Abstract
Background
The objective of this study is to evaluate the global burden of ischemic heart disease (IHD) attributable to High body mass index (HBMI) by utilizing data from Global Burden of Disease (GBD) 2019.
Methods
This study utilized data from the GBD 2019 to examine the impact of HBMI on deaths and disability-adjusted life years (DALYs). The analysis focused on age-standardized rates and considered a 30-year time frame. Trends were assessed using estimated annual percentage changes (EAPCs).
Results
Since 1990, a significant global increase in IHD attributable to HBMI has been observed. This increase is particularly notable among elderly males and in regions with low-middle Socio-Demographic Index (SDI), such as Central Asia and Eastern Europe. In 2019, IHD globally resulted in 1,662,339 deaths and 41,369,773 DALYs. Despite the high age-standardized death rate (20.73 per 100,000) and DALY rate (499.41 per 100,000), a declining trend was noted. This trend is reflected by the EAPCs of -0.35 for DALYs and − 0.67 for deaths. Notably, males and middle SDI countries exhibited higher rates of IHD, whereas high SDI regions such as High-income Asia Pacific and Western Europe showed decreasing trends in IHD.
Conclusion
Over the past three decades, there has been a significant increase in IHD caused by HBMI, especially in low-middle and low SDI regions. This highlights the importance of targeted interventions in addressing this issue. Notably, regions including Central Asia, Eastern Europe, North Africa, and the Middle East have been heavily affected.
Similar content being viewed by others
Background
Cardiovascular diseases (CVD) have been the leading cause of mortality worldwide for decades, with ischemic heart disease (IHD) being the most prevalent form and responsible for 16% of total global deaths. However, there are significant regional and national variations in the burden of IHD. This study seeks to evaluate the global burden of IHD linked to high body mass index (HBMI) by conducting a meticulous analysis spanning 30 years, from 1990 to 2019. The aim is to assess the extent to which HBMI contributes to the global burden of IHD.
Obesity, once defined by the HBMI, has reached epidemic proportions worldwide [1]. The new definition of obesity is based on the waist-to-height ratio [2]. This study primarily examined the HBMI as a measure of obesity, as the HBMI still has research value. HBMI is known to indirectly increase the risk of IHD through the development of hyperlipidemia, hypertension, diabetes, and related conditions [3]. HBMI has become a widely used metric in epidemiological studies and has reached pandemic levels globally in the past two decades [4]. The prevalence of obesity, a major contributor to Non-Communicable Diseases (NCDs) such as cardiovascular disease, cancer, chronic respiratory diseases, and diabetes, has alarmingly doubled since 1980 [5]. Presently, approximately one-third of the global population is classified as overweight or obese, with the number reaching 3 billion in 2019 [6]. This rise has been linked to over 5 million obesity-related deaths each year, primarily affecting adults aged 20 and above [7]. While previous research has established the association between HBMI and various cardiovascular outcomes, the specific impact on IHD risk yields varied findings [8].
Despite these insights, comprehensive data on the global burden of IHD attributable to HBMI, especially its temporal trends, remain limited. Accurate and up-to-date burden estimates are essential for guiding research, informing evidence-based strategies, and enhancing the effectiveness of efforts in IHD prevention and management.
Methods
Data source
Our study utilized data from the Global Burden of Disease Study 2019 (GBD 2019) to analyze the global impact of IHD attributable to HBMI. The GBD 2019 provides comprehensive assessments of health loss for 329 diseases in 204 countries and territories. These entities are categorized into 21 regions based on epidemiological and geographical considerations [9]. Furthermore, these regions are stratified into five Socio-Demographic Index (SDI) categories: high (> 0.81), high-middle (0.70–0.81), middle (0.61–0.69), low-middle (0.46–0.60), and low (< 0.46) [10]. For our analysis, we thoroughly examined data from 1990 to 2019, with a specific focus on mortality, disability-adjusted life years (DALYs) [10], and age-standardized rates (ASRs) relevant to IHD. To discern global trends and implications of HBMI on IHD, we conducted a detailed analysis by age, location, and year. This study is based on a publicly available database and does not require ethical approval.
Defining HBMI and clinical diagnostic criteria for IHD
Within the HBMI classification, overweight is defined as a BMI ranging from 25.00 to 29.99 kg/m2, while obesity is defined as a BMI of ≥ 30.00 kg/m2 [11].
In the GBD 2019 analysis, IHD is classified as a ‘non-communicable disease’ and a ‘cardiovascular disease’, specifically as a level 3 cause with the code B.2.2. To identify cases of IHD, the study uses the International Classification of Diseases, Ninth Revision (ICD-9) codes 410-414.9 and Tenth Revision (ICD-10) codes I20–I25.9 [12]. This comprehensive approach covers various conditions, including acute myocardial infarction, chronic IHD and chronic stable angina, in accordance with the Fourth Universal Definition of Myocardial Infarction and the Rose Angina Questionnaire [13]. Moreover, premature mortality from IHD is defined as deaths occurring before the age of 55 in men and 65 in women, following international guidelines [14].
Statistical analyses
To account for differences in age structure and to provide a more precise assessment of the burden of IHD associated with HBMI, we utilized age-standardized rates in our analysis [15]. By adjusting for variations in age distribution, this methodology allows for a more accurate understanding of the IHD burden related to HBMI. To examine the temporal trends of these age-standardized rates from 1990 to 2019, we employed annual percent change (EAPC) analysis. A linear regression model, ln(ASR) = α + βX + ε, where ‘X’ represents the calendar year, was used to assess trends. The EAPC and its 95% confidence interval (CI) were determined using the formula: 100 × (exp(β) − 1). Trends were considered stable if the 95% CI of the EAPC included 0 (P ≥ 0.05); otherwise, they were classified as either increasing (EAPC and its 95% CI > 0) or decreasing (EAPC and its 95% CI < 0). This robust analytical approach improves our understanding of the IHD burden associated with HBMI, taking into account epidemiological and socio-demographic factors. For more comprehensive insights, we direct readers to the GBD Compare visualization tool (https://vizhub.healthdata.org/gbd-compare/) and the GBD Results Tool (http://ghdx.healthdata.org/gbd-results-tool) [11].
Result
Evolving global impact of IHD related to HBMI (1990–2019)
From 1990 to 2019, there was a notable global rise in the prevalence of IHD associated with HBMI. During this time period, there was a significant increase of 192.84% in deaths and a 195.76% increase in DALYs caused by HBMI-related IHD, as shown in Table 1. Differences in this trend based on gender were evident, with a 207.21% increase in deaths among men compared to a 177.92% increase among women. Conversely, the rise in DALYs was more substantial in women (55.41%) than in men (48.28%) during the same timeframe, as illustrated in Table 1.
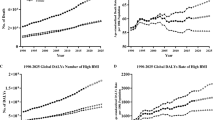
The age-standardized death rate of IHD witnessed a global decline, dropping from 23.75 per 100,000 in 1990 to 20.73 per 100,000 in 2019 (Figure S2; Table 2). This downward trend was also observed in the age-standardized death and DALY rates (Figure S2).The global age-standardized DALY rate decreased from 521.77 per 100,000 in 1990 to 499.41 per 100,000 in 2019 (Table 1; Figure S1 B and Figure S2). Although there was a slight decrease in the global age-standardized death rate of IHD from 23.75 per 100,000 in 1990 to 20.73 per 100,000 in 2019, these rates exhibited an overall decline over the three-decade period, as indicated by EAPC values of -0.35 (-0.43, -0.27) for DALYs and − 0.67 (-0.75, -0.60) for deaths (Table 1; Fig. 1; Supplementary Table 6).
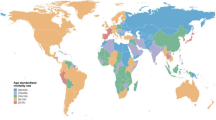
The Global Burden of ischemic heart disease attributable to high body-mass index: age-standardized DALY rate and ASDR in 1990 and 2019: (A) ASDR in 1990; (B) age-standardized DALY rate in 1990; (C) ASDR in 2019; (D) age-standardized DALY rate in 2019; (E) EAPCs of ASDR; (F) EAPCs of age-standardized DALY rate. ASRs = age-standardized rates. ASDR = age-standardized Death rate. DALY = disability adjusted life-year. EAPCs = Estimated Annual Percentage Changes
Regional and national variations in IHD Burden due to high BMI
The analysis of IHD attributable to HBMI at a regional level revealed striking contrasts. Australasia experienced the most pronounced decrease in the age-standardized DALY rate, with an EAPC of -3.98. Conversely, South Asia saw the steepest rise in this measure, with an EAPC of 3.09. In terms of the ASDR, Australasia again reported the largest decline, with an EAPC of -3.89, while East Asia witnessed a significant increase with an EAPC of 2.98 (Table 1; Supplementary Table 1; Fig. 1 and Figure S1).
In 2019, the region of Central Asia recorded the highest observed rates of DALY and deaths linked to IHD resulting from exposure to HBMI (Supplementary Table 1). Since 1990, South Asia has witnessed the most substantial increase in the age-standardized DALY rate for HBMI-attributable IHD, while East Asia has experienced a significant rise in ASDR (Figure S1 A, Figure S1 B, and Supplementary Table 2). Conversely, high-income regions such as Asia Pacific, Western Europe, and Australasia have demonstrated noteworthy decreases in both age-standardized death and DALY rates associated with IHD and HBMI over the past three decades (Supplementary Table 4; Supplementary Table 5).
At the national level, Uzbekistan and Nauru reported the highest ASDR and DALY rates due to HBMI in 2019, respectively. Meanwhile, Japan exhibited the lowest rates in both categories. Over the span of 30 years, Mozambique experienced the most significant increases in both ASDR and age-standardized DALY rates attributable to HBMI exposure. These findings are detailed in Table 3, Supplementary Table 2, Figure S1 A, and Figure S1 B. In contrast, Israel, Denmark, and the Netherlands showed the most substantial decreases in these rates, as indicated in Table 3, Supplementary Table 2, Supplementary Table 3, Figure S1 A, and Figure S1 B.
Age and gender disparities in the Burden of IHD related to HBMI
Age-specific analysis revealed significant variations in deaths and DALYs. Globally, there were notable differences in the percentages of deaths and DALYs across different age groups. The highest number of deaths, both in males and females, was observed in the 60–69 age group, while the age-standardized rate peaked in the 95 + age group. Similarly, the counts of DALYs and age-standardized rates increased with age. In terms of DALYs, both sexes had the highest peak in the 60–64 age group, with the highest age-standardized rate in the 95 + age group. The age-standardized rates clearly indicate that the burden of IHD (both in terms of deaths and DALYs) is significantly higher in older age groups, highlighting the importance of age as a risk factor for IHD (Table 4).
In terms of deaths and DALYs, men across all age groups were found to carry a greater burden of IHD compared to women (Table 2). The impact of HBMI on the burden of IHD was observed to increase more rapidly in males, with the ASDR exhibiting an EAPC of -0.36 (95% CI: -0.42 to -0.29) for males, and a corresponding EAPC of -0.97 (95% CI: -1.05 to -0.88) for females. Likewise, the EAPC for the male age-standardized DALY rate was − 0.11 (95% CI: -0.18 to -0.04), which was higher compared to the female rate of -0.65 (95% CI: -0.74 to -0.56) (Table 1; Figure S3).
Socio-demographic influences on IHD Burden Linked to HBMI
The relationship between the SDI and the burden of IHD caused by HBMI is complex and can vary. It is worth noting that the regions with the highest rates of DALYs and deaths due to IHD attributed to HBMI are the high-middle SDI regions, followed closely by the middle SDI regions. On the other hand, the regions with the lowest DALY rates are the high SDI and low SDI regions, with the lowest death rates specifically seen in the high SDI regions (Table 1; Figure S2; Figure S4).
This pattern demonstrates a worldwide rise in the number of deaths and DALYs linked to HBMI. Interestingly, regions with high-middle and high SDI demonstrate a decrease in age-standardized rates, indicating the effectiveness of management and intervention strategies. In contrast, regions with low-middle, low, and middle SDI experience an increase in these rates, emphasizing the ongoing public health challenges in addressing the impact of HBMI on IHD.
Discussion
Our global analysis spanning a period of 30 years and encompassing 204 countries and regions uncovered significant variations in the burden of IHD attributed to HBMI in 2019. Notably, Central Europe, Eastern Europe, and Central Asia, as well as South Asia, reported higher death rates, underscoring the persistent challenge in effectively managing IHD in these areas. Conversely, high-income regions demonstrated the lowest rates in 2019, suggesting that their healthcare systems have been successful in addressing IHD. The data affirms the existence of notable regional disparities in the burden of IHD. High-income regions have achieved a reduction in IHD death rates by virtue of their superior healthcare systems, reduction in modifiable risk factors [16]. In contrast, regions such as Sub-Saharan Africa, Southeast Asia, East Asia, Oceania, and South Asia have experienced increased death rates, potentially influenced by factors like evolving economies leading to lifestyle changes, escalating urbanization, and potentially limited accessibility and quality of healthcare [16, 17]. Despite some improvements, Central Europe, Eastern Europe, and Central Asia continue to bear relatively high death rates from IHD, indicative of ongoing public health challenges [18, 19]. The disparate trends observed across regions underscore the necessity for region-specific approaches in combating IHD, which take into account local health systems, socio-economic circumstances, and lifestyle patterns [20]. Furthermore, the escalating trends in low- and middle-income regions emphasize the need for targeted focus on preventive healthcare, public awareness, and more effective management of risk factors such as diet, physical activity, and tobacco use [21].
Our analysis of the burden of IHD in relation to HBMI shows notable age-related differences, with a substantial increase in both deaths and DALYs with increasing age. This is similar to a previous study [22]. The most significant burden is observed in the 60–69 age group, and it sharply escalates in individuals over the age of 95. This pattern highlights the importance of age as a key determinant of the prevalence and severity of IHD, while also emphasizing the need for healthcare strategies that are tailored to specific age groups, especially older populations [23].
Men of all ages bear a higher burden of IHD than women, as reflected in both mortality and DALYs. This is similar to previous studies [24, 25]. This gender difference is further highlighted by the distinct trends seen in age-standardized rates, as indicated by the EAPC. The EAPC for male age-standardized death rates stand at -0.36, suggesting a slower decline compared to females (-0.97). Similarly, the EAPC for male age-standardized DALY rates is -0.11, contrasting with − 0.65 for females. These disparities in IHD burden between genders are likely influenced by a complex interplay of biological, lifestyle, and socio-economic factors, as well as differential access to healthcare and health-seeking behaviors [23].
Our study highlights the urgent need for comprehensive public health strategies and medical interventions tailored to the specific challenges of IHD in different age groups and genders [26]. The findings highlight an important avenue for future research aimed at understanding the factors contributing to gender differences in IHD [27]. Such knowledge is essential for the development of more precise, targeted prevention and treatment approaches, particularly those designed to address the challenges posed by ageing demographics and the specific health needs of different sexes.
Our analysis revealed differences in deaths and DALYs from IHD attributable to HBMI between SDI regions. In particular, a decrease in these indicators was observed in high and high-middle SDI regions, with significantly lower values in high SDI regions. This finding is similar to previous studies [28].This trend suggests that regions with higher socio-economic status are increasingly prioritizing health issues related to HBMI and implementing effective strategies to prevent and control IHD. In contrast, middle and low-middle SDI regions experienced a worsening trend in IHD burden due to HBMI, exacerbated by limited resources and inadequate healthcare infrastructure for widespread prevention and treatment of the disease. This disparity is particularly evident in rapidly growing and aging populations in these regions, emphasizing the urgent need for improved primary preventive efforts on a global scale [1].
Great efforts should be made to promote the prevention of obesity and its progression to IHD. Intake of simple sugars, complex carbohydrates and total calories should be reduced. Community prevention programmes should be implemented to improve relevant knowledge among the population in countries with a high IHD burden. Countries with a low SDI and an ageing population should promote healthcare. Possible government interventions could include mandatory calorie/nutrient menu labelling and regulation of food ingredients, as well as control of advertising and certain forms of taxation on beverages and foods [1].
In this study, we employed BMI as the primary indicator of body size [29]. Due to the change in the definition of obesity, there are limitations to the use of BMI as a measure of body size. In addition, BMI is a straightforward measure, it does have certain limitations, such as its inability to differentiate between lean body mass and adipose tissue. Nevertheless, BMI continues to be a valuable predictor of CVD and has demonstrated a non-linear association with mortality risk [30]. Other anthropometric measurements have also been investigated in relation to obesity-related outcomes, each offering distinct advantages and limitations.
The disparities in disease burden between developing and developed countries necessitate additional investigation. For the purposes of this paper, the geographical breakdown of the data is primarily based on the SDI classification of countries, and urban-rural and race data are missing, so it is not possible to explore further the differences in disease burden between factors such as urban-rural and race. Our study, which encompasses the largest epidemiological dataset on IHD to date, sought to accurately measure the burden of IHD caused by HBMI. Despite encountering challenges related to limited availability of high-quality epidemiological data and substantial regional variation, we employed standardized methodological criteria over a span of three decades to mitigate the impact of these limitations. We are confident that this approach has ensured a uniform quality of data across the included studies, thus offering a dependable overview of the global burden of IHD associated with HBMI.
Conclusion
Our findings showed that, globally, from 1990 to 2019, the disease burden of IHD in both deaths and DALYs attributable to HBMI have more than doubled in both sexes. However, after age-standardizing the HBMI-related DALY rates and Deaths rate, a decrease trend were noted in both sexes. This increasing trend emphasizes the utmost importance of prioritizing efforts to prevent overweight and obesity in all age groups, highlighting a significant global challenge in identifying the underlying causes of disparities and changing patterns in IHD burden. This is particularly pertinent when considering countries with different income levels. The insights gained from this study play a crucial role in guiding the development, implementation, and assessment of effective strategies aimed at preventing, managing, and rehabilitating IHD across diverse national contexts and population groups. Not only do these findings contribute to a broader understanding of IHD epidemiology, but they also provide a valuable framework for tailoring public health initiatives to mitigate the global impact of HBMI on IHD.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IHD:
-
ischemic heart disease
- GBD:
-
Global Burden of Disease
- DALYs:
-
disability-adjusted life years
- EAPCs:
-
estimated annual percentage changes
- SDI:
-
Socio-Demographic Index
- CVD:
-
Cardiovascular diseases
- HBMI:
-
high body mass index
- ASRs:
-
age-standardized rates
- ICD:
-
International Classification of Diseases
References
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Busetto L, Dicker D, Frühbeck G, Halford JCG, Sbraccia P, Yumuk V et al. A new framework for the diagnosis, staging and management of obesity in adults. Nat Med. 2024.
Guo X, Li J, Yin X, Zhang Z, Zhong Q, Zhu F. Trends in deaths and disability-adjusted life-years of stroke attributable to high body-mass index worldwide, 1990–2019. Front Neurol. 2023;14:1211642.
Ryan DH, Barquera S, Cavalcanti OB, Ralston J. The Global Pandemic of Overweight and Obesity. Handbook of Global Health. 2020.
Wagner KH, Brath H. A global view on the development of non communicable diseases. Prevent Med. 2012;54 Suppl:S38–41.
Nilson EAF, Gianicchi B, Ferrari G, Rezende LFM. The projected burden of non-communicable diseases attributable to overweight in Brazil from 2021 to 2030. Sci Rep. 2022;12(1):22483.
Sarma S, Sockalingam S, Dash S. Obesity as a multisystem disease: Trends in obesity rates and obesity-related complications. Diabetes Obes Metab. 2021;23(Suppl 1):3–16.
Mubarik S, Wang F, Malik SS, Shi F, Wang Y, Nawsherwan, et al. A hierarchical age-period-cohort analysis of breast cancer mortality and disability adjusted life years (1990-2015) attributable to modified risk factors among Chinese women. Int J Environ Res Public Health. 2020;17(4):1367.
Chen J, Wang C, Shao B. Global, regional, and national thyroid cancer age-period-cohort modeling and bayesian predictive modeling studies: a systematic analysis of the global burden of disease study 2019. Heliyon. 2023;9(11):e22490.
Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet (London England). 2020;396(10258):1204–22.
Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London England). 2018;392(10159):1923–94.
Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London England). 2018;392(10159):1789–858.
Aminorroaya A, Saeedi Moghaddam S, Tavolinejad H, Aryan Z, Heidari B, Ebrahimi H, et al. Burden of Ischemic Heart Disease and its attributable risk factors in North Africa and the Middle East, 1990 to 2019: results from the GBD Study 2019. J Am Heart Association. 2024;13(2):e030165.
Németh N, Boncz I, Pakai A, Elmer D, Horváth L, Pónusz R, et al. Inequalities in premature mortality from ischaemic heart disease in the WHO European region. Cent Eur J Public Health. 2023;31(2):120–6.
Liu Z, Jiang Y, Yuan H, Fang Q, Cai N, Suo C, et al. The trends in incidence of primary liver cancer caused by specific etiologies: results from the global burden of Disease Study 2016 and implications for liver cancer prevention. J Hepatol. 2019;70(4):674–83.
Alston LV, Peterson KL, Jacobs JP, Allender S, Nichols M. A systematic review of published interventions for primary and secondary prevention of ischaemic heart disease (IHD) in rural populations of Australia. BMC Public Health. 2016;16(1):895.
Kulshreshtha A, Goyal A, Dabhadkar K, Veledar E, Vaccarino V. Urban-rural differences in coronary heart disease mortality in the United States: 1999–2009. Public Health Rep. 2014;129(1):19–29.
Murphy A, Johnson CO, Roth GA, Forouzanfar MH, Naghavi M, Ng M, et al. Ischaemic heart disease in the former Soviet Union 1990–2015 according to the global burden of Disease 2015 study. Heart. 2018;104(1):58–66.
Movsisyan NK, Vinciguerra M, Medina-Inojosa JR, Lopez-Jimenez F. Cardiovascular diseases in Central and Eastern Europe: a call for more surveillance and evidence-based Health Promotion. Annals Global Health. 2020;86(1):21.
Sakamoto H, Rahman MM, Nomura S, Okamoto E, Koike S, Yasunaga H, et al. Japan Health System Review. 2018.
Budreviciute A, Damiati S, Sabir DK, Onder K, Schuller-Goetzburg P, Plakys G, et al. Management and Prevention Strategies for non-communicable diseases (NCDs) and their risk factors. Front Public Health. 2020;8:574111.
Yan W, Yan X, Mubarik S, Nawsherwan. Epidemiological trend and age-period-cohort effects on cardiovascular disease mortality and disability-adjusted life years attributable to dietary risks and high body mass index at the regional and country level across China and Pakistan. Front Nutr. 2023;10:1158769.
Fallon CK. Husbands’ hearts and women’s health: gender, Age, and Heart Disease in Twentieth-Century America. Bull Hist Med. 2019;93(4):577–609.
Yeh TL, Chen YR, Hsu HY, Tsai MC, Wu YC, Lo WC, et al. Cardiovascular Disease Burden Attributable to High Body Mass Index in Taiwan. Acta Cardiol Sinica. 2023;39(4):628–42.
Dong XJ, Zhang XQ, Wang BB, Hou FF, Jiao Y, Wang JG. The burden of cardiovascular disease attributable to high body mass index-an observational study. Eur Heart J Qual care Clin Outcomes. 2024;10(2):154–67.
Aggarwal NR, Patel HN, Mehta LS, Sanghani RM, Lundberg GP, Lewis SJ, et al. Sex differences in ischemic heart disease: advances, obstacles, and next steps. Circulation Cardiovasc Qual Outcomes. 2018;11(2):e004437.
Bhargava A, Arnold AP, Bangasser DA, Denton KM, Gupta A, Hilliard Krause LM, et al. Considering sex as a Biological Variable in Basic and Clinical studies: an endocrine Society Scientific Statement. Endocr Rev. 2021;42(3):219–58.
Li Z, Lin L, Wu H, Yan L, Wang H, Yang H, et al. Global, Regional, and National Death, and disability-adjusted life-years (DALYs) for Cardiovascular Disease in 2017 and trends and Risk Analysis from 1990 to 2017 using the global burden of Disease Study and implications for Prevention. Front Public Health. 2021;9:559751.
Wiedmann MKH, Brunborg C, Di Ieva A, Lindemann K, Johannesen TB, Vatten L, et al. The impact of body mass index and height on the risk for glioblastoma and other glioma subgroups: a large prospective cohort study. Neurooncology. 2017;19(7):976–85.
Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019.
Acknowledgements
We thank all authors for their contributions to the article and the GBD collaborators.
Funding
This study was funded by the Yuyao Science and Technology Bureau (grant number 2023YYB05).
Author information
Authors and Affiliations
Contributions
W.Y.: Conceptualization, Methodology, and Data curation. W.Y. and Y.H.: Writing-Original draft preparation; Y.H.: Writing- Reviewing and Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was based on a publicly available databases and does not require ethical approval. All of the participants or their legal representatives provided written informed consent during recruitment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yan, W., Hua, Y. Trends in deaths and disability-adjusted life-years of ischemic heart disease attributable to high body-mass index worldwide, 1990–2019. BMC Cardiovasc Disord 24, 482 (2024). https://doi.org/10.1186/s12872-024-04136-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-024-04136-y