Abstract
Background
The purpose of present study was to determine whether obesity was associated with increased adverse outcomes after cardiac surgery.
Methods
This is a retrospective cohort study from a large international database called the Medical Information Mart for Intensive Care III (MIMIC-III). Patients who underwent cardiac surgery and greater than 18 years old were divided into either nonobese (BMI < 30 kg/m2) or obese (BMI ≥ 30 kg/m2). The primary outcome of this study was 28-day mortality from the date of operation. Secondary outcomes included ICU mortality, 1-year mortality, incidence of postoperative atrial fibrillation (POAF), hospital length of stay (HOS_LOS) and ventilation-free days within 28 days (VFD_28).
Results
Multivariate logistic regression analysis revealed a negative effect of obesity on 28-day mortality, with an adjusted odds ratio (OR) of 1.57 (95% CI 1.14–2.16; p = 0.005). The association remained significant when PSM analysis and double robust analysis with all covariates were performed. In terms of 28-day mortality, the mediating effect of longer ventilation duration on obese patients was noticeable, and the proportion of the effect mediated was 8.2% (95% CI 2.1–25.5%; p = 0.012).
Conclusions
Among patients with cardiac surgery, obesity is associated with higher 28-day mortality. The longer ventilation duration may have mediated this effect. In future, considering the elevated incidence of the obese patients undergoing cardiac surgery, obesity stat should be included as one of the predictive variables for stratification of perioperative death risk.
Similar content being viewed by others
Background
According to the World Health Organization, obesity prevalence is increasing worldwide [1]. Furthermore, obesity is a well-established risk factor for cardiovascular disease and its associated complications, such as heart failure, hypertension, or diabetes [2]; consequently, cardiac surgery has become widespread in obese patients, particularly in severely obese individuals [3, 4]. Previous studies have suggested that obese patients have worse clinical outcomes after cardiac surgery [5,6,7], however, other studies have found that obesity can be a positive factor. Obese patients have fewer problems and deaths after cardiac surgery than normal or underweight patients, in what is known as the “obesity paradox” [8,9,10]. These conflicting conclusions indicate that the relationship between obesity and the adverse outcomes of cardiac surgery remains uncertain.
Thus, the purpose of the present study was to determine whether obesity was associated with increased adverse outcomes after cardiac surgery. We hypothesized that obesity would have no paradoxical effect on postoperative outcomes.
Methods
Study design and participants
A large international database called the Medical Information Mart for Intensive Care III (MIMIC-III) [11] provided data in this a retrospective cohort study. The MIMIC-III is a large, single-center database comprising information relating to over 50,000 patients admitted to critical care units at the Beth Israel Deaconess Medical Center between 2001 and 2012. Data includes vital signs, medications, laboratory measurements, observations and notes charted by care providers, fluid balance, procedure codes, diagnostic codes, imaging reports, hospital length of stay, survival data, and more. By completing a test and earning certification, author Jiang was accountable for extracting data (certification number: 9,322,422).
Patients who underwent cardiac surgery in the MIMIC-III were eligible for inclusion. Cardiac surgery mainly concluded coronary artery bypass graft (CABG), valve surgery, pericardium surgery, septa surgery and thoracic aorta surgery. Patients who were under the age of 18 or missing BMI data were excluded. Furthermore, we analyzed only patient’s first ICU admission.
Variable extraction
Structured Query Language (SQL) was used to obtain preoperative baseline characteristics, such as age, sex, BMI, ethnicity, admission type, surgery type, and comorbidities. Comorbidities including hypertension, diabetes, congestive heart failure (CHF), chronic pulmonary condition, stroke, renal disease, liver condition, cancer, coagulopathy and anemia were identified based on recorded ICD-9 codes.
Patients were classified as either nonobese (BMI < 30 kg/m2) or obese (BMI ≥ 30 kg/m2) according to the World Health Organization classification [1].
Clinical outcomes
The primary outcome of this study was 28-day mortality from the date of operation. Secondary outcomes included ICU mortality, 1-year mortality, incidence of postoperative atrial fibrillation (POAF), hospital length of stay (HOS_LOS) and ventilation-free days within 28 days (VFD_28).
Statistical analysis
Continuous variables are presented as the means and standard deviations, and values are presented as total numbers and percentages for categorical variables. Student’s t test was used to compare continuous data, the X2 or Fisher’s exact test was used to compare categorical data as appropriate. To avoid bias caused by missing data, the analysis was conducted after multiple imputations.
Multivariate regression was selected to evaluate the correlation between obesity and the clinical outcome. Baseline variables including age, sex, ethnicity, admission type, surgery type, and comorbidities were entered into a multivariate regression model as covariates. These variables were selected because of their clinical relevance. We used a stepwise backward elimination technique with a p < 0.05 to build our final models.
Sensitivity analyses, including propensity score matching (PSM) [12] and doubly robust analysis with all confounders [13, 14] — the combination of the PSM model and multivariate logistic regression analysis, were applied to evaluate the robustness of the primary findings of the study. When estimating the propensity scores of the patients, a multivariate logistic regression model was employed. A 1:1 nearest neighbor matching and a caliper width of 0.01 was applied in this study.
Causal mediation analysis (CMA) [15] is a technique for partitioning the total effect of an intervention into direct and indirect effects. The mediator mediates the indirect effect on the outcome. The analysis included average causal mediating effects (ACME), average direct effects (ADE), and total effects. In present study, we used CMA to investigate if the effect of obesity on the major outcome is partially mediated by the ventilation duration.
All statistical analyses were performed using the SPSS version 22.0 (IBM, Armonk, NY, USA) and EmpowerStats software (http://www.empowerstats.com), p < 0.05 were considered significant.
Results
Baseline characteristics
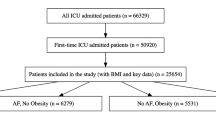
A total of 7160 patients with cardiac surgery were enrolled in present study. Figure 1 depicts the study selection process. Among the selected patients, 4737 patients had their BMI < 30 kg/m2, and 2423 patients had their BMI ≥ 30 kg/m2. Table 1 summarizes the baseline characteristics of the nonobese and obese groups. Compared with nonobese patients, obese people were more likely to with higher prevalence of hypertension, diabetes, chronic pulmonary condition, and coagulopathy.
Primary outcome
Multivariate logistic regression analysis revealed a negative effect of obesity on 28-day mortality, with an adjusted odds ratio (OR) of 1.57 (95% CI 1.14–2.16; p = 0.005) (Fig. 2). Using a 1:1 matching algorithm, 2371 patients in the nonobese group were matched with 2371 patients in the obese group after PSM (Table S1). The association remained significant when PSM analysis and double robust analysis with all covariates were performed (Fig. 2, OR 1.37, 95% CI 1.02–1.96, p = 0.05; OR 1.55, 95% CI 1.06–2.27, p = 0.023, respectively).
To investigate the effect of morbid obesity in cardiac surgery patients, additional analyses that classified obesity into overweight, class 1 and class 2–3 found an elevated risk of 28-day death in obese class 2–3 (Table 2). Subgroup analyses were also conducted to determine the relationship between obesity and the primary outcome according to the surgery type (valve surgery, CABG and combined surgery), and the results were presented in Table S2.
Secondary outcomes
Figure 3 presents the detailed results of the secondary outcome multivariate regression. Obesity significantly increased the ICU mortality and incidence of POAF (Fig. 3a), prolonged hospital length of stay, and decreased the number of ventilator-free days within 28 days (Fig. 3b). However, the two groups did not differ significantly in terms of 1-year mortality.
Association between obesity and secondary outcomes. a Odds ratio represents the odds of death or POAF in obese patients compared to nonobese. b Effect estimates and 95% confidence interval from the multivariable linear regression for VFD_28 and Hos_los. Effect estimate refers to the change in the outcome variable of obese patients compared to nonobese. POAF: postoperative atrial fibrillation; VFD_28: Ventilator-free days at day 28; Hos_los: length of hospital stay
Causal mediation analysis (CMA)
The direct and indirect effects of obesity on 28-day mortality were explored by CAM. When ventilation-free days within 28 days were employed as a mediator variable, the indirect effect was substantial. The total effect was 0.013 (95% CI 0.004–0.022; p = 0.002), the ACME was 0.001 (95% CI 0.0002–0.002; p = 0.02), the ADE was 0.012 (95% CI 0.003–0.021; p = 0.008), and the proportion of the effect mediated was 8.2% (95% CI 2.1–25.5%; p = 0.012) (Fig. 4). We concluded that obesity has a negative effect on 28-day mortality, which is mediated in part by a prolonged ventilation duration.
Discussion
The results of this study indicate that obesity is related to a considerably higher 28-day mortality than non-obesity, as well as elevated ICU mortality and incidence of POAF, longer hospital length of stay, and lower ventilation-free days within 28 days, while there is no association with 1-year mortality. In terms of 28-day mortality, the mediating effect of a longer ventilation duration on obese patients was noticeable.
The increasing incidence of obesity and its accompanying health risks is a major public health issue worldwide. Specifically, excessive surgery is known to be associated with a BMI greater than 30 kg/m2 [16]. However, the EuroSCORE II model does not incorporate BMI as a risk factor for perioperative death stratification [17], as the risk of obesity in cardiac surgery remains controversial. Several studies [10, 18, 19] and a recent meta-analysis [9] have reported an “obesity paradox,” demonstrating a similar or even lower morbidity and mortality in obese patients than nonobese patients. Conversely, previous studies have also suggested higher morbidity and mortality rates in obese patients undergoing cardiac surgery. For instance, Kuduvalli et al. [20] reported a significantly prolonged ventilation duration and longer length of hospital stay in obese patients after CABG. Habib et al. [5] also concluded that obese patients experienced a greater incidence of morbidity and mortality following coronary artery bypass grafting. Our results are consistent with these findings, and refute the “obesity paradox” in terms of postoperative outcomes. The increase in 28-day mortality in obese patients remained significant after PSM and doubly robust analyses.
There are a number of reasons for why “obesity paradox” was observed in some cohort studies. Patients who are leaner may exhibit health behaviors such as smoking, frailty, comorbidities, or even cachexia, such as cancer. This leaner body habitus or a higher burden of comorbidities will independently contribute to increased morbidity and mortality. However, these health behaviors and comorbidities were considered in the multivariable model. Selection bias may be the most important explanation for “obesity paradox”. Risk stratification was adequately assessed for elective cardiac surgeries. Those with a high BMI but no metabolic syndrome are more likely to be deemed surgical candidates than those at a higher risk of obesity consequences [21]. The data of the present study were provided by MIMIC, which comprises not only elective surgery but also emergency and urgent surgery.
The present study indicates that obesity was not associated with 1-year mortality. Obesity may not be a risk factor for long-term survival due to renin–angiotensin responses, cytokine and neuroendocrine profiles, and differences in the pathogenesis of cardiovascular disease in obese and non-obese patients [22, 23]. Furthermore, changes in health habits after cardiac surgery may also affect long-term survival. Therefore, it is unclear whether the association between obesity and long-term mortality remains significant.
A mismatch between ventilation and perfusion, reduced functional residual capacity, and low respiratory reserve are more likely to occur in obese patients [16, 23]. By performing CMA, we observed that the effect of obesity on 28-day mortality in cardiac surgery patients was partially attributable to the prolonged ventilation duration.
Numerous limitations should be considered in this investigation. First, this study was performed using MIMIC databases spanning more than ten years, and we were unable to ascertain the exact year of patient admission. It is possible that changes in medical therapy and surgical techniques had an impact on the outcomes. Second, our study included a significantly higher proportion of non-obese patients than obese patients. Hence, we performed PSM to evaluate the robustness of the study’s primary findings in the sensitivity analysis. In addition, when separating obesity status to investigate different classes on the prognosis, the present study did not consider the underweight cohort (BMI < 18.5 kg/m2) due to the lack of patients (n = 96). Finally, the effect of metabolic syndrome [24, 25] on stratification of obesity based on fat distribution was not considered in the present study. Nonetheless, BMI continues to be a key starting point for patient categorization and comparisons with other studies, despite its limitations as a measure of obesity.
Conclusion
Among patients undergoing cardiac surgery, obesity was associated with higher 28-day mortality rates. A longer duration of ventilation may have mediated this effect. A major part of pre-surgery counseling has focused on the influence of comorbidities and surgery risk, such as in the EuroSCORE II model. In the future, considering the elevated incidence of obese patients undergoing cardiac surgery, obesity status should be included as a predictive variable for stratification of perioperative death risk.
Availability of data and materials
The datasets of the current study are available from the corresponding author on reasonable request.
Abbreviations
- CABG:
-
coronary artery bypass graft
- SQL:
-
Structured Query Language
- BMI:
-
body mass index
- CHF:
-
congestive heart failure
- POAF:
-
postoperative atrial fibrillation
- ICU:
-
intensive care unit
- LOS:
-
length of stay
- VFD_28:
-
Ventilator-free days at day 28
- PSM:
-
propensity score matching
- CMA:
-
Causal mediation analysis
- ACME:
-
average causal mediating effects
- ADE:
-
average direct effects
References
Obesity. Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii, 1–253.
Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96.
Alnasser SM, Huang W, Gore JM, Steg PG, Eagle KA, Anderson FA Jr, Fox KA, Gurfinkel E, Brieger D, Klein W, et al. Late Consequences of Acute Coronary Syndromes: Global Registry of Acute coronary events (GRACE) follow-up. Am J Med. 2015;128(7):766–75.
Prabhakar G, Haan CK, Peterson ED, Coombs LP, Cruzzavala JL, Murray GF. The risks of moderate and extreme obesity for coronary artery bypass grafting outcomes: a study from the Society of thoracic Surgeons’ database. Ann Thorac Surg. 2002;74(4):1125–30. discussion 1130 – 1121.
Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah A. Effects of obesity and small body size on operative and long-term outcomes of coronary artery bypass surgery: a propensity-matched analysis. Ann Thorac Surg. 2005;79(6):1976–86.
Ho KM, Bertenshaw C, Same S, Schneider M, Williams KA, Godsell T, Hird K. Differential associations between body mass index and outcomes after elective adult cardiac surgery: a linked data cohort study. Anaesth Intensive Care. 2013;41(5):573–83.
Lopez-Delgado JC, Esteve F, Manez R, Torrado H, Carrio ML, Rodríguez-Castro D, Farrero E, Javierre C, Skaltsa K, Ventura JL. The influence of body mass index on outcomes in patients undergoing cardiac surgery: does the obesity paradox really exist? PLoS ONE. 2015;10(3):e0118858.
Hartrumpf M, Kuehnel RU, Albes JM. The obesity paradox is still there: a risk analysis of over 15 000 cardiosurgical patients based on body mass index. Interact Cardiovasc Thorac Surg. 2017;25(1):18–24.
Mariscalco G, Wozniak MJ, Dawson AG, Serraino GF, Porter R, Nath M, Klersy C, Kumar T, Murphy GJ. Body Mass Index and Mortality among adults undergoing cardiac surgery: a Nationwide Study with a systematic review and Meta-analysis. Circulation. 2017;135(9):850–63.
Stamou SC, Nussbaum M, Stiegel RM, Reames MK, Skipper ER, Robicsek F, Lobdell KW. Effect of body mass index on outcomes after cardiac surgery: is there an obesity paradox? Ann Thorac Surg. 2011;91(1):42–7.
Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016;3:160035.
Zhang Z. Propensity score method: a non-parametric technique to reduce model dependence. Ann Transl Med. 2017;5(1):7.
Funk MJ, Westreich D, Wiesen C, Stürmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. Am J Epidemiol. 2011;173(7):761–7.
McCaffrey DF, Griffin BA, Almirall D, Slaughter ME, Ramchand R, Burgette LF. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. 2013;32(19):3388–414.
Zhang Z, Zheng C, Kim C, Van Poucke S, Lin S, Lan P. Causal mediation analysis in the context of clinical research. Ann Transl Med. 2016;4(21):425.
Wigfield CH, Lindsey JD, Muñoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI > or = 40. Eur J Cardiothorac Surg. 2006;29(4):434–40.
Nashef SA, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, Lockowandt U. EuroSCORE II. Eur J Cardiothorac Surg. 2012;41(4):734–44. discussion 744 – 735.
Johnson AP, Parlow JL, Whitehead M, Xu J, Rohland S, Milne B. Body Mass Index, Outcomes, and Mortality following cardiac surgery in Ontario, Canada. J Am Heart Assoc. 2015;4(7):e002140.
Reeves BC, Ascione R, Chamberlain MH, Angelini GD. Effect of body mass index on early outcomes in patients undergoing coronary artery bypass surgery. J Am Coll Cardiol. 2003;42(4):668–76.
Kuduvalli M, Grayson AD, Oo AY, Fabri BM, Rashid A. Risk of morbidity and in-hospital mortality in obese patients undergoing coronary artery bypass surgery. Eur J Cardiothorac Surg. 2002;22(5):787–93.
Murphy RA, Reinders I, Garcia ME, Eiriksdottir G, Launer LJ, Benediktsson R, Gudnason V, Jonsson PV, Harris TB. Adipose tissue, muscle, and function: potential mediators of associations between body weight and mortality in older adults with type 2 diabetes. Diabetes Care. 2014;37(12):3213–9.
Nakamura K, Fuster JJ, Walsh K. Adipokines: a link between obesity and cardiovascular disease. J Cardiol. 2014;63(4):250–9.
Ghanta RK, LaPar DJ, Zhang Q, Devarkonda V, Isbell JM, Yarboro LT, Kern JA, Kron IL, Speir AM, Fonner CE, et al. Obesity increases risk-adjusted morbidity, mortality, and cost following cardiac surgery. J Am Heart Assoc. 2017;6(3):e003831.
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010;375(9710):181–3.
Cichos KH, Churchill JL, Phillips SG, Watson SL, McGwin G Jr, Ghanem ES, Ponce BA. Metabolic syndrome and hip fracture: Epidemiology and perioperative outcomes. Injury. 2018;49(11):2036–41.
Acknowledgements
None.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
Xiaofeng Jiang: Conceptualization, Methodology, Writing - original draft; Yanhong Zhu: Project administration, Resources, Supervision, Writing - review & editing; Jianbo Xu: Formal analysis, Investigation, Validation; Shuai Zhen: Formal analysis, Validation. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki. Both BIDMC and the Massachusetts Institute of Technology (MIT) Institutional Review Boards agreed to approve this project (certification number: 9322422), and informed consent was waived for this retrospective study.
Consent for publication
NA.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Comparisons of Demographics According to Body Mass Index Category after Matching.
Additional file 2:
Table S2. Multivariable analyses of obesity and 28-day mortality according to surgery type.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, X., Xu, J., Zhen, S. et al. Obesity is associated with postoperative outcomes in patients undergoing cardiac surgery: a cohort study. BMC Anesthesiol 23, 3 (2023). https://doi.org/10.1186/s12871-022-01966-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01966-1