Abstract
Background
Cryptococcosis is progressively acknowledged among people, irrespective of the human with or without immunodeficiency virus (HIV). This change in epidemiology has been recorded in recent years, prompting closer examination and a broader understanding of the disease manifestations and risk factors.
Methods
The data of cryptococcal infections in China during 11 years were retrospectively analyzed. According to the position of infection, the patients were categorized into the pulmonary infection group and extrapulmonary infection group. The composition of the two groups was compared, and the potential risk factors of disseminated infection were analyzed. Logistic regression was used to analyze the prognostic risk factors of the disease.
Results
A total of 165 patients were enrolled. 113 (68.5%) were male, and the age was 47.49 (18–82) years. 101 cases (61.2%) had a normal immune function and 64 cases (38.8%) had impaired immune function. 45 patients had extrapulmonary infection, involving the central nervous system, bone and joint, skin and bloodstream, and 120 patients had simple pulmonary infection. The mortality of the extrapulmonary infection group (48.9%) was significantly higher than that of the pulmonary infection group (0.8%). According to univariate logistic regression analysis, immune status (hazard ratio [HR], 4.476; 95% confidence interval [CI], 1.725–11.618; P = 0.002), infection position ([HR], 113.826; [CI], 14.607-886.967; P < 0.001), white blood cell count, ([HR],1.209;[CI], 1.054–1.386; P = 0.007), hemoglobin ([HR], 0.970; [CI], 0.955–0.986; P < 0.001), platelet count ([HR], 0.993; [CI], 0.987–0.999; P = 0.026), neutrophil percentage ([HR], 1.115; [CI], 1.065–1.168; P < 0.001), lymphocyte percentage ([HR], 0.875; [CI], 0.827–0.927; P < 0.001), neutrophil-to-lymphocyte Ratio (NLR) ([HR], 1.144; [CI], 1.072–1.221; P < 0.001), monocyte percentage ([HR], 0.752; [CI], 0.618–0.915; P = 0.004) were related to the prognosis. Multivariate logistic regression analysis showed that the infection position was remained related to the prognosis with statistical significance ([HR], 0.018; [CI], 0.001–0.384; P = 0.001).
Conclusion
Extrapulmonary infection of Cryptococcosis is an important risk factor for prognosis. High levels of neutrophils and NLR, and low levels of lymphocytes and monocytes may lead to disseminated infection of Cryptococcosis. Further studies are needed to reduce the occurrence rate of extrapulmonary infection and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cryptococcus is an opportunistic pathogenic yeast that is prevalent in the environment, thriving in pigeon guano, some plants (e.g. eucalyptus trees) and soil [1]. Normally, Cryptococcus in the environment invade the lungs through the respiratory tract, which is often confined to the lungs or resolved by the human innate immune system. However, Cryptococcus may cause life-threatening illnesses in immunocompromised individuals, such as cryptococcal meningitis (CM), either from reactivation of a previously acquired latent infection or novel exposure [2,3,4].
The mortality rate among patients with extrapulmonary cryptococcosis is extremely high, particularly in the case of CM, where the mortality rate can reach as high as 60–80% within 6 months after diagnosis [5]. Although, in recent years, it has not only been in those with HIV and natural or iatrogenic immunosuppression but also in apparently immunocompetent individuals [6,7,8,9]. In a previous study, it was reported that 67% of instances of pulmonary cryptococcosis among immunocompetent patients progressed to disseminate into the central nervous system, leading to CM, not to mention immunocompromised patients [10].
To further improve our comprehension of the manifestations and consequences of cryptococcosis diagnosed in Chinese people with or without HIV infection, we performed a retrospective study. The aim of this study is to compare the clinical characteristics and treatment strategies between pulmonary and extrapulmonary infection of Cryptococcus, explore the potential risk factors for the development of pulmonary cryptococcosis to CM, identify the prognostic factors of cryptococcosis, and provide new ideas for preventing extrapulmonary infection and improving the prognosis of patients.
Materials and methods
Research objects
One hundred and sixty-five patients diagnosed with cryptococcosis in the First Affiliated Hospital with Nanjing Medical University from January 2010 to December 2021 were included in the study, including 113 males and 52 females. Inclusion criteria: cryptococcal disease had to be “proven” by radiographic anomalies consistent with the disease, coupled with confirmed culture positivity from sterile fluid or biopsy confirmation. Alternatively, a diagnosis of “probable” cryptococcosis was assigned in cases exhibiting antigen positivity in blood or cerebrospinal fluid (CSF). Instances where microbial retrieval from sputum or bronchoalveolar lavage lacked concordance with clinical and/or radiographic evidence were categorized as “possible” pulmonary disease. Diseases involving the central nervous system (CNS) with evidence of Cryptococcus in histological examination, antigen detection, or culture of brain tissue or CSF were also included [11, 12]. The exclusion criteria: patients under the age of 18.
The study conformed to the ethical guidelines of the Declaration of Helsinki and was approved by The Ethics Committee of The First Affiliated Hospital with Nanjing Medical University. Because it was a retrospective nature of the study with anonymized clinical data, the informed consent was waived.
Research methods
A retrospective analysis of the clinical data of 165 patients, including gender, age, immune status, comorbidities, clinical symptoms; laboratory indicators: blood routine examination, serum procalcitonin (PCT), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), fasting plasma glucose; antifungal regimens; treatment efficacy, etc. Outcomes: all-cause case fatality at 30 days after the diagnosis.
Statistical methods
All data statistics used are carried out by SPSS 26.0 software. Count data were expressed as n (%) and χ2 test or Fisher’s exact probability test was used. Normally, distributed measurement data were expressed as x ± s and analyzed with independent samples t-test. Non-normally distributed measurement data were expressed as median (M) and interquartile range (Q1–Q3) indicates that the non-parametric test was used. Logistic regression analysis was used for multivariate analysis. P < 0.05 was considered statistically significant.
Results
General information
According to the inclusion and exclusion criteria, a total of 165 adult cases of cryptococcosis were screened, as shown in Fig. 1. Subject demographic characteristics, exposures, and immunosuppressive conditions are summarized in Table 1. Among 165 patients, 113 (68.5%) were male, the age was 47.49 (18–82) years, and 58 (35.2%) patients had a history of smoking. Normal immune function was observed in 101 cases (61.2%), whereas 64 cases (38.8%) exhibited impaired immune function. The majority of patients with abnormal immune status had conditions such as diabetes mellitus, autoimmune diseases, and glucocorticoid therapy.
Characteristics at admission
Of the 165 patients, 45 individuals were afflicted with extrapulmonary infection, which affected their central nervous system, bones and joints, skin, or bloodstream. Meanwhile, the remaining 120 patients suffered from a more straightforward pulmonary infection.
Upon analyzing the composition of the pulmonary infection group and the extrapulmonary infection group, it was observed that the proportion of patients with abnormal immune function in the extrapulmonary infection group was higher, and the clinical manifestations of the two groups were significantly different. The main manifestations of the pulmonary infection group were cough (57.5%), expectoration (38.4%), and chest pain (16.8%). In contrast, the extrapulmonary infection group primarily exhibited symptoms such as headache (80.0%), fever (68.9%), nervous system symptoms (57.8%), and vomiting (42.2%). Furthermore, in the laboratory examination, the percentage of neutrophils (82.5%) and NLR (6.7131) in the extrapulmonary infection group were higher, hemoglobin (115 g/L), platelet count (179.04 × 109/L) and lymphocyte percentage (14.17%) were lower. Additionally, an increase in PCT, CRP and fasting blood glucose was more common. (Table 2).
Treatment
The lung infection mainly accepts azole monotherapy, while extrapulmonary infection only 19 cases (42.2%) use azole monotherapy. Out of the remaining 26 patients with extrapulmonary infections, 19 patients were subjected to treatment using amphotericin B alone or in conjunction with azoles or in combination with 5-FC. 2 patients were subjected to triple therapy. 4 patients were left untreated as a consequence of either discontinuing their treatment prematurely or the rapid progression of their disease. In addition to antifungal treatment, adjunctive treatment was also provided (Table 3). 11 patients with pulmonary infection underwent lung resection and resection of lesions. In cases of extrapulmonary infection, especially for patients with cryptococcal meningitis, 15 patients were administered high-dose corticosteroids to control inflammation, and 13 patients received serial LP to manage high-pressure and relieve symptoms such as headaches. The mortality of extrapulmonary infection group (48.9%) was significantly higher than that of pulmonary infection group (0.8%).
Prognostic analysis
According to univariate Logistic regression analysis, several factors were found to be related to the prognosis of cryptococcosis, including immune status (hazard ratio [HR], 4.476; 95% confidence interval [CI], 1.725–11.618; P = 0.002), infection position ([HR], 113.826; [CI], 14.607-886.967; P < 0.001), white blood cell count, ([HR],1.209;[CI], 1.054–1.386; P = 0.007) ,hemoglobin ([HR], 0.970; [CI], 0.955–0.986; P < 0.001), platelet count ([HR], 0.993; [CI], 0.987–0.999; P = 0.026), neutrophil percentage ([HR], 1.115; [CI], 1.065–1.168; P < 0.001), lymphocyte percentage ([HR], 0.875; [CI], 0.827–0.927; P < 0.001), Neutrophil-to-Lymphocyte Ratio (NLR) ([HR], 1.144; [CI], 1.072–1.221; P < 0.001), Monocyte percentage ([HR], 0.752; [CI], 0.618–0.915; P = 0.004) were related to the prognosis (Table 4). Multivariate logistic regression analysis showed that the infection position remained was related to the prognosis, with statistical significance ([HR], 0.018; [CI], 0.001–0.384; P = 0.001), fasting blood glucose ([HR], 4.359; [CI]1.678–11.325; P = 0.003), and azole monotherapy ([HR], 0.134; [CI], 0.052–0.344; P < 0.001) were related to the prognosis. Further multivariate logistic regression analysis revealed that infection position remained significantly related to the prognosis ([HR], 0.018; [CI], 0.001–0.384; P = 0.010). (Fig. 2).
Discussion
Cryptococcus is an opportunistic pathogen that invades the lungs through the respiratory tract and gives rise to pulmonary cryptococcosis, which is the most prevalent form of cryptococcosis. When the immune system is compromised, Cryptococcus can breach the pulmonary immune defenses and disseminate to other body sites such as the central nervous system, lymph nodes, bones and joints, and skin, leading to disseminated cryptococcosis.
Cryptococcus is a lethal fungus whose polysaccharide capsules are considered the primary virulence factors [13]. Polysaccharides are immunomodulators, One of their target cell populations for modulation are macrophages, Polysaccharide capsules affect the immune function of macrophages by reducing the antigen presentation function, changing co-stimulatory molecules, regulating the secretion of pro-inflammatory and anti-inflammatory cytokines, and up-regulating the death receptor Fas/FasL to stimulate cell apoptosis [14,15,16,17,18]. Various studies have proved that cryptococcal antigen (CrAg) titer in blood and CSF could act as risk factors for predicting the extent of pulmonary cryptococcosis and outcome in non-HIV patients [19, 20]. We also analyzed the association of CrAg with cryptococcosis, but we found that there was no significant difference between the two groups for CrAg in serum, and no relationship was shown between CrAg and cryptococcosis outcome, which might due to the small size and individual difference.
Macrophages are vital cellular components of innate immunity, serving as the primary barrier against pathogens and regulating homeostasis and inflammatory responses. Macrophages hold an integral role in the defense against Cryptococcus, especially alveolar macrophages (AMs) as first responders, whose surface complement binds to mannose receptors, mediates phagocytosis, clears Cryptococcus or forms inflammatory granulomas to confine Cryptococcus to the lungs [21, 22]. Host cytokines kill Cryptococcus by inducing macrophage polarization. It has been shown that activation of M1 macrophages and downstream Th1 response effectively control Cryptococcus infection [23,24,25,26]. In addition, macrophages release high levels of reactive nitrogen intermediates (RNI), nitric oxide, reactive oxygen intermediates(ROI) and superoxide, which damage DNA and a number of chemical moieties of Cryptococcus [27]. Malfunction in macrophage development, activation, proliferation, and signaling collectively contribute to a heightened risk of disseminated cryptococcal infection [28,29,30,31]. Monocytes in the blood give rise to macrophages, which escape from blood vessels and infiltrate the tissues following further differentiation. We have observed a statistically significant decrease in the number of monocytes in the extrapulmonary infection group compared to that in the pulmonary infection group, which consequently leads to a secondary decrease in macrophages that could potentially facilitate the development of disseminated cryptococcosis.
NLR is regarded as a diagnostic and predictive marker of disease severity in patients with inflammatory ailments, which can mirror the balance between innate and adaptive immune reactions [32, 33], and the increase in NLR may indicate the inflammatory response to fungal infection, revealing, to some extent, the imbalance between inflammation and immune response in our investigation. Some studies found that an increase in the NLR during treatment may be used as an indicator of treatment failure for patients with cryptococcal meningitis [34]. In HIV-negative immunocompetent cryptococcal meningitis, they got the same conclusion, in addition, they proved the baseline high IgM indicated a low risk of post-infectious inflammatory response syndrome (PIIRS) development during the treatment [35]. lymphopenia and monocytopenia may be risk factors for cryptococcal dissemination [36], which agrees with our study. In our study, the percentage of neutrophils in the extrapulmonary infection group was higher than pulmonary infection group, hemoglobin, platelet count and lymphocyte percentage were lower. And univariate Analysis found that elevated white blood cells and neutrophils, decreased lymphocytes may serve as risk factors for the prognosis of cryptococcosis, which is consistent with the findings of prior investigations [37, 38]. Evidence suggests that neutrophils promote non-specific immunity and initiate the body’s response to inflammation, while lymphocytes are protective elements against inflammation. The increase of white blood cells and neutrophils in patients with cryptococcosis may be closely related to lymphopenia. It is well known that the patients with lymphopenia easily leads to microbial infection which can directly induce the recruitment of neutrophils to tissue sites and further promote the activation of neutrophils, resulting in the increase of the total number of white blood cells and the percentage of neutrophils [39,40,41]. To a certain extent, we can predict the prognosis by assessing the patient’s condition based on high neutrophils and low lymphocytes. Previous study also has proved that low CRP levels and high haemoglobin levels were risk factors for developing CM in cryptococcemia patients [42]. But in our study, we found that there was no significant difference between the two groups for CRP, and no relationship was shown between CRP and cryptococcosis outcome, which might due to the small size and individual difference.
Tian et al. found that underlying disease, dyskinesia, anemia, high peripheral blood neutrophils, low platelet count, high CSF fungal burden (measured by CrAg titer), and high CSF OP, were independently associated with prognosis in patients infected with ST5 lineage without HIV [20]. The results of another study in HIV-negative CM patients with acute/subacute onset suggest that the ratio of CSF glucose/blood glucose, impaired consciousness, and hospitalization length were indicated to be not only independent prognosis factors, but also factors significantly related to the survival time [43]. In a retrospective analysis of pulmonary cryptococcosis and extrapulmonary cryptococcosis, compared with pulmonary cryptococcosis, a larger proportion of extrapulmonary cryptococcosis patients were found to have immunocompromised conditions, which is consistent with the results of our study. Fever and headache were more common in extrapulmonary cryptococcosis patients [36]. And headache is an independent risk factor for poor prognosis in AIDS patients with cryptococcosis [44]. However, no similar phenomenon was found in our study, which may be for different groups of people, and the sample size can be further increased in the future to strengthen the robustness of the results.
In our study, multivariate analysis showed that extrapulmonary infection was a risk factor for the prognosis of cryptococcosis, and CM accounted for 86.7% of extrapulmonary infection. Breaking through the blood-brain barrier (BBB)is the most critical step in the pathogenesis of CM, current studies have found that Cryptococcus may have three potential traversal pathways to cross the BBB: Transcellular traversal, Trojan horse dissemination and the paracellular pathway [45, 46], and in which the transcellular traversal is primarily main pathway crossing the BBB [45, 47,48,49]. CD44 expressed on the surface of human brain microvascular endothelial cells (HBMEC) binds to hyaluronic acid in Cryptococcus, causing Cryptococcus to attach to HBMEC [50,51,52,53]. It has been shown that the cytoplasmic tail of CD44 interacts with HBMEC cytoskeletal linker proteins, which accumulate actin at the site of infection and promote cytoskeletal rearrangement [50]. Moreover, they found that Rac1 and other GTP-bound small Rho family proteins can regulate host cell actin cytoskeleton [54, 55]. Cryptococcus Plb1 helps fungi cross the BBB by activating host cell Rac1 and its association with STAT3 [56]. Although the mechanism of Cryptococcus entry into HBMEC remains further exploration, these related studies are based on the adhesion of Cryptococcus to HBMEC via hyaluronic acid and CD44, indicating the importance of CD44 in the invasion of Cryptococcus into the BBB. CD44 overexpression has been found in many diseases with abnormal immune status, such as HIV infection, tumors, and autoimmune diseases etc. Overexpression of the CD44 receptor results in heightened sensitivity to hyaluronic acid binding, which in turn promotes the invasiveness of Cryptococcus through the BBB [57,58,59,60,61,62]. This study reveals that the incidence of abnormal immune status was greater in the group with extrapulmonary infections, particularly in patients with CM, suggesting that abnormal immune status may contribute to central nervous system involvement.
There are several limitations of this study that must be acknowledged. Firstly, Cryptococcal disease was classified as “proven” based on the presence of consistent radiographic abnormalities and culture positivity obtained from sterile fluid or confirmed by biopsy. Unfortunately, the pulmonary puncture technique was not utilized during the early clinical period, which resulted in a miss ed diagnosis of pulmonary cryptococcal infection. Additionally, not all patients were tested for cryptococcal podococcal antigen due to doctors’ empirical consultations, which may have resulted in a missed diagnosis of peripheral blood cryptococcal infection. Secondly, this study involved a limited number of cases, and a large prospective study is needed to further confirm our findings. Finally, since this was a retrospective study, medical records were limited, and some clinical information, such as inflammatory indicators, were missing. However, this did not affect our analysis or final conclusions.
Conclusions
In conclusion, patients with abnormal immune status, decreased lymphocytes and monocytes, and increased neutrophils and NLR are more likely to develop extrapulmonary infection, whether novel exposure or through reactivation of a previously acquired latent infection. CM has a high mortality rate compared with pulmonary cryptococcosis. Timely identification of high-risk groups of CM and preventive antifungal treatment can reduce the incidence of CM. By delving into mechanisms of cryptococcal action that disrupt the BBB, inhibit receptor-ligand binding, and impede the transmission of signaling pathways, as well as by synergizing with antifungal medications, the objective of preventing and treating CM can be attained. This is poised to markedly elevate the prognostic outlook of cryptococcosis and mitigate its mortality.
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Mohamed SH, Nyazika TK, Ssebambulidde K, Lionakis MS, Meya DB, Drummond RA. Fungal CNS infections in Africa: the Neuroimmunology of Cryptococcal Meningitis. Front Immunol. 2022;13:804674.
Suwatanapongched T, Sangsatra W, Boonsarngsuk V, Watcharananan SP, Incharoen P. Clinical and radiologic manifestations of pulmonary cryptococcosis in immunocompetent patients and their outcomes after treatment. Diagn Interv Radiol. 2013;19(6):438–46.
Sun L, Chen H, Shao C, Song Y, Bai C. Pulmonary cryptococcosis with trachea wall invasion in an immunocompetent patient: a case report and literature review. Respiration. 2014;87(4):324–8.
Gao LW, Jiao AX, Wu XR, Zhao SY, Ma Y, Liu G, et al. Clinical characteristics of disseminated cryptococcosis in previously healthy children in China. BMC Infect Dis. 2017;17(1):359.
Ngan NTT, Flower B, Day JN. Treatment of cryptococcal meningitis: how have we got Here and where are we. Going? Drugs. 2022;82(12):1237–49.
Zhu LP, Wu JQ, Xu B, Ou XT, Zhang QQ, Weng XH. Cryptococcal meningitis in non-HIV-infected patients in a Chinese tertiary care hospital, 1997–2007. Med Mycol. 2010;48(4):570–9.
Chen J, Varma A, Diaz MR, Litvintseva AP, Wollenberg KK, Kwon-Chung KJ. Cryptococcus neoformans strains and infection in apparently immunocompetent patients, China. Emerg Infect Dis. 2008;14(5):755–62.
Li Z, Liu Y, Cao H, Huang S, Long M. Epidemiology and clinical characteristics of cryptococcal meningitis in China (1981–2013): a review of the literature. Med Mycology: Open Access. 2017;03(01).
Zhou L-H, Jiang Y-K, Li R-Y, Huang L-P, Yip C-W, Denning DW, et al. Risk-based Estimate of Human Fungal Disease Burden, China. Emerg Infect Dis. 2020;26(9):2137–47.
Setianingrum F, Rautemaa-Richardson R, Denning D. Pulmonary cryptococcosis: a review of pathobiology and clinical aspects. Med Mycol. 2019;57(2):133–50.
Donnelly J, Chen S, Kauffman C, Steinbach W, Baddley J, Verweij P, et al. Revision and update of the Consensus definitions of Invasive Fungal Disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infect Diseases: Official Publication Infect Dis Soc Am. 2020;71(6):1367–76.
Marr K, Sun Y, Spec A, Lu N, Panackal A, Bennett J, et al. A Multicenter, Longitudinal Cohort Study of Cryptococcosis in Human Immunodeficiency Virus-negative people in the United States. Clin Infect Diseases: Official Publication Infect Dis Soc Am. 2020;70(2):252–61.
Decote-Ricardo D, LaRocque-de-Freitas IF, Rocha JDB, Nascimento DO, Nunes MP, Morrot A, et al. Immunomodulatory Role of Capsular Polysaccharides constituents of Cryptococcus neoformans. Front Med (Lausanne). 2019;6:129.
Larocque-De-Freitas IF, Da Silva-Junior EB, Gemieski LP, Da Silva Dias Lima B, Diniz-Lima I, De Carvalho Vivarini A, et al. Inhibition of Microbicidal Activity of Canine macrophages DH82 Cell line by Capsular polysaccharides from Cryptococcus neoformans. J Fungi. 2024;10(5):339.
Larocque-De-Freitas IF, Rocha JDB, Nunes MP, Oliveira PAV, Nascimento DDO, Freire-De-Lima L et al. Involvement of the capsular GalXM-induced IL-17 cytokine in the control of Cryptococcus neoformans infection. Sci Rep. 2018;8(1).
Villena SN, Pinheiro RO, Pinheiro CS, Nunes MP, Takiya CM, DosReis GA, et al. Capsular polysaccharides galactoxylomannan and glucuronoxylomannan from Cryptococcus neoformans induce macrophage apoptosis mediated by Fas ligand. Cell Microbiol. 2008;10(6):1274–85.
Monari C, Paganelli F, Bistoni F, Kozel TR, Vecchiarelli A. Capsular polysaccharide induction of apoptosis by intrinsic and extrinsic mechanisms. Cell Microbiol. 2008;10(10):2129–37.
Monari C, Pericolini E, Bistoni G, Casadevall A, Kozel TR, Vecchiarelli A. Cryptococcus neoformans capsular glucuronoxylomannan induces expression of fas ligand in macrophages. J Immunol. 2005;174(6):3461–8.
Lin C, Yang TY, Chan MC, Hsu KH, Huang YH, Tseng JS. Comprehensive Analysis and Risk Identification of Pulmonary Cryptococcosis in Non-HIV patients. J Fungi (Basel). 2021;7(8).
Tian Y, Wang J, Shen Y, Zhao J, Hu J, Zhu X, et al. Characteristics and prognostic risk factors of patients with sequence type 5 lineage-associated cryptococcosis in China. Int J Infect Diseases: IJID : Official Publication Int Soc Infect Dis. 2023;128:244–53.
Redlich S, Ribes S, Schütze S, Eiffert H, Nau R. Toll-like receptor stimulation increases phagocytosis of Cryptococcus neoformans by microglial cells. J Neuroinflammation. 2013;10:71.
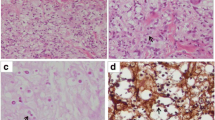
Wang DX, Zhang Q, Wen QT, Ding GX, Wang YG, Du FX, et al. Comparison of CT findings and histopathological characteristics of pulmonary cryptococcosis in immunocompetent and immunocompromised patients. Sci Rep. 2022;12(1):5712.
Hardison SE, Herrera G, Young ML, Hole CR, Wozniak KL, Wormley FL. Jr. Protective immunity against pulmonary cryptococcosis is associated with STAT1-mediated classical macrophage activation. J Immunol. 2012;189(8):4060–8.
De Leon-Rodriguez CM, Rossi DCP, Fu MS, Dragotakes Q, Coelho C, Guerrero Ros I, et al. The outcome of the Cryptococcus neoformans-Macrophage Interaction depends on phagolysosomal membrane Integrity. J Immunol. 2018;201(2):583–603.
Alvarez M, Casadevall A. Cell-to-cell spread and massive vacuole formation after Cryptococcus neoformans infection of murine macrophages. BMC Immunol. 2007;8(1):16.
Chrisman CJ, Albuquerque P, Guimaraes AJ, Nieves E, Casadevall A. Phospholipids trigger Cryptococcus neoformans capsular enlargement during interactions with amoebae and macrophages. PLoS Pathog. 2011;7(5):e1002047.
Nathan C, Shiloh MU. Reactive oxygen and nitrogen intermediates in the relationship between mammalian hosts and microbial pathogens. Proc Natl Acad Sci U S A. 2000;97(16):8841–8.
Leopold Wager CM, Hole CR, Wozniak KL, Olszewski MA, Wormley FL. Jr. STAT1 signaling is essential for protection against Cryptococcus neoformans infection in mice. J Immunol. 2014;193(8):4060–71.
Leopold Wager CM, Hole CR, Wozniak KL, Olszewski MA, Mueller M, Wormley FL. Jr. STAT1 signaling within macrophages is required for antifungal activity against Cryptococcus neoformans. Infect Immun. 2015;83(12):4513–27.
Campuzano A, Castro-Lopez N, Martinez AJ, Olszewski MA, Ganguly A, Leopold Wager C et al. CARD9 is required for classical macrophage activation and the induction of protective immunity against Pulmonary Cryptococcosis. mBio. 2020;11(1).
Viola GM, Malek AE, Rosen LB, DiNardo AR, Nishiguchi T, Okhuysen PC, et al. Disseminated cryptococcosis and anti-granulocyte-macrophage colony-stimulating factor autoantibodies: an underappreciated association. Mycoses. 2021;64(6):576–82.
Han Q, Wen X, Wang L, Han X, Shen Y, Cao J, et al. Role of hematological parameters in the diagnosis of influenza virus infection in patients with respiratory tract infection symptoms. J Clin Lab Anal. 2020;34(5):e23191.
Liu S, Wang X, She F, Zhang W, Liu H, Zhao X. Effects of Neutrophil-to-lymphocyte ratio combined with Interleukin-6 in Predicting 28-Day mortality in patients with Sepsis. Front Immunol. 2021;12:639735.
Zhang K, Li H, Zhang L, Liao W, Cai L, Li X, et al. The change in the Neutrophil/Lymphocyte ratio predicts the prognosis of patients with cryptococcal meningitis. Mycopathologia. 2021;186(6):857–62.
Wang Y, Wei H, Shen L, Su X, Liu J, Xu X, et al. Immunological predictors of Post Infectious Inflammatory Response Syndrome in HIV-Negative immunocompetent cryptococcal meningitis. Front Immunol. 2022;13:895456.
Shi J, Chen J, Hu L, Ma AHY, Hu H, Wang C, et al. Retrospective analysis of pulmonary cryptococcosis and extrapulmonary cryptococcosis in a Chinese tertiary hospital. BMC Pulm Med. 2023;23(1):277.
Mednick AJ, Feldmesser M, Rivera J, Casadevall A. Neutropenia alters lung cytokine production in mice and reduces their susceptibility to pulmonary cryptococcosis. Eur J Immunol. 2003;33(6):1744–53.
Wozniak KL, Kolls JK, Wormley FL. Depletion of neutrophils in a protective model of pulmonary cryptococcosis results in increased IL-17A production by gamma/delta T cells. BMC Immunol. 2012;13(1):65.
Hazeldine J, Lord J. Neutrophils and COVID-19: active participants and rational therapeutic targets. Front Immunol. 2021;12:680134.
Yang L, Liu S, Liu J, Zhang Z, Wan X, Huang B, et al. COVID-19: immunopathogenesis and immunotherapeutics. Signal Transduct Target Therapy. 2020;5(1):128.
Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respiratory Med. 2020;8(4):420–22.
Zhao H, Zhou M, Zheng Q, Zhu M, Yang Z, Hu C, et al. Clinical features and outcomes of Cryptococcemia patients with and without HIV infection. Mycoses. 2021;64(6):656–67.
Zheng H, Chen Q, Xie Z, Wang D, Li M, Zhang X, et al. A retrospective research of HIV-negative cryptococcal meningoencephalitis patients with acute/subacute onset. Eur J Clin Microbiol Infect Dis. 2016;35(2):299–303.
Liu S, Chen W, Cheng F, Ye X, Pan N, Lu H. Clinical characteristics and prognostic factors of 60 patients with acquired immune deficiency syndrome combined with Cryptococcus neoformans. BMC Infect Dis. 2023;23(1):204.
Chang Y, Stins M, McCaffery M, Miller G, Pare D, Dam T, et al. Cryptococcal yeast cells invade the central nervous system via transcellular penetration of the blood-brain barrier. Infect Immun. 2004;72(9):4985–95.
Stie J, Fox D. Blood-brain barrier invasion by Cryptococcus neoformans is enhanced by functional interactions with plasmin. Microbiology. 2012;158:240–58.
Liu T, Perlin D, Xue C. Molecular mechanisms of cryptococcal meningitis. Virulence. 2012;3(2):173–81.
Sabiiti W, May R. Capsule independent uptake of the fungal pathogen Cryptococcus neoformans into brain microvascular endothelial cells. PLoS ONE. 2012;7(4):e35455.
Jong A, Wu C, Gonzales-Gomez I, Kwon-Chung K, Chang Y, Tseng H, et al. Hyaluronic acid receptor CD44 deficiency is associated with decreased Cryptococcus neoformans brain infection. J Biol Chem. 2012;287(19):15298–306.
Jong A, Wu C-H, Shackleford GM, Kwon-Chung KJ, Chang YC, Chen H-M, et al. Involvement of human CD44 during Cryptococcus neoformans infection of brain microvascular endothelial cells. Cell Microbiol. 2008;10(6):1313–26.
Huang SH, Long M, Wu CH, Kwon-Chung KJ, Chang YC, Chi F, et al. Invasion of Cryptococcus neoformans into human brain microvascular endothelial cells is mediated through the lipid rafts-endocytic pathway via the dual specificity tyrosine phosphorylation-regulated kinase 3 (DYRK3). J Biol Chem. 2011;286(40):34761–9.
Long M, Huang SH, Wu CH, Shackleford GM, Jong A. Lipid raft/caveolae signaling is required for Cryptococcus neoformans invasion into human brain microvascular endothelial cells. J Biomed Sci. 2012;19(1):19.
Jong A, Wu CH, Chen HM, Luo F, Kwon-Chung KJ, Chang YC, et al. Identification and characterization of CPS1 as a hyaluronic acid synthase contributing to the pathogenesis of Cryptococcus neoformans infection. Eukaryot Cell. 2007;6(8):1486–96.
Chang YC, Stins MF, McCaffery MJ, Miller GF, Pare DR, Dam T, et al. Cryptococcal yeast cells invade the Central Nervous System via Transcellular Penetration of the blood-brain barrier. Infect Immun. 2004;72(9):4985–95.
Kim KS. Mechanisms of microbial traversal of the blood–brain barrier. Nat Rev Microbiol. 2008;6(8):625–34.
Maruvada R, Zhu L, Pearce D, Zheng Y, Perfect J, Kwon-Chung KJ, et al. Cryptococcus neoformans phospholipase B1 activates host cell Rac1 for traversal across the blood-brain barrier. Cell Microbiol. 2012;14(10):1544–53.
He X, Shi X, Puthiyakunnon S, Zhang L, Zeng Q, Li Y, et al. CD44-mediated monocyte transmigration across Cryptococcus neoformans-infected brain microvascular endothelial cells is enhanced by HIV-1 gp41-I90 ectodomain. J Biomed Sci. 2016;23:28.
Deboux C, Ladraa S, Cazaubon S, Ghribi-Mallah S, Weiss N, Chaverot N, et al. Overexpression of CD44 in neural precursor cells improves trans-endothelial migration and facilitates their invasion of perivascular tissues in vivo. PLoS ONE. 2013;8(2):e57430.
Hiscox S, Baruha B, Smith C, Bellerby R, Goddard L, Jordan N, et al. Overexpression of CD44 accompanies acquired tamoxifen resistance in MCF7 cells and augments their sensitivity to the stromal factors, heregulin and hyaluronan. BMC Cancer. 2012;12:458.
Hou C, Ishi Y, Motegi H, Okamoto M, Ou Y, Chen J, et al. Overexpression of CD44 is associated with a poor prognosis in grade II/III gliomas. J Neurooncol. 2019;145(2):201–10.
Liu Y, Wu T, Lu D, Zhen J, Zhang L. CD44 overexpression related to lymph node metastasis and poor prognosis of pancreatic cancer. Int J Biol Markers. 2018;33(3):308–13.
Grisar J, Munk M, Steiner CW, Amoyo-Minar L, Tohidast-Akrad M, Zenz P, et al. Expression patterns of CD44 and CD44 splice variants in patients with rheumatoid arthritis. Clin Exp Rheumatol. 2012;30(1):64–72.
Acknowledgements
Not applicable.
Funding
This work was supported by Xiaowu Zhu famous doctor studio under grant NO.CY2019002.
Author information
Authors and Affiliations
Contributions
ZWT, QQP designed this study. YLS and QQP performed the data acquisition. ZWT, CYW and ZH performed data analysis. ZWT, YLS, SCZ and YJ edited the manuscript. YLW and XWZ supervised the present study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study conformed to the ethical guidelines of the Declaration of Helsinki and was approved by The Ethics Committee of The First Affiliated Hospital with Nanjing Medical University. With the approval of the Ethics Committee (protocol 2021-SR-566), informed consent was waived because of the retrospective nature of the study, and the analysis used anonymous clinical data. Clinical trial number: not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tao, Z., Pu, Q., Shen, Y. et al. Clinical characteristics and prognostic factors of pulmonary and extrapulmonary cryptococcosis. BMC Infect Dis 24, 1018 (2024). https://doi.org/10.1186/s12879-024-09895-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09895-9