Abstract
The neurological complications of influenza affect mainly the pediatric Asian population. In the category of influenza-associated encephalopathy, acute necrotizing encephalopathy (ANE) is a rapidly progressive and fulminant brain disorder associated with significant neurological sequelae and mortality. To date, only a few adult cases of influenza-associated ANE have been reported. We describe a 44-year-old woman who presented with rapid progression of consciousness impairment and recurrent generalized convulsions. Influenza was diagnosed three days prior to presentation, and infection with influenza A (H3N2) pdm09 was subsequently confirmed. A diagnosis of ANE was made based on the presence of characteristic brain MRI findings, the exclusion of central nervous system infection, and an elevated serum interleukin-6 level. Pulse steroid therapy followed by tocilizumab was initiated, which led to clinical stabilization and improvement. Genetic testing revealed that the patient carried heterozygous human leukocyte antigen DQB1 03:03 and DRB1 09:01 genotypes. An analysis of the adult cases of influenza-associated ANE in the literature and the present case revealed a wide range of ages (22–71 years), a short interval (median 3 days) between the clinical onset of influenza and ANE, and a high overall mortality rate (32%). The thalamus was the most frequent (91%) location of the lesions. Our report highlights the importance of identifying this devastating but treatable neurological complication of influenza in adults, especially those of Asian descent. As a cytokine storm is the most accepted pathogenic mechanism for ANE, cytokine-directed therapies may be promising treatments for which further investigation is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Influenza is a highly contagious infectious disease that causes a substantial burden on health services. Seasonal epidemics of influenza lead to approximately one billion cases worldwide, including 3 to 5 million cases of severe illness associated with a death rate of up to 10% [1]. In Taiwan, the Center of Disease Control noted 3.5 to 9.5 influenza cases with severe complications per 100,000 people annually during the pre-COVID-19 epidemic era [2]. Moreover, influenza may be associated with diverse complications along the neuroaxis. The most common neurological complications are seizure and influenza-associated encephalopathy. Less common or rare conditions include meningitis, central nervous system demyelination, Reye syndrome, stroke, Guillain–Barré syndrome and myopathy [3, 4]. Influenza-associated neurological complications affect mainly pediatric patients, occurring in up to 7.6 to 16.9% of children hospitalized with influenza [3, 5,6,7]. Moreover, Asian race has been identified as a risk factor for the development of influenza-associated neurological complications [3].
In the category of influenza-associated encephalopathy, acute necrotizing encephalopathy (ANE) is a rare brain disorder characterized by multiple symmetric brain lesions, alterations in mental status with rapidly progressive neurological deterioration, and a high rate of significant neurological sequelae or mortality [8]. ANE usually develops following infection with various viruses, including influenza A and B, SARS-CoV-2, enterovirus, human herpesvirus 6 (HHV-6) and dengue virus, and rarely Mycoplasma pneumoniae [8]. However, there is little evidence of direct brain invasion by infectious pathogens. In some cases, ANE can occur spontaneously, recurs, or is associated with a family history, suggesting an underlying genetic predisposition [9]. In line with this, mutations in RANBP2 have been found to be linked to the development of a specific type of ANE that is named ANE1 [9].
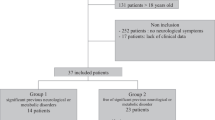
Since it was first described in Japanese children in 1995 [10], ANE has been found to predominantly affect the Asian pediatric population, especially those under 5 years of age [11]. In contrast, only a limited number of adult cases of influenza-associated ANE have been reported to date. Here, we report the case of an adult patient with ANE and antecedent infection with influenza A virus who subsequently received steroid and anticytokine treatment and survived. We also report our findings from a review of the literature on adult cases of influenza-associated ANE.
Case presentation
A 44-year-old Taiwanese female with a history of thyroid goiter had headache, fever, sore throat, cough and rhinorrhea in August 2023. She was diagnosed with influenza A infection through a rapid throat swab test on the third day of symptom presentation and was treated with inhaled zanamivir. The next day, she was sent to the emergency service because of sudden alterations in consciousness and recurrent tonic‒clonic seizure episodes. Her Glasgow Coma Scale (GCS) score was E1V1M4, temperature was 37.2 °C, blood pressure was 112/52 mmHg, and heart rate was 95/min. Her blood leukocyte count was 7100/μL (neutrophil percentage = 87.7%), C-reactive protein level was 7.89 mg/L (normal < 5), aspartate aminotransferase level was 41 U/L (normal < 34), alanine aminotransferase level was 24 U/L (normal < 36), ammonia level was 72 μg/dL (normal < 96), and creatinine level was 0.61 mg/dL. Brain CT showed multiple subcortical hypodense lesions in the bilateral cerebral hemispheres. Cerebrospinal fluid (CSF) analysis revealed one monocyte/μL, 1080 erythrocytes/μL, an elevated protein level (77 mg/dL), and normal glucose (84 mg/dL) and lactate (18.3 mg/dL) levels. She subsequently required endotracheal intubation for mechanical ventilation due to respiratory failure. Lorazepam and levetiracetam (for status epilepticus), peramivir (for severe complicated influenza) and ceftriaxone (empiric antibiotic for suspected adult bacterial meningitis) were given.
She was admitted to the neurology intensive care unit on Day 2 of the neurological episode. Electroencephalography demonstrated generalized continuous theta activity. Her neurological condition improved only slightly (GCS E3VeM4), although her seizure activity subsided after treatment. Brain MRI revealed extensive T2 and FLAIR-hyperintense lesions in the white matter of the bilateral cerebral hemisphere, corpus callosum, thalamus, and midbrain and the right middle cerebellar peduncle (Fig. 1A-E). Some of the lesions contained areas of restricted diffusion (Fig. 1F). Proton magnetic resonance spectroscopy revealed increased intensity of the lactate peaks in the white matter lesions (Fig. 1G). Autoantibodies from the autoimmune encephalitis panel were negative. For detecting pathogens, the patient’s CSF was examined for bacterial culture, virus isolation and DNA of herpes simplex virus (HSV) and varicella zoster virus (VZV), and tested with a FilmArray Meningitis/Encephalitis Panel (bioMérieux, France) for detecting genomes of cytomegalovirus, enterovirus, HSV-1, HSV-2, VZV, human herpes virus 6, human parechovirus, E. coli K1, Haemophilus influenzae, Listeria monocytogenes, Neisseria meningitides, Streptococcus agalactiae, Streptococcus pneumonia, and Cryptococcus neoformans/gattii. Serological tests for Japanese encephalitis virus and dengue viruses were negative. bacterial culture, virus isolation, serological tests and PCR for genome for various infectious pathogens in CSF were all negative. Acute disseminated encephalomyelitis (ADEM) was initially considered, and steroid therapy (methylprednisolone 1 g/day for five days, followed by oral prednisolone 1 g/kg body weight/day) was initiated on Day 5. Repeated brain MRI on Day 9 revealed similar findings. On Day 11, a blood test revealed an increase in the interleukin-6 (IL-6) level (46.7 pg/ml, normal < 7) despite the concurrent use of steroids. On the basis of these findings, combined with the prodromal viral infection, the brain MRI findings and the exclusion of infectious encephalitis, ANE related to influenza A was diagnosed. A dose of tocilizumab 400 mg (2 mg/kg body weight) was thus administered intravenously, and oral prednisolone treatment was continued. She soon became more awake and was able to open her eyes spontaneously two days later. The endotracheal tube and mechanical ventilation were removed on Day 17. Urinary tract infection by Klebsiella aerogenes developed on Day 18, which resolved with a course of treatment with cefperazone/sulbactam. However, the residual neurological deficits were severe. She presented with akinetic mutism (GCS E4V1M4) with general spasticity, rigidity and hyperreflexia and was wheelchair-ridden when discharged one month later. She needed one-person assistance to stand, had a modified Rankin scale score of 4, and had the same neurological examination findings three months after discharge.
A-E Brain MRI demonstrated diffuse and generally symmetric T2 and FLAIR-hyperintense lesions in the white matter of the bilateral cerebral hemisphere, corpus callosum, thalamus and midbrain (A, B, D, E, FLAIR; C, T2 weighted image). Small areas of restricted diffusion were present (F, diffuse weighted image). 1H-magnetic resonance spectroscopy revealed increased intensity of lactate peaks in the cerebral white matter lesion (G, arrow)
Infection with the influenza A(H3N2)pdm09 strain was subsequently confirmed by RT‒PCR. To investigate genetic predisposition for ANE, sequence-based genotyping for HLA and CPT2 were performed. It revealed that the patient carried heterozygous HLA-DQB1 03:03 and HLA-DRB1 09:01 alleles and was homozygous for p.lIe368 and p.Met647 in CPT2, all of these four variants having been associated with increased risk for ANE [12, 13].
Discussion
Review of the literature on adult cases of influenza-associated ANE
We searched in PubMed and Google Scholar with the terms “acute necrotizing encephalopathy”, “influenza” and “adult” without limitation of language from 1995 (the year ANE first described). After eliminating duplicate cases and including the present case, we identified a total of 22 adult (≥ 18 years of age) patients (11 males, 11 females) with influenza-associated ANE, with one patient who experienced an ANE episode during childhood (Table 1) [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. The ages ranged from 22 to 71 (median 47) years. The influenza type was known in 20 patients, including influenza A in 15 patients and influenza B in 5 patients. Among the 9 patients who received influenza A virus typing, the H1N1 strain was identified in 7, and the H3N2 strain was identified in the other 2.
The median interval between the onset of ANE and that of prodromal influenza was 3 days (ranging from 0 to 9 days, data available in 18 patients). The leading clinical manifestations were conscious impairment (68%), altered mentality or behaviors (50%) and convulsive seizures (36%). The most common neuroimaging abnormality was acute inflammation of the thalamus (91%), which was usually bilaterally affected, followed by the cerebral hemisphere (59%), brainstem (50%), cerebellum (36%), basal ganglion (18%) and corpus callosum (14%). Regarding CSF studies (performed in 17 patients), an increase in protein levels (> 45 mg/dl) was the most common abnormality (14 patients, 82%), while leukocyte pleocytosis (> 5/mm3) was found in only five (29%) patients. For immunotherapy, 9 patients received combined corticosteroids and intravenous immunoglobulin (IVIg) treatment, 9 received corticosteroids alone, and 1 received IVIg only. Our patient is the only one who received tocilizumab treatment. Seven patients died during acute stage of the disease, with a mortality rate 32%. The survival rate was 74% for patients receiving corticosteroids, IVIg or both and 33% for those not receiving immunotherapy, suggesting a statistically nonsignificant trend toward increased survival associated with any immunotherapy (odds ratio 5.6, 95% CI 0.41–76; p = 0.163). It is noteworthy, however, that the sample size was small, and the timing, type and duration of immunotherapy were highly variable among these patients. Compared with pediatric cases of ANE related to influenza or other pathogens, there were no obvious differences in the intervals between the onset of influenza and ANE, clinical presentations, brain images, CSF profiles or mortality rate for these adult cases of influenza-associated ANE.
Clinical manifestations of ANE
Despite the diversity of infection pathogens, the clinical, radiological and laboratory presentations of parainfectious ANE are relatively stereotypic. Clinically, three stages in the clinical course could be identified in most ANE patients [34]. During the prodromal stage, the patients presented systemic manifestations of acute viral infections, most frequently respiratory tract manifestations, as well as generalized symptoms such as fever, headache, myalgia and malaise, but still had normal consciousness. Brain imaging findings were usually normal at this stage. The acute encephalopathy stage followed suddenly a few days after prodromal onset. It was characterized by rapidly progressive neurological dysfunction with mental and conscious deterioration, which was often combined with seizures and focal neurological deficits. The typical brain imaging findings during this stage were multifocal and generally symmetric inflammatory lesions of the cerebral cortex, white matter, deep gray matter, cerebellum and brainstem, with bilateral thalamic involvement being the most common and distinctive presentation [35, 36]. Occasionally, petechial hemorrhage occurred in the lesions. Acute extraneural organ injury, such as hepatic, hematological and pulmonary dysfunction, occurred in some patients [37]. The mortality rate could reach 25–40% [8, 38, 39]. While some patients with catastrophic encephalopathy who survived recovered gradually in the following several weeks, most of them had persistent and significant neurological sequelae.
Diagnosis of ANE
The diagnostic criteria for ANE was proposed by Muzuguchi in 1997 [40]. Focusing on a neurological complication following viral infection and with exclusion of several clinical mimics in mind, this criteria encompasses the characteristic clinical presentation (rapid conscious alternation, convulsion), brain imaging features (symmetric multifocal lesions with bilateral thalamic lesions), CSF study findings (increase of protein level without leukocyte pleocytosis) and systemic involvement (increase of serum aminotransferase levels with elevation of ammonia). It is still widely applied to date in diagnosis of spontaneous or infection-provoked ANE.
The differential diagnosis for ANE includes practically all of the post-infectious central nervous system complications, with ADEM, Reye syndrome and infectious encephalitis as the leading conditions to consider. ADEM and ANE shared a lot of clinical similarities, such as rapid development of conscious disturbance, altered mentality, seizure and multiple brain lesions. While ANE occurs during the early febrile period of viral infection, ADEM typically develops up to several (mean 12.5) days after the initial symptoms and signs of infection subsides [41]. Different from normal cell counts in CSF in most cases of ANE [42], ADEM patients usually show neutrophil pleocytosis in CSF analysis. Regarding neuroimaging findings, the multiple brain lesions are generally symmetric in distribution in ANE and the bilateral thalamic involvement is highly specific. In contrast, the bilateral brain lesions are asymmetric and the bilateral thalamic lesion is present only in 30—50% of ADEM patients [43]. Reye syndrome also has similar clinical manifestations with ANE. However, the most common laboratory finding for Reye syndrome is hyperammonemia occurring 1 to 2 days after onset, sometimes combined with hypoglycemia and coagulation dysfunction. These findings however are absent in ANE patients [40]. Besides, imaging and pathology studies in Reye syndrome shows only diffuse brain edema, in contrast that multifocal lesions in neuroimaging are essential for diagnosing ANE. Finally, ANE can be differentiated from infectious meningoencephalitis through specific antibody testing, microbial culture or isolation, or direct detection of the pathogen genome in CSF.
Pathogenesis of ANE
Although the pathogenesis of ANE remains unclear, the uncontrolled production of proinflammatory cytokines by the innate immune system (“cytokine storm”) in response to viral infection is the most commonly proposed mechanism [8, 44]. The cytokines involved in ANE may include various interleukins, interferons and chemokines, with IL-6 and tumor necrosis factor-α being the most prominent [8, 44]. In in vivo and in vitro studies, the administration of IL-6 and tumor necrosis factor-α to cerebral vessels led to vasodilation, endothelial tight junction perturbation and subsequent blood‒brain barrier (BBB) breakdown [45,46,47]. In line with this, brain biopsy and postmortem pathologic examinations in ANE patients have shown minimal lymphocytic or neutrophilic infiltrations or demyelination, despite marked brain parenchyma abnormalities such as hemorrhagic or coagulation necrosis and edema and axonal damage [23, 24, 48,49,50], and CSF pleocytosis is usually absent [42]. In addition to disrupting BBB integrity, excessive cytokines also cause excitotoxic neuronal damage, immune cell overactivation and secondary organ damage. Microglial priming, a condition in which microglia multiply and become activated, may also underlie ANE. Priming increases the sensitivity of microglia to a secondary inflammatory stimulus (e.g., peripheral cytokine release), which can induce an exaggerated immunological response. This mechanism has been shown to contribute to the neurological complications associated with nonneurotropic influenza strains, such as H1N1 [51] and H3N2 [52]. Clinically, a higher serum level of IL-6 is correlated with the development of brainstem dysfunction, which has been associated with an increased risk of mortality in ANE patients [53, 54].
Host genetic factors of ANE
Genetic background may contribute to the predilection of ANE in East Asian populations. The HLA DQB1 03:03 and DRB1 09:01 genotypes and the thermolabile CPT2 variants, which have the highest frequencies in the eastern ethnicities, have been associated with ANE [12, 13]. Our patient carried two HLA alleles and two homozygous CPT2 risk variants for ANE. HLA genes govern antigen presentation and are crucial components of the human immune system. Carnitine palmitoyl transferase II, the protein encoded by CPT2, is one of the mitochondrial enzymes essential for long-chain fatty acid oxidation. Mitochondrial dysfunction and energy deficiency may underlie BBB disruption and cerebral edema in ANE [55]. On the other hand, the relationship between ANE1 (the ANE caused by RANBP2 mutations) penetrance and environmental triggers [9] and a case report of a Caucasian infant who resided in East Asia for the first several months of life and developed HHV-6-associated ANE three months after returning to a western country [56] imply the role of environmental factors in the predisposition to ANE occurrence. More studies are needed to elucidate the complexity of interactions between infectious pathogens and genetic or environmental factors in ANE development.
Treatment of ANE
Although there has been no definitive guideline for management of ANE to date, most recommended treatments involve immunotherapeutic regimens which are given early and in combinations. A retrospective case-series study showed that administration of corticosteroids, either methylprednisolone or dexamethasone, within 24 h after onset was associated with better prognosis [57]. The common immunomodulatory treatments combined with steroid include IVIg and plasmapheresis. Furthermore, regarding the potentially pivotal role of cytokines in ANE development, anticytokine therapy is considered a rational treatment for ANE. Tocilizumab, a monoclonal antibody blocking the IL-6 receptor, has been shown to significantly lower IL-6 levels and has become an emerging therapy for ANE. Case reports and a small uncontrolled study findings have suggested that tocilizumab may have synergistic effects with corticosteroid and may be effective for severe ANE when administered early in the disease course [58,59,60,61]. However, whether tocilizumab reduces mortality or possibility of severe neurological sequelae is still unclear.
Conclusions
In the face of the growing prevalence of re-emerging and emerging infectious diseases in recent years, the occurrence of neurological complications related to viral infections, including ANE, is expected to increase. For instance, with the pandemic of COVID-19, ANE related to SARS-CoV-2 has been increasingly recognized in recent years. SARS-CoV2-associated ANE is similar to influenza-associated ANE in presenting symptoms, onset time related to prodromal infection, typical locations of brain lesions, CSF and serum cytokine profiles, and disease outcome [62]. Remarkably, adult patients may account for a higher proportion in SARS-CoV2-associated ANE, up to 80% in a case series [62]. Our report highlights the importance of identifying this devastating but treatable neurological complication of viral infections in adults, especially in East Asian populations. In addition, cytokine-inhibiting monoclonal antibodies may be promising treatments for ANE, for which further investigation is warranted.
Availability of Data and Materials
The datasets generated and/or analyzed during the current study are available in the figshare repository, https://figshare.com/articles/figure/An_adult_case_of_acute_necrotizing_encephalopathy/25992166.
Abbreviations
- ADEM:
-
Acute disseminated encephalomyelitis
- ANE:
-
Acute necrotizing encephalopathy
- BBB:
-
Blood‒brain barrier
- CSF:
-
Cerebrospinal fluid
- GCS:
-
Glasgow Coma Scale
- HHV-6:
-
Human herpesvirus 6
- HLA:
-
Human leukocyte antigen
- HSV:
-
Herpes simplex virus
- IL-6:
-
Interleukin 6
- IVIg:
-
Intravenous immunoglobulin
- VZV:
-
Varicella zoster virus
References
World Health Organization website. https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal). Accessed 15 Apr 2024.
Taiwan Center for Disease Control website. https://www.cdc.gov.tw/Category/MPage/6YQ32GG9EOdXNTjPqUDT1A. Accessed 17 Apr 2024.
Antoon JW, Hall M, Herndon A, Johnson DP, Brown CM, Browning WL, et al. Prevalence, risk factors, and outcomes of influenza-associated neurologic complications in children. J Pediatr. 2021;239:32-38.e5.
Tsai JP, Baker AJ. Influenza-associated neurological complications. Neurocrit Care. 2013;18:118–30.
Choi GJ, Park JY, Choi JS, Choi SR, Kim D, Lee JH, et al. Influenza-associated neurologic complications in hospitalized pediatric patients: a multicenter retrospective study in Republic of Korea. Pediatr Infect Dis J. 2021;40:e466–71.
Frankl S, Coffin SE, Harrison JB, Swami SK, McGuire JL. Influenza-associated neurologic complications in hospitalized children. J Pediatr. 2021;239:24-31.e1.
Jantarabenjakul W, Paprad T, Paprad T, Anugulruengkitt S, Pancharoen C, Puthanakit T, et al. Neurological complications associated with influenza in hospitalized children. Influenza Other Respir Viruses. 2023;17:e13075.
Shukla P, Mandalla A, Elrick MJ, Venkatesan A. Clinical manifestations and pathogenesis of acute necrotizing encephalopathy: the interface between systemic infection and neurologic injury. Front Neurol. 2022;12:628811.
Neilson DE, Adams MD, Orr CM, Schelling DK, Eiben RM, Kerr DS, et al. Infection-triggered familial or recurrent cases of acute necrotizing encephalopathy caused by mutations in a component of the nuclear pore, RANBP2. Am J Hum Genet. 2009;84:44–51.
Mizuguchi M, Abe J, Mikkaichi K, Noma S, Yoshida K, Yamanaka T, et al. Acute necrotising encephalopathy of childhood: a new syndrome presenting with multifocal, symmetric brain lesions. J Neurol Neurosurg Psychiatry. 1995;58:555–61.
Wang GF, Li W, Li K. Acute encephalopathy and encephalitis caused by influenza virus infection. Curr Opin Neurol. 2010;23:305–11.
Hoshino A, Saitoh M, Miyagawa T, Kubota M, Takanashi JI, Miyamoto A, et al. Specific HLA genotypes confer susceptibility to acute necrotizing encephalopathy. Genes Immun. 2016;17:367–9.
Shinohara M, Saitoh M, Takanashi J, Yamanouchi H, Kubota M, Goto T, et al. Carnitine palmitoyl transferase II polymorphism is associated with multiple syndromes of acute encephalopathy with various infectious diseases. Brain Dev. 2011;33:512–7.
Abdelrahman HS, Safwat AM, Alsagheir MM. Acute necrotizing encephalopathy in an adult as a complication of H1N1 infection. BJR Case Rep. 2019;5:20190028.
Alkhashan S, Samir N. Acute necrotizing encephalitis in an adult patient with novel influenza A (H1N1) infection. Open Access J Neurol Neurosurg. 2015;1:1–4.
Alsolami A, Shiley K. Successful treatment of influenza-associated acute necrotizing encephalitis in an adult using high-dose oseltamivir and methylprednisolone: case report and literature review. Open Forum Infect Dis. 2017;4:ofx145.
Bloch C, Suter B, Fischmann A, Gensicke H, Rüegg S, Weisser M. Only a touch of the flu? the simultaneous manifestation of acute necrotizing encephalopathy in two consanguineous patients. Open Forum Infect Dis. 2015;2:ofv013.
Chen KC, Gow CH, Yang CJ, Chang HT. Successful high-dosage dexamethasone treatment of H1N1 influenza A pneumonia complicated with acute necrotizing encephalitis in an HIV-Infected adult. Case Rep Clin Med. 2015;4:245–9.
Erdil E, Vural E, Koytak PK, Tuncer EN. Successful treatment of influenza B associated acute necrotizing encephalopathy in an adult using combination of high dose oseltamivir-IVIG-pulse methylprednisolone. Acta Neurol Belg. 2021;121:1863–5.
Fasano A, Natoli GF, Cianfoni A, Ferraro D, Loria G, Bentivoglio AR, Servidei S. Acute necrotizing encephalopathy: a relapsing case in a European adult. J Neurol Neurosurg Psychiatry. 2008;79:227–8. https://doi.org/10.1136/jnnp.2007.127670.
Hernandez R, Ota R, Medina Y, Hernandez Y, Julayanont P, Wilms H. Acute necrotizing encephalopathy. Proc (Bayl Univ Med Cent). 2022;35:725–7.
Huijsmans RLN, Braber A, Fokke C, Lo Ten Foe JR, Kuindersma M. Influenza-geassocieerde acute necroticserende encefalitis. Ned Tijdschr Geneeskd. 2023;167:D7537 (Dutch).
Ishii N, Mochizuki H, Moriguchi-Goto S, Shintaku M, Asada Y, Taniguchi A, Shiomi K, Nakazato M. An autopsy case of elderly-onset acute necrotizing encephalopathy secondary to influenza. J Neurol Sci. 2015;354(1–2):129–30.
Lee YJ, Smith DS, Rao VA, Siegel RD, Kosek J, Glaser CA, Flint AC. Fatal H1N1-related acute necrotizing encephalopathy in an adult. Case Rep Crit Care. 2011;2011(562516).
Iijima H, Wakasugi K, Ayabe M, Shoji H, Abe T. A case of adult influenza A virus-associated encephalitis: magnetic resonance imaging findings. J Neuroimaging. 2002;12:273–5.
Iizuka K, Suzuki K, Shiina T, Nakamura T, Funakoshi K, Hirata K. Two adult patients with acute necrotizing encephalopathy following influenza virus infection. Rinsho Shinkeigaku. 2020;60:157–61. (Japanese).
McCray BA, Forst D, Jindal J, Henderson GV. Clinical reasoning: A 57-year-old woman who developed acute amnesia following fever and upper respiratory symptoms. Neurology. 2015;84:e102–6.
Meijer WJ, Linn FH, Wensing AM, Leavis HL, van Riel D, GeurtsvanKessel CH, Wattjes MP, Murk JL. Acute influenza virus-associated encephalitis and encephalopathy in adults: a challenging diagnosis. JMM Case Rep. 2016;3:e005076.
Ochi N, Takahashi K, Yamane H, Takigawa N. Acute necrotizing encephalopathy in an adult with influenza A infection. Ther Clin Risk Manag. 2018;14:753–6.
Odagiri A, Yamaoka A, Miyata K, Bunya N, Kasai T, Takeyama Y, Uemura S, Mikami T, Narimatsu E. Elderly-onset acute necrotizing encephalopathy mimicking severe heat stroke: a case report and review of the literature. Acute Med Surg. 2019;6:316–20.
Piradov MA, Ryabinkina YV, Luneva IE, Polishchuk RV, Chernobaeva LS, Bormin AA, Antipiat NA. Ostryĭ nekroticheskiĭ éntsefalit, assotsiirovannyĭ s virusom grippa u vzroslykh. Zh Nevrol Psikhiatr Im S S Korsakova. 2019;119:100–5 (Russian).
Tsubota M, Kato A, Goshima T, Imai K, Yamagishi Y, Matsushima A, Sasano H, Hattori T. Rapidly progressive acute necrotizing encephalopathy associated with influenza A in an elderly adult. Acute Med Surg. 2020;7:e611.
Ventura E, Summa A, Ormitti F, Picetti E, Crisi G. Influenza A H1N1 related acute necrotizing encephalopathy: radiological findings in adulthood. Neuroradiol J. 2012;25:397–401.
Levine JM, Ahsan N, Ho E, Santoro JD. Genetic acute necrotizing encephalopathy associated with RANBP2: clinical and therapeutic implications in pediatrics. Mult Scler Relat Disord. 2020;43:102194.
Vanjare HA, Selvi BT, Karuppusami R, Manesh A, Gunasekaran K, Prabhakar AT, et al. Clinical and radiologic findings of acute necrotizing encephalopathy in young adults. AJNR Am J Neuroradiol. 2020;41:2250–4.
Wu L, Peng H, Jiang Y, He L, Jiang L, Hu Y. Clinical features and imaging manifestations of acute necrotizing encephalopathy in children. Int J Dev Neurosci. 2022;82:447–57.
Lee YJ, Hwang SK, Kwon S. Acute necrotizing encephalopathy in children: a long way to go. J Korean Med Sci. 2019;34:e143.
Mizuguchi M. Acute necrotizing encephalopathy. Nihon Rinsho. 2011;69:465–70.
Lee CG, Kim JH, Lee M, Lee J. Clinical outcome of acute necrotizing encephalopathy in related to involving the brain stem of single institution in Korea. Korean J Pediatr. 2014;57:264–70.
Mizuguchi M. Acute necrotizing encephalopathy of childhood: a novel form of acute encephalopathy prevalent in Japan and Taiwan. Brain Dev. 1997;19:81–92.
Li K, Li M, Wen L, Wang Q, Ding X, Wang J. Clinical presentation and outcomes of acute disseminated encephalomyelitis in adults worldwide: systematic review and meta-analysis. Front Immunol. 2022;13:870867.
Wu X, Wu W, Pan W, Wu L, Liu K, Zhang HL. Acute necrotizing encephalopathy: an under recognized clinicoradiologic disorder. Mediators Inflamm. 2015;2015:792578.
Alper G. Acute necrotizing encephalopathy mimicking ADEM. In: Waubant E, Lotze TE, editors. Pediatric demyelinating diseases of the central nervous system and their mimics: a case-based clinical guide. Cham: Springer; 2017. p. 11–5.
Qin N, Wang J, Peng X, Wang L. Pathogenesis and management of acute necrotizing encephalopathy. Expert Rev Neurother. 2023;23:641–50.
de Vries HE, Blom-Roosemalen MC, van Oosten M, de Boer AG, van Berkel TJ, Breimer DD, et al. The influence of cytokines on the integrity of the blood-brain barrier in vitro. J Neuroimmunol. 1996;64:37–43.
Tsao N, Hsu HP, Wu CM, Liu CC, Lei HY. Tumour necrosis factor-alpha causes an increase in blood-brain barrier permeability during sepsis. J Med Microbiol. 2001;50:812–21.
Cheng Y, Desse S, Martinez A, Worthen RJ, Jope RS, Beurel E. TNFα disrupts blood brain barrier integrity to maintain prolonged depressive-like behavior in mice. Brain Behav Immun. 2018;69:556–67.
Chen CI, Mar S, Brown S, Song SK, Benzinger TL. Neuropathologic correlates for diffusion tensor imaging in postinfectious encephalopathy. Pediatr Neurol. 2011;44:389–93.
San Millan B, Teijeira S, Penin C, Garcia JL, Navarro C. Acute necrotizing encephalopathy of childhood: report of a Spanish case. Pediatr Neurol. 2007;37:438–41.
Lyon JB, Remigio C, Milligan T, Deline C. Acute necrotizing encephalopathy in a child with H1N1 influenza infection. Pediatr Radiol. 2010;40:200–5.
Jurgens HA, Amancherla K, Johnson RW. Influenza infection induces neuroinflammation, alters hippocampal neuron morphology, and impairs cognition in adult mice. J Neurosci. 2012;32:3958–68.
Hosseini S, Wilk E, Michaelsen-Preusse K, Gerhauser I, Baumgärtner W, Geffers R, et al. Long-term neuroinflammation induced by influenza A virus infection and the impact on hippocampal neuron morphology and function. J Neurosci. 2018;38:3060–80.
Aiba H, Mochizuki M, Kimura M, Hojo H. Predictive value of serum interleukin-6 level in influenza virus-associated encephalopathy. Neurology. 2001;57:295–9.
Ichiyama T, Isumi H, Ozawa H, Matsubara T, Morishima T, Furukawa S. Cerebrospinal fluid and serum levels of cytokines and soluble tumor necrosis factor receptor in influenza virus-associated encephalopathy. Scand J Infect Dis. 2003;35:59–61.
Kubota M, Chida J, Hoshino H, Ozawa H, Koide A, Kashii H, et al. Thermolabile CPT II variants and low blood ATP levels are closely related to severity of acute encephalopathy in Japanese children. Brain Dev. 2012;34:20–7.
Kansagra SM, Gallentine WB. Cytokine storm of acute necrotizing encephalopathy. Pediatr Neurol. 2011;45:400–2.
Okumura A, Mizuguchi M, Kidokoro H, Tanaka M, Abe S, Hosoya M, Aiba H, Maegaki Y, Yamamoto H, Tanabe T, Noda E, Imataka G, Kurahashi H. Outcome of acute necrotizing encephalopathy in relation to treatment with corticosteroids and gammaglobulin. Brain Dev. 2009;31:221–7.
Hosie PH, Lim C, Scott TRD, Cardamone M, Farrar MA, Frith C, et al. Treatment of severe acute necrotizing encephalopathy of childhood with interleukin-6 receptor blockade in the first 24 h as add-on immunotherapy shows favorable long-term outcome at 2 years. Brain Dev. 2023;45:401–7.
Azmi A, Zainal Abidin AS. Good outcome with respect to acute necrotizing encephalitis in children associated with post-infectious SARS-CoV-2. Cureus. 2023;15:e43198.
Huang Y, Zhou B, Hong S, Cai Y. A case report and literature review on tocilizumab-cured acute necrotizing encephalopathy caused by influenza A virus. Front Pediatr. 2024;12:792578.
Koh JC, Murugasu A, Krishnappa J, Thomas T. Favorable outcomes with early interleukin 6 receptor blockade in severe acute necrotizing encephalopathy of childhood. Pediatr Neurol. 2019;98:80–4.
Geng C, Zhao W, Wang Z, Wu J, Jiang D, Jiang N, Liu M, Yao M, Guan H. Acute necrotizing encephalopathy associated with COVID-19: case series and systematic review. J Neurol. 2023;270:5171–81.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
MYL, YLT and YYC: study conceptualization and design. HC, SCL, YLT and YTL: data collection. SCL: literature review. SCL and MYL: genetic testing and data analysis. HC: writing of the first draft. MYL: manuscript review and critique. All authors reviewed the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, H., Lan, SC., Tseng, YL. et al. Acute necrotizing encephalopathy in adult patients with influenza: a case report and review of the literature. BMC Infect Dis 24, 931 (2024). https://doi.org/10.1186/s12879-024-09844-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09844-6