.0000000000003018. PMID: 30575675.
Magee LA, Brown MA, Hall DR, Gupte S, Hennessy A, Karumanchi SA, Kenny LC, McCarthy F, Myers J, Poon LC, Rana S, Saito S, Staff AC, Tsigas E, von Dadelszen P. The 2021 International Society for the Study of Hypertension in Pregnancy classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2022;27:148–69. Epub 2021 Oct 9. PMID: 35066406.
Corrigan L, O’Farrell A, Moran P, Daly D. Hypertension in pregnancy: prevalence, risk factors and outcomes for women birthing in Ireland. Pregnancy Hypertens. 2021;24:1–6. https://doi.org/10.1016/j.preghy.2021.02.005. Epub 2021 Feb 14. PMID: 33618054.
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics. ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019;133(1):e26-e50. https://doi.org/10.1097/AOG.0000000000003020. PMID: 30575676.
Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020;135(6):e237-e260. https://doi.org/10.1097/AOG.0000000000003891. PMID: 32443079.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R, Pre-eclampsia. Lancet. 2010;376(9741):631–44. https://doi.org/10.1016/S0140-6736(10)60279-6. Epub 2010 Jul 2. PMID: 20598363.
Cruz MO, Gao W, Hibbard JU. Obstetrical and perinatal outcomes among women with gestational hypertension, mild preeclampsia, and mild chronic hypertension. Am J Obstet Gynecol. 2011;205(3):260. .e1-260.e9.
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, Gülmezoglu AM, Temmerman M, Alkema L. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2(6):e323–33. https://doi.org/10.1016/S2214-109X(14)70227-X. Epub 2014 May 5. PMID: 25103301.
12, Orós M, Siscart J, Perejón D, Serna MC, Godoy P, Salinas-Roca B. Ethnic disparities and obesity risk factors in pregnant women: a Retrospective Observational Cohort Study. Nutrients. 2023;15(4):926. https://doi.org/10.3390/nu15040926. PMID: 36839284; PMCID: PMC9961767.
Siscart J, Orós M, Serna MC, Perejón D, Galván L, Ortega M. Adherence to treatment for hypothyroidism in pregnancy and relationship with thyrotropin control: a retrospective observational cohort study. BMC Pregnancy Childbirth. 2022;22(1):168. https://doi.org/10.1186/s12884-022-04483-8. PMID: 35232385; PMCID: PMC8886742.
Fernández Alba JJ, Mesa Páez C, Vilar Sánchez Á, Soto Pazos E, González Macías M, del Serrano Negro C. Overweight and obesity at risk factors for hypertensive states of pregnancy: a retrospective cohort study. Nutr Hosp. 2018;35(4):874–80.
Spradley FT, Palei AC, Granger JP. Increased risk for the development of preeclampsia in obese pregnancies: weighing in on the mechanisms. Am J Physiol Regul Integr Comp Physiol. 2015;309(11):R1326–43. https://doi.org/10.1152/ajpregu.00178.2015. Epub 2015 Oct 7. PMID: 26447211; PMCID: PMC4698403.
Robillard PY, et al. Increased BMI has a linear association with late-onset preeclampsia: a population-based study. PLoS ONE. 2019;14:e0223888.
Sibai BM, Caritis SN, Hauth JC, MacPherson C, VanDorsten JP, Klebanoff M, Landon M, Paul RH, Meis PJ, Miodovnik M, Dombrowski MP, Thurnau GR, Moawad AH, Roberts J. Preterm delivery in women with pregestational diabetes mellitus or chronic hypertension relative to women with uncomplicated pregnancies. The National institute of Child health and Human Development Maternal- Fetal Medicine Units Network. Am J Obstet Gynecol. 2000;183(6):1520-4. https://doi.org/10.1067/mob.2000.107621. PMID: 11120521.
An H, Jin M, Li Z, Zhang L, Li H, Zhang Y, Ye R, Li N. Impact of gestational hypertension and pre-eclampsia on preterm birth in China: a large prospective cohort study. BMJ Open. 2022;12(9):e058068. https://doi.org/10.1136/bmjopen-2021-058068. PMID: 36167382; PMCID: PMC9516080.
Berhe AK, Ilesanmi AO, Aimakhu CO, et al. Effect of pregnancy induced hypertension on adverse perinatal outcomes in Tigray regional state, Ethiopia: a prospective cohort study. BMC Pregnancy Childbirth. 2019;20:7.
Mulualem G, Wondim A, Woretaw A. The effect of pregnancy induced hypertension and multiple pregnancies on preterm birth in Ethiopia: a systematic review and meta-analysis. BMC Res Notes. 2019;12:91.
Bramham K, Parnell B, Nelson-Piercy C, Seed PT, Poston L, Chappell LC. Chronic hypertension and pregnancy outcomes: systematic review and meta-analysis. BMJ. 2014;348:g2301. https://doi.org/10.1136/bmj.g2301. PMID: 24735917; PMCID: PMC3988319.
Ramos Filho FL, Antunes CMF. Hypertensive Disorders: Prevalence, Perinatal Outcomes and Cesarean Section Rates in Pregnant Women Hospitalized for Delivery. Rev Bras Ginecol Obstet. 2020;42(11):690–696. doi: 10.1055/s-0040-1714134. Epub 2020 Nov 30. PMID: 33254262; PMCID: PMC10309246.
23, Fang J, Madhavan S, Alderman MH. The influence of maternal hypertension on low birth weight: differences among ethnic populations. Ethn Dis. 1999 Autumn;9(3):369 – 76. PMID: 10600059.
Wu DD, Gao L, Huang O, Ullah K, Guo MX, Liu Y, Zhang J, Chen L, Fan JX, Sheng JZ, Lin XH, Huang HF. Increased Adverse Pregnancy Outcomes Associated With Stage 1 Hypertension in a Low-Risk Cohort: Evidence From 47 874 Cases. Hypertension. 2020;75(3):772–780. doi: 10.1161/HYPERTENSIONAHA.119.14252. Epub 2020 Feb 3. PMID: 32008433.
25, Tian T, Wang L, Ye R, Liu J, Ren A. Maternal hypertension, preeclampsia, and risk of neonatal respiratory disorders in a large-prospective cohort study. Pregnancy Hypertens. 2020;19:131–7. https://doi.org/10.1016/j.preghy.2020.01.006. Epub 2020 Jan 14. PMID: 31982835.
Gu Y, Shi H, Zeng W, Zheng Y, Yang M, Sun M, Shi H, Gu W. Association between gestational visit-to-visit blood pressure variability and adverse neonatal outcomes. J Clin Hypertens (Greenwich). 2022;24(6):779–88. https://doi.org/10.1111/jch.14500. Epub 2022 May 14. PMID: 35567772; PMCID: PMC9180330.
Bromfield SG, Ma Q, DeVries A, Inglis T, Gordon AS. The association between hypertensive disorders during pregnancy and maternal and neonatal outcomes: a retrospective claims analysis. BMC Pregnancy Childbirth. 2023;23(1):514. https://doi.org/10.1186/s12884-023-05818-9. PMID: 37452285; PMCID: PMC10347833.
Minhas R, Young D, Naseem R, Mueller A, Chinthala S, Perdigao JL, Yeo KJ, Chan SL, Tung A, White JB, Shahul S, Rana S. Association of antepartum blood pressure levels and angiogenic profile among women with chronic hypertension. Pregnancy Hypertens. 2018;14:110–114. doi: 10.1016/j.preghy.2018.09.003. Epub 2018 Sep 5. PMID: 30527096.
Tita AT, Szychowski JM, Boggess K, Dugoff L, Sibai B, Lawrence K, Hughes BL, Bell J, Aagaard K, Edwards RK, Gibson K, Haas DM, Plante L, Metz T, Casey B, Esplin S, Longo S, Hoffman M, Saade GR, Hoppe KK, Foroutan J, Tuuli M, Owens MY, Simhan HN, Frey H, Rosen T, Palatnik A, Baker S, August P, Reddy UM, Kinzler W, Su E, Krishna I, Nguyen N, Norton ME, Skupski D, El-Sayed YY, Ogunyemi D, Galis ZS, Harper L, Ambalavanan N, Geller NL, Oparil S, Cutter GR, Andrews WW. Chronic hypertension and pregnancy (CHAP) Trial Consortium. Treatment for mild chronic hypertension during pregnancy. N Engl J Med. 2022;386(19):1781–92. https://doi.org/10.1056/NEJMoa2201295. Epub 2022 Apr 2. PMID: 35363951; PMCID: PMC9575330.
Attar A, Hosseinpour A, Moghadami M. The impact of antihypertensive treatment of mild to moderate hypertension during pregnancy on maternal and neonatal outcomes: An updated meta-analysis of randomized controlled trials. Clin Cardiol. 2023;46(5):467–476. doi: 10.1002/clc.24013. Epub 2023 Mar 28. PMID: 369873Society for Maternal-Fetal Medicine. Society for Maternal‐Fetal Medicine statement: antihypertensive therapy for mild chronic hypertension in pregnancy—the chronic hypertension and preg-nancy trial. Am J Obstet Gynecol. 2022;227(2):B24‐B2790; PMCID: PMC10189071.
Society for Maternal-Fetal Medicine. Publications Committee. Electronic address: pubs@smfm.org. Society for maternal-fetal Medicine Statement: antihypertensive therapy for mild chronic hypertension in pregnancy-the chronic hypertension and pregnancy trial. Am J Obstet Gynecol. 2022;227(2):B24–7. https://doi.org/10.1016/j.ajog.2022.04.011. Epub 2022 Apr 19. PMID: 35710594.
Espeche WG, Salazar MR, Minetto J, Leiva Sisnieguez CE, Cerri G, Balbín E, Stavile RN, Carrera Ramos P, Soria A, Santillan C, Grassi F, Torres S, Carbajal HA. Hypertension arising after 20 weeks of gestation: gestational hypertension or masked chronic hypertension? J Hum Hypertens. 2023;37(9):813–7. https://doi.org/10.1038/s41371-022-00767-w. Epub 2022 Oct 12. PMID: 36224324.
Acknowledgements
The authors would like to acknowledge Dr. Miquel Butí for his valuable contribution and support to design and build the database. Joaquim Sol for his contribution to the statistics analysis, and Gol i Gurina Foundation.
Funding
The authors declare no contribution from any organization for the submitted work; no financial relationships with organizations that might have an interest in the submitted work for the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Contributions
AB and DP conceptualized the study, analysed the data, and wrote the first draft of the manuscript; MCS, JS, IG contributed to the design of the study, data management, and manuscript development and review; MO also contributed to the design of the study, and to the creation of data bases and data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the ethics and clinical research committee at the Institut d’Investigació IDIAP Jordi Gol under the code 19/195-P and conducted in accordance with the principles of the Declaration of Helsinki. Information was obtained from electronic medical records stored in the centralized ECAP (computerized clinical history) database and extracted by the Department of Healthcare Evaluation and Research Management. Accordingly, it was not necessary to ask participants for their informed consent. The variables in the ECAP database were processed anonymously and with full confidentiality guarantees as established by Spanish national law and Regulation 2016/679 of the European Parliament and the Council on the protection of natural persons with regard to the processing of personal data, and to the free distribution of such data. The data used in this study are only available for the participating researchers, in accordance with current European and national laws. Thus, the distribution of the data is not allowed. However, researchers from public institutions can request data from SIDIAP. Ethics committee of (Idiap Jordi Gol i Gurina) waived the need for informed consent due to retrospective observational cohort study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Perejón, D., Bardalet, A., Gascó, I. et al. Hypertension subtypes and adverse maternal and perinatal outcomes - a retrospective population-based cohort study. BMC Pregnancy Childbirth 24, 568 (2024). https://doi.org/10.1186/s12884-024-06754-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06754-y