Abstract
Alginate is one of the well-studied natural polysaccharides that is most commonly used for the encapsulation of biological objects. Alginate hydrogels exhibit good biocompatibility and are often used to create shells around pancreatic islets of Langerhans in order to produce stable transplants, making possible long-term normoglycemia, and to prevent fatal hypoglycemia in absolute insulin deficient diseases. However, there exists the problem of rejection and loss of an encapsulated transplant owing to immune response. One of the lines of research into reduction of rejection and increase in the compatibility and stability of an alginate shell is the chemical modification of alginate. At present, a large number of chemically functionalized alginates are available for different purposes. This makes it possible to gain insight into relationship between the character of modification and the properties of modified alginates. The review highlights techniques and features of the chemical modification of sodium alginate designed for the microencapsulation of insulin producing cells.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The transplantation of pancreatic islets of Langerhans capable of secreting insulin directly into the bloodstream in response to rising glucose level is an effective and promising approach for the treatment of type 1 diabetes and other insulin-deficient states. In the long run, this approach will make it possible to completely free patients from lifelong injections of endogenous insulin, which is currently the standard treatment protocol [1–3]. The latest technologies of insulin delivery, such as closed loop systems with continuous glucose monitoring and bolus (continuous) infusion of both insulin and glucagon, are not widely available because of high costs of buying equipment and sensor replacement, growth of scar tissue owing to multiple punctures with microneedles, and premature sensor failure [4]. The more so that artificial systems do not guarantee complete glycemic control [5]. The transplantation of the pancreas is the only pathogenetic method for the treatment of insulin-deficient diseases which considerably improves the patient’s quality of life [6]. The transplantation of pancreatoduodenal organocomplex faces a considerable risk of serious complications, such as pancreatitis, bleeding, and humoral and cellular rejection options. In addition, the existing organ deficiency limits the availability of surgery [7]. A less invasive alternative is the transplantation of pancreatic islets of Langerhans [8]. At present, the most progressive clinical techniques for the allogeneic pancreatic islet transplantation make it possible to attain insulin independence for almost 50% recipients 5 years after transplantation [9]. The achievement of insulin independence is not the major goal of transplantation since the major goal is to prevent fatal hypoglycemia, the predominant cause of death of type 1 diabetic patients. The disadvantage of this technique is the need for immunosuppressive therapy that worsens the quality of life of the patient and increases the risk of infectious, oncological, cardiovascular, and metabolic diseases. The consequences of long-term immunosuppression may largely level out transplant advantages, which in conjunction with the donor shortage problem make a wide application of this technique hardly possible [10–12]. The encapsulation of the cells being transplanted into porous polymer shells protecting transplanted cells by their physical isolation from immune cellular reactions of the organism will enable one to fully reject systemic immunosuppression and appreciably increase the lifetime of cells in the recipient organism. A polymer shell for encapsulation should satisfy the following criteria [13, 14]: pass insulin into the blood and oxygen and glucose into cells; do not pass leukocytes and phagocytes; be compatible with both encapsulated cells and recipient organism in order not to cause immunological and fibrous reactions; do not biodegrade for a long time (5–10 years); have a smooth topography without rough surface; and preferably stimulate the growth of vessels around a capsule (for better supplying encapsulated cells with nutrition and a rapid “drainage” of released insulin).
The need to ensure the maximum survival and preservation of the normal vital activity of cells also imposes restrictions on encapsulation conditions, such as elimination of organic solvents, implementation of a procedure in an aqueous solution isotonic to cell cytosol (in the medium of physiological solution in the presence of a phosphate saline buffer), maintenance of pH between 7.2 and 7.5, maintenance of temperature from room temperature to 40°С (ideally at 37°С in an atmosphere of 5% water vapor saturated carbon dioxide), and a rapid solution gelation to reach an even distribution of cells or islets and avoid sedimentation.
These things considerably narrow the scope of materials intended for use. The above conditions are well matched by polymer hydrogels. Many water-soluble natural polymers, such as agaroseа, chitosan, cellulose, and collagen, show not bad results in cell encapsulation [15]. Among synthetic polymers, poly(ethylene glycol) and its derivatives are in common use. However, the most popular polymer for cell encapsulation is sodium alginate [16–18] which can rapidly form hydrogels in the presence of polyvalent ions at neutral pH and moderate temperatures. The properties of alginate capsules depend on many factors: the structure and purity of alginate, the type of a crosslinking cation, the concentration of alginate and crosslinking cation, and the size of capsules. This implies that, in theory, stable alginate capsules able to minimize fibrosis and prolong the lifetime of encapsulated cells can be prepared by the careful selection of reactants and encapsulation conditions. However, even in the case of the best selection of compositions and parameters, it is not excluded that capsules can be destabilized as a result of leaching of cations under physiological conditions by chelating compounds, such as phosphates, and their replacement with sodium ions. One of the pioneering and most studied approaches to improve the stability of alginate microcapsules is their coating with poly(amino acids), such as poly(L-lysin), poly(L-ornithine), and poly(L-guanidine) [19–23]. This approach has a positive impact on the mechanical properties of hydrogels and enhances the stability of capsules but can in vivo lead to the activation of inflammatory cytokines and increase fibrosis [24]. A poly(amino acid) layer-coated alginate capsule with cells is shown below.

Despite considerable achievements in the strategy of using alginate for the encapsulation of insulin producing cells, studies often fail on going to the stage of clinical trials owing to transplant death related to the immune response of the recipient organism to a foreign body and the degradation of capsules. Up to now there has been no versatile technique ensuring a good survival of cells and their long functioning in the recipient organism without systemic immunosuppression.
At present, one of the promising approaches for increasing stability and compatibility of alginate capsules is the chemical modification of alginate. This review is focused on description of chemically modified alginates which have been used for the microencapsulation of insulin producing cells.
UNMODIFIED ALGINATE: STRUCTURE AND MICROENCAPSULATION TECHNIQUES
Sodium(I) alginate is the sodium salt of alginic acid, the heteropolymer of two uronic acids, β-D-mannuronic acid (М) and its epimer, α-L-guluronic acid (G), linked by glycoside linkages. The structure of sodium alginate and the crosslinking of alginate by di- or higher valent metal cations are presented below.

The moieties of β-D-mannuronic and α-L-guluronic acids form homopolymer fragments, so-called M and G blocks, and hetero fragments, MG blocks, in a polymer molecule. The ratio of acids in a molecule depends on the specific type of algae and can be altered by enzymatic treatment [25, 26]. Alginate forms hydrogels (II) easily and quickly and, at the same time, softly (harmless to cells) with divalent cations (Ca2+, Ba2+) under physiological conditions and has low cost and toxicity [16, 27, 28].
The properties of alginate capsules, including permeability, depend on many factors: the degree of crosslinking, the maximum possible value of which is determined by the alginate structure, the ratio and sequential arrangement of М and G blocks [29–31], and molecular weight [32]. It was shown that gelation primarily occurs by the binding of divalent cations with the G blocks of alginate [33–36]. Sodium alginate can form gels with various polyvalent metal cations [37–39]. The nature of a crosslinking cation influences the properties of the resulting hydrogels [40, 41]. Hydrogels crosslinked by Ca2+ ions are most widely used for cell encapsulation, while Ba2+ ions are used less often because their application is considerably limited by potential toxicity creating a risk of poisoning during ion leaching under physiological conditions [42]. For alginate gels with a high content of G moieties, the stability of sizes and strength of the gel increase on going from Ca2+ to Ba2+ ions. The use of Ba2+ ions decreases the size of crosslinked capsules and reduces their permeability. In the case of Sr2+ ions, gels with intermediate characteristics were produced. For alginate with a high content of М moieties, there was the opposite situation; namely, capsules obtained using Ba2+ and Sr2+ ions were larger than calcium alginate capsules and showed the tendency to a more pronounced swelling, which caused an additional increase in permeability. As evidenced by studies, different alginate blocks bind ions to varying degrees. For example, Ca2+ ions bind only with G and MG blocks, Ba2+ ions bind with G blocks and to a lesser extent with G blocks, and Sr2+ ions bind with G blocks [16, 43, 44]. It was also shown that more stable calcium-crosslinked capsules can be produced by the enzymatic modification of alginate which upon modification contains only G and MG blocks [29]. The stability of capsules is also facilitated by alginate crosslinking by a solution of calcium ions with a small amount of barium ions. The as-produced capsules can ensure protection from the immune reactions of encapsulated human islets of Langerhans in transplantation into mice diabetics for up to 220 days with normoglycemia being maintained on average for 134 days [30]. The data on the effect of the ratio between G and M moieties on the biocompatibility of capsules are contradictory [45–50]. The degree of crosslinking is also affected by such factors as the pH of solution [51] and the concentration of alginate and crosslinking cation [52].
According to the sizes of the resulting capsules, macroencapsulation, microencapsulation, and nanoencapsulation can be distinguished [53, 54]. Microencapsulation typically involves the preparation of spherical capsules with a diameter ranging from two millimeters to tens of microns (in the case of cells) [55]. Microencapsulation is most widely used for the immunoisolation of cells since a capsule has the optimal volume to surface ratio providing a rapid exchange of insulin, oxygen, and nutrients [56, 57]. The process of microencapsulation generally includes two steps: the first step involves the generation of droplets of an aqueous solution of a mixture of alginate and cells, and the second stage consists in the crosslinking of droplets by divalent ions to afford gel capsules. The key stage is the generation of alginate solution droplets. Microencapsulation techniques are generally classified according to the droplet formation procedure. For cell microencapsulation, several procedures were developed [58, 59], including emulsification (Fig. 1a) [60]; alginate solution extrusion (Fig. 1b) [61, 62]; electrospraying (Figs. 1c) [63, 64]; the use of microfluidic devices (Fig. 1d) [65, 66]; and micromolding (Fig. 1e) [67, 68], including molds produced by lithography [69, 70].
The emulsion procedure is easiest from the technical point of view. Its benefits are a low equipment cost and simple scaling. However, this procedure suffers from drawbacks, such as a high variability of capsule sizes, possible damage to capsules at the interface [72], and reduction in the survival of cells because of their contact with an organic phase. For this reason, the emulsion procedure is used rarely for cell microencapsulation, like the micromolding procedure, which does not allow production of spherical particles and in which control of the uniformity of crosslinking and the removal of gel particles from a mold are hardly possible. The narrow size distribution of capsules and their reproducibility are of importance for further transplantation. These criteria are well matched by electrospraying and microfluidics procedures. Electrospraying is the most frequently used procedure of cell microencapsulation [73] in which a droplet is ejected from a tip of metal capillary nozzle when exposed to the electric field. This process is accompanied by the redistribution of charge in solution, and at a sufficiently strong applied field, a jet is formed, which subsequently splits into fine droplets [74]. The promising procedure for the encapsulation of insulin producing cells is the use of microfluidic devices allowing a high level of standardization of encapsulation conditions [75–79].
MODIFIED ALGINATE
There are many ways for the chemical modification of alginate for different purposes [80–84]. They can be conditionally divided into two types: alginate modification without additional crosslinking and alginate modification with additional crosslinking. Alginate modifications supposing no additional crosslinking are primarily aimed at decreasing the level of immune response, preventing the formation of fibrosis tissue around a capsule, and reducing inflammatory processes. The modification of alginate with moieties providing additional crosslinking primarily improves the stability of capsules owing to an increase in the time of biodegradation. The majority of modifications are performed via a carboxyl group by the carbodiimide method using water-soluble carbodiimide 1-ethyl-3-(3-dimethylaminopropyl)carbodiimide (EDC) combined with N-hydroxysuccinimide (NHS) [80, 81].
Modification without Additional Crosslinking
A team of researchers [85] made up a library of barium-crosslinked hydrogels based on 774 derivatives of low molecular weight (\({{M}_{{v}}}\) ~ 25 × 103) sodium alginate with a high content of guluronic acid moieties (>60%) [85]. The general schematic synthesis of sodium alginate derivatives is depicted below.

Alginate derivatives bearing amino, alkoxy, alkynyl, or azide groups were synthesized. It was shown that 634 modified alginates are capable of gelation in the presence of divalent cations. Hydrogels obtained using barium ions were evaluated in vivo on immunocompetent C57BL/6J mice in subcutaneous implantation. The level of acute inflammation was analyzed using a visualizing agent which yielded enhanced fluorescence in response to an increase in the activity of cathepsin, an immune cell activation marker. Two hundred functionalized alginate hydrogels exhibited fluorescence levels lower than that of the initial unmodified alginate gel. Among them, 16 most effective polymers and 53 of their structural analogs were used to prepare barium alginate microcapsules with a diameter from 300 to 350 µm (at this size, alginate induces the strongest response to the foreign body [86]), and the degree of fibrous tissue formation on them 28 days after intraperitoneal implantation into C57BL/6J mice was evaluated. Of the tested polymers the authors isolated three hydrogels which were characterized by the lowest fibrosis score: III (14.7% degree of functionalization, per amount of carboxyl groups), IV (24.9% degree of functionalization), and V (15.1% degree of functionalization):

These hydrogels also demonstrated a smaller fibrous tissue overgrowth on capsules 6 months after transplantation into nonhuman primates compared with the initial alginate.
The distribution of functional groups in a microcapsule was investigated by confocal Raman spectroscopy. It was found that for III and IV, the intensity of signals due to functional groups was higher on the microcapsule surface than that in its core. Capsules based on alginate V had a uniform signal distribution over the entire cross section, but surface modification also took place. All three polymers were triazole derivatives. This fact allowed the authors to assume that this class of molecules can mitigate response of the organism to the foreign body owing to the inhibited activation of immune cells on the surface of materials and as a result the deterioration of fibrotic processes.
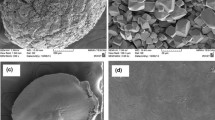
The best results on reduction in inflammation and fibrosis were exhibited by hydrogels based on derivative IV, which was used in further studies of the encapsulation of insulin producing cells. A mixture of derivative IV with the unmodified alginate at a weight ratio of 87 : 13 was employed for the encapsulation of β cells produced from human stem cells [87]. In accordance with the data on the rat islets of Langerhans encapsulated in the unmodified alginate gel [86], spherical capsules with a diameter of 1.5 mm were used. The resulting capsules had a heterogeneous structure with pore sizes in the range from <1 to 1–3 µm, which made it possible to avoid the penetration of cells and large proteins. The encapsulated cells were transplanted into the intraperitoneal space of immunocompetent C57BL/6J mice with induced type 1 diabetes. It was shown that these transplants induced glycemic correction without immunosuppression up to their retrieval 174 days after transplantation. The retrieved transplants contained viable insulin producing cells. These results are the first example of long-term glycemic correction with human β cells by the example of the immunocompetent model of animals with induced type 1 diabetes.
Later, derivative IV was also tested as a polymer for the encapsulation of allogeneic pancreatic islets of Langerhans in the nonhuman primate model [88]. Research was done on cynomolgus macaques. Capsules with pancreatic islets were prepared using a mixture of derivative IV and the unmodified alginate at a weight ratio of 79.5 : 20.5. Gel crosslinking was performed using barium ions. The obtained microcapsules were transplanted into the omental bursa of macaques. The use of capsules based on the chemically modified alginate IV in conjunction with the minimally invasive technique of transplantation into the omental bursa provided the viability and glucose sensitivity of encapsulated allogeneic islets for 4 months without the need for immunosuppressive therapy. Upon retrieval 1 and 4 months after transplantation no pericapsular fibrotic overgrowth on capsules obtained from IV was observed for six of seven animals. The average survival of the encapsulated islet cells was 93.5% 1 month and 90.0% 4 months after transplantation.
Using the ability of zwitter ionic polymers to reduce the nonspecific adsorption of protein and other blood serum and plasma components [89, 90] and to hinder the formation of a fibrous capsule on the surface of the hydrogel implant [91], the authors of [92] modified sodium alginate with zwitter ionic moieties. Sulfobetaine (VI) and carboxybetaine (VII) sodium alginate derivatives with different MW (25 × 103, (75–220) × 103, (200–300) × 103) and the content of guluronic acid moieties >60% were synthesized. The degree of functionalization relative to the initial alginate was 30.5% for derivative VI and 24.7% for derivative VII.

Experiments with barium-crosslinked cell-free capsules with a size of 500–700 µm showed that the modified hydrogels noticeably mitigate the excessive cellular overgrowth on alginate capsules compared with unmodified alginates for C57BL/6J mice (intraperitoneal implantation, retrieval after 14, 100, and 180 days), beagle dogs (intraperitoneal implantation, retrieval after 45 and 90 days), and Göttingen minipigs (implantation into omental bursa, retrieval after 1 month). The best results were obtained for hydrogels VI modified with sulfobetaine moieties. Afterwards, rat pancreatic islets encapsulated in this hydrogel (the capsule size, 800–1000 µm) were transplanted into immunocompetent C57BL/6J mice with induced type 1 diabetes. Microcapsules based on the modified alginate provided a much better long-term glycemic control up to 200 days compared with a maximum of 100 days for unmodified capsules. The characterization of retrieved microcapsules and islets confirms the ability of modified alginate microcapsules to attenuate fibrosis. Modified alginate encapsulated islets which were retrieved 200 days after transplantation were capable of secreting insulin. Moreover, the retrieved microcapsules were almost free of cellular overgrowth and fibrosis on the surface. The authors state that compared with the above-described approach (the schematic synthesis of sodium alginate derivatives), modification with zwitter ionic moieties is a much more facile and less expensive strategy for designing and development of superbiocompatible alginates.
Modification of alginate by moieties of compounds used in combined encapsulation. The combined encapsulation of pancreatic islets and anti-inflammatory and immunosuppressive drugs, including ketoprofen [93], contributes to softening of the immune response of the recipient organism and reduction in the degree of pericapsular fibrotic overgrowth after transplantation owing to drug release [94–96]. Using ketoprofen-functionalized alginate, it was shown that the covalent conjugation of the drug and its release during linkage hydrolysis under physiological conditions in the encapsulation of insulin producing cells can prolong this effect [97]. For this purpose, alginate derivatives containing ketoprofen conjugated to the hydroxyl groups of alginate by a PEGylated bridge via ester or amide linkages were synthesized:

A change in the ratio between the PEGylated ketoprofen derivative and alginate in the reaction allows the synthesis of derivatives with a degree of functionalization of 7 and 20%. Calcium-crosslinked cell-free capsules functionalized by ketoprofen via an ester linkage (diameter, 500–600 µm) demonstrated in vitro at physiological рН (7.4) a continuous release of the drug for 2 weeks without the explosive release of ketoprofen for the first hours after the formation of capsules. Under the same conditions for ketoprofen derivative with the amide linkage, only traces of the drug were released for 2 weeks because of a much lower rate of hydrolysis of the amide linkage. After 14 days, both types of cell-free alginate capsules still released ketoprofen. Capsules containing MIN6 pancreatic β cells which were produced from the ketoprofen derivative with the ester linkage released ketoprofen in vitro for the first 7 days at higher concentrations than cell-free capsules. This result can be explained by the presence of hydrolytic enzymes of the ester linkage in the cellular content. In general, the covalent binding of alginate with ketoprofen provides a longer drug release controlled by the rate of hydrolysis of the chemical linkage. To perform in vivo tests, cell-free capsules and capsules containing MIN6 cells were transplanted into immunocompetent mice either in the abdomen or under the renal capsule and subsequently retrieved after 30 days. A comparison with unmodified alginate capsules transplanted under the same conditions demonstrated evident reduction in the degree of pericapsular fibrotic overgrowth for capsules functionalized with ketoprofen. The effect was more distinct when the drug was covalently conjugated by the ester linkage. This made it possible to reach a higher concentration of the anti-inflammatory drug at the site of transplantation. The retrieved encapsulated cells were capable of producing insulin.
Along with publications aimed at decreasing the degree of capsule overgrowth by undesirable fibrous tissue, there are papers addressing factors promoting formation of a network of small vessels around a capsule which facilitates the supply of encapsulated cells with oxygen and nutrients. To initiate vascularization and angiogenesis in transplantation, a well-known protein, the vascular endothelial growth factor (VEGF), was used. VEGF was conjugated to alginate (Mw = 250 × 103), and the effects of VEGF chemically conjugated to alginate (IX) and the coencapsulated free VEGF on the angiogenesis and viability of encapsulated mouse pancreatic islets in allogeneic transplantation were compared [98]:

Encapsulation was performed using 1.4 wt % alginate IX solution with a content of chemically conjugated VEGF of 100 ng/mL, the maximum content of VEGF which did not worsen the properties of hydrogels. Hydrogels obtained from the modified alginates at the VEGF content above 200–250 ng/mL for the 1.4 wt % solution showed a sharp worsening of mechanical properties and could not form a fairly densely crosslinked shape-retentive hydrogel which could be transplantable. Chemical conjugation prevents the rapid release of VEGF and makes possible the local stimulation of vascularization. For the modified alginate hydrogel under in vitro conditions, no free VEGF was detected after 1 day and only 30% was released after 1 month owing to the slow hydrolysis of the linkage. The release of 90% free VEGF from the alginate hydrogel was observed for 24 h. Islet-free polymer IX gel disks with a thickness of 1 mm and a diameter of 5 mm were subcutaneously transplanted into C57BL/6 mice. Transplants retrieved after one month were coated with different size blood vessels with a calculated density of 13.87 vessel per 0.1 mm2, which was higher than the content of vessels in the neighboring normal tissue. For the reference alginate gel and the alginate gel with free VEGF of the same concentration, the calculated density was 1.66 and 0.47 vessel per 0.1 mm2, respectively. The pancreatic islets of healthy C57BL/6 mice encapsulated in these three hydrogels were subcutaneously transplanted into immunocompetent C57BL/6 mice with induced type 1 diabetes. Normoglycemia was attained for about 45 days for modified alginate and up to 15 days for both reference gels.
The extraction of pancreatic islets from the donor organism is associated with the destruction of their interactions with the extracellular matrix [9]. The addition of extracellular matrix proteins contributes to the survival and normal functioning of insulin producing cells [99–101]. At present, it is known that basic amino acid sequences are present in many proteins of the extracellular matrix and correspond to the adhesion of cells to it, for example, the common sequence of L-arginine, glycine, and L-aspartic acid, the so-called RGD fragment. The joint encapsulation of arginylglycylaspartic acid (RGD peptide) and a tripeptide corresponding to the RGD fragment [101] improves the survival and functioning of human pancreatic islets. The authors of [102] modified sodium alginate ((75–200) × 103; the content of guluronic acid fragments, ~68%) with the RGD peptide.

Derivative X was used for the encapsulation of pancreatic islet INS-1E β cells. To this end, a 2% alginate solution containing 200 µmol/L of chemically conjugated peptide was applied. The resulting cell-encapsulated microspheres (average diameter, 1270 µm) were transplanted into the neck subcutaneous space of type II diabetic Goto-Kakizaki rats and retrieved after 21 days.
The encapsulated cells improved the glycemic profile for rat diabetics within the entire time of the experiment. After retrieval, a thin collagen membrane surrounding transplanted hydrogels was observed on the capsules. This membrane was well vascularized and had many microvessels. After retrieval, transplanted β cells gave the positive insulin staining, which indicated their viability and functional activity. As opposed to the results obtained in vitro, in vivo INS-1E cells did not form pseudo-islet spheroids during transplantation into rats: only several INS-1E agglomerates were detected inside retrieved capsules.
Alginates functionalized by the RGD peptide were also synthesized by the effective two-step procedure in which alginate was oxidized by sodium m-periodate and subsequently functionalized by peptide via reductive amination using the nontoxic reducing agent 2-picoline-borane complex (pic-BH3) [103]. This procedure makes it possible to increase the degree of functionalization by peptides and does not result in N-acylurea binding to the alginate skeleton or formation of urea derivatives [104]. According to this technique, the authors of [104] synthesized alginates functionalized by peptides LRE, YIGSR, PDGEA, and PDSGR (XI) that were also responsible for the adhesion of cells to the extracellular matrix:

Alginates with a degree of functionalization of up to 8% which made possible the preparation of spherical microcapsules were tested. Using encapsulated pig pancreatic islets in vitro, it was shown that only the RGD-functionalized alginate increases survival and capability of glucose-stimulated insulin release.
Modification to Ensure Additional Crosslinking
Capsules with insulin producing cells belong to long-term transplants. In this case, a fairly rapid degradation of the shell required in the case of implant replacement by the regenerating body tissue in regenerative medicine leads to the impaired defense of transplanted cells and their loss. It was found that addition of the covalent crosslinking to the ionic one makes alginate gels more stable and can improve their mechanical behavior [105, 106]. Covalent crosslinking in alginate gels can be reached by several methods [107–110]. Among them are the photoinduced polymerization of groups specially introduced by functionalization of the raw materials of capsules [111, 112], addition of polymerizable monomers [113, 114], or the combination of these two approaches [115]. The first approach is mostly presented by studies with methacrylated sodium alginate [116, 117]. There are several techniques for introducing methacrylate moieties into alginate and subsequent photopolymerization during the encapsulation of cells [118, 119]. As applied to the encapsulation of insulin producing cells, the technique of obtaining methacylated alginate XII by the reaction with 2-aminoethyl methacrylate hydrochloride alginate and the use of the resulting polymer for the encapsulation of MIN6 β cells were described in [120]:

Alginate XII methacylated derivatives with a degree of functionalization of 0.31, 1.12, 2.19, 3.95, and 5.55% were synthesized. XII-based capsules with average diameters of 2560 and 1350 µm were obtained by drop extrusion in a calcium сhloride crosslinking solution followed by UV irradiation for 15 min in the presence of photoinitiator Irgacura 1173. Upon double crosslinking in vitro, the stability of capsules was enhanced without any signs of degradation even at the lowest degree of methacylation (0.31%) compared with the unmodified alginate demonstrating a rapid degradation of capsules. The basic level of insulin secretion for encapsulated MIN6 cells in vitro was higher for capsules with a degree of methacylation of 1.12%; however, differences between groups were not statistically significant. The survival of cells was above 95% 10 days after encapsulation for all alginates. To evaluate the stability of the methacrylated hydrogel in vivo, cell-free capsules based on methacrylated alginate (1.12%) were implanted into the omental bursa of Sprague Dawley rats jointly with a local injection of 5 µg of lipopolysaccharide to stimulate a strong inflammatory response. Transplants were retrieved after 1 and 3 weeks and subjected to histological analysis. After 1 week, a considerable inflammation and degradation of most nonmethacrylated alginate microcapsules were observed, whereas methacrylated capsules remained intact. Capsules with double crosslinking were stable for 3 weeks.
MIN6 cells were encapsulated in alginate hydrogels with the additional covalent crosslinking via disulfide linkages [121]. This type of covalent crosslinking is used more frequently for the targeted delivery of drugs [122, 123]. Sodium alginate derivatives containing thiol (XIII) (the degree of functionalization, 5.2–13.0%) or 1,2-dithiolane (XIV) (the degree of functionalization, 6.7–21.0%) functional groups were synthesized:

The preparation of double crosslinked capsules from these polymers does not require the use of photoinitiators. Capsules are formed by a rapid ionic gelation followed by a slow covalent crosslinking. Compared with unmodified alginates, gels with the disulfide bridge possess improved mechanical properties, specifically, better shape recovery after several compressions. For capsules with a diameter of 500 µm, the average survival of cells in vitro was 70% after 15 days; encapsulation in both gels in vitro had no effect on the ability of cells to secret insulin in response to glucose stimulation. For hydrogels with XIV (PEGylated bridge with n = 44), degradation in the medium of free cells was observed after 10 days. Cell-free capsules with a diameter of ~1000 µm were implanted into mouse peritoneum and retrieved after 30 days; there were no signs of inflammation and connective tissue or fibrosis formation (however, information about the integrity of capsules was absent).
There is a line of research focused on an increase in the stability of alginate hydrogels by the full replacement of ionic crosslinking linkages with covalent ones, including linkages between catechol moieties [124, 125]. In [126], mouse pancreas islet cells were first encapsulated in a hydrogel based on catechol-containing alginate (XV) crosslinked only via the dimerization of catechol moieties:

The resulting capsules were noncytotoxic ex vivo to islet cells for a long time. However, it was shown that encapsulation in the catechol-containing alginate considerably decreases glucose-stimulated insulin secretion. Eventually, the authors stated that it is undesirable to use catechol as a crosslinking moiety for alginate gelation in the encapsulation of islet cells and their transplantation. An increase in the adhesion ability of a hydrogel as a result of introducing catechol moieties may entail the formation of strong linkages between the gel surface and the cell membrane [127]. Therefore, the authors assumed that reduction in insulin secretion by cells encapsulated in the catechol-containing gel may be associated with the malfunction of membrane proteins of islet cells, such as glucose transporters, and ionic channels.
A facile and beautiful way of decreasing the degree of biodegradation is to include in a material chemical crosslinks formed by so-called bioorthogonal reactions, that is, chemical reactions that occur inside living systems and exert no effect on biochemical processes in them and their vital activity. These reactions do not proceed in living systems because living organisms lack enzymes specializing in the breakage of thus formed linkages. Therefore, bioorthogonal reactions are commonly used to improve the compatibility of implanted materials and to impart stability to them owing to prevention of degradation in the organism. K.M. Gatta’s-Asfura et al. [128] synthesized azide-containing alginate (XVI) (Mw = (200–300) × 103; the content of guluronic fragments, >60%) and used it to prepare alginate hydrogels with additional covalent crosslinking by the Staudinger bioorthogonal ligation:

The degree of functionalization with azide was varied from 3 to 13%. The functionalized polymer was capable of gelation in the presence of Ca2+ or Ba2+ cations. At the same time, interaction with calcium ions became weaker upon functionalization. For example, Ca2+ crosslinked granules of functionalized alginate dissolved at room temperature over 2 h during incubation in the phosphate buffered saline containing no Ca2+, whereas standard alginate capsules crosslinked by Ca2+ did not dissolve until >20 h under the same conditions. Furthermore, both Ba2+ crosslinked alginate hydrogels remained stable for several weeks during incubation in the phosphate buffered saline containing no Ba2+ or Ca2+ ions. Studies were performed using the azide-containing alginate with a degree of functionalization of 11%. Covalent crosslinking of the azide-containing alginate was performed using several crosslinkers [129]:

The authors of [129] synthesized two groups of hydrogels (capsule diameter, about 2.6 mm): the alginate gel crosslinked by Ca2+ or Ba2+ ions and the alginate gel crosslinked by ions Ca2+ or Ba2+ and ligated according to Staudinger. The degree of ligation was ~70% in 7 h for all crosslinkers. All the tested hydrogels showed better survival and proliferation of cells compared with the unmodified alginate.
According to the authors of [129], the alginate-based crosslinker XIX is the most promising one owing to its ability to mix well with the azide-functionalized alginate and to form covalent crosslinking without preliminary incubation, as well as the moderate proliferation of cells in capsules obtained using this alginate.
The authors of paper [130], which was published the same year as [129], examined the effect of encapsulation in the alginate gel crosslinked by crosslinker XVII on the survival and vital activity of MIN6 cells and rat and human pancreatic islets in vitro. The survival of all three encapsulants is comparable with that of the reference samples based on the unmodified alginate. However, for MIN6 cells, a statistically significant difference in metabolic activity was observed by day 7. For encapsulated islets, there was no substantial difference in the level of insulin secretion for all groups. Cell-free capsules with double crosslinking were less swellable and, in contrast to reference capsules, did not dissolve during exposure in an ethylenediaminetetraacetic acid solution. Later, the authors used this approach to obtain a thin three-layer coating [131] and a four-layer coating [132] for islet encapsulation.
CONCLUSIONS
Despite considerable limitations in reactions involving sodium alginate which are related to its insolubility in organic solvents and acidic aqueous solutions, a number of techniques for the synthesis of diverse functionalized alginates have been developed so far. The modifications of alginate for the microencapsulation of insulin-producing cells are predominantly performed via the carboxyl group. Currently, there are not many publications addressing the encapsulation of insulin producing cells in functionalized alginate gels. Owing to the scarce number of papers on preclinical trials and the absence of publications on the clinical trials of drugs, there is no unambiguous understanding of relationship between the character of alginate modification and its effect on the activity of encapsulated cells in vivo, and the immune response of the recipient organism upon transplantation is frequently unknown. However, as follows from the available data, the correctly chosen chemical modification of alginate can positively affect the ability of alginate gel capsules to hamper fibrous overgrowth and attenuate the influence of immune response on the capsule and can improve its stability and increase the biodegradation time compared with capsules based on the unmodified alginate. Further studies in this direction may contribute to removing barriers that now limit the extensive use of transplantation of encapsulated allogeneic insulin-producing cells for the treatment of type 1 diabetes.
REFERENCES
W. F. Ballinger and P. E. Lacy, Soc. Univ. Surg. 72, 175 (1972).
M. Y. Fan, W. R. Z. P. Lum, X. W. Fu, L. Levesque, I. T. Tai, and A. M. Sun, Diabetes 39, 192 (1990).
J. J. Altman, A. Houlbert, P. Callard, P. McMillan, B. A. Solomon, J. Rosen, and P. M. Galetti, Diabetes 6, 625 (1986).
E. Bekiari, K. Kitsios, and H. Thabit, BMJ [Br. Med. J.] 361, k131 (2018).
P. G. Jacobs, J. El Youssef, and R. Reddy, Diabetes, Obes. Metab. 18, 1110 (2016).
A. C. Gruessner and R. W. Gruessner, Curr. Opin. Organ Transplant. 21, 377 (2016).
J. Kim, K. Kang, C. J. Drogemuller, G. G. Wallace, and P. T. Coates, Curr. Diabetes Rep. 19 (8), 53 (2019).
M.-C. Vantyghem, E. J. P. de Koning, F. Pattou, and M. R. Rickels, Lancet 394 (10205), 1274 (2019).
A. R. Pepper, A. Bruni, and A. M. J. Shapiro, Curr. Opin. Organ Transplant. 23, 428 (2018).
N. M. Desai, J. A. Goss, S. Deng, B. A. Wolf, E. Markmann, M. Palanjian, A. P. Shock, S. Feliciano, F. C. Brunicardi, C. F. Barker, A. Naji, and J. F. Markmann, Transplantation 76, 1623 (2003).
N. Zhang, D. Su, S. Qu, T. Tse, R. Bottino, A. N. Balamurugan, J. Xu, J. S. Bromberg, and H. H. Dong, Diabetes 55, 2429 (2006).
A. D. Salama, K. L. Womer, and M. H. Sayegh, J. Immunol. 178, 5419 (2007).
B. L. Strand, A. E. Coron, and G. Skjak-Braek, Stem Cells Transl. Med. 6, 1053 (2017).
Transplantation, Bioengineering, and Regeneration of the Endorcine Pancreas, Ed. by G. Orlando, L. Piemonti, C. Ricordi, R. J. Stratta, and R. W. G. Gruessner (Acad. Press, Cambridge, 2020).
S. Hu and P. de Vos, Front. Bioeng. Biotechnol. 7, 134 (2019).
K. Y. Lee and D. J. Mooney, Prog. Polym. Sci. 37, 106 (2012).
C. J. Kearney and D. J. Mooney, Nat. Mater 12, 1004 (2013).
Polysaccharide Carriers for Drug Delivery, Ed. by S. Maiti and S. Jana (Woodhead Publ., Cambridge, 2019).
A. M. Rockstad, O. L. Brekke, B. Steinkjer, L. Ryan, G. Kollarikova, B. L. Strand, G. Skjak-Braek, J. D. Lambris, I. Lacik, T. E. Mollnes, and T. Espevika, Biomaterials 34, 621 (2013).
S. A. Safley, H. Cui, S. Cauffiel, C. Tucker-Burden, and C. J. Weber, J. Diabetes Sci. Technol. 2, 760 (2008).
M. Kollmer, A. A. Appel, S. I. Somo, and E. M. Brey, Tissue Eng., Part B 22, 34 (2015).
A. Mooranian, R. Negrulj, F. Arfuso, and H. Al-Salami, Artif. Cells Nanomed. Biotechnol. 44, 194 (2016).
R. M. Kleinberger, N. A. Burke, C. Zhou, and H. D. Stover, J. Biomater. Sci., Polym. Ed. 27, 351 (2016).
B. L. Strand, L. Ryan, P. In’t Veld, B. Kulseng, A. M. Rokstad, G. Skjåk-Bræk, and T. Espevik, Cell Transplant. 10, 263 (2001).
Carbohydrate Biotechnology Protocol, Ed. by C. Bucke (Humana Press, Totowa, 1999).
Alginates: Biology and Applications, Ed. by B. H. A. Rehm (Springer, Berlin; Heidelberg, 2009).
M. Otterlei, K. Østgaard, G. Skjåk-Bræk, O. Smidsrød, P. Soon-Shiong, and T. Espevik, J. Immunother. 10, 286 (1991).
M. Pervaiz, I. Ahmad, M. Yousaf, S. Kirn, A. Munawar, Z. Saeed, A. Adnan, T. Gulzar, T. Kamal, A. Ahmad, and A. Rashidal, Spectrochim. Acta, Part A 206, 642 (2019).
Y. A. Morch, I. Donati, and B. L. Strand, Biomacromolecules 8, 2809 (2007).
M. Qi, Y. Mørch, I. Lacík, K. Formo, E. Marchese, Y. Wang, K. K. Danielson, K. Kinzer, S. Wang, B. Barbaro, G. Kolláriková, D. Chorvát, Jr, D. Hunkeler, G. Skjåk-Bræk, J. Oberholzer, and B. L. Strand, Xenotransplantation 19, 355 (2012).
J. L. Drury, R. G. Dennis, and D. J. Mooney, Biomaterials 25, 3187 (2004).
A. Martinsen, G. Skjak-Braek, and O. Smidrsod, Biotechnol. Bioeng. 33, 79 (1989).
N. Emmerichs, J. Wingender, H.-C. Flemming, and C. Mayer, Int. J. Biol. Macromol. 34, 73 (2004).
I. Braccini and S. Pérez, Biomacromolecules 2, 1089 (2001).
P. Sikorski, F. Mo, G. Skjåk-Bræk, and B. T. Stokke, Biomacromolecules 8, 2098 (2007).
H. Hecht and S. Srebnik, Biomacromolecules 17, 2160 (2016).
A. Dodero, L. Pianella, S. Vicini, M. Alloisio, M. Ottonelli, and M. Castellano, Eur. Polym. J. 118, 586 (2019).
L. Iskandar, L. Rojo, L. Di Silvio, and S. Deb, J. Biomater. Appl. 34, 573 (2019).
R. J. Rodrigues and R. Lagoa, J. Carbohydr. Chem. 25, 219 (2006).
B. A. Harper, S. Barbut, L.-T. Lim, and M. F. Marcone, J. Food Sci. 79, E562 (2014).
M. Urbanova, M. Pavelkova, J. Czernek, K. Kubova, J. Vyslouzil, A. Pechova, D. Molinkova, J. Vyslouzil, D. Vetchy, and J. Brus, Biomacromolecules 20, 4158 (2019).
Y. A. Mørch, M. Qi, P. O. M. Gundersen, K. Formo, I. Lacik, G. Skjåk-Bræk, J. Oberholzer, B. L. Strand, J. Biomed. Mater. Res., Part A 100, 2939 (2012).
Y. A. Mørch, I. Donati, B. L. Strand, and G. Skjåk-Bræk, Biomacromolecules 7, 1471 (2006).
A. Haug and O. Smidsrod, Acta Chem. Scand. 24, 843 (1970).
S. Veriter, J. Mergen, R. M. Goebbels, N. Aouassar, C. Grégoire, B. Jordan, P. Levêque, B. Gallez, P. Gianello, and D. Dufrane, Tissue Eng., Part A 16, 1503 (2010).
S. K. Tam, J. Dusseault, S. Bilodeau, G. Langlois, J. P. Hallé, and L. H. Yahia, J. Biomed. Mater. Res., Part A 98, 40 (2011).
M. Otterlei, K. Ostgaard, G. Skjakbraek, O. Smidsrod, P. Soonshiong, and T. Espevik, J. Immunother. 10, 286 (1991).
U. Zimmermann, G. Klock, K. Federlin, K. Haning, M. Kowaslski, R. G. Bretzel, A. Horcher, H. Entenmann, U. Siebers, and T. Zekorn, Electrophores 13, 269 (1992).
G. Orive, S. Ponce, R. M. Hernandez, A. R. Gascon, M. Igartua, and J. L. Pedraz, Biomaterials 23, 3825 (2002).
S. Heiligenstein, M. Cucchiarini, M. W. Laschke, R. M. Bohle, D. Kohn, M. D. Menger, and H. Madry, Tissue Eng., Part C 17, 829 (2011).
J.-J. Chuang, Y.-Y. Huang, S.-H. Lo, T.-F. Hsu, W.‑Y. Huang, S.-L. Huang, and Y.-S. Lin, Int. J. Polym. Sci. 2017, Article ID 3902704 (2017).
A. I. Pravdyuk, Yu. A. Petrenko, N. A. Volkova, A. Yu. Petrenko, Biotekhnologiya, No. 3, 62 (2010).
T. M. S. Chang, Artif. Cells, Blood Substitutes, Biotechnol. 32, 1 (2004).
P. T. J. Hwang, D. K. Shah, J. A. Garcia, C. Y. Bae, D.-J. Lim, R. C. Huiszoon, G. C. Alexander, and H.‑W. Jun, Nano Convergence 3, Article No. 28 (2016).
T. B. Lopez-Mendez, E. Santos-Vizcaino, J. L. Pedraz, R. M. Hernandez, and G. Orive, Drug Discovery Today 26, 852 (2021).
Current Trends and Future Developments on (Bio-) Membranes: Membrane Desalination Systems: the Next Generation, Ed. by A. Basile and E. Curcio (Elsevier, Amsterdam; Oxford; Cambridge, 2018).
A. Murua, A. Portero, G. Orive, R. M. Hernández, M. de Castro, and J. L. Pedraz, J. Controlled Release 132, 76 (2008).
Cell Microencapsulation, Ed. by E. C.Opara (Springer, New York, 2017).
J. A. M. Steele, J.-P. Halle, D. Poncelet, and R. J. Neufeld, Adv. Drug Delivery Rev. 67–68, 74 (2014).
C. A. Hoesli, R. L. Kiang, D. Mocinecova, C. Donald-Hague, I. Lacík, T. J. Kieffer, and J. M. Piret, J. Biomed. Mater. Res., Part B 100, 1017 (2012).
C. Farias, R. Lyman, C. Hemingway, H. Chau, A. Mahacek, E. Bouzos, and M. Mobed-Miremadi, Bioengineering 5, 59 (2018).
M. P. Silva, F. L. Tulini, E. Martins, M. Penning, C. S. Favaro-Trindade, and D. Poncelet, LWT—Food Sci. Technol. 89, 392 (2018).
D. Yang, W. Wu, and S. Wang, Int. J. Polym. Mater. 67, 1087 (2018).
S. K. Boda, X. Li, and J. Xie, J. Aerosol Sci. 125, 164 (2018).
D. Headen, J. Garcia, and A. Garcia, Microsyst. Nanoeng. 4, 17076 (2018).
T. Rossow, P. S. Lienemann, and D. J. Mooney, Macromol. Chem. Phys. 218, 1600380 (2017).
B. R. Lee, J. W. Hwang, Y. Y. Choi, S. F. Wong, Y. H. Hwang, D. Y. Lee, and S.-H. Lee, Biomaterials 33, 837 (2012).
K. H. Lee, S.-H. Kim, J. H. Ryoo, S. F. Wong, and S.‑H. Lee, Lab Chip 11, 1168 (2011).
G. Choe, J. Park, H. Park, and J. Y. Lee, Polymers 10, 997 (2018).
A. R. Kang, J. S. Park, J. Ju, G. S. Jeong, and S.‑H. Lee, Biomaterials 35, 2651 (2014).
H. Zhang, E. Tumarkin, R. Peerani, Z. Nie, R. M. A. Sullan, G. C. Walker, and E. Kumacheva, J. Am. Chem. Soc. 128, 12205 (2006).
B. L. Ekerdt, C. M. Fuentes, Y. Lei, M. M. Adil, A. Ramasubramanian, R. A. Segalman, and D. V. Schaffer, Adv. Healthcare Mater. 7, 1800225 (2018).
A. M. Nikoo, R. Kadkhodaee, B. Ghorani, H. Razzaq, and N. Tucker, J. Microencapsulation 33, 605 (2016).
S. Rutkowski, T. Si, M. Gai, J. Frueh, and Q. He, RSC Adv. 8, 24243 (2018).
E. C. Opara, S.-H. Mirmalek-Sani, O. Khanna, M. L. Moya, and E. M. Brey, J. Invest. Med. 58, 831 (2010).
S. Tendulkar, S.-H. Mirmalek-Sani, C. Childers, J. Saul, E. Opara, and M. Ramasubramanian, Biomed. Microdevices 14, 461 (2012).
H.-T. Liu, H. Wang, W.-B. Wei, H. Liu, L. Jiang, and J.-H. Qin, Small 14, 1801095 (2018).
W. Chen, M. Lisowski, G. Khalil, I. R. Sweet, and A. Q. Shen, PLoS One 7, e33070 (2012).
S. Wiedemeier, F. Ehrhart, E. Mettler, G. Gastrock, T. Forst, M. M. Weber, H. Zimmermann, and J. Metze, Eng. Life Sci. 11, 165 (2011).
J.-S. Yang, Y.-J. Xie, and W. He, Carbohydr. Polym. 84, 33 (2011).
S. N. Pawar and K. J. Edgar, Biomaterials 33, 3279 (2012).
S. R. Banks, K. Enck, M. Wright, E. C. Opara,and M. E. Welker, J. Agric. Food Chem. 67, 10481 (2019).
A. Benettayeb, E. Guibal, A. Morsli, and R. Kessas, Chem. Eng. J. 316, 704 (2017).
C. Garía-Astrain and L. Avérous, Carbohydr. Polym. 190, 271 (2018).
A. J. Vegas, O. Veiseh, J. C. Doloff, M. Ma, H. H. Tam, K. Bratlie, J. Li, A. R. Bader, E. Langan, K. Olejnik, P. Fenton, J. W. Kang, J. Hollister-Locke, M. A. Bochenek, A. Chiu, S. Siebert, K. Tang, S. Jhunjhunwala, S. Aresta-Dasilva, N. Dholakia, R. Thakrar, T. Vietti, M. Chen, J. Cohen, K. Siniakowicz, M. Qi, J. McGarrigle, A. C. Graham, S. Lyle, D. M. Harlan, D. L. Greiner, J. Oberholzer, G. C. Weir, R. Langer, and D. G. Anderson, Nat. Biotechnol. 34, 345 (2016).
O. Veiseh, J. C. Doloff, M. Ma, A. J. Vegas, H. H. Tam, A. R. Bader, J. Li, E. Langan, J. Wyckoff, W. S. Loo, S. Jhunjhunwala, A. Chiu, S. Siebert, K. Tang, J. Hollister-Lock, S. Aresta-Dasilva, M. Bochenek, J. Mendoza-Elias, Y. Wang, M. Qi, D. M. Lavin, M. Chen, N. Dholakia, R. Thakrar, I. Lacík, G. C. Weir, J. Oberholzer, D. L. Greiner, R. Langer, and D. G. Anderson, Nat. Mater. 14, 643 (2015).
A. J. Vegas, O. Veiseh, M. Gürtler, J. R. Millman, F. W. Pagliuca, A. R. Bader, J. C. Doloff, J. Li, M. Chen, K. Olejnik, H. Hei Tam, S. Jhunjhunwala, E. Langan, S. Aresta-Dasilva, S. Gandham, J. J. McGarrigle, M. A. Bochenek, J. Hollister-Lock, J. Oberholzer, D. L. Greiner, G. C. Weir, D. A. Melton, R. Langer, and D. G. Anderson, Nat. Med. 22, 306 (2016).
M. A. Bochenek, O. Veiseh, A. J. Vegas, J. J. McGarrigle, M. Qi, E. Marchese, M. Omami, J. C. Doloff, J. Mendoza-Elias, M. Nourmohammadzadeh, A. Khan, C.-C. Yeh, Y. Xing, D. Isa, S. Ghani, J. Li, C. Landry, A. R. Bader, K. Olejnik, M. Chen, J. Hollister-Lock, Y. Wang, D. L. Greiner, G. C. Wei, B. Løkensgard Strand, A. M. A. Rokstad, I. Lacik, R. Langer, D. G. Anderson, and J. Oberholzer, Nat. Biomed. Eng. 2, 810 (2018).
S. Jiang and Z. Cao, Adv. Mater. 22, 920 (2010).
J. Ladd, Z. Zhang, S. Chen, J. C. Hower, and S. Jiang, Biomacromolecules 9, 1357 (2008).
L. Zhang, Z. Cao, T. Bai, L. Carr, J.-R. Ella-Menye, C. Irvin, B. D. Ratner, and S. Jiang, Nat. Biotechnol. 31, 553 (2013).
Q. Liu, A. Chiu, L.-H. Wang, D. An, M. Zhong, A. M. Smink, B. J. de Haan, P. de Vos, K. Keane, A. Vegge, E. Y. Chen, W. Song, W. F. Liu, J. Flanders, C. Rescan, L. Groth Grunnet, X. Wang, and M. Ma, Nat. Commun. 10, 5262 (2019).
M. Ricci, P. Blasi, S. Giovagnoli, C. Rossi, G. Macchiarulo, G. Luca, G. Basta, and R. Calafiore, J. Controlled Release 107, 395 (2005).
S. A. Azadi, E. Vasheghani-Farahani, S. Hashemi-Najafbabadi, and A. Godini, Prog. Biomater. 5, 101 (2016).
T. Dang, A. V. Thai, J. Cohen, J. E. Slosberg, K. Siniakowicz, J. C. Doloff, M. Ma, J. Hollister-Lock, K. M. Tang, Z. Gu, H. Cheng, G. C. Weir, R. Langer, and D. G. Anderson, Biomaterials 34, 5792 (2013).
H.-S. Park, J.-W. Kim, S.-H. Lee, H. K. Yang, D.‑S. Ham, C.-L. Sun, T. H. Hong, G. Khang, C.‑G. Park, and K.-H. Yoon, J. Tissue Eng. Regener. Med. 11, 1274 (2017).
F. Noverraz, E. Montanari, J. Pimenta, L. Szabo, D. Ortiz, C. Gonelle-Gispert, L. H. Buhler, S. Gerber-Lemaire, Bioconjugate Chem. 29, 1932 (2018).
N. Yin, Y. Han, H. Xu, Y. Gao, T. Yi, J. Yao, L. Dong, D. Cheng, and Z. Chen, Mater. Sci. Eng., C 59, 958 (2016).
S. E. Townsend and M. Gannon, Endocrinology 160, 1885 (2019).
J. Daoud, M. Petropavlovskaia, L. Rosenberg, and M. Tabrizian, Biomaterials 31, 1676 (2010).
A. Llacua, B. J. de Haan, S. A. Smink, and P. de Vos, J. Biomed. Mater. Res., Part A 104, 1788 (2016).
J. Crisóstomo, A. M. Pereira, S. J. Bidarra, A. C. Gonçalves, P. L. Granja, J. F. J. Coelho, C. C. Barrias, R. Seiça, J. Appl. Biomater. Funct. Mater. 17, 2280800019848923 (2019).
J. D. Medina, M. Alexander, M. D. Hunckler, M. A. Fernández-Yagüe, M. M. Coronel, A. M. Smink, J. R. Lakey, P. de Vos, and A. J. García, Adv. Healthcare Mater. 9, 2000102 (2020).
I. Sandvig, K. Karstensen, A. M. Rokstad, F. L. Aachmann, K. Formo, A. Sandvig, G. Skjåk-Bræk, and B. Løkensgard Strand, J. Biomed. Mater. Res., Part A 103, 896 (2015).
S. Birnbaum, R. Pendleton, P.-O. Larsson, and K. Mosbach, Biotechnol. Lett. 3, 393 (1981).
K. Y. Lee, J. A. Rowley, P. Eiselt, E. M. Moy, K. H. Bouhadir, and D. J. Mooney, Macromolecules 33, 4291 (2000).
D. Nataraj and N. Reddy, Int. J. Chem. Res 4, 1 (2020).
E. Kim, M. H. Kim, J. H. Song, C. Kang, W. H. Park, Int. J. Biol. Macromol. 154, 989 (2020).
H. Sánchez-Morán, A. Ahmadi, B. Vogler, and K. H. Roh, Biomacromolecules 20, 4419 (2019).
C. T. Moody, S. Palvai, and Y. Brudno, Acta Biomater. 112, 112 (2020).
E. E. Coates, C. N. Riggin, and J. P. Fisher, J. Biomed. Mater. Res., Part A 101, 1962 (2013).
A. Mignon, D. Devisscher, G. J. Graulus, B. Stubbe, J. Martins, P. Dubruel, N. De Beliea, and S. Van Vlierberghe, Carbohydr. Polym. 155, 448 (2017).
Q. Zhou, H. Kang, M. Bielec, X. Wu, Q. Cheng, W. Wei, and H. Dai, Carbohydr. Polym. 197, 292 (2018).
D. Zhao, C. Tie, B. Cheng, S. Yang, X. Wang, Z. Sun, M. Yinc, H. Zhud, and M. Yin, Polym. Degrad. Stab. 179, 109297 (2020).
J. Zhao, X. Zhao, B. Guo, and P. X. Ma, Biomacromolecules 15, 3246 (2014).
Y. Gao and X. Jin, Mar. Drugs 17, 557 (2019).
F. Araiza-Verduzco, E. Rodriguez-Velázquez, H. Cruz, I. A. Rivero, D. R. Acosta-Martínez, G. Pina-Luis, and M. Alatorre-Meda, Materials 13, 534 (2020).
A. D. Rouillard, C. M. Berglund, J. Y. Lee, W. J. Polacheck, Y. Tsui, L. J. Bonassar, and B. J. Kirby, Tissue Eng., Part C 17, 173 (2011).
C. Mu, S. Sakai, H. Ijima, and K. Kawakami, J. Biosci. Bioeng. 109, 618 (2010).
S. I. Somo, K. Langert, C.-Y. Yang, M. K. Vaicik, V. Ibarra, A. A. Appel, B. Akar, M.-H. Cheng, and E. M. Brey, Acta Biomater. 65, 53 (2018).
S. Passemard, L. Szabó, F. Noverraz, E. Montanari, C. Gonelle-Gispert, L. Bühler, C. Wandrey, and S. Gerber-Lemaire, Biomacromolecules 18, 2747 (2017).
A. D. Ayub, H. I. Chiu, S. N. A. Mat Yusuf, E. Abd Kadir, S. H. Ngalim, and V. Lim, Artif. Cells, Nanomed., Biotechnol. 47, 353 (2019).
Bioadhesives in Drug Delivery, Ed. by K. L. Mittal, I. S. Bakshi, and J. K. Narang (Wiley-Scrivener, Hoboken, 2020).
C. Lee, J. Shin, J. S. Lee, E. Byun, J. H. Ryu, S. H. Um, D.-I. Kim, H. Lee, and S.-W. Cho, Biomacromolecules 14, 2004 (2013).
S. H. Hong, M. Shin, J. Lee, J. H. Ryu, S. Lee, J. W. Yang, W. D. Kim, and H. Lee, Adv. Healthcare Mater. 5, 75 (2016).
Y.-S. Kim, S.-W. Cho, B. Ko, J. Shin, and C. W. Ahn, Diabetes Metab. J. 42, 164 (2018).
J. Hou, C. Li, Y. Guan, Y. Zhang, and X. X. Zhu, Polym. Chem. 6, 2204 (2015).
K. M. Gattás-Asfura and C. L. Stabler, Biomacromolecules 10, 3123 (2009).
K. K. Hall, K. M. Gattas-Asfura, and C. L. Stabler, Acta Biomater. 7, 614 (2011).
K. M. Gattás-Asfura, C. A. Fraker, and C. L. Stabler, J. Biomed. Mater. Res., Part A 99, 47 (2011).
K. M. Gattas-Asfura and C. L. Stabler, ACS Appl. Mater. Interfaces 5, 9964 (2013).
K. M. Gattás-Asfura, N. J. Abuid, I. Labrada, and C. L. Stabler, ACS Biomater. Sci. Eng. 6, 2641 (2020).
Funding
This work was supported by the Ministry of Public Health of the Russian Federation (State Assignment АААА-А20-120022590096-6, theme Development of Pancreatic Islet Encapsulation Technology for Compensation of Absolute Insulin-Deficient States).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Additional information
Translated by T. Soboleva
Rights and permissions
About this article
Cite this article
Len’shina, N.A., Konev, A.N., Baten’kin, A.A. et al. Alginate Functionalization for the Microencapsulation of Insulin Producing Cells. Polym. Sci. Ser. B 63, 640–656 (2021). https://doi.org/10.1134/S1560090421060129
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S1560090421060129