Abstract
Background
Identifying valid and accessible tools for monitoring and improving physical activity levels is essential for promoting functional ability and healthy aging. The Physical Activity Scale for the Elderly (PASE) is a commonly used and recommended self-report measure of physical activity in older adults. The objective of this scoping review was to map the nature and extent to which the PASE has been used in the literature on community-dwelling older adults, including the evidence for its psychometric properties.
Methods
Seven electronic databases (MEDLINE (Ovid), Embase (Ovid), AMED (Ovid), Emcare (Ovid), CINAHL (EBSCO), Ageline (EBSCO)) were searched from inception to January 25, 2023. Studies were included if physical activity was part of the aim(s) and measured using the PASE, participants had a mean age of 60 years or older and lived in the community, and papers were peer-reviewed journal articles published in English. Pairs of independent reviewers screened abstracts, full-texts, and extracted data. Where possible, weighted mean PASE scores were calculated for different subgroups based on age, sex, and clinical population.
Results
From 4,124 studies screened, 232 articles from 35 countries met the inclusion criteria. Most studies were cross-sectional (60.78%), completed in high-income countries (86.4%) and in North America (49.57%). A variety of clinical conditions were included (n = 21), with the most common populations being osteoarthritis (n = 13), Parkinson’s disease (n = 11), and cognitive impairment (n = 7). Psychometric properties of ten versions of the PASE were found. All versions demonstrated acceptable test-retest reliability. Evidence for construct validity showed moderate correlations with self-reported physical activity, fair to moderate with accelerometry derived activity and fair relationships with physical function and self-reported health. Pooled means were reported in graphs and forest plots for males, females, age groups, and several clinical populations.
Conclusion
The PASE was widely used in a variety of clinical populations and geographical locations. The PASE has been culturally adapted to several populations and evaluated for its reliability and convergent validity; however, further research is required to examine responsiveness and predictive validity. Researchers can use the weighted mean PASE scores presented in this study to help interpret PASE scores in similar populations.
OSF registration
osf.io/7bvhx
Similar content being viewed by others
Background
A pressing issue in the current healthcare system is the growing burden of chronic disease and multimorbidity associated with the world’s aging population [1, 2]. There is an increasing number of older adults who require home care or housing options to support additional needs, including retirement homes, assisted living, or long-term care facilities [1]. Maintaining functional ability in later adulthood is a key public health priority and the promotion of physical activity (PA) is a central strategy for healthy aging initiatives [3]. Regular participation in PA has been shown to improve physical function, reduce impairments, promote independent living, and improve quality of life in older adults [4]. Physical activity can assist in maintaining cardiovascular, metabolic, and cognitive function; all of which reduce the risk of multimorbidity [5,6,7].
The World Health Organization (WHO) defines PA as “any bodily movement produced by skeletal muscles that requires energy expenditure” [8]. A growing body of evidence has demonstrated the importance of overall activity levels, including lighter intensity activities [9]. In addition to recommendations for moderate to vigorous activities, PA guidelines encourage changes in time allocation from sitting activities to light intensity activities, including standing [8, 10]. Given the inclinations for lighter intensity activities in older ages (e.g., walking, gardening), clinicians and researchers must have tools to accurately assess and monitor the full spectrum of physical activities in this population.
Direct measures of PA (e.g., pedometers, accelerometers, and the gold standard of the doubly labelled water method) [11] can capture the full spectrum of activities. However, these measures can be more expensive, rely on equipment availability, and place a greater burden on participants [5]. Alternatively, self-report measures can be a low-cost, feasible tool for assessing and monitoring activity levels [12]. While not all questionnaires capture the same breadth of activities, the Physical Activity Scale for the Elderly (PASE) has been recommended for use in older adults for its inclusion of lighter intensity activities [5]. The PASE was designed to consider a greater number of activity domains more representative of the typical activities undertaken by older adults (e.g., gardening and household tasks) [13]. The questionnaire was developed for older adults (≥ 65), takes approximately 10 min to complete (10 questions), and asks participants to recall their activity over the last 7-days [13, 14]. Activity types include sitting, walking, sport/recreation, exercise, occupational, and household [13]. A total score for PA can be calculated using these answers and the predetermined weights associated with each activity [13]. The PASE has been described as a suitable PA outcome measure for older adults who have multiple chronic conditions and is a recommended for measuring total PA in older adults based on evidence for its reliability and validity compared to other questionnaires [12].
To date, there has not been a comprehensive review of the populations and settings in which the PASE has been used. Rather, the literature on the PASE has focused on comparing the psychometric properties of multiple self-report measures of PA for specific populations. For example, Sattler et al. (2020) explored PA measures in healthy older adults and Garnett et al. (2019) in community-dwelling older adults with multiple chronic conditions. As part of their syntheses of all self-report PA measures both included a summary on the PASE, of ten and seven studies respectively [5, 12]. As both these reviews recommend the use of the PASE, a more thorough exploration of the PASE with broader criteria is warranted. Further, the extent of the literature on its psychometric properties has not been thoroughly investigated. Therefore, the purpose of this scoping review was to map the nature and extent of the literature on the PASE in older populations (mean age 60) and to consolidate knowledge about the characteristics of studies using the PASE as an outcome measure, including available data on its psychometric properties. Our research questions were as follows:
-
1.
To what extent has the PASE been used in older populations (e.g., number of studies, PASE administration, outcome operationalization from the PASE)?
-
2.
What are the characteristics of studies that have used the PASE as an outcome measure (e.g., locations, sample characteristics, study designs)?
-
3.
What is the nature and extent of the literature on the psychometric properties of the PASE in older populations (e.g., reliability, validity, cultural translation)?
Methods
The JBI guidelines for scoping reviews were followed in addition to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) guidelines (checklist available in Additional file 1 Table A1) [15, 16]. This review protocol was registered with Open Science Framework (https://doi.org/10.17605/OSF.IO/7BVHX).
Search strategy
A broad search strategy was created with the assistance of a research librarian at the Health Sciences Library at McMaster University using the following key terms: “Physical Activity Scale for the Elderly”, “PASE”, “physical activity profile”, and “older”. Unique search strategies were developed for the following electronic databases: MEDLINE (Ovid), Embase (Ovid), Allied and Complementary Medicine Database (AMED; Ovid), Emcare (Ovid), CINAHL (EBSCO), Ageline (EBSCO). Databases were searched from inception to January 25th, 2023. Backward citation searching was performed in Web of Science (Clarivate) for the original PASE article by Washburn and colleagues [13]. The complete search strategy for all databases is available in Additional file 1 Table A2. Reference lists of relevant systematic reviews, meta-analyses, and scoping reviews were screened and hand searched for additional articles.
Inclusion/exclusion criteria
To be included in this review studies must have populations consisting of older adults with a mean age greater than or equal to 60 years in line with the United Nations definition of older adults [17]. No restrictions were placed on sex, race or cultural background.
The overarching concept for this scoping review was the PASE; this included the original version and translated versions. Therefore, to be included studies must have incorporated PA in their aims and present results from the administration of the PASE. This criterion was further refined to specify that PASE must be included as a primary or secondary outcome (i.e., not just a covariate). The outcomes of interest to this review were the characteristics of the studies (e.g., cross-sectional vs prospective) and populations the PASE was used in (e.g., country, clinical populations, sex), mean total scores of the PASE, how the PASE was used (e.g., to look at relationships with PA, to determine intervention efficacy), as well as psychometric properties that have been evaluated.
Studies from any geographic location were included. After initial full-text screening the inclusion criteria was further refined to improve heterogeneity of included studies and ensure feasibility of the project due to the large number of results. The setting was restricted to designated community-dwelling populations which reflects the original context the PASE was designed in [13].
Studies were excluded if they were not written in English or if they were conference abstracts, presentations, systematic reviews, meta-analyses, scoping reviews, evidence maps, rapid reviews, literature reviews, narrative reviews, or critical reviews. Reviews were flagged and screened for additional citations.
Study selection
Results from the comprehensive literature search were organized in Endnote 20 (Clarivate, Philadelphia, USA) and uploaded to Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) for screening. Duplicated studies were removed using both programs prior to screening and any remaining were removed by hand. Prior to each phase of screening the reviewer team conducted pilot screening to improve agreement. For title and abstracts screening and full-text eligibility two independent reviewers (NB, LL, JL, IV, SH, and CD) confirmed the predetermined eligibility criteria. Due to the volume of full-text screening authors were not contacted for further details; where information for a given eligibility criteria was not reported or unclear the paper was excluded. Any disagreements during the abstract or the full-text review process were resolved by either consensus or arbitration by a third reviewer when necessary.
Data extraction and analysis
Data was extracted from the studies verbatim by two or more independent reviewers (NB, LL, JL, IV, SH, and CD). Modifications to the initial data extraction table made during the piloting process included the removal of details not necessary in a scoping review (e.g., funding sources, conflicts of interest) and the aims of this study (e.g., setting, recruitment methods). Additionally, separate columns were added to distinguish values calculated or extrapolated by reviewers versus authors (e.g., mean PASE scores, income classification). The following descriptive data was extracted: study details (geographical location, outcome measures, study design), population description (number of participants, mean age, sex, clinical population), PASE version and administration method, how the PASE was reported (e.g., mean vs categorical, subcategories vs full questionnaire), and psychometric properties reported.
Data was summarized in a descriptive manner through counts and percentages in tabular presentation. Weighted means and variances were calculated for total PASE scores across identified subgroups (sex, age, and clinical populations) where appropriate using the ‘metamean’ package in RStudio Team (R version 4.2.2, 2020, PBC, Boston, MA). In studies that reported only subgroup mean total PASE score or age, the authors combined the subgroup data using methods recommended in the Cochrane handbook [18]. Where possible, studies that provided median scores were converted to mean scores using the methodology developed by Wan et al. [19]. Studies that did not provide sufficient information for either transformation were omitted from some review syntheses. Studies were grouped by income based on the World Bank ratings from 2023 [20].
Results
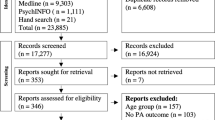
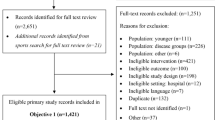
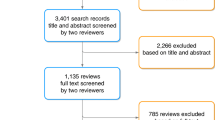
The database search produced 6,372 articles and hand searching citations produced another 24 articles for a total of 6,396. A total of 886 studies were assessed for full-text eligibility and 536 articles were found to use the PASE in older adults, 232 of which met all inclusion criteria (i.e., community-dwelling and the PASE was a primary/secondary outcome). An overview of the screening process can be found in PRISMA-ScR flow diagram (Fig. 1), and reasons for full-text study exclusions can be found in Additional file 2 Table A2.
Summary of PASE use
The PASE was used for a variety of reasons with the most common being to explore the effect of PA on a health outcome(s) (e.g., an association of PA type with all-cause mortality) [21], and the relationship of a determinant with PA (e.g., the association between walkability and walking time) [22]. Almost all the studies used the PASE in its entirety (96.55%). The studies that used partial aspects of PASE often focused on leisure time PA (e.g., walking, sport/recreation, and exercise) [23,24,25], and two studies focused on walking exclusively [26, 27]. Most authors (93.97%) used total PASE scores (i.e., used provided activity weights). Nineteen studies (8.19%) included a measure other than central tendency for total PASE score (e.g., dichotomous, tertiles, quartiles, quintiles). Eleven studies did not use the PASE score but instead operationalized PA using different pieces of the PASE (e.g., frequency, time). Details on the use of PASE are summarized in Table 1.
The PASE was primarily delivered in person (69.40%) followed by mail (11.21%); 45 studies were either unclear or did not report how the PASE was administered to participants. A total of 15 different versions or languages were reported; the most common version used was English (63.79%). Six studies did not report which version or language the PASE was delivered in. In many cases, only the seminal paper on the English version by Washburn et al. was cited, with no further clarification of the version or modifications made, including several papers from countries where the primary language is not English (n = 29).
Study characteristics
A summary of the study characteristics can be found in Table 2. The PASE was used throughout the world; however, nearly half of the studies were completed in North America (49.57%). In total, studies from 35 different countries were included in this review; the most common countries outside of North America included China (n = 20), Australia (n = 19), and Japan (n = 10). Most studies were conducted in high-income countries (86.64%). The mean age for studies ranged from 60.00 [28] to 84.40 [29] with the majority (43.10%) falling between 70–74 years old. Most studies included mixed sex samples (n = 184), with only 17 looking at females and 22 at males. Fifty-three studies looked specifically at 21 clinical conditions (e.g., musculoskeletal, cognitive impairment, and cardiorespiratory). The 232 studies of community-dwelling older adults included 171,206 participants, with individual study samples ranging from 8 [30] to 14,881 [31]. Studies were published between 1993 [13] and 2023 [32,33,34,35,36]. The PASE was used in a variety of study designs, including cross-sectional studies (60.78%), prospective studies (25.43%), and experimental (12.07%).
Where possible, weighted means for different subgroups were summarised based on age, sex, and clinical population. Studies with a mean age between 60–64 years had the highest mean PASE scores (159.53 (95% CI 146.58, 172.49)) and studies with a mean age over 80 years old had the lowest mean PASE scores (67.17 (95% CI 51.95, 82.39)) (Fig. 2, Forest plots available in Additional file 1 Figure B1-B5). Figure 3 presents forest plots for the combined total mean PASE score for female only studies (n = 13) 123.99 (95% CI 108.09, 139.88) [26, 37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] and male only studies (n = 14) 136.27 (95% CI 122.46, 150.09) [52,53,54,55,56,57,58,59,60,61,62,63,64,65]. Based on data availability, pooled means were created for the following clinical populations: cancer (n = 2) [28, 66], Chronic Obstructive Pulmonary Disease (COPD) (n = 2) [67, 68], cognitive impairment (n = 6) [33, 69,70,71,72,73], Diabetes (n = 3) [74,75,76], Osteoarthritis (n = 12) [46, 77,78,79,80,81,82,83,84,85,86,87], and Parkinson’s disease (PD) (n = 10) [88,89,90,91,92,93,94,95,96,97]. Forest plots for clinical populations are available in Additional file 1 Figure B6.
Psychometric properties of the PASE
Several papers evaluated the psychometric properties of the original PASE (n = 5) along with a number of validation studies (n = 14) for different translations and clinical populations (acute coronary event [98], COPD [68], Cancer [28, 66], and Parkinson’s disease [89]). In total, ten different versions of the PASE were assessed for reliability and/or validity in community-dwelling older adults, including: English (n = 5) [13, 14, 66, 98, 99], Malay (n = 2) [100, 101], Arabic (n = 1) [102], Chinese (n = 2) [68, 103], Italian (n = 1) [104], Norwegian (n = 1) [105], Persian (n = 1) [106], Polish (n = 1) [107], Taiwanese (n = 2) [28, 108], Turkish (n = 1) [109], and two studies did not report the version [65, 89].
Sixteen studies reported on the test-retest reliability of the PASE, time frames ranging from 3 days [99, 105] to 3–7 weeks [13] and sample sizes ranging from 18 [98] to 349 [100] (details available in Table 3). Across all versions of the PASE 12 studies reporting ICCs for the total score, only two fell below acceptable limits proposed in the COSMIN guidelines [110] (Malay version 0.49 (95% CI 0.37, 0.59) [100] and version NR 0.66 (95% CI 0.46–0.71) [89]). However, the majority of values were 0.90 and above (n = 8). Internal consistency was examined in seven versions and all Cronbach alpha’s fell within an acceptable range (0.70 (Arabic and Persian subcategory lowest) to 0.82 (Italian total score)). Only four studies examined measurement error. Alqarni et al. reported the minimal detectable change (MDC95) for PASE subcategories (9.0–23.6) [102] of the Arabic version and MDC95 for total scores were provided for the Chinese version (19.21) [68] and the Polish version (38.39) [107]. Two studies also included standard errors of measurement for the PASE total score (Chinese version 6.93 [68] and NR version 30.00 [89]).
Four studies stated they were exploring criterion validity; however, each used a different measurement tool as their gold standard for PA: pedometer (walking steps and energy expenditure) [68], Actigraph (activity counts/minutes) [28], International Physical Activity Questionnaire (IPAQ) [109], doubly labeled water (total energy expenditure, energy expenditure/resting metabolic rate) and VO2max [65]. The PASE was significantly correlated to all but the doubly labelled water outcomes and VO2max [65]. During the development of the PASE Washburn et al. assessed the three aspects content validity by asking participants (n = 36) about the appropriateness of the items, the completeness (i.e., comprehensiveness), and the comprehensibility; results were used to inform the final version of the PASE [13]. Three additional studies assessed and reported acceptable content validity for the PASE across three different clinical groups: acute coronary events (English) [98], COPD (Chinese) [68], and cancer survivors (Taiwanese) [28]. Only the English version had responsiveness and minimal important difference (MID) reported and this was in a sample of individuals with lung cancer [66].
Construct validity was the most commonly assessed form of validity, predominantly exploring convergent validity (details available in Table 4). Physical function performance measures and self-report questionnaires were commonly cited, and relationships ranged from fair to moderate, including the Timed Up and Go (r = -0.45 to r = -0.69) [102, 106, 107], Berg Balance (r = 0.20 to r = 0.82) [14, 104, 107], and the physical function section of the Short Form-36 (r = 0.53 to r = 0.58) [68, 103, 109]. Muscle strength was another common construct with poor to fair correlations; specifically, grip strength (r = 0.29 to r = 0.43) [13, 68, 100, 102, 103], and lower limb strength (r = 0.18 to r = 0.37) [13, 66, 103]. There were also several self-report measures examining general health (r = -0.12 to r = 0.44) [13, 68, 98, 100, 103] and activities of daily living (r = 0.10 to r = 0.78) [100, 106]. The PASE demonstrated moderate correlations with the IPAQ (r = 0.65 to r = 0.74) [68, 107, 109]. Five studies compared the PASE to a direct measure of PA (e.g., accelerometers and pedometers), including outcomes such as steps per day (r = 0.39 to r = 0.61) [66, 68, 101] and activity counts (r = 0.43 to r = 0.64) with fair to moderate correlations [28, 99, 101]. Only Bonnefoy et al. used the gold standard doubly labelled water, and they found no significant correlations [65].
Discussion
To the authors’ knowledge, this is the first review to provide a comprehensive summary of the use of the PASE in community-dwelling older adults. The PASE has been used extensively to measure PA in older adults (536 primary papers before restricting to community-dwelling settings); however, it was mainly used in high-income countries with cross-sectional research designs. While strong evidence was summarized supporting test-retest reliability and construct validity, there was a paucity of evidence examining the PASE’s responsiveness, important change thresholds, and predictive validity. In addition, we have presented pooled means for different age groups and clinical populations to provide preliminary reference values to improve interpretations of total scores.
The PASE has been used extensively in community-dwelling older adults; 171,206 participants from 35 countries were included in this review. The PASE was developed in the United States, which is reflected in the greater uptake in North America and high-income countries [13]. However, the PASE has been used across five continents and in some middle-income countries (n = 8). Importantly, we have seen the validation of several translated versions including Arabic, Chinese, Malay, Persian, and Turkish. Furthermore, the application of the PASE to clinical and disease-specific populations has also occurred, and the high content validity in these populations is promising. The use of the PASE in persons with chronic conditions has been supported previously based on feasibility and psychometric properties [5]. While the literature summarized is extensive, more is available outside of community-dwelling populations not captured in this review, including further translations and validations (e.g., Nigerian translation) [111]. Our results show the PASE is a commonly used measure of worldwide but has been used sparingly in countries outside of North America and in lower-income countries. Decreasing the heterogeneity in how PA is measured is imperative for meaningful comparisons and data harmonization. Large numbers of self-report PA measures already exist, and previous work has recommended using these rather than creating more [12, 112]. This review shows the large uptake of the PASE, presenting a suitable choice for research on older adults. However, it is important that psychometric measures are assessed for the population of interest.
Psychometric properties are essential for outcome measures to ensure their validity, reliability, and interpretability. Of the 232 studies included, 19 studies aimed to examine the psychometric properties of the PASE in community-dwelling older adults. According to COSMIN, most studies (12/15) found acceptable test-retest reliability for the PASE total score. However, there was variability between studies that was more pronounced between subcategories of activity types (e.g., ICC subcategory values 0.56–0.94 [99], 0.76–0.93 [106], 0.78–0.99 [107]), which may suggest more variation week to week in single activity types and less for overall activity. There was a paucity of evidence on measurement error, including MDC and standard error of measurement. Of the four studies reporting in this area, one only provided values for activity subcategories, not total score [102], and two were for clinical populations (COPD and Parkinson’s disease). The varying populations may explain the large difference in values (e.g., MDC95 = 38.4 (general) vs MDC95 = 19.2(COPD); and SEM = 30 (PD) vs SEM = 6.9 (COPD)). Establishing the minimal detectable change values is essential for ensuring differences are real and not from measurement error. In addition, none of the included studies reported minimal clinically important differences (MCID), another important parameter for interpreting change in score. This paucity of evidence must be addressed across versions in community-dwelling older adults to support further use and interpretability of the PASE.
The PASE was validated in community-dwelling older adults in ten different languages. Content validity is regarded as the most important psychometric measurement property [113]; however, other than the sentinel paper, only three included studies reported on the relevance, comprehensiveness, and comprehensibility [28, 68, 98]. As presented in these papers, PA appears to be influenced by cultural/societal norms, highlighting the importance and continued need to verify the content validity of PA questionnaires when validating in new populations [28]. Fair to moderate relationships between the PASE and performance-based measures of physical function and mobility, strength, and health outcomes were regularly reported for construct validity. Four studies stated they examined criterion validity, which compares the PASE score to the gold standard of the same construct. However, only one study used the commonly regarded gold standard of PA doubly labelled water and did not find a significant relationship [65]. The remaining three studies found moderate correlations (> 0.60) using more accessible measures of PA: a pedometer [68], accelerometer [28], and a questionnaire [109]. The PASE-Polish [107] demonstrated the highest correlation at 0.74 with the IPAQ, which has been validated in 12 different countries, including low-income countries and rural samples [114]. The IPAQ was the only PA questionnaire reported, and only two other studies compared direct measures of PA (i.e., accelerometers). The correlations with the IPAQ ranged from 0.65–0.74, whereas correlations with direct measures tended to be lower and more variable (e.g., activity counts 0.43–64, walking steps 0.39–0.61). Several PASE versions did not contain a measure of PA in their validity analysis (n = 3). Further studies investigating these metrics using a wider variety of measures of PA (e.g., different questionnaires and more direct measures) are needed to clarify these relationships.
No studies reported on longitudinal validity, demonstrating a great need for studies to evaluate the PASE’s predictive validity for important health outcomes in community-dwelling populations across the globe. Despite almost 20 studies using the PASE to measure change in PA, responsiveness, which is critical for ensuring the PASE can accurately reflect change over time, has not been reported in any of the included studies. Therefore, research is needed to explore the predictive validity and responsiveness of the PASE to inform whether the PASE can be used to predict important health outcomes (e.g., future falls, hospitalization) and change in PA (e.g., over time or through intervention) for community-dwelling older adults.
A noteworthy finding of this review was the reporting of pooled means by age, sex, and clinical population. Pooled PASE scores decreased with increasing age groups from < 65 (159.53 (95% CI 146.58, 172.49)) to the 80 years and older group (67.17 (95% CI 51.95, 82.39)). In general, this is consistent with the literature where levels of PA progressively decrease with age for both men and women [115, 116]. Some clinical populations appeared to have greater decreases in PA than others (e.g., cognitive impairment 91.11 (95% CI 72.77, 109.40) vs osteoarthritis 129.53 (95% CI 110.40, 148.65)). Clinical groups also appear to be important in addition to age for PA level; for example, the studies in the cognitive impairment group were mostly younger age groups (5/6 less than 80 years old), but the mean PASE score was closer to the two oldest age groups. The provided reference data for age, sex, and clinical population can be used to improve the interpretability of PASE scores among similar populations of community-dwelling older adults. However, future research creating normative values for the PASE could further improve interpretability and uptake of this questionnaire.
There are several limitations of this scoping review that should be acknowledged. First, several eligibility criteria were placed on this review, resulting in papers related to the PASE being excluded. Specifically, studies were restricted to the English language, age of 60 years or older, and community-dwelling settings. These decisions were made for feasibility and to reflect the original PASE; however, they have limited our understanding of how far the PASE has been applied in different populations. With the robust search strategy reviewed by a health research librarian, we are confident that the summarized evidence accurately reflects the current literature for community-dwelling older adults. A second limitation is that only published studies were included, and grey literature was not considered, which opens the possibility that new and emerging research regarding the PASE was missed. Finally, several studies used data from the same databases/studies, resulting in the same or overlapping samples; we did not extract the information necessary to tease this apart. Therefore, pooled means will be biased toward samples included more than once. In addition, pooled mean PASE scores in clinical populations with only two studies should be interpreted cautiously due to limited sample sizes.
This review has identified areas for future consideration, including further expanding the validation of the PASE to middle- and low-income countries. A systematic review focused on the psychometric properties of the PASE with no setting restrictions may provide a valuable resource for researchers. Future investigations are needed on psychometric properties of the PASE, including thresholds of important change, responsiveness, and predictive validity for all versions of the PASE, as well as data on psychometric properties in specific clinical populations.
Conclusion
This review found that the PASE is a widely used PA measure among community-dwelling older adults, with evidence supporting its test-retest reliability and construct validity. The widespread use of a questionnaire increases the ability for data harmonization across studies and improves the ability to compare between studies. Further research is warranted to investigate the PASE’s ability to detect meaningful change (i.e., MDC, MCID) along with predictive validity and responsiveness. Pooled mean total PASE scores reported in this review can provide preliminary reference values for different age groups and clinical populations to help improve the interpretability of PASE scores until normative values are established.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Abbreviations
- COPD:
-
Chronic Obstructive Pulmonary Disease
- IPAQ:
-
International Physical Activity Questionnaire - Short Form
- PA:
-
Physical activity
- PASE:
-
Physical Activity Scale for the Elderly
- PD:
-
Parkinson’s Disease
- PRISMA-ScR:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
- MCID:
-
Minimal clinical important difference
- MDC:
-
Minimal detectable change
- ICC:
-
Intraclass correlation coefficient
- IQR:
-
Interquartile range
- SD:
-
Standard deviation
- SEM:
-
Standard error of measurement
- TUG:
-
Timed Up and Go
- WHO:
-
World Health Organization
- NR:
-
Not reported
- CI:
-
Confidence Interval
References
Statistics Canada. Census in Brief: A portrait of Canada’s growing population aged 85 and older from the 2021 Census. Catalogue no. 98-200-X(2021004). 2022. Available from: https://www12.statcan.gc.ca/census-recensement/2021/as-sa/98-200-X/2021004/98-200-X2021004-eng.cfm#moreinfo.
Kirkland SA, Griffith LE, Menec V, Wister A, Payette H, Wolfson C, et al. Mining a unique Canadian resource: the Canadian longitudinal study on aging. Can J Aging. 2015;34(3):366–77.
Decade of healthy aging: baseline report. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
Cunningham C, O’Sullivan R. Why physical activity matters for older adults in a time of pandemic. Eur Rev Aging Phys Act. 2020;17(1):16.
Garnett A, Ploeg J, Markle-Reid M, Strachan PH. Self-report tools for assessing physical activity in community-living older adults with multiple chronic conditions: a systematic review of psychometric properties and feasibility. Can J Aging. 2020;39(1):12–30.
Mcphee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. 2016;17(3):567–80.
Steeves JA, Shiroma EJ, Conger SA, Van Domelen D, Harris TB. Physical activity patterns and multimorbidity burden of older adults with different levels of functional status: NHANES 2003–2006. Disabil Health J. 2019;12(3):495–502.
WHO guidelines on physical activity and sedentary behaviour. Geneva: Worl Health Organization; 2020.
Mayo A, Sénéchal M, Boudreau J, Bélanger M, Bouchard DR. Potential functional benefits of a comprehensive evaluation of physical activity for aging adults: a CLSA cross-sectional analysis. Aging Clin Exp Res. 2021;33(2):285–9.
Ross R, Chaput JP, Giangregorio LM, Janssen I, Saunders TJ, Kho ME, et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S57–102.
Rao AK. Wearable Sensor Technology to Measure Physical Activity (PA) in the Elderly. Current Geriatrics Reports. 2019;8(1):55–66.
Sattler MC, Jaunig J, Tosch C, Watson ED, Mokkink LB, Dietz P, et al. Current evidence of measurement properties of physical activity questionnaires for older adults: an updated systematic review. Sports Med (Auckland, NZ). 2020;50(7):1271–315.
Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153–62.
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52(7):643–51.
Aromataris E, Munn Z. JBI manual for evidence synthesis. 2020.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
United Nations, Department of Economic and Social Affairs PD. World Population Ageing 2017. 2017;ST/ESA/SER.A/408. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/May/un_2017_worldpopulationageing_report.pdf.
Higgins J, Li T, Deeks JE. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane handbook for systematic reviews of interventions version 62 (updated February 2021). Cochrane; 2021. Available from www.training.cochrane.org/handbook.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135.
The World Bank. World Bank Country and Lending Groups - World Bank Data Help Desk. The World Bank Group. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.Cited 2021 July.
Yu R, Leung J, Woo J. Housework reduces all-cause and cancer mortality in Chinese men. PLoS One. 2013;8(5):e61529.
Yu R, Cheung O, Lau K, Woo J. Associations between perceived neighborhood walkability and walking time, wellbeing, and loneliness in community-dwelling older Chinese people in Hong Kong. Int J Environ Res Public Health. 2017;14(10):1199.
Liang Y, Lai FTT, Kwan JLY, Chan W, Yeoh E-K. Sport and recreational physical activities attenuate the predictive association of multimorbidity with increased geriatric depressive symptoms: a 14-year follow-up study of community-dwelling older adults. J Aging Phys Act. 2022;30(2):252–60.
Kitano N, Tsunoda K, Tsuji T, Osuka Y, Jindo T, Tanaka K, et al. Association between difficulty initiating sleep in older adults and the combination of leisure-time physical activity and consumption of milk and milk products: a cross-sectional study. BMC Geriatr. 2014;14:118.
Wang YF, Li NY, Zhu JJ, Deng Q, Hu JLL, Xu J, et al. Association between socio-ecological factors and leisure time physical activity (LTPA) among older adults in Sichuan, China: a structural equation modeling analysis. BMC Geriatr. 2022;22(1):60.
Kenny AM, Dawson L, Kleppinger A, Iannuzzi-Sucich M, Judge JO. Prevalence of sarcopenia and predictors of skeletal muscle mass in nonobese women who are long-term users of estrogen-replacement therapy. J Gerontol A Biol Sci Med Sci. 2003;58(5):M436–40.
Julien D, Gauvin L, Richard L, Kestens Y, Payette H. Longitudinal associations between walking frequency and depressive symptoms in older adults: results from the VoisiNuAge study. J Am Geriatr Soc. 2013;61(12):2072–8.
Su C-C, Lee K-D, Yeh C-H, Kao C-C, Lin C-C. Measurement of physical activity in cancer survivors: a validity study. J Cancer Surviv. 2014;8(2):205–12.
Moored KD, Qiao Y, Boudreau RM, Roe LS, Cawthon PM, Cauley JA, et al. Prospective associations between physical activity and perceived fatigability in older men: differences by activity type and baseline marital status. J Gerontol A Biol Sci Med Sci. 2022;77(12):2498–506.
Li JX, Hodgson N, Lyons MM, Chen KC, Yu F, Gooneratne NS. A personalized behavioral intervention implementing mHealth technologies for older adults: a pilot feasibility study. Geriatr Nurs. 2020;41(3):313–9.
Chang VC, Do MT. Risk factors for falls among seniors: implications of gender. Am J Epidemiol. 2015;181(7):521–31.
Bernstein JP, Noland MD, Dorociak KE, Leese MI, Lee SY, Hughes A. Executive functioning predicts discrepancies between objective and self-reported physical activity in older adults: a pilot study. Aging Neuropsychol Cogn. 2023;30(1):124–34.
Boa Sorte Silva NC, Dao E, Hsu CL, Tam RC, Lam K, Alkeridy W, et al. Myelin and Physical Activity in Older Adults with Cerebral Small Vessel Disease and Mild Cognitive Impairment. The journals of gerontology Series A, Biological sciences and medical sciences. 2022;78(3):545–3.
Escher C, Asken BM, VandeBunte A, Fonseca C, You M, Kramer JH, et al. Roles of physical activity and diet in cognitive aging: is more better? The Clinical neuropsychologist. 2022;37(2):1–18.
Haggard AV, Tennant JE, Shaikh FD, Hamel R, Kline PW, Zukowski LA. Including cognitive assessments with functional testing predicts capabilities relevant to everyday walking in older adults. Gait Posture. 2023;100:75–81.
Ibrahim AM, Singh DKA, Mat S, Mat Ludin AF, Shahar S. Incidence and Predictors of Physical Inactivity Among Malaysian Community-Dwelling Older Persons. Journal of aging and physical activity. 2022;31(1):105–6.
Gregorio L, Brindisi J, Kleppinger A, Sullivan R, Mangano KM, Bihuniak JD, et al. Adequate dietary protein is associated with better physical performance among post-menopausal women 60–90 years. J Nutr Health Aging. 2014;18(2):155–60.
Nemmers TM, Miller JW. Factors influencing balance in healthy community-dwelling women age 60 and older. J Geriatr Phys Ther (2001). 2008;31(3):93–100.
McAuley E, Hall KS, Motl RW, White SM, Wojcicki TR, Hu L, et al. Trajectory of declines in physical activity in community-dwelling older women: social cognitive influences. J Gerontol B Psychol Sci Soc Sci. 2009;64(5):543–50.
McAuley E, Morris KS, Doerksen SE, Motl RW, Hu L, White SM, et al. Effects of change in physical activity on physical function limitations in older women: mediating roles of physical function performance and self-efficacy. J Am Geriatr Soc. 2007;55(12):1967–73.
Martin FC, Hart D, Spector T, Doyle DV, Harari D. Fear of falling limiting activity in young-old women is associated with reduced functional mobility rather than psychological factors. Age Ageing. 2005;34(3):281–7.
Morris KS, McAuley E, Motl RW. Neighborhood satisfaction, functional limitations, and self-efficacy influences on physical activity in older women. Int J Behav Nutr Phys Act. 2008;5:13.
Legg HS, Arnold CM, Trask C, Lanovaz JL. Does functional performance and upper body strength predict upper extremity reaction and movement time in older women? Hum Mov Sci. 2021;77:102796.
Leis KS, Reeder BA, Chad KE, Spink KS, Fisher KL, Bruner BG. The relationship of chronic disease and demographic variables to physical activity in a sample of women aged 65 to 79 years. Women Health. 2010;50(5):459–74.
Liu-Ambrose T, Khan KM, Eng JJ, Lord SR, McKay HA. Balance confidence improves with resistance or agility training - Increase is not correlated with objective changes in fall risk and physical abilities. Gerontology. 2004;50(6):373–82.
Lange AK, Singh MAF, Smith RM, Foroughi N, Baker MK, Shnier R, et al. Degenerative meniscus tears and mobility impairment in women with knee osteoarthritis. Osteoarthritis Cartilage. 2007;15(6):701–8.
Greenspan SL, Resnick NM, Parker RA. The effect of hormone replacement on physical performance in community-dwelling elderly women. Am J Med. 2005;118(11):1232–9.
Newton RA, Cromwell RL, Rogers HL. The relationship between physical performance and obesity in elderly African-American women. Phys Occup Ther Geriatr. 2009;27(6):423–40.
Talley KMC, Wyman JF, Gross CR, Lindquist RA, Gaugler JE. Change in balance confidence and its associations with increasing disability in older community-dwelling women at risk for falling. J Aging Health. 2014;26(4):616–36.
Kenny AM, Kleppinger A, Wang Y, Prestwood KM. Effects of ultra-low-dose estrogen therapy on muscle and physical function in older women. J Am Geriatr Soc. 2005;53(11):1973–7.
Bellantonio S, Fortinsky R, Prestwood K. How well are community-living women treated for osteoporosis after hip fracture? J Am Geriatr Soc. 2001;49(9):1197–204.
Klima DW. Physical performance and balance confidence among community-dwelling older adult men. 2010. (Ph.D.). p. 159.
Eendebak RJAH, Ahern T, Swiecicka A, Pye SR, O’Neill TW, Bartfai G, et al. Elevated luteinizing hormone despite normal testosterone levels in older men-natural history, risk factors and clinical features. Clin Endocrinol. 2018;88(3):479–90.
Laddu D, Parimi N, Cauley JA, Cawthon PM, Ensrud KE, Orwoll E, et al. The association between trajectories of physical activity and all-cause and cause-specific mortality. J Gerontol A Biol Sci Med Sci. 2018;73(12):1708–13.
Lange-Maia BS, Cauley JA, Newman AB, Boudreau RM, Jakicic JM, Glynn NW, et al. Sensorimotor peripheral nerve function and physical activity in older men. J Aging Phys Act. 2016;24(4):559–66.
Mackey DC, Hubbard AE, Cawthon PM, Cauley JA, Cummings SR, Tager IB. Usual physical activity and hip fracture in older men: an application of semiparametric methods to observational data. Am J Epidemiol. 2011;173(5):578–86.
Cousins JM, Petit MA, Paudel ML, Taylor BC, Hughes JM, Cauley JA, et al. Muscle power and physical activity are associated with bone strength in older men: the osteoporotic fractures in men study. Bone. 2010;47(2):205–11.
Mesinovic J, Scott D, Seibel MJ, Cumming RG, Naganathan V, Blyth FM, et al. Risk factors for incident falls and fractures in older men with and without type 2 diabetes mellitus: the Concord Health and Ageing in Men Project. J Gerontol A Biol Sci Med Sci. 2021;76(6):1090–100.
Hsu B, Merom D, Blyth FM, Naganathan V, Hirani V, Le Couteur DG, et al. Total physical activity, exercise intensity, and walking speed as predictors of all-cause and cause-specific mortality over 7 years in older men: the Concord Health and Aging in Men Project. J Am Med Dir Assoc. 2018;19(3):216–22.
Ng CA, Scott D, Seibel MJ, Cumming RG, Naganathan V, Blyth FM, et al. Higher Impact Physical Activity is Associated with Maintenance of Bone Mineral Density but Not Reduced Incident Falls or Fractures in Older Men: The Concord Health and Ageing in Men Project. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research. 2020;36(4):662–72.
Cronholm F, Rosengren BE, Nilsson J, Ohlsson C, Mellstrom D, Ribom E, et al. The fracture predictive ability of a musculoskeletal composite score in old men - data from the MrOs Sweden study. BMC Geriatr. 2019;19(1):90.
Kenny AM, Biskup B, Robbins B, Marcella G, Burleson JA. Effects of vitamin D supplementation on strength, physical function, and health perception in older, community-dwelling men. J Am Geriatr Soc. 2003;51(12):1762–7.
Kenny AM, Prestwood KM, Kenny AM, Prestwood KM, Marcello KM, Raisz LG. Determinants of bone density in healthy older men with low testosterone levels. J Gerontol A Biol Sci Med Sci. 2000;55(9):M492–7.
Liu PY, Wishart SM, Handelsman DJ. A double-blind, placebo-controlled, randomized clinical trial of recombinant human chorionic gonadotropin on muscle strength and physical function and activity in older men with partial age-related androgen deficiency. J Clin Endocrinol Metab. 2002;87(7):3125–35.
Bonnefoy M, Normand S, Pachiaudi C, Lacour JR, Laville M, Kostka T. Simultaneous validation of ten physical activity questionnaires in older men: a doubly labeled water study. J Am Geriatr Soc. 2001;49(1):28–35.
Granger C, Parry S, Denehy L, Granger CL, Parry SM. The self-reported Physical Activity Scale for the Elderly (PASE) is a valid and clinically applicable measure in lung cancer. Support Care Cancer. 2015;23(11):3211–8.
Oliveira CC, McGinley J, Lee AL, Irving LB, Denehy L. Fear of falling in people with chronic obstructive pulmonary disease. Respir Med. 2015;109(4):483–9.
Tao Y-X, Wang L, Dong X-Y, Zheng H, Zheng Y-S, Tang X-Y, et al. Psychometric properties of the Physical Activity Scale for the Elderly in Chinese patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:105–14.
Burns JM, Mayo MS, Anderson HS, Smith HJ, Donnelly JE. Cardiorespiratory fitness in early-stage Alzheimer disease. Alzheimer Dis Assoc Disord. 2008;22(1):39–46.
Farina N, Tabet N, Rusted J. Habitual physical activity (HPA) as a factor in sustained executive function in Alzheimer-type dementia: a cohort study. Arch Gerontol Geriatr. 2014;59(1):91–7.
Lin YP, Yang YH, Hsiao SF. Physical activity, muscle strength, and functional fitness: comparing older adults with and without Alzheimer dementia. Top Geriatr Rehabil. 2019;35(4):280–8.
Talamonti D, Gagnon C, Vincent T, Nigam A, Lesage F, Bherer L, et al. Exploring cognitive and brain oxygenation changes over a 1-year period in physically active individuals with mild cognitive impairment: a longitudinal fNIRS pilot study. BMC Geriatr. 2022;22(1):648.
van Santen J, Droes RM, Twisk JWR, Henkemans OAB, van Straten A, Meiland FJM. Effects of exergaming on cognitive and social functioning of people with dementia: a randomized controlled trial. J Am Med Dir Assoc. 2020;21(12):1958-#x0002B;
El Rahi B, Shatenstein B, Morais JA. The joint effects of diet quality and physical activity on functional decline among diabetic older adults from the NuAge cohort. J Am Geriatr Soc. 2013;61(SUPPL. 1):S209.
Rahi B, Morais JA, Gaudreau P, Payette H, Shatenstein B. Decline in functional capacity is unaffected by diet quality alone or in combination with physical activity among generally healthy older adults with T2D from the NuAge cohort. Diabetes Res Clin Pract. 2014;105(3):399–407.
Sazlina S-G, Browning CJ, Yasin S. Effectiveness of personalized feedback alone or combined with peer support to improve physical activity in sedentary older Malays with type 2 diabetes: a randomized controlled trial. Front Public Health. 2015;3:178.
Barker KL, Room J, Knight R, Dutton S, Toye F, Leal J, et al. Home-based rehabilitation programme compared with traditional physiotherapy for patients at risk of poor outcome after knee arthroplasty: the CORKA randomised controlled trial. BMJ Open. 2021;11(8):e052598.
Batsis JA, Zbehlik AJ, Barre LK, Bynum JPW, Pidgeon D, Bartels SJ. Impact of obesity on disability, function, and physical activity: data from the Osteoarthritis Initiative. Scand J Rheumatol. 2015;44(6):495–502.
Bennell KL, Ahamed Y, Jull G, Bryant C, Hunt MA, Forbes AB, et al. Physical therapist-delivered pain coping skills training and exercise for knee osteoarthritis: randomized controlled trial. Arthritis Care Res. 2016;68(5):590–602.
Bieler T, Anderson T, Beyer N, Rosthoj S. The impact of self-efficacy on activity limitations in patients with hip osteoarthritis: results from a cross-sectional study. ACR Open Rheumatol. 2020;2(12):741–9.
Chmelo E, Nicklas B, Davis C, Legault C, Miller GD, Messier S. Physical activity and physical function in older adults with knee osteoarthritis. J Phys Act Health. 2013;10(6):777–83.
Dunlop DD, Semanik P, Song J, Sharma L, Nevitt M, Jackson R, et al. Moving to maintain function in knee osteoarthritis: evidence from the Osteoarthritis Initiative. Arch Phys Med Rehabil. 2010;91(5):714–21.
Hinman RS, Wrigley TV, Metcalf BR, Campbell PK, Paterson KL, Hunter DJ, et al. Unloading shoes for self-management of knee osteoarthritis: a randomized trial. Ann Intern Med. 2016;165(6):381–9.
McDonald DD, Shellman JM, Graham L, Harrison L. The relationship between reminiscence functions, optimism, depressive symptoms, physical activity, and pain in older adults. Res Gerontol Nurs. 2016;9(5):223–31.
Sharma L, Cahue S, Song J, Hayes K, Pai Y, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70.
Skou ST, Wise BL, Lewis CE, Felson D, Nevitt M, Segal NA. Muscle strength, physical performance and physical activity as predictors of future knee replacement: a prospective cohort study. Osteoarthritis Cartilage. 2016;24(8):1350–6.
Smith TO, Mansfield M, Dainty J, Hilton G, Mann CJV, Sackley CM. Does physical activity change following hip and knee replacement? Matched case-control study evaluating Physical Activity Scale for the Elderly data from the Osteoarthritis Initiative. Physiotherapy. 2018;104(1):80–90.
Amara AW, Chahine L, Seedorff N, Caspell-Garcia CJ, Coffey C, Simuni T, et al. Self-reported physical activity levels and clinical progression in early Parkinson’s disease. Parkinsonism Relat Disord. 2019;61:118–25.
Ånfors S, Kammerlind A-S, Nilsson MH. Test-retest reliability of physical activity questionnaires in Parkinson’s disease. BMC Neurol. 2021;21(1):1–13.
Ashburn A, Pickering R, McIntosh E, Hulbert S, Rochester L, Roberts HC, et al. Exercise- and strategy-based physiotherapy-delivered intervention for preventing repeat falls in people with Parkinson’s: the PDSAFE RCT. Health Technol Assess (Winchester, England). 2019;23(36):1–150.
Balci B, Aktar B, Buran S, Tas M, Colakoglu BD. Impact of the COVID-19 pandemic on physical activity, anxiety, and depression in patients with Parkinson’s disease. Int J Rehabil Res. 2021;44(2):173–6.
Bryant MS, Hou JG, Collins RL, Protas EJ. Contribution of axial motor impairment to physical inactivity in Parkinson disease. Am J Phys Med Rehabil. 2016;95(5):348–54.
Bryant MS, Kang GE, Protas EJ. Relation of chair rising ability to activities of daily living and physical activity in Parkinson’s disease. Arch Physiother. 2020;10(1):22.
Bryant MS, Rintala DH, Hou J-G, Protas EJ. Relationship of falls and fear of falling to activity limitations and physical inactivity in Parkinson’s disease. J Aging Phys Act. 2015;23(2):187–93.
Ellis T, Cavanaugh JT, Earhart GM, Ford MP, Foreman KB, Fredman L, et al. Factors associated with exercise behavior in people with Parkinson disease. Phys Ther. 2011;91(12):1838–48.
Mantri S, Wood S, Duda JE, Morley JF. Understanding physical activity in Veterans with Parkinson disease: a mixed-methods approach. Parkinsonism Relat Disord. 2019;61:156–60.
Mantri S, Wood S, Duda JE, Morley JF. Comparing self-reported and objective monitoring of physical activity in Parkinson disease. Parkinsonism Relat Disord. 2019;67:56–9.
Allison MJ, Keller C, Hutchinson PL. Selection of an instrument to measure the physical activity of elderly people in rural areas. Rehabil Nurs. 1998;23(6):309–14.
Dinger MK, Oman F, Taylor EL, Vesely SK, Able J. Stability and convergent validity of the Physical Activity Scale for the Elderly (PASE). J Sports Med Phys Fitness. 2004;44(2):186–92.
Ismail N, Hairi F, Choo WY, Hairi NN, Peramalah D, Bulgiba A. The Physical Activity Scale for the Elderly (PASE): validity and reliability among community-dwelling older adults in Malaysia. Asia Pac J Public Health. 2015;27(8 Suppl):62S-72S.
Singh DKA, Rahman NNAA, Rajaratnam BS, Yi TC, Shahar S. Validity and reliability of physical activity scale for elderly in Malay language (PASE-M). Malays J Public Health Med. 2018;2018(Specialissue1):116–23.
Alqarni AM, Vennu V, Alshammari SA, Bindawas SM. Cross-cultural adaptation and validation of the Arabic version of the Physical Activity Scale for the Elderly among community-dwelling older adults in Saudi Arabia. Clin Interv Aging. 2018;13:419–27.
Ngai SP, Cheung RT, Lam PL, Chiu JK, Fung EY. Validation and reliability of the Physical Activity Scale for the Elderly in Chinese population. J Rehabil Med. 2012;44(5):462–5.
Covotta A, Gagliardi M, Berardi A, Maggi G, Pierelli F, Mollica R, et al. Physical Activity Scale for the Elderly: Translation, Cultural Adaptation, and Validation of the Italian Version. Current Gerontology & Geratrics Research. 2018;8294568:1–7.
Loland NW. Reliability of the physical activity scale for the elderly (PASE). Eur J Sport Sci. 2002;2(5):1–12.
Keikavoosi-Arani L, Salehi L. Cultural adaptation and psychometric adequacy of the Persian version of the physical activity scale for the elderly (P-PASE). BMC Res Notes. 2019;12(1):555.
Wisniowska-Szurlej A, Cwirlej-Sozanska A, Woloszyn N, Sozanski B, Wilmowska-Pietruszynska A, Washburn R. Cultural adaptation and validation of the Polish version of the physical activity scale for older people living in a community: a cross-sectional study. Eur Rev Aging Phys Act. 2020;17(1):19.
Wu C-Y, Su T-P, Fang C-L, Yeh CM. Sleep quality among community-dwelling elderly people and its demographic, mental, and physical correlates. J Chin Med Assoc. 2012;75(2):75–80.
Ayvat E, Kilinc M, Kirdi N. The Turkish version of the Physical Activity Scale for the Elderly (PASE): its cultural adaptation, validation, and reliability. Turk J Med Sci. 2017;47(3):908–15.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27(5):1147–57.
Okoye EC, Akosile CO, Maruf FA, Onwuakagba IU, Chukwuma VC. Cross-cultural adaptation and validation of Nigerian (Igbo) version of the physical activity scale for the elderly. J Aging Phys Act. 2021;29(4):553–61.
D’Amore C, Saunders S, Bhatnagar N, Griffith LE, Richardson J, Beauchamp MK. Determinants of physical activity in community-dwelling older adults: an umbrella review. Int J Behav Nutr Phys Act. 2023;20(1):135.
Terwee CB, Prinsen CAC, Chiarotto A, Westerman MJ, Patrick DL, Alonso J, et al. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res. 2018;27(5):1159–70.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–95.
Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. 2013;13(1):449.
Aleksovska K, Puggina A, Giraldi L, Buck C, Burns C, Cardon G, et al. Biological determinants of physical activity across the life course: a “Determinants of Diet and Physical Activity” (DEDIPAC) umbrella systematic literature review. Sports Med Open. 2019;5(1):2.
Acknowledgements
Ms. Neera Bhatnagar, a librarian at Health Sciences Library at McMaster University, for guiding the authors in the development of the search strategy.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MB and CD conceptualized the research question; LL, NB, SH, JL, IV in consultation with Ms Bhatnagar and CD, QH, and MB created protocol and search strategies. NB, LL, SH, JL, IV and CD carried out screening and extracting papers. JL, CD and QH carried out analyses and all authors contributed to the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Author MB is supported by a Tier 2 Canada Research Chair in Mobility, Aging and Chronic Disease.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
D’Amore, C., Lajambe, L., Bush, N. et al. Mapping the extent of the literature and psychometric properties for the Physical Activity Scale for the Elderly (PASE) in community-dwelling older adults: a scoping review. BMC Geriatr 24, 761 (2024). https://doi.org/10.1186/s12877-024-05332-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05332-3