Abstract
Background
Based on our observations at the largest outpatient urology clinic in Iran, patients for whom finasteride is prescribed as a secondary drug to tamsulosin tend to experience earlier and more severe sexual side effects without any difference in the amelioration of symptoms. This study aimed to compare the time lag, efficacy, and side effects of combination therapy with varying doses of dutasteride or finasteride added to tamsulosin for benign prostatic hyperplasia (BPH) treatment.
Methods
In this study 165 were randomized into 5 groups (each N = 33); receiving tamsulosin 0.4mg plus either of A: finasteride 3mg, B: placebo, C: dutasteride 0.25mg, D: finasteride 5mg or E: dutasteride 0.5mg. During the 6-month period of the study, International Prostate Symptom Score (IPSS), post-void residual urine (PVR), International Index of Erectile Function (IIEF-5), prostate volume (PV), prostate specific antigen (PSA) and maximum urinary flow rate (Qmax) were evaluated at baseline and at the 1st, 3rd and 6th month. The differences between each time point and baseline were then compared between groups.
Results
At 3-month follow-up, group E exhibited a higher decrease in PSA but a greater increase in Qmax compared to group A (p = 0.047 and 0.006, respectively). Group C showed higher Qmax increase compared to group A at 3 and 6 months (p = 0.003 and 0.014) and concurrently a more pronounced PV decrease at 1 and 3 months (p = 0.047 and 0.003, respectively). Group D had a significantly more decrease in their IIEF-5 compared to group A at one-month visit (p = 0.006).
Conclusions
In summary, at the sixth-month follow-up, dutasteride demonstrated superiority over finasteride solely in enhancing Qmax. Therefore, dutasteride may be marginally more beneficial as a secondary component of combination therapy in BPH.
Trial registration IRCT, IRCT20120516009772N2. Registered 18 January 2021 Retrospectively registered, https://irct.behdasht.gov.ir/search/result?query=IRCT20120516009772N2.
Similar content being viewed by others
1 Background
In recent decades, medical treatment has surpassed surgical techniques to become the central treatment strategy for benign prostatic hyperplasia (BPH). Alpha-1A adrenergic receptor blockers (ABs) and 5-alpha reductase inhibitors (5ARIs) are the most prescribed drugs for BPH [1]. Tamsulosin, an AB which is established as the first-line treatment for BPH, is commonly combined with 5ARIs (i.e., finasteride and dutasteride) to enhance its efficacy and postpone BPH progression [2]. Nevertheless, these combination therapies are not free of adverse events, as they have been reported to lead to higher instances of erectile and ejaculation disorders, as well as decreased libido [2].
Previous studies have demonstrated that finasteride and dutasteride, two of the most prescribed 5ARIs, are similarly effective in alleviating lower urinary tract symptoms (LUTS) when used as monotherapy [3, 4]. Nonetheless, finasteride has been associated with a higher incidence of sexual adverse events [5]. Historically, studies have suggested that both drugs achieve maximal efficacy and maximum adverse effects severity only after six months, either as monotherapy or in combination with ABs [6, 7]. However, based on the experience of one of the authors (A.B.), who has a long history of treating BPH/LUTS patients, those treated with finasteride as a secondary drug to tamsulosin tend to experience earlier onset and more severe sexual side effects, but not necessarily earlier amelioration of LUTS, compared to those treated with tamsulosin and dutasteride. Moreover, preliminary data from our outpatient clinic, located at Iran’s largest referral urology hospital, suggest that the prevalence of sexual adverse events in BPH patients treated with the standard dose of finasteride (5mg daily) is higher in Iranian patients compared to international literature. On the other hand, there is some evidence that a low dose of finasteride (1mg daily) can have comparable effects on objective parameters such as peak urinary flow rate and prostate volume, with a lower rate of adverse events [6].
Considering these observations, we hypothesized that ethnic background and medication dosage might affect the efficacy, timing of treatment response, and incidence of side effects with the combination of tamsulosin and finasteride compared to tamsulosin and dutasteride. To address this, we designed a study to compare the efficacy and adverse events of these combination therapies involving different doses of finasteride or dutasteride with a fixed dose of tamsulosin.
2 Methods
2.1 Trial design and participants
In this randomized clinical trial, 165 men with a definitive diagnosis of BPH as established through medical history (mainly secondary LUTS) and physical exam (including digital rectal exam) for at least 6 months were included; 155 of whom completed the study. Inclusion criteria were: age ≥ 45 years, initial International Prostate Symptoms Score (IPSS) > 8 and total serum prostatic specific antigen (PSA) < 4.0 ng/mL or PSA between 4.0 and 4–5 ng/mL and negative trans-rectal ultrasound scan biopsy (TRUS biopsy), with at least an eight-week interval between TRUS biopsy and initiation of the treatment. Patients with a history of BPH treatment during the past month, evidence of concurrent prostate or bladder pathology (e.g., malignancy, inflammation), prior history of prostatic, pelvic, perineal or lumbar spinal surgery, simultaneous cardiovascular or lumbar degenerative disc disease, concurrent treatment with short- or long-acting nitrates, and simultaneous urinary tract infection were excluded. Patients were randomized into five groups (each N = 33) according to the drug regimens which were prescribed for them. Treatment regimens were Group A: (tamsulosin 0.4mg/day + finasteride 3mg/day), group B: (tamsulosin 0.4 mg/day + placebo, control group), group C: (tamsulosin 0.4 mg/day + dutasteride 0.25 mg/day), group D: (tamsulosin 0.4 mg/day + finasteride 5 mg/day) and group E: (tamsulosin 0.4 mg/day + dutasteride 0.5 mg/day). All participants were recruited from patients who referred to our tertiary urology hospital in Tehran, Iran; between April 2021 and December 2022.
2.2 Study interventions
On the first appointment, baseline demographics and past medical and drug history were collected through direct interview. A comprehensive lab test including prostate specific antigen (PSA) was ordered at baseline. An abdominal ultrasound (US) and a uroflowmetry were obtained from each patient to evaluate their prostate volume (PV), post-void residual volume (PVR) and maximum urinary flow rate (Qmax) at baseline, respectively. All patients also filled in the International Prostate Symptom Score (IPSS) and the abridged, 5-item version of the International Index of Erectile Function (IIEF-5) questionnaires at baseline to evaluate them for LUTS and erectile dysfunction (ED). The patients were treated for six months according to the treatment group they belonged to and they were instructed to exclusively adhere to their treatment and refrain from any additional medication or complementary treatment. Participants were instructed to return to the urology clinic on the first, third and sixth month after the initiation of treatment. Similar to the first appointment, PSA, PV, PVR, Qmax, IPSS and IIEF-5 were measured for the patients on these appointments. Finally, these outcomes were utilized to compare the efficacy of the different treatment regimens.
2.3 Efficacy measurements
The primary outcome measure was change in IPSS score in comparison with baseline at each appointment as measured by the standard IPSS questionnaire. The secondary outcomes were changes in PSA, PV, PVR, Qmax and IIEF-5 as measured by lab tests, abdominal US, uroflowmetry and the standard IIEF-5 questionnaire. The IPSS and IIEF-5 scoring systems have been described in detail elsewhere [8].
2.4 Sample size and randomization
The minimum sample size was computed to be 28 patients in each group, considering a type one error of 0.05, type two error of 0.20, and an \(\begin{array}{*{20}c} {effect\begin{array}{*{20}c} {} \\ \end{array} \begin{array}{*{20}c} {size = \frac{{\mu_{1} - \mu_{2} }}{\sigma }} \\ \end{array} } \\ \end{array}\) of 0.75. This calculation utilized the following equation: \({\text{n}} \ge \,\frac{{2\left( {Z_{1 - \alpha /2} + Z_{1 - \beta } } \right)^{2} \sigma^{2} }}{{\left( {\mu_{0} - \mu_{1} } \right)^{2} }}\). With consideration of a dropout rate of approximately 15%, we allocated 33 patients to each group. The eligible patients were then randomly assigned to one of the five intervention groups (A, B, C, D and E) using a simple randomization method. The random sequence was generated by a computer program before the study. The allocation ratio was 1:1. The study participants, statistician and researcher were unaware of patient allocation. One of the study investigators sequentially coded the drug and placebo containers, with the codes remaining confidential until the data analyses were completed.
2.5 Statistical analysis
All data were analyzed using SPSS software version 23 (IBM, Armonk, NY, United States). Quantitative and qualitative (categorical) variables were described as mean ± standard deviation and frequency (percentage), respectively. Normality assumptions were checked by Shapiro–Wilk test. Based on normality test results either a one-way analysis of variances (ANOVAs) or a Kruskal–Wallis H test was used to compare quantitative outcomes between the five groups. In case of overall significance, pairwise comparisons were utilized with a Bonferroni correction for multiple comparisons. A p-value < 0.05 was considered statistically significant in all statistical tests.
3 Results
3.1 Study population
Of the total 190 patients screened for this study, 165 were randomly assigned to different treatment regimens (each N = 33). All participants were aged between 45 to 88 years old. Figure 1 illustrates the participants included in the study. As shown, 33 (100%), 31 (94%), 29 (88%), 30 (91%), 32 (97%) patients from groups A, B C, D, and E completed the study and were included in the final analysis, respectively. Table 1 shows the baseline characteristics of the patients who completed the study. As observed, the five groups were similar regarding these baseline characteristics. The number of excluded cases were not significantly different among different study groups (p = 0.300).
3.2 Subjective outcomes
Table 2 illustrates the changes in IPSS and IIEF-5 values compared to the baseline values on first, second and third appointments. As observed, differences between IPSS change was different between treatments at the first, third and sixth months. Pairwise comparisons using Bonferroni corrections indicated that groups C, D and E exhibited significantly greater IPSS reduction than the control group B at months one (p = 0.021, 0.003 and 0.016, respectively), three (p = 0.001, 0.005 and 0.001, respectively) and six (p < 0.001, p = 0.022 and 0.002, respectively). Similar trends were seen for IIEF-5 reduction, with groups C, D and E showing more significant decreases compared to control group B at months one (p = 0.011, < 0.001 and 0.015, respectively) and three (p = 0.022, 0.001 and 0.006, respectively). Furthermore, in the first month follow-up, group D had significantly greater IIEF-5 reduction compared to group A (p = 0.006).
3.3 Objective outcomes
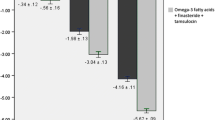
Table 3 depicts the changes of PSA, PV, PVR and Qmax across treatment groups. PSA change varied across treatment groups at the first, third and sixth month. Pairwise comparisons with Bonferroni corrections did not show any significant difference among different groups at the first month. At third month, groups D and E had more pronounced PSA decrease compared to the control group, B (p < 0.001 and p = 0.001, respectively). Group E also had significantly greater PSA reduction compared to group A (p = 0.047). By month six, groups C, D and E showed significantly greater PSA reductions than the placebo group B (p = 0.018, 0.003 and 0.011, respectively). PV change was similarly different at first, third and sixth month. Groups C, D and E demonstrated significantly greater PV reductions than group B at the first (p = 0.010, 0.011 and 0.035, respectively), third (p < 0.001, p = 0.003 and 0.001, respectively) and sixth (p < 0.001, p = 0.004 and 0.001, respectively) month follow-ups. Moreover, group C showed meaningfully greater PV reduction than group A at month one (p = 0.047) and month three (p = 0.003).
PVR changes also differed among various treatment groups at the third and sixth follow-up months. However, significant pairwise comparisons emerged only at the sixth month follow-up, indicating that groups C and E experienced a significantly greater decrease in their PVR compared to control group B (p = 0.004 and 0.025, respectively). Qmax changes varied in first, third and sixth months. At month one, group E had significantly more increase compared to control group B (p = 0.008) and group A (p = 0.020). At 3-month follow-up groups C, D and E had significantly more pronounced Qmax increases than control group B (p = 0.001, < 0.001 and 0.002, respectively) and group A (p = 0.003, < 0.001 and 0.006, respectively). Similarly, at the 6-month visit, groups A, C, D and E experienced higher Qmax increases than placebo group B (p = 0.032, p < 0.001, p < 0.001 and p < 0.001, respectively). Additionally, at the sixth month follow-up, group C had significantly greater Qmax increase compared to group A (p = 0.014).
4 Discussion
There is an ongoing debate regarding the treatment of choice for BPH. Various mono- and combination therapies have been proposed and approved in this regard [9]. According to the latest BPH management guideline of the American Urological Association (AUA), the combination of ABs and 5ARIs is suggested for moderate to severe LUTS in patients who have large prostates [10]. Nevertheless, controversy persists regarding the optimal combination regimen.
One of the main objectives of a successful treatment is to alleviate the patients’ symptoms. Our results indicated that in all three follow-ups patients who have undergone treatment with combination regimens, except for those who were treated with low-dose finasteride (3mg/day) and tamsulosin, have significantly better improvement in their IPSS score compared to tamsulosin alone. Moreover, finasteride (5mg/day) and dutasteride (either 0.25 or 0.5 mg/day) were similar to each other as secondary treatments to tamsulosin with regard to time lag to initiation of therapeutic effects and overall efficacy in reducing IPSS. Previous meta-analyses had conflicting views regarding the superiority of dutasteride vs. finasteride monotherapy in reducing IPSS, with two suggesting a slight superiority for dutasteride [11, 12], while one rejecting this supremacy [13]. Our results suggested that none of these drugs were better than the other when combined with tamsulosin. Nevertheless, our findings were generally in contrast with results from the CombAT trial, which showed that only after a minimum 9-month treatment with a combination therapy of dutasteride and tamsulosin, will it overtake tamsulosin monotherapy with regard to IPSS reduction [14].
Moreover, our analysis of IIEF-5 scores revealed that combination therapies tend to decrease sexual function significantly more than monotherapy with tamsulosin in the first- and third-month follow-up. Furthermore, similar to symptom relief, the time lag to presentation and severity of sexual side effects were comparable between finasteride (5mg/day) and dutasteride (either 0.25 or 0.5 mg/day). This finding rejects our preliminary postulation of the earlier emergence and more severe sexual side effects of finasteride. Previously, a meta-analysis had suggested that the risk of ED is significantly more pronounced with combination therapy compared to monotherapy with ABs [15]. Nevertheless, an interesting finding of our study was that at the sixth month appointment, the decrease of IIEF-5 was comparable between different combination therapies and monotherapy with tamsulosin, indicating similar sexual function in long-term follow-up. This finding was in line with some previous studies which demonstrated equal sexual function between combination therapy and monotherapy at long-term follow-up [7, 16].
Our analyses revealed that while PSA decrease was not meaningfully different among different treatment groups at the first month, it tended to be more prominent among combination groups at third- and sixth-month follow-ups. Our results were also suggestive of a possibly higher efficacy of dutasteride 0.5mg/day vs. finasteride 3mg/day when combined with tamsulosin in reducing PSA at the 3-month visit. Nevertheless, their efficiencies were similar at sixth month appointment. These results were in line with a previous study which indicated that dutasteride may decrease PSA more rapidly than finasteride when prescribed in combination with alfuzosin [17]. However, the final cumulative reduction of PSA seems to be similar between these two drugs at long-term follow-up [13, 18].
With regard to PV, combination therapies appeared to be more efficient in reducing PV compared to tamsulosin monotherapy at the first, third and sixth follow-up appointments. At first and third month follow-ups, dutasteride 0.25mg/day reduced PV significantly more than finasteride 3mg/day, when combined with tamsulosin. Nonetheless, PV decrease was comparable between these groups at the sixth month visit. In accordance, the literature suggests that although dutasteride monotherapy may cause a steeper decrease in PV compared to finasteride during the initial months of treatment [17], the total amount of PV reduction is similar between these two treatments [11,12,13].
It is worth noting that according to our findings, none of the IPSS, IIEF-5, PSA and PV items demonstrated significant changes in the low-dose finasteride (3mg/day) group, suggesting that low-dose finasteride (3mg/day) may not reach its physiologic threshold in any time frame, making it unsuitable as an auxiliary component in combination with tamsulosin for BPH treatment.
Our data also demonstrated that while PVR reduction was comparable at the first month follow-up, it was significantly different at the third and sixth posttreatment months. Nevertheless, significant between-group differences between combination therapies and the placebo group were only observed after six months. When compared with other objective and subjective outcomes, these results may suggest that PVR alleviation is relatively delayed compared to the improvement of other outcomes. Additionally, our pairwise comparisons showed that different combination therapies had comparable efficacy with one another with regard to PVR reduction. Likewise, previous studies have reported similar PVR reduction between finasteride or dutasteride either as monotherapy or as components of combination therapies with alfuzosin [11, 17].
With regard to Qmax, our data were suggestive of a superiority of combination therapies over monotherapy. Combination therapy comprising dutasteride 0.5mg/day and tamsulosin 0.4mg/day was the regimen with the earliest ameliorating effect on Qmax, starting as soon as the first posttreatment month. The effectiveness of combination therapies continued through the third and sixth month appointments and at the last visit at 6 months, all combination therapies were significantly more effective than tamsulosin alone. Previous studies demonstrated similar findings regarding the higher efficacy of a combination of ABs and 5ARIs in improving Qmax [2, 14]. Our analysis also clarified that a combination regimen of dutasteride and tamsulosin is superior to a combination of finasteride and tamsulosin in enhancing Qmax. This finding is in parallel with a recently published meta-analysis which suggested a marginal benefit for monotherapy with dutasteride over finasteride in improving Qmax [13]. Nevertheless, controversy persists in this regard; with many studies suggesting comparable Qmax outcomes after treatment with these drugs [11, 12, 17].
Our study was subject to some limitations. The relatively small sample size and the short follow-up period could potentially influence the robustness of our findings. The wide age-range of participants (45–88 years) introduces the possibility of increased comorbidities among the elderly, which may have affected our outcomes. Our study was constrained by time considerations, necessitating the inclusion of a few patients with PSA levels between 4.0 and 4.5 ng/ml. Although we ensured that none of them had any underlying prostate pathology other than BPH before starting the treatment; this inclusion criteria might have affected our results. Lastly and most importantly, our patients were evaluated by different sonologists and uroflowmetry stechnologists. The potential interobserver variability may justify some of our paradoxical findings such as the more reduction of PV and PVR values with low dose vs. high dose dutasteride (Table 3). However, it is worth highlighting that as far as we are concerned, our study represents the first ever investigation to directly compare the addition of dutasteride or finasteride to tamsulosin. Moreover, the multi-arm design of our study makes our findings worthy of consideration.
5 Conclusion
In conclusion, our findings indicated that dutasteride may be more efficient than finasteride in decreasing PSA and PV and increasing Qmax at the first posttreatment months. However, the final decrease in PSA and PV were comparable between combination therapies with dutasteride and finasteride and dutasteride was only associated with a more prominent increase in Qmax at the six-month follow-up. These findings may marginally favor the addition of dutasteride to tamsulosin compared to finstaeride, as a secondary treatment in BPH.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 5ARI:
-
5-Alpha reductase inhibitor
- AB:
-
Alpha-1A adrenergic receptor blocker
- BPH:
-
Benign prostatic hyperplasia
- IIEF-5:
-
International Index of Erectile Function
- IPSS:
-
International Prostate Symptom Score
- LUT:
-
Lower urinary tract symptoms
- PSA:
-
Prostate specific antigen
- PV:
-
Prostate volume
- PVR:
-
Post-void residual urine
- Qmax:
-
Maximum urinary flow rate
- TRUS:
-
Trans-rectal ultrasound scan
References
Plochocki A, King B (2022) Medical treatment of benign prostatic hyperplasia. Urol Clin North Am 49(2):231–238
Zhou Z et al (2019) Meta-analysis of the efficacy and safety of combination of tamsulosin plus dutasteride compared with tamsulosin monotherapy in treating benign prostatic hyperplasia. BMC Urol 19(1):17
Nickel JC et al (2011) Comparison of dutasteride and finasteride for treating benign prostatic hyperplasia: the enlarged prostate international comparator study (EPICS). BJU Int 108(3):388–394
Park T, Choi JY (2014) Efficacy and safety of dutasteride for the treatment of symptomatic benign prostatic hyperplasia (BPH): a systematic review and meta-analysis. World J Urol 32(4):1093–1105
Gupta AK et al (2022) Relative efficacy of minoxidil and the 5-α reductase inhibitors in androgenetic alopecia treatment of male patients: a network meta-analysis. JAMA Dermatol 158(3):266–274
Gormley GJ et al (1992) The effect of finasteride in men with benign prostatic hyperplasia. The finasteride study group. N Engl J Med 327(17):1185–91
Roehrborn CG et al (2011) Clinical outcomes after combined therapy with dutasteride plus tamsulosin or either monotherapy in men with benign prostatic hyperplasia (BPH) by baseline characteristics: 4-year results from the randomized, double-blind Combination of Avodart and Tamsulosin (CombAT) trial. BJU Int 107(6):946–954
Vartolomei L et al (2022) Lower urinary tract symptoms are associated with clinically relevant depression, anxiety, and stress symptoms. Aging Male 25(1):62–66
Zahir M et al (2023) Sildenafil Vs. tadalafil for the treatment of benign prostatic hyperplasia: a single-arm self-controlled clinical trial. Urol J 20:255
Lerner LB et al (2021) Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA GUIDELINE PART I-initial work-up and medical management. J Urol 206(4):806–817
Zhou Z et al (2020) Efficacy and safety of dutasteride compared with finasteride in treating males with benign prostatic hyperplasia: a meta-analysis of randomized controlled trials. Exp Ther Med 20(2):1566–1574
Yin T et al (2017) Comparisons of the efficacy and safety of finasteride and dutasteride for benign prostatic hyperplasia: a network meta-analysis. Am J Ther 24(5):e517–e523
Li Y et al (2022) The efficacy and safety of dutasteride and finasteride in patients with benign prostatic hyperplasia: a systematic review and meta-analysis. Transl Androl Urol 11(3):313–324
Roehrborn CG et al (2010) The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol 57(1):123–131
Favilla V et al (2016) Impact of combination therapy 5-alpha reductase inhibitors (5-ARI) plus alpha-blockers (AB) on erectile dysfunction and decrease of libido in patients with LUTS/BPH: a systematic review with meta-analysis. Aging Male 19(3):175–181
Lepor H et al (1996) The efficacy of terazosin, finasteride, or both in benign prostatic hyperplasia. Veterans affairs cooperative studies benign prostatic hyperplasia study group. N Engl J Med 335(8):533–9
Choi YH, Cho SY, Cho IR (2010) The different reduction rate of prostate-specific antigen in dutasteride and finasteride. Korean J Urol 51(10):704–708
Kang HW et al (2017) Change in prostate specific antigen concentration in men with prostate specific antigen less than 2.5 ng/ml taking low dose finasteride or dutasteride for male androgenetic alopecia. J Urol 198(6):1340–1345
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Research conceptualization and design: AB, AHK. Data acquisition: RZ, ARA, SG. Data analysis and interpretation: NB. Drafting of the manuscript: MZa. Critical revision of the manuscript: AB, MZa, MZo, NB. Administrative and technical support: AB, AHK, ARA. Approval of the final manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was in accordance with Helsinki and Istanbul declarations. It was ethically reviewed and approved by the IRB of Shahid Beheshti University of Medical Sciences (approval number: IR.SBMU.UNRC.REC.1399.014). Written consent forms were obtained from all patients before the initiation of interventions. This study has been registered in the Iranian registry of clinical trials (IRCT) (accreditation code: IRCT20120516009772N2).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Basiri, A., Zare, R., Zahir, M. et al. Comparison of combination therapy with tamsulosin and dutasteride or finasteride in patients with benign prostatic hyperplasia: a randomized clinical trial. Afr J Urol 30, 48 (2024). https://doi.org/10.1186/s12301-024-00451-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-024-00451-0