Abstract
Clinical and laboratory examination was performed for 50 patients with ankylosing spondylitis (AS) (mean age 38.1 ± 1.3 years) with degree II of general activity of the pathological process and disease history of 1–8 years (mean BASDAI score 3.6 ± 0.2). Close relationships between the level of oxidative stress, the severity of low-intensity inflammation, and the activity of the humoral component of anti-endotoxin immunity were observed in the active phase of AS, implicating endotoxin aggression of intestinal origin in disease pathogenesis. Based on cluster analysis, a deficiency of class M anti-endotoxin antibodies was associated with a higher level of oxidative stress and low-intensity inflammation in the AS patients. Medical procedures and drugs that can normalize systemic endotoxemia were therefore considered advisable to include in AS treatment. The anti-endotoxin component of the treatment is expected to increase the treatment efficacy and to reduce the need for cytostatics and, therefore, their iatrogenic side effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Ankylosing spondylitis (AS), or Bechterew’s disease, is a main nosological form of seronegative spondyloarthropathies, the incidence of which ranges from 0.15 to 1.4% in European countries and is tightly associated with the HLA-B27 genetic marker in the European population. AS is usually diagnosed before age 45 and is 2–3 times more frequent in men than in women. Stable and early disability characteristic of AS and a continuously increasing AS incidence render the disease highly important both socially and economically [1]. Recent studies have shown that immune disorders play a substantial role in AS origin and development, determine the inflammatory component of the AS pathogenesis, and are mainly due to a shift towards proinflammatory cytokines in the cytokine profile [2]. Excess production of these mediators is commonly thought to determine inflammatory processes in the gastrointestinal (GI) tract, and GI inflammation is an important extra-articular manifestation of AS [3]. Nonsteroidal anti-inflammatory drugs and cytostatic agents are used as first-line therapy for AS. The drugs to treat AS are administered for extended (nearly life-long) periods of time and at maximal therapeutic doses, which is an additional risk factor of GI complications [4]. Thus, AS patients are substantially predisposed to impaired integrity of the intestinal barrier; excess release of the intestinal endotoxin (ET) into circulation; and ET aggression, which can induce autoimmune processes [5] and act as a primary factor of AS pathogenesis. The inflammatory response determines, to a great extent, the integral effect of ET on the body, and its intensity and pathogenetic significance greatly depend on the state of anti-ET immunity [6]. The latter idea is supported by data from our study of acantholytic vesicular dermatitis patients; i.e., a deficit of class M anti-ET antibodies is tightly associated with activation of chronic low-intensity inflammation [7]. The finding indicates that a lower adaptive immune response to enterobacterial ET is possible to consider as a key factor that facilitates the proinflammatory effect of ET aggression. Consequently, the objective of this work was to study the relationship between the activity of the low-intensity inflammatory process, the level of oxidative stress, and the state of anti-ET immunity in AS patients.
METHODS
A study sample included 50 AS patients (40 males and 10 females, mean age 38.1 ± 1.3 years) with degree II of general activity of the pathological process (mean BASDAI score 3.6 ± 0.2) and disease history of 1–8 years. The patients were examined during a hospitalization to the Rheumatology Department of Semashko Republican Clinical Hospital (Simferopol). The AS diagnosis was established according to American College of Rheumatology guidelines (2015). All patients had clinical and X-ray signs of sacroiliac disease and chronic inflammatory GI complications (gastritis and ulcerative colitis). Patients with comorbidities involving the cardiovascular, endocrine, central nervous, and peripheral nervous systems were not included in the study. All AS patients received standard drug therapy, including disease-modifying drugs and symptomatic treatments. A control group included healthy volunteers (n = 25), who matched the AS patients in age and sex, had no history of chronic disorders and no sign of acute infection at the time of examination.
Venous blood serum and saliva samples were collected by standard procedures and stored at −25°C for no more than 6 months. Class A, M, and G anti-ET antibodies (ET-ABs) in the blood serum and secretory class A ET-ABs in saliva were measured by ELISA [8]. Commercial Escherichia coli K235 ET (Sigma, United States) was used as an antigen.
Total blood immunoglobulins of classes A, M, and G (IgA, IgM, and IgG); total salivary secretory IgA; and serum C-reactive protein were assayed by ELISA with commercial kits (Vektor-BEST, Russia). Oxidative modification of serum proteins (OMP) was assessed spectrophotometrically, using the reaction of 2,4-diphenyl hydrazine (Sigma, United States) with carbonyl groups of oxidized proteins [9]. The reaction product 2,4-dinitrophenyl hydrazone was measured using a UV/VIS NanoPhotometer P360 spectrophotometer (Implen, Germany).
Statistical analyses of the results were performed using the software package STATISTICA 6.0 (StatSoft, United States). All numerical data were presented as the median (Me) and the first and third quartiles (Q1 and Q3). Differences between independent samples were tested for significance by the nonparametric Mann–Whitney U-test and considered significant at p < 0.05. Associations between parameters were assessed using Spearman’s rank correlation coefficient. Cluster analyses were carried out by the McKinsey iterative k-means method.
RESULTS AND DISCUSSION
Laboratory testing showed (Table 1) that the serum content of class M ET-ABs in the AS patients was generally significantly lower than in the controls (by 34.3% on average, p < 0.001), while the levels of class A and class G ET-ABs in the patients did not significantly differ from the respective reference values. Given that glucocorticoids are used to treat AS and can induce systemic immunosuppression [10], total blood concentrations of IgA, IgM, and IgG were measured in the patients to obtain an integral characteristic of B-cell immunity (Table 2). The total IgM concentration in the AS patients was significantly higher than in the controls (by 46.6%, p < 0.001), while total IgA and total IgG did not significantly differ from the respective reference values. Statistical analyses with Spearman’s rank correlation coefficient r showed that the serum levels of ET-ABs of various classes did not significantly correlate with the serum contents of total immunoglobulins of the respective classes in the AS patients. Thus, imbalanced levels of serum ET-ABs of different classes did not reflect systemic changes in humoral immunity in the AS patients.
The salivary total secretory IgA concentration in the AS patients was, on average, 21.5% lower than in the control subjects (p < 0.05), while the salivary level of secretory class A ET-ABs in the patients were higher than normal by 28.0% on average (p < 0.05) (Table 3). The salivary concentration of total secretory IgA did not correlate with the level of secretory class A ET-ABs in the AS patients. Secretory IgA is an important effector molecule of mucosal immunity and plays a key role in protecting mucous membranes from being invaded and colonized by pathogenic bacteria, viruses, and protozoans. An imbalance of the factors involved in anti-ET immunity is therefore possible to consider as a consequence of the impaired barrier function of the intestine in the AS patients. A greater amount of ET finds its way into the body interior to cause the anti-ET adaptive immune response, which is a compensatory reaction to the increasing antigenic load.
Our study showed that chronic low-intensity inflammation and free-radical oxidation of proteins were significantly intensified in the AS patients (Table 4). The C-reactive protein and OMP serum concentrations of the AS patients were, respectively, 3.1 and 2.3 times higher than the reference values on average (p < 0.001). It should be noted that the finding agrees well with published data that the OMP concentration in the blood is elevated in AS patients and is directly associated with BASDAI score [11].
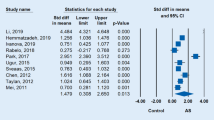
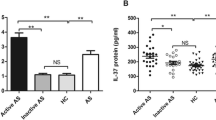
A cluster analysis showed two clusters (conventionally designated AS-1 and AS-2) in our sample of AS patients. Associations of imbalanced anti-ET immunity, chronic low-intensity inflammation, and free-radical oxidation of proteins were observed within each cluster (Fig. 1, Table 5).
Associations between the serum levels of ET-ABs of various classes, C-reactive protein (CRP), and OMP in the AS patients of different clusters (McKinsey iterative k-means method): a, cluster AS-1; b, cluster AS-2; (*) difference from the reference value was significant; (#) difference between the clusters was significant.
Cluster AS-1 included 23 AS patients (46.0% of the total patient sample). The class M ET-AB levels in these patients were 2.4 times lower than in the control healthy subjects on average, while the C-reactive protein and OMP concentrations in the blood were, respectively, 4.7 and 2.9 times higher than the reference values (p < 0.001). At the same time, a higher level of class A secretory ET-ABs and a lower concentration of total secretory IgA in the saliva were observed in the AS patients of the cluster as compared with the control group (the differences were 43.5% and 40.3%, respectively, on average; p < 0.01).
Cluster AS-2 included 27 AS patients (54.0% of the total sample). Their serum levels of antibodies of various classes, secretory class A ET-ABs, and total secretory IgA in the saliva did not significantly differ from the reference values, while the C-reactive protein and OMP concentrations in the blood were, respectively, 2.2 and 2.3 times higher than in the healthy controls on average. An analysis of differences between clusters AS-1 and AS-2 showed that the AS-1 patients had significantly lower levels of class M ET-ABs (by 56.0% on average), virtually normal levels of class A ET-ABs, and significantly higher levels of class G ET-ABs (by 80.9% on average). The C-reactive protein and OMP concentrations of the AS-1 patients were, respectively, 2.1 times and 28.3% higher than in the AS-2 patients on average.
CONCLUSIONS
Our study showed that, in the AS patients, an imbalance of various components of anti-ET immunity is tightly associated with activation of chronic low-intensity inflammation and more intense free-radical oxidation, which is accompanied by generation of reactive oxygen species (ROS). ROS are highly reactive and damage various biomolecules. The ROS production rate and activities of antioxidant systems of the body are in dynamic equilibrium in physiological conditions. Distortion of the equilibrium leads to oxidative stress [12], which provides a pathogenetic basis for the development and progression of many diseases [13], including AS [14]. The diseases are accompanied by OMP accumulation in the blood. Activation of innate immunity effector cells (tissue macrophages and granulocytes) may be a leading cause of higher ROS production, and ET acts as an inducer of this activation [15].
Thus, a tight association between the level of oxidative stress, chronic low-intensity inflammation, and a distorted adaptive immune response to enterobacterial ET is characteristic of AS patients according to the results of our study. The association suggests an important, if not triggering, role in the disease pathogenesis for the intestinal factor. Drugs that normalize systemic endotoxemia are known to improve the efficacy of therapy in many diseases [5, 16, 17] and can be recommended for use in AS. This may be expected to substantially reduce the need in cytostatic agents, to decrease their iatrogenic effects, and to substantially improve the treatment efficacy and life quality of AS patients.
REFERENCES
Dean, L.E., Jones, G.T., MacDonald, A.G., et al., Global prevalence of ankylosing spondylitis, Rheumatology, 2014, vol. 53, no. 4, p. 650.
Erdes, Sh.F., Interleukin 17a—a new target for anticytokine therapy in ankylosing spondylitis, Nauchno-Prakt. Revmatol., 2016, vol. 54, suppl. 1, p. 60.
Zarco, P., Gonzalez, C., Rodriguez de la Serna, A., et al., Extra-articular disease in patients with spondyloarthritis: baseline characteristics of the spondyloarthritis cohort of the AQUILES study, Reumatol. Clin., 2015, vol. 11, no. 2, p. 83.
Kunder, E.V., Treatment of patients with ankylosing spondylitis, Mezhdunar. Obz.: Klini. Prakt. Zdorov’e, 2013, no. 4, p. 55.
Yakovlev, M.Yu., Sistemnaya endotoksinemiya: gomeostaz i obshchaya patologiya (Systemic Endotoxinemia: Homeostasis and General Pathology), Moscow: Nauka, 2021.
Cross, A.S., Anti-endotoxin vaccines: back to the future, Virulence, 2014, vol. 5, no. 1, p. 219.
Gordienko, A.I., Beloglazov, V.A., Kubyshkin, A.V., et al., Humoral anti-endotoxin immunity imbalance as a probable factor in the pathogenesis of autoimmune diseases, Hum. Physiol., 2019, vol. 45, no. 3, p. 337. https://doi.org/10.1134/S036211971903006X
Gordienko, A.I., The use of enzyme-linked immunosorbent assay to determine human total and antiendotoxin secretory IgA, Tavricheskii Med.-Biol. Vestn., 2009, vol. 12, no. 3(47), p. 82.
Dubinina, E.E., Burmistrov, S.O., Khodov, D.A., and Porotov, I.G., Oxidative modification of human blood serum proteins, method for its determination, Vopr. Med. Khim., 1995, no. 1, p. 24.
Han, A., A practical approach to treating autoimmune bullous disorders with systemic medications, J. Clin. Aesthet. Dermatol., 2009, vol. 2, no. 5, p. 19.
Yazici, C., Köse, K., Calis, M., et al., Protein oxidation status in patients with ankylosing spondylitis, Rheumatology (Oxford), 2004, vol. 43, no. 10, p. 1235.
Lushchak, V.I., Environmentally induced oxidative stress in aquatic animals, Aquat. Toxicol., 2011, vol. 101, no. 1, p. 13.
Martínez-Sánchez, G., Giuliani, A., Pérez-Davison, G., and León-Fernández, O.S., Oxidized proteins and their contribution to redox homeostasis, Redox Rep., 2005, vol. 10, no. 4, p. 175.
Feijóo, M., Túnez, I., Tasset, I., et al., Infliximab reduces oxidative stress in ankylosing spondylitis, Clin. Exp. Rheumatol., 2009, vol. 27, no. 1, p. 167.
Kadiiska, M.B., Peddada, S., Herbert, R.A., et al., Biomarkers of oxidative stress study: VI. Endogenous plasma antioxidants fail as useful biomarkers of endotoxin-induced oxidative stress, Free Radic. Biol. Med., 2015, vol. 81, p. 100.
Anikhovskaya, I.A., Beloglazov, V.A., Gordienko, A.I., et al., A brief history of the study of the role of gut in aging and/or induction of systemic inflammation: achievements, challenges, Patogenez, 2019, vol. 17, no. 1, p. 4.
Anikhovskaya, I.A., Kubatiev, A.A., Maiskii I.A., et al., Search directions for tools to reduce endotoxin concentration in the general hemocirculation, Patogenez, 2014, vol. 12, no. 4, p. 25.
ACKNOWLEDGMENTS
We are grateful to researchers of the Central Research Laboratory, Vernadsky Crimean Federal University (Simferopol).
Funding
This work was supported by third-party organizations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Statement of Compliance with Standards of Research Involving Humans as Subjects
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments and were approved by the local Ethics Committee at Vernadsky Crimean Federal University (Simferopol). All individual participants involved in the study gave their informed consent for participation after being informed about the potential risks and benefits and the study nature.
Conflict of Interests
The authors declare that they have no conflict of interest.
Additional information
Translated by T. Tkacheva
Rights and permissions
About this article
Cite this article
Gordienko, A.I., Beloglazov, V.A., Anikhovskaya, I.A. et al. Activity of Humoral Antiendotoxin Immunity Is Associated with Low-Intensity Inflammation and Oxidative Stress in Ankylosing Spondylitis: Endotoxin Component of Disease Pathogenesis. Hum Physiol 48, 577–581 (2022). https://doi.org/10.1134/S0362119722600230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119722600230