Abstract
Background
Impaired vascular compliance is common among persons with HIV (PWH) and a risk factor for cardiovascular disease (CVD), though many studies documenting this are from regions with a high prevalence of overweight and obesity. The prevalence and characteristics of impaired vascular compliance among PWH with low body mass index (BMI) is not well described, particularly in sub-Saharan Africa (SSA) where the majority of PWH live, a low BMI is more common, and the burden of CVD is rising.
Aim
To assess non-invasive vascular compliance measurements, including augmentation index (AIX), pulse wave velocity (PWV) and pulse waveforms, in underweight, normal weight, and overweight PWH on long-term antiretroviral therapy (ART) in SSA.
Methods
A cross-sectional study among PWH on ART at the University Teaching Hospital in Lusaka, Zambia. All participants had been on a regimen of efavirenz, emtricitabine, and tenofovir disoproxil fumarate for five or more years. Carotid-femoral PWV (cfPWV), carotid-radial PWV (crPWV), and the corresponding augmentation indexes (cfAIX and crAIX), were measured in all participants, in addition to aortic pressure waveforms, classified as type A, B, C and D according to reflected wave timings and amplitude. Multiple linear regression assessed relationships between demographic and clinical factors with vascular measurement endpoints.
Results
Ninety one PWH on long-term ART were enrolled; 38 (42%) were underweight (BMI < 18.5 kg/m2), 43 (47%) were normal weight (18.5–24.9 kg/m2) and 10 (11%) were overweight (> 25 kg/m2). Median age was 41, 40 and 40 years, among the three groups, respectively, and the proportion of women increased with BMI level. Overweight participants had a 39% higher cfAIX compared to normal-weight participants, while being underweight was associated with 27% lower cfAIX, after adjusting for age, sex and blood pressure (P = 0.02 and P = 0.01, respectively), but measurements of cfPWV, crPWV and crAIX did not differ.
Conclusion
Underweight PWH in SSA had lower cfAIX measurements compared to normal weight individuals, indicating less arterial stiffness. However, similar cfPWV, crPWV and crAIX values among the underweight and overweight PWH suggest a low BMI may not confer substantial protection against impaired vascular compliance as a contributor to CVD risk among individuals on ART.
Similar content being viewed by others
Introduction
Globally, the prevalence of cardiovascular diseases (CVD) has tripled over the past two decades [1]. The risk of cardiovascular events, namely myocardial infarction, heart failure and stroke, among persons with HIV (PWH) is roughly two-fold higher compared to HIV-negative persons [1]. Increased cardiovascular risk in PWH is multifactorial and includes chronic innate and adaptive immune activation, dyslipidaemias, insulin resistance, and other factors [2,3,4]. Prior studies have also implicated impaired vascular compliance, or a reduced ability for blood vessel walls to expand and contract passively with changes in pressure [5], as a common finding in PWH and a possible mechanism contributing to this increased CVD risk. [2, 6]. The decrease in vascular compliance has been attributed to heightened inflammation, immune activation, oxidative stress, and insulin resistance in PWH [7,8,9,10,11] and linked to reduced bioavailability of endothelial nitric oxide (NO) [12]. However, there are few studies of vascular compliance among PWH in sub-Saharan Africa (SSA), a region with the highest burden of HIV, an increasing prevalence of CVD among PWH, and a high proportion of low body mass index (BMI) individuals frequently underrepresented in prior studies.
Non-invasive methods for measuring vascular compliance include flow-mediated dilation, a measure of endothelial function and smooth muscle response to hypoxia, and pulse wave velocity (PWV), a measure of arterial distensibility or stiffness. Many studies have shown that aortic stiffness, measured as the velocity at which ventricular contraction of the heart, propagate along the arterial tree (distance/time [m/s]), as measured by carotid-femoral pulse wave velocity (cfPWV), a gold standard for aortic stiffness [13], is an independent risk factor for cardiovascular events (both fatal or non fatal) and all-cause mortality [14]. A systematic review and meta-analysis of 17 longitudinal studies in the general population found an increase of 1 m/s in PWV is associated with a 14% increase in CVD events and a 15% increase in mortality [14]. Furthermore, PWV measurement can be incorporated into routine clinical assessments and maybe useful for risk stratification [15,16,17]. In addition to cfPWV, the carotid-radial pulse wave velocity (crPWV) and pulse pressure are independently associated with cardiovascular events [18, 19]. These non-invasive measures of arterial stiffness are calculated from the duration and features of the arterial pulse propagated from the carotid to the femoral or radial arteries [20].
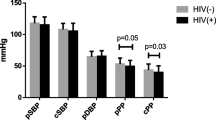
Additional parameters important to the assessment of vascular compliance include the central diastolic blood pressure (cDBP; the average minimal blood pressure value over one heartbeat), central pulse pressure (cPP; the maximal peak-to-peak amplitude of the pressure wave over one heartbeat), mean arterial pressure (MAP; the calculated average blood pressure value over one heartbeat), central systolic blood pressure (cSBP; the average blood pressure value during systole) and the augmentation pressure, or the increase in blood pressure induced by the early arrival of the reflected wave [21]. The augmentation index (AIX), the difference in the peak-to-peak amplitude of the pressure wave expressed as a percentage of pulse pressure, represents another important measure of vascular compliance [21, 22].
Impaired vascular function has emerged as an important contributor to CVD in studies of PWH from high resource countries with a relatively higher proportion of overweight and obese individuals[2, 6]. Most studies using non-invasive physiological measures of vascular function have reported impaired vascular compliance in overweight/obese PWH who are already at risk of CVD [10, 23]. Our group previously reported that lean PWH on ART for more than five years had increased arterial stiffness using the measure AIX [24]. However, reports of PWV measurements in PWH, especially lean individuals, have been inconsistent. While some studies show similar findings as in HIV-negative persons, others [25] show an increase in PWH [26]. Given the rising burden of CVD among individuals on long-term ART in SSA, where the majority of PWH reside [27], there is a critical need to understand cardiovascular risk factors specific to this region and population. Here, we assess whether underweight PWH on long term ART may have improved vascular compliance compared to normal weight and overweight individuals in Zambia, which could reflect a protective effect of low BMI for the development of CVD.
Materials and methods
We conducted a cross-sectional study among PWH on long-term ART at the University Teaching Hospital (UTH) in Lusaka, Zambia between September 2018 and June 2019. The sample size of 91 was estimated using Epi info version, based on the 11% prevalence of HIV in Zambia and 80% power. This sample size was calculated prior to the time of data collection [28]. Simple random sampling was used to select participants. All PWH had been on a regimen of efavirenz, emtricitabine, and tenofovir disoproxil fumarate for more than five years. Persons who were pregnant or with any known CVD, rheumatologic disease, diabetes, or any other active infectious conditions aside from HIV, or with current tobacco use were excluded. Sociodemographic data such as history of tobacco use, alcohol intake, sex and age were collected using the WHO STEPS questionnaire [29]. Height, recorded in centimeters, and weight, in kilograms, was measured using the micro T3 PW-BMI digital physician scale. While taking the measurement, participants were requested to remove footwear or head gear, have feet together, arms on the side while facing ahead. BMI was categorized as < 18.5 kg/m2 (underweight), 18.5–24.9 kg/m2 (normal), and > = 25.0 kg/m2 (overweight) [30].
Arterial stiffness measurements
PWV was measured at the femoral and radial sites, in addition to AIX, pulse waveforms and central blood pressures, using the ALAM Complior Analyse device (ALAM medical, France). Non-invasive probes were applied to the skin’s surface over the carotid, femoral and radial arteries with participants lying in a supine position and after resting for a minimum of five minutes in a quiet room. Participants wore minimal clothing, jewellery was removed, and telephones and other personal electronics were placed in a separate room. Participants were not allowed to move, speak, or sleep during the measurements [20]. All measurements were performed by the same operator and reported as cfPWV, crPWV, and carotid femoral AIX (cfAIX) and carotid radial AIX (crAIX).
Aortic pressure waves can be classified into Types A, B, C and D according to the reflected wave’s timing and amplitude from peripheral sites [13]. Types A and B occur when the systolic peak (P2) occurs in late systole after a clear inflexion point. AIX is calculated as the difference between P2 and the pressure at the systolic shoulder (P1), expressed as a percentage of the pulse pressure. In Type A, the AIX is higher than 12 per cent, whereas it is between 0 and 12 per cent in Type B [13]. Type C waves have inflexion points after the systolic peak. In contrast, in Type D, no inflexion point is measured because the reflected wave arrives in early systole and merges with the incident wave [13]. Types A and B are characteristic of impaired vascular compliance. Type C is characteristic of typical vascular function, whereas Type D is commonly observed in age-related arterial changes in the elderly [13].
Statistical analysis
Microsoft Excel (Microsoft, Redmond, Washington, USA) and STATA 14.2 (StataCorp LLC, College Station, Texas, USA) [31] were used for data analysis. To check the normality of the data, Q-Q plots were used and validated with the Shapiro–Wilk test. Homogeneity of variance was tested using Levene's test for one-way anova for endothelial function and BMI. The assumptions of normality and homoscedasticity of anova were not met, so the Kruskal Wallis test was used. Descriptive data were presented as medians and interquartile ranges for continuous variables and percentages for categorical variables. The relationships between various clinical and demographic factors across BMI categories were assessed using the Kruskal Wallis test. Univariate and multivariate linear regression were used to assess the relationships of endothelial function (crPWV, cfPWV, crAiX, and cfAiX) with sex, age and BMI category, as well as SBP, DBP, and MAP. P ≤ 0.05 was considered statistically significant [32].
Results
Ninety one adult participants, comprised of 57 females and 34 males, were enrolled in the study; 38 participants (42%) were underweight, 43 (47%) normal weight and 10 (11%) overweight. The median ages were 41, 40 and 40 years, respectively (Table 1). Median central blood pressure measurements were also comparable across BMI categories and no significant differences were observed. A summary of the data is shown in Table 1.
Overweight participants had a 39% higher cfAIX compared to normal-weight participants after adjusting for age, sex and blood pressure and other factors (p > 0.02), while being underweight was associated with a 27% lower cfAIX (P = 0.01). None of the other demographic, anthropometry and hemodynamic parameters were significantly associated with cfPWV (Table 2).
Table 3 shows the regression analysis of crPWV and crAIX. A unit increase in central diastolic blood pressure was associated with a 0.16 m/s increase in arterial stiffness as measured by crPWV (P = 0.03) when adjusted for other variables in the study. None of the other factors was significantly associated with crAIX.
Waveform analysis
Table 4 shows the waveform distribution across BMI categories. The predominant waveform in all three BMI categories was type A, followed by type B. Overall, there was no significant difference in the waveforms between BMI categories (P value = 0.08).
Discussion
In a cohort of PWH on a single ART regimen in Zambia, we found that PWH on long-term ART across BMI strata had similar measurements of both carotid-radial and carotid-femoral pulse wave velocities and augmentation indexes, suggesting a lower BMI may not offer substantial protection against impaired vascular compliance. Further, most participants had an AIX above 0%, which suggests that underweight PWH have a similar vascular phenotype as overweight PWH. A concordant relationship has been reported between augmentation index and pulse wave velocity in those at high risk of impaired vascular compliance [33, 34]. However, due to lack of a HIV negative control group, this could not be determined. We found that nearly all participants had either Type A or B waveforms, which represent the return of the reflective wave in systole instead of diastole [13]. Type C waveforms, considered desirable, (AIX < 0%) represent a return to the ascending aorta after ventricular ejection has ceased. However, typical in A and B waveforms, increases in the AIX cause decrease in the diastolic coronary pressure. These, typical in hypertensive patients, are characterised by increased ventricular afterload and increased myocardial workload and mass. Studies have also shown that the less compliant proximal arteries reduce the pressure gradient of proximal arteries to distal arteries. This may cause increased pressure in the microcirculatory system, a condition that could be harmful to areas of the brain and kidneys [35,36,37].
Vascular compliance measurements are modulated by vasomotor tone which is determined, in part, by endothelial function, the sympathetic nervous system and the renin angiotensin aldosterone system [38]. Our study reported no univariate differences in the haemodynamic parameters measured. Further, our result ranges are similar to other studies [39]. Further, increases in diastolic blood pressures were associated with increases in carotid radial pulse wave velocity. However, decreases in the bioavailability of nitric oxide can modulate vascular compliance independent of increases in the blood pressure [40, 41]. Thus, investigations are needed to determine the influence that sympathetic tone may have on aortic stiffness [38].
Long-term ART exposure has been associated with increased visceral fat and increasing CVD risk [42,43,44]. The association between ART and weight gain is yet to be determined but has been attributed to off target effects of the treatment [45]. The disposition of fat in central parts of the body increases one’s risk of cardiovascular disease [46]. Our study reported no significant differences in the waist hip ratio among groups. Further, using cfAIX, our results show that increased body mass is likely to increase the AIX and represent impaired vascular compliance while controlling for other variables. Indeed, obesity is a known risk factor for CVD, potentially mediated by endothelial dysfunction [47, 48]. Among the underweight, using cfAIX, our results show that an increase in body mass may decrease the AIX, restoring vascular compliance after controlling for other variables. This is similar to what Kumar and Samaras [49] described as healthy weight gain or a “return to health”. It however remains uncertain whether underweight PWH are protected against elevated arterial stiffness by their body composition.
Several studies have attributed impaired vascular compliance to ART. Nucleoside reverse transcriptase inhibitors such as abacavir have been implicated in causing endothelial dysfunction by decreasing the bioavailability of nitric oxide [50]. Studies have also shown that exposure of endothelial cells to protease inhibitors increases leukocyte recruitment and adhesion to these cells [51, 52]. This adhesion stimulates the increased secretion of cytokines such as interleukin 6 (IL6) and tumour necrosis factor (TNFα), which have been implicated in attenuating the production of nitric oxide [53]. Decreases in nitric oxide result in decreased vascular compliance. In contrast, Dorjee, Desai [54] reported that while some ART regimens such as abacavir and tenofovir based drug combinations have been associated with increased cardiovascular risk, tenofovir and emtricitabine-efavirenz were associated with a lower risk of acute myocardial infarction [54]. However, more studies are needed to validate these findings.
Our study had several strengths, but also some limitations. It is among the few describing arterial stiffness measures and waveforms to assess cardiovascular risk in PWH on ART, particularly among low BMI individuals underrepresented in prior analyses. Additionally, our study adds to the presently limited data on CVD risk factors among PWH in sub-Saharan Africa, the region with the highest burden of HIV. However, due to the cross-sectional design, causality could not be determined. Further, the study lacked an HIV negative control group and was conducted in a primarily urban population in Zambia. Further studies will be needed to assess the generalizability of the results to other populations in SSA as well as other regions.
Conclusion
In SSA, underweight and overweight PWH had a similar distribution of vascular waveforms suggesting that low BMI may not confer substantial protection against impaired vascular compliance among individuals on long-term ART. As PWH can now survive decades on effective ART the burden of CVD continues to increase. Future studies of interventions to reduce CVD risk in PWH should include greater representation of low BMI individuals, as well as assessing effectiveness specifically in the context of the HIV epidemic in SSA.
Data availability
The data that support the findings of this study are available from the corresponding author, L.K., upon reasonable request.
References
Shah ASV, Stelzle D, Lee KK, Beck EJ, Alam S, Clifford S, et al. Global burden of atherosclerotic cardiovascular disease in people living with HIV: systematic review and meta-analysis. Circulation. 2018;138(11):1100–12.
Cerrato E, D’Ascenzo F, Biondi-Zoccai G, Calcagno A, Frea S, Grosso Marra W, et al. Cardiac dysfunction in pauci symptomatic human immunodeficiency virus patients: a meta-analysis in the highly active antiretroviral therapy era. Eur Heart J. 2013;34(19):1432–6.
Douglas PS, Umbleja T, Bloomfield GS, Fichtenbaum CJ, Zanni MV, Overton ET, et al. Cardiovascular risk and health among people with human immunodeficiency virus (HIV) eligible for primary prevention: insights from the REPRIEVE trial. Clin Infect Dis. 2021;73(11):2009–22.
Karand JC, Reis K, Stephano PF, Gargurevich N, Zhou J, Desderius B, et al. Sex-dependent correlates of arterial stiffness in Tanzanian adults. Trop Med Int Health. 2021;26(11):1494–502.
Hall JE. Guyton and hall textbook of medical physiology. 13th ed. London: W B Saunders; 2015.
Losina E, Hyle EP, Borre ED, Linas BP, Sax PE, Weinstein MC, et al. Projecting 10-year, 20-year, and lifetime risks of cardiovascular disease in persons living with human immunodeficiency virus in the United States. Clin Infect Dis. 2017;65(8):1266–71.
Caballero AE. Endothelial dysfunction in obesity and insulin resistance: a road to diabetes and heart disease. Obesity Res. 2003;11(11).
Kline ER, Sutliff RL. The roles of HIV-1 proteins and antiretroviral drug therapy in HIV-1-associated endothelial dysfunction. J Investig Med. 2008;56(5):752–69.
Longenecker CT, Funderburg NT, Jiang Y, Debanne S, Storer N, Labbato DE, et al. Markers of inflammation and CD8 T-cell activation, but not monocyte activation, are associated with subclinical carotid artery disease in HIV-infected individuals. HIV Med. 2013;14(6):385–390.
Grome HN, Barnett L, Hagar CC, Harrison DG, Kalams SA, Koethe JR. Association of T Cell and macrophage activation with arterial vascular health in HIV. AIDS Res Hum Retroviruses. 2017;33(2):181–6.
Tejero J, Shiva S, Gladwin MT. Sources of vascular nitric oxide and reactive oxygen species and their regulation. Physiol Rev. 2019;99(1):311–79.
De Caterina R, Libby P. Endothelial dysfunctions and vascular disease: Blackwell Publishing; 2007.
Nichols W, O’Rourke M, Vlachopoulos C. McDonald’s blood flow in arteries theoretical, experimental and clinical principles. Sixth ed. Taylor & Francis Group, LLC; 2011.
Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55(13):1318–27.
Mueller N, Streis J, Muller S, Pavenstadt H, Felderhoff T, Reuter S, et al. Pulse wave analysis and pulse wave velocity for fistula assessment. Kidney Blood Press Res. 2020;45(4):576–88.
Starzak M, Stanek A, Jakubiak GK, Cholewka A, Cieslar G. Arterial Stiffness assessment by pulse wave velocity in patients with metabolic syndrome and its components: is it a useful tool in clinical practice? Int J Environ Res Public Health. 2022;19(16).
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63(7):636–46.
Lee Y-S, Kim K-S, Nam C-W, Han S-W, Hur S-H, Kim Y-N, et al. Clinical implication of carotid-radial pulse wave velocity for patients with coronary artery disease. Korean Circulation J. 2006;36:565–72.
Said MA, Eppinga RN, Lipsic E, Verweij N, van der Harst P. Relationship of arterial stiffness index and pulse pressure with cardiovascular disease and mortality. J Am Heart Assoc. 2018;7(2).
Alam M. Complior Analyse; Measure of pulse wave velocity and central pressure analysis Operator Manual. Alam medical v1.9beta version; 2013.
Proença MRPB, F. Bonnier, G. Delgado-Gonzalo, R. Lemkaddem, A. Verjus, C. Ferrario, D. Lemay M. The Handbook of cuffless blood pressure monitoring: pulse wave analysis techniques. Swiss Center for Electronics and Microtechnology (PREPRINT). 2019.
Laurent S. Surrogate measures of arterial stiffness: do they have additive predictive value or are they only surrogates of a surrogate? Hypertension. 2006;47(3):325–6.
Karim R, Mack WJ, Kono N, Tien PC, Anastos K, Lazar J, et al. T-cell activation, both pre- and post-HAART levels, correlates with carotid artery stiffness over 6.5 years among HIV-infected women in the WIHS. J Acquir Immune Defic Syndr. 2014;67(3):349–56.
Kaluba L, Goma F, Guure C, Munsaka S, Mutale W, Heimburger DC, et al. Immune activation and arterial stiffness in lean adults with human immunodeficiency virus on antiretroviral therapy. S Afr J HIV Med. 2021;22(1).
Maloberti A, Dozio D, Betelli M, Bandera A, Squillace N, Gori A, et al. Brachial and central blood pressure in HIV-infected subjects. Hypertens Res. 2015;38(6):405–12.
Gleason RL Jr, Caulk AW, Seifu D, Parker I, Vidakovic B, Getenet H, et al. Current Efavirenz (EFV) or ritonavir-boosted lopinavir (LPV/r) use correlates with elevate markers of atherosclerosis in HIV-infected subjects in Addis Ababa, Ethiopia. PLoS ONE. 2015;10(4): e0117125.
Vos AG, Barth RE, Klipstein-Grobusch K, Tempelman HA, Deville WLJ, Dodd C, et al. Cardiovascular disease burden in rural Africa: does HIV and antiretroviral treatment play a role? Baseline analysis of the NDLOVU cohort study. J Am Heart Assoc. 2020;9(7): e013466.
MOH. Zambia population-based HIV impact assessment (ZAMPHIA) 2016: final report. Lusaka: Ministry of Health, Zambia; 2016 February 2019.
WHO. WHO STEPwise approach to surveillance , WHO STEPS instrument. 2003.
American College of Cardiology/American Heart Association Task Force on Practice Guidelines OEP. Executive summary: Guidelines (2013) for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society published by the Obesity Society and American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Based on a systematic review from the The Obesity Expert Panel, 2013. Obesity (Silver Spring). 2014;22 Suppl 2:S5–39.
Stata Statistical Software: Release 14 [Internet]. StataCorp LP. 2015.
Kim J. How to Choose the Level of Significance: A Pedagogical Note MPRA. 2015;66373.
Ngatchou W, Lemogoum D, Ndobo P, Yagnigni E, Tiogou E, Nga E, et al. Increased burden and severity of metabolic syndrome and arterial stiffness in treatment-naive HIV+ patients from Cameroon. Vasc Health Risk Manag. 2013;9:509–16.
Msoka TF, Van Guilder GP, Smulders YM, van Furth M, Bartlett JA, van Agtmael MA. Association of HIV-infection, antiretroviral treatment and metabolic syndrome with large artery stiffness: a cross-sectional study. BMC Infect Dis. 2018;18(1):708.
Lopez M, San Roman J, Estrada V, Vispo E, Blanco F, Soriano V. Endothelial dysfunction in HIV infection - the role of circulating endothelial cells, microparticles, endothelial progenitor cells and macrophages. AIDS rev. 2012;14:223–30.
Shao Y, Cheng Z, Li X, Chernaya V, Wang H, Yang X. Immunosuppresive/anti-inflammatory cytokines directly and indirectly inhibit endothelial dysfunction- a novel mechanism for maintaining vascular function. Journal of Hematology and Oncology. 2014;7(80).
Majeed BA, Eberson LS, Tawinwung S, Larmonier N, Secomb TW, Larson DF. Functional aortic stiffness: role of CD4(+) T lymphocytes. Front Physiol. 2015;6:235.
Robbertse PS, Doubell AF, Innes S, Lombard CJ, Herbst PG. Pulse wave velocity demonstrates increased aortic stiffness in newly diagnosed, antiretroviral naive HIV infected adults: a case-control study. Medicine (Baltimore). 2022;101(34): e29721.
Fourie CMT, Botha-Le Roux S, Smith W, Schutte AE, Breet Y, Mels CMC, et al. Vascular function and cardiovascular risk in a HIV infected and HIV free cohort of African ancestry: baseline profile, rationale and methods of the longitudinal EndoAfrica-NWU study. BMC Infect Dis. 2020;20(1):473.
Benetos A, Waeber B, Izzo J, Mitchell G, Resnick L, Asmar R, et al. Influence of age, risk factors, and cardiovascular and renal disease on arterial stiffness: clinical applications. AJH. 2002;15:1101–8.
Guers JJ, Farquhar WB, Edwards DG, Lennon SL. Voluntary wheel running attenuates salt-induced vascular stiffness independent of blood pressure. Am J Hypertens. 2019;32(12):1162–9.
Feigl AB, Bloom DE, Danaei G, Pillay D, Salomon JA, Tanser F, et al. The effect of HIV and the modifying effect of anti-retroviral therapy (ART) on body mass index (BMI) and blood pressure levels in rural South Africa. PLoS ONE. 2016;11(8): e0158264.
McComsey GA, Moser C, Currier J, Ribaudo HJ, Paczuski P, Dube MP, et al. Body composition changes after initiation of raltegravir or protease inhibitors: ACTG A5260s. Clin Infect Dis. 2016;62(7):853–62.
Sax PE, Erlandson KM, Lake JE, McComsey GA, Orkin C, Esser S, et al. Weight gain following initiation of antiretroviral therapy: risk factors in randomized comparative clinical trials. Clin Infect Dis. 2020;71(6):1379–89.
Bailin SS, Gabriel CL, Wanjalla CN, Koethe JR. Obesity and weight gain in persons with HIV. Curr HIV/AIDS Rep. 2020.
Okello S, Amir A, Bloomfield GS, Kentoffio K, Lugobe HM, Reynolds Z, et al. Prevention of cardiovascular disease among people living with HIV in sub-Saharan Africa. Prog Cardiovasc Dis. 2020;63(2):149–59.
Gustafson B, Hammarstedt A, Andersson CX, Smith U. Inflamed adipose tissue: a culprit underlying the metabolic syndrome and atherosclerosis. Arterioscler Thromb Vasc Biol. 2007;27(11):2276–83.
Lukich A, Gavish D, Shargorodsky M. Normal weight diabetic patients vs obese diabetics relation of overall and abdominal adiposity to vascular health.pdf. Cardiovascular Diabetology. 2014;13(141).
Kumar S, Samaras K. The impact of weight gain during HIV treatment on risk of pre-diabetes, diabetes mellitus, cardiovascular disease, and mortality. Front Endocrinol (Lausanne). 2018;9:705.
Hsue PY, Hunt PW, Wu Y, Schnell A, Ho JE, Hatano H, et al. Association of abacavir and impaired endothelial function in treated and suppressed HIV-infected patients. AIDS. 2009;23(15):2021–7.
Mondal D, Pradhan L, Ali M, Agrawal K. HAART drugs induce oxidative stress in human endothelial cells and increase endothelial recruitment of mononuclear cells. Cardiovasc Toxicol. 2004;4:287–302.
Chow DC, Stein JH, Seto TB, Mitchell C, Sriratanaviriyakul N, Grandinetti A, et al. Short-term effects of extended-release niacin on endothelial function in HIV-infected patients on stable antiretroviral therapy. AIDS. 2010;24(7):1019–23.
Anderson HD, Rahmutula D, Gardner DG. Tumor necrosis factor-alpha inhibits endothelial nitric-oxide synthase gene promoter activity in bovine aortic endothelial cells. J Biol Chem. 2004;279(2):963–9.
Dorjee K, Desai M, Choden T, Baxi SM, Hubbard AE, Reingold AL. Acute myocardial infarction associated with abacavir and tenofovir based antiretroviral drug combinations in the United States. AIDS Res Ther. 2021;18(1):57.
Acknowledgements
The authors would like to thank the staff at the NUSTART centre at the University Teaching Hospital, Lusaka.
Funding
This work was supported by the Fogarty International Centre of the U.S. National Institutes of Health under the Award Number D43 TW009744, the NIH-funded Vanderbilt Clinical and Translational Science Award from NCRR/NIH Grant UL1 RR024975, the NIH-funded Tennessee Centre for AIDS Research Grant P30 AI110527, and National Institutes of Health grant K01HL130497. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
LK, TC, FG, WM, DH and JRK wrote the main manuscript text. MM, LK and TC prepared the tables. All authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Participants provided written informed consent, and ethical approval was obtained from the University of Zambia Biomedical Research Ethics Committee (UNZABREC reference number 003–01-18; IRB00001131 of IORG0000774) and the National Health Research Authority (NHRA). All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kaluba, L., Chikopela, T., Goma, F. et al. Vascular dysfunction and body mass index in African adults with HIV. BMC Cardiovasc Disord 23, 64 (2023). https://doi.org/10.1186/s12872-023-03093-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03093-2