Abstract
Introduction: Systemic thrombolytic therapy (STLT) with recombinant tissue plasminogen activator (rtPA) is the “gold standard” of reperfusion therapy in certain patients with ischemic stroke during the first 4.5 h after stroke onset. Objective: To assess the clinical (severity of neurological symptoms) and laboratory (complete blood cell count test) factors that affect the disease outcome after STLT. Materials and methods: Seventy patients (48 males and 22 females) aged 61 [54; 69] years with ischemic stroke who received rtPA therapy at a dose of 0.9 mg/kg were prospectively studied. Blood for the complete blood count test including neutrophil and lymphocyte counts was sampled before the thrombolytic therapy. The severity of neurological impairment was assessed using the NIH Stroke Scale (NIHSS). The functional outcome was assessed 3 months after stroke with the modified Rankin scale (mRS). ROC analysis was used to reveal factors of unfavorable outcome in acute phase of ischemic stroke (mRS score ≥ 3). Results: Severity of neurological deficit was assessed according to the NIHSS at admission was 15 [11; 17] points. Time between the manifestation of neurological symptoms and admission to the hospital was 138 [117; 170] min, and time between admission and initiation of STLT (the door-to-needle time), was 40 [30; 55] min. An unfavourable functional outcome of systemic thrombolytic therapy can be predicted according to the results of ROC analysis: the NIHSS score upon admission 12 or higher (sensitivity, 94%; specificity, 57%); neutrophil count, >7.8 × 109/L (sensitivity, 45.5%; specificity, 90.6%); lymphocyte count < 1.8 × 109/L (sensitivity, 81.8%; specificity, 59.4%). Conclusions: Personalized approach to systemic thrombolytic therapy may help to predict its effectiveness and contribute the development of more reliable strategies of patient management. Patients with potentially unfavorable outcome after intravenous thrombolysis can be the target group for mechanical reperfusion techniques such as thrombus extraction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Despite the diversity of approaches for the treatment of patients with ischemic stroke (IS), only five strategies have a high class (I) and a level of evidence (A) with respect to the outcome: admission of patients with suspected stroke to the hospitals with departments for patients with acute cerebrovascular disorders (AVC); administration of acetylsalicylic acid in the first 48 hours after the onset of the first symptoms; STLT with recombinant tissue plasminogen activator (rtPA) to appropriate patients in the first 4.5 h after the IS; mechanical extraction of the thrombus with stent retrievers in the first 6 post-stroke hours in patients with confirmed occlusion of the internal carotid artery (ICA) or proximal segments (segment M1) of the middle cerebral artery (MCA); decompressive hemicranectomy for the treatment of cerebral edema manifesting in occlusion of the main CMA lumen during the first 48 h after the IS.
STLT remains the “gold standard” of reperfusion therapy. Thus, when considering the possibility of performing endovascular reperfusion therapies in patients fitting the criteria for systemic thrombolysis, it is necessary to perform rtPA treatment, according to the North American guidelines on treatment of acute stroke updated in 2015 [1].
For the first time in Russia STLT with the administration of rtPA was put into practice in the Institute of cerebrovascular pathology and stroke of the N.I. Pirogov Russian State Medical University on the basis of the City Clinical Hospital no. 31 in 2005–2006 [2], since 2008 it has been performed in the Research Center of Neurology [3–5]. The method of STLT was approved by the Federal Supervisory Agency for Health Care and Social Development as an advanced medical technology (authorization for the new medical technology: FS no. 2008/169 dated 01.08.2008). Since 2008 thrombolysis has been an integral part of providing medical care to patients with stroke in primary vascular units and regional vascular centers established under the program on the vascular diseases mortality reduction [6, 7].
The procedure of thrombolytic therapy is regulated by the Order of the Russian Ministry of Health “Approval of the medical care provision procedure to patients with AVC” no. 389n dated July 6, 2009 (amended Orders of the Russian Ministry of Health no. 44n dated February 2, 2010 and no. 357n dated April 27, 2011), and by the Order of the Russian Ministry of Health no. 928n dated November 15, 2012 “Approval of the medical care provision procedure to patients with AVC”. In 2014, the All-Russian Society of Neurologists issued the Russian Guidelines on Thrombolysis in Ischemic Stroke (www.neurologia.info).
The invention of the new generation devices for the thrombectomy (Solitaire), as well as the improvement of the protocols for endovascular interventions, led to a revision of the strategy of patient management in IS caused by occlusion of the proximal part of the intracranial arteries. The results of 5 controlled studies that proved the efficacy and safety of the combination of rtPA therapy with subsequent endovascular intervention (primarily mechanical thrombus extraction/ thrombectomy) were published in 2015.
Taking into account the positive results of the above-mentioned studies, in 2015, AHA-ASA guidelines for the treatment of patients in the acute period of stroke were updated. Thus, in an appropriate patient with IS if the occlusion of the ICA or M1 segment of the MCA is confirmed after systemic thrombolytic therapy a performance of mechanical thrombus extraction with stent retrievers is recommended in the first 4.5 h (Class I, Level of Evidence A). Indications for mechanical thrombectomy are as follows: functional independence of the patient (0–1 point on the modified Rankine scale (mRS)) before stroke; age over 18 years; 6 or more points on the stroke scale of the National Institutes of Health of the United States (NIHSS), 6 or more points on the ASPECTS scale (prevalence of cerebral ischemia according to CT); the technical possibility of arterial puncture in the first 6 hours after stroke (Class I, level of evidence A).
When intravenous thrombolysis is contraindicated (patients with past history of stroke, patients taking oral anticoagulants, etc.) mechanical thrombectomy is also possible within the first 6 hours (Class IIa, level of evidence C). Endovascular interventions in appropriate patients with IS in the first 6 hours beyond the above indications (Class IIb) can be considered: if occlusion of arteries of smaller diameter (segments M2, M3 of the MCA, anterior or posterior cerebral artery) (evidence level C) occurs, IS due to the occlusion of the ICA or M1 of the MCA segment in patients with a functional independence level before the stroke of more than 1 point on the mRS scale, as well as with score on NIH and ASPECTS stroke scales of less than 6 (level of evidence B).
It should be emphasized that in any clinical situation when patient meets the criteria for systemic thrombolysis, it is necessary to perform this type of therapy, even if subsequent endovascular treatment is considered (Class I, level of evidence A) [1].
The careful adherence to the protocol is fundamental to the success and safety of reperfusion therapy. However, as with any treatment, it is possible to identify factors of favorable outcome or failure.
The goal of the current study is to reveal factors both the clinical (severity of neurologic symptoms on admission) and laboratory (blood count test) that probably impact on the outcome of systemic thrombolytic therapy.
MATERIALS AND METHODS
We prospectively observed 70 patients (48 men and 22 women) aged 32 to 76 years (mean age 61 [54, 69] years) with IS who underwent therapy with rtPA at a dose of 0.9 mg/kg performed according to the Russian and international guidelines.
After thrombolysis all patients received conventional therapy which included hemodilution, hypoglycemic therapy, hypotensive therapy; antiplatelet therapy with acetylsalicylic acid administered 24 hours after the symptoms development; anticoagulant therapy with low molecular weight heparins (patients with pronounced motor impairment 48 hours after the onset of IS for prevention of venous thromboembolic complications) and oral anticoagulants (patients with cardiogenic embolic stroke after 7–14 days); neurometabolic therapy; lipid-lowering therapy (statins), early rehabilitation.
All patients enrolled in the study underwent magnetic resonance imaging (MRI) performed with a Magnetom Symphony (Siemenes, Germany) MRI scanner with a magnetic field density of 1.5 T. The study was performed in the coronary, sagittal and axial planes in standard modes (T1, T2-weighted images (T1-VI, T2-VI), T2-FLAIR, T2*-weighted images (T2*-VI)), diffusion-weighted MRI (DW-MRI) was also included. The images were processed with eFilm Workstation medical imaging program. Imaging was performed before and 24 hours after the STLT.
Severity of neurologic deficit was assessed with the NIH stroke scale. The functional outcome was assessed 3 months after a stroke with the mRS scale. A favorable outcome of stroke was considered a result of 2 or less, an unfavorable outcome—3 or more points on this scale.
A routine blood test including hemoglobin, erythrocyte count, platelets, leukocyte count, differential leukocyte count, erythrocyte sedimentation rate-ESR measurement was performed using hematologic analyzer MEK-7222, NIHON KOHDEN, Japan, and a test tube with K3-ethylenediaminetetraacetic acid.
The odds ratio (for binary indicators) and the ROC analysis (Receiver Operating Characteristic) were calculated using the De Long method, 2014 (for quantitative indices) to determine the factors of the unfavorable outcome of the acute period of the stroke (mRS score 3 or more points). The area under the ROC curve (AUC) ranges from 0.5 (test is not informative) to 1 (high accuracy of the test). Sensitivity, specificity, the prognostic value of the positive result and the prognostic value of the negative result were measured. When constructing the ROC curve, the optimal threshold value of the indicator was calculated (a combination of maximum values of sensitivity and specificity). The results were considered statistically significant at p < 0.05.
RESULTS
In the study group at herothrombotic stroke was diagnosed in 29 cases (41%), cardiogenic embolic stroke in 33 (47%), lacunar stroke in 3 (4%) patients and stroke due to coagulopathy in 5 (7%) patients.
Severity of neurologic symptoms on the NIH scale was 7 to 25 points upon admission, 15 [11, 17] points on average. The stroke of mild severity (the NIH score less than 7 points) was observed in 5 patients (7%); moderate severity (NIHSS 7–13 points)—in 21 (30%) patients; severe (NIHSS 14 or more) in 44 (63%) patients.
The time since the development of the neurological symptoms to the admission ranged from 40 to 245 min (mean 138 [117, 170] min), the time before the administration of STLT (“the door-to-needle time”) was from 15 to 90 minutes (mean 40 [30, 55] min). The interval between the onset of the stroke and the admission of thrombolysis was 60–270 min (mean 180 [150, 210] min).
A favorable functional outcome (mRS 2 points and less 3 months after the stroke) was observed in 42 patients (60%), lethal outcome—in 5 patients (7.1%).
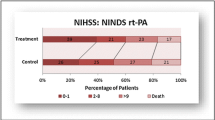
Based on the ROC analysis (Fig. 1), the area under curve performed for the NIHSS score before the STLT was 0.766 ± 0.058 (95% CI 0.65–0.86; p < 0.001). The threshold of the total NIHSS score for the unfavorable functional outcome (mRS scale score 3 and more points in 90 days after the IS) was more than 12 points (sensitivity: 94%, specificity: 57%) if systemic thrombolytic therapy was performed.
The results of the evaluation of the prognostic significance of the full blood count-the number of neutrophils and lymphocytes-in patients with IS who underwent STLT is given in Table 1. The ROC analysis of the thrombolytic therapy results of 70 patients with IS showed that the increased neutrophil count and/or the lower lymphocyte count in the peripheral blood before STLT is a predictor of the unfavorable functional outcome of IS (mRS score 3 and more points in 90 days after the stroke).
There was a significant difference in plasma glucose level before intravenous thrombolysis among the patients. So, the blood glucose at admission in the group of patients with type 2 diabetes mellitus was 9.1 ± 2.4 mmol/L, in the group without diabetes mellitus—5.8 ± 0.6 mmol/L. Glycated hemoglobin was increased up to 8.0 ± 1.29% in patients with duration of diabetes from 1 to 7 years. The administration of rtPA for patients with diabetes mellitus did not lead to clinical improvement in 40% of cases, whereas in patients without diabetes only in 17%.
DISCUSSION
Time is the key factor which determines the effectiveness of STLT [8–10]. The earlier admission of thrombolytic agent leads to its greater efficacy and safety [8]. Time is crucial for achieving a favorable functional outcome for endovascular reperfusion interventions as well. Thus, according to the guidelines of the AHA-ASA, the goal of endovascular treatment is to reach the TICI 2b/3 reperfusion level as quickly as possible (within 6 hours after IS) (Class I, level of evidence A). Additional intra-arterial administration of fibrinolytics (Class IIb, level of evidence B) is possible if necessary. The efficacy of mechanical thrombectomy performed later than 6 h after IS is uncertain (Class II, level of evidence C).
The severity of neurologic symptoms is also an undeniable factor of the efficacy and safety of STLT. The probability of achieving a positive effect of systemic thrombolysis is higher in patients with an NIHSS score of up to 10 points and from 16 to 21 points. At the same time, the greater severity of neurologic symptoms does not exclude thrombolytic therapy administration [8], although it is associated with greater risk of unfavorable outcome.
As mentioned above, the NIH stroke scale score (more than 6 points) is one of the key criteria for determining indications for endovascular methods of reperfusion. At the same time it is possible to consider the NIHSS score 12 points as the threshold for the selection of patients for endovascular treatment, because the severity of neurologic symptoms of 11 points or less on the NIH stroke scale is associated with a favorable functional outcome after STLT.
The age of patients has been considered to be a predictor of the effectiveness and safety of thrombolysis. STLT is more effective in patients younger than 75 years, but older age is not a limitation as well [8, 10, 11], but requires more careful assessment of potential risks. For example, elderly age is one of the key risk factors for the development of a symptomatic hemorrhage during or after thrombolytic therapy [12, 13].
Questions concerning the volume and composition of the thrombus and the effectiveness of thrombolysis remain relatively debatable. Extended thrombus with a complex composition located in the intracranial arteries are less susceptible to recanalization [14] with intravenous rtPA. Indeed, the probability of successful restoration of blood flow in the occluded M2 MCA segment (according to the opinion of different authors varies from 30.8% [15] to 77% [16]) is significantly higher than the recanalization of ICA, where the given index for STLT is from 4% [15] to 35% [16].
Thrombi in the intracranial part of the ICA or the proximalM1 segment of the MCA more than 8 mm reduce the likelihood of blood flow restoration under systemic rtPA administration to zero, but with a thrombus length of 2 mm or less, the chances of successful recanalization exceed 90% [17]. Given this, patients with IS caused by occlusion of the proximal part of the intracranial arteries with large, poorly lysed thrombi/embolus with intravenous fibrinolytic action are the main group of patients in whom the combination of STLT and endovascular interventions is potentially more effective than systemic fibrinolysis alone.
With regard to thrombus structure, it should be noted that fresh “red” thrombi consisting of fibrin are more sensitive to thrombolytics, as evidenced by the rapid lysis of “venous” thrombi compared with “arterial” thrombi, where morphologically “white” thrombi predominate. At the same time, thrombi with a high content of fibrinogen and lipids are more resistant to lysis [18, 19]. However, there are no ultrasound and neuroimaging methods that allow rapid antemortemanalysis of thrombus composition. At the same time, studies that correlate clinical, imaging and laboratory data with morphological findings of thrombi obtained during endovascular thrombectomy or postmortem have been initiated around the world.
Blood glucose level is essential for the administration of systemic thrombolytic therapy. Hypoglycemia less than 2.7 mmol/L and hyperglycemia greater than 22.0 mmol/L are contraindications for systemic thrombolysis [20]. Hyperglycemia is associated with a high incidence of hemorrhagic transformation, a lack of recanalization, and a severe clinical outcome [13, 21, 22]. Hyperglycemia more than 7 mmol/L is a predictor of ineffectiveness of STLT [23]. The likelihood of developing a symptomatic hemorrhage increases if a blood glucose level is more than 16.7 mmol/L [24]. A meta-analysis of 55 clinical studies confirmed a linear dependency between high glucose levels and development of symptomatic brain hematoma after STLT [25].
In subsequent studies it was found that the level of HbA1c is also a predictor of hemorrhagic transformation of cerebral infarction after rtPA therapy [26], which may indicate that acute hyperglycaemia and damage to the vascular wall are important in the pathogenesis of hemorrhagic transformation [27, 28]. Many researchers agreed that the level of HbA1c is more significant predictor in determining the probability of development of the hemorrhagic component than a single blood glucose test or anamnestic indications for diabetes mellitus. An increase in glycemia more than 7.7 mmol/L and HbA1c more than 6.5 is associated with an unfavorable clinical outcome and a high lethality after thrombolysis, especially with glycemia values greater than 11.1 mmol/L and HbA1c greater than 8 [26].
Thus, reperfusion therapy is effective in a specific cohort of patients with IS. A personalized approach to its implementation can help to predict the effectiveness of STLT and develop appropriate strategies of patient management.
CONCLUSIONS
(1) The factors of the unfavorable functional outcome (the mRS scale score 3 or more points 90 days after the IS) are a total score on the NIH stroke scale more than 12 points and an increased neutrophil count and/or a lower lymphocyte count in the peripheral blood of patients before initiation of STLT.
(2) History of diabetes mellitus, poorglycemic control lead to the absence of clinical improvement after STLT.
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of interests. The authors declare that they have no conflict of interest.
Statement of compliance with standards of research involving humans as subjects. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants involved in the study.
REFERENCES
Powers, W.J., Derdeyn, C.P., Biller, J., et al., 2015 AHA/ASA focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. A Guideline for healthcare professionals from the American Heart Association/American Stroke Association, Stroke, 2015, vol. 46, no. 10, pp. 3020–3035. PMID 26123479. doi 10.1161/STR.0000000000000074
Skvortsova, V.I., Golukhov, G.N., Gubskii, L.V., et al., Systemic thrombolysis in ischemic stroke, Zh. Nevropatol. Psikhiatr. im. S.S. Korsakova, 2006, vol. 106, no. 12, pp. 24–31.
Domashenko, M.A., Maksimova, M.Yu., Loskutnikov, M.A., et al., Systemic thrombolysis in acute ischemic stroke, Ann. Klin. Eksp. Nevrol., 2008, vol. 2, pp. 5–12.
Domashenko, M.A., Maksimova, M.Yu., Loskutnikov, M.A., et al., Mechanisms of reperfusion with intravenous thrombolytic therapy in patients with ischemic stroke, Nevrol., Neiropsikhiatriya, Psikhosom., 2012, vol. 4, pp. 53–58.
Piradov, M.A., Domashenko, M.A., and Maksimo-va, M.Yu. Reperfusion treatment of ischemic stroke, in Nevrologiya XXI veka: diagnosticheskie, lechebnye i issledovatel’skie tekhnologii. Rukovodstvo dlya vrachei (Neurology of 21 Century: Diagnostics, Medical Course, and Study Technologies. Manual for Physicians), Pira-dov, M.A., Illarioshkin, S.N., and Tanashyan, M.M., Eds., Moscow: ATMO, 2015, vol. 2, pp. 9–45.
Skvortsova, V.I., Stakhovskaya, L.V., Lelyuk, V.G., et al., Development of the care system for stroke patients in Russian Federation, Materialy Vserossiiskoi nauchno-prakticheskoi konferentsii “Sovershenstvovanie okazaniya meditsinskoi pomoshchi bol’nym s sosudistymi zabolevaniyami” (Proc. All-Russ. Sci.-Pract. Conf. “Improvement of Medical Care for Patients with Vascular Diseases”), Yaroslavl, 2011, pp. 13–33.
Shamalov, N.A. Problems and prospects of reperfusion therapy in ischemic stroke in Russia, Farmateka, 2015, vol. 9, pp. 14–19.
Emberson, J., Lees, K.R., Lyden, P., et al., Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischemic stroke: a meta-analysis of individual patient data from randomized trials, Lancet, 2014, vol. 384, no. 9958, pp. 1929–1935. PMID 25106063. http:// dx.doi.org/10.1016/S0140-6736(14)60584-5.
Lees, K., Bluhmki, E., von Kummer, R., et al., Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials, Lancet, 2010, vol. 375, pp. 1695–1703. PMID 20472172. http://dx. doi.org/10.1016/S0140-6736(10)60491-6.
Sandercock, P., Wardlaw, J.M., Lindley, R.I., et al., The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischemic stroke (the Third International Stroke Trial [IST-3]): a randomized controlled trial, Lancet, 2012, vol. 379, pp. 2352–2363. PMID 22632908. doi 10.1016/S0140-6736(12)60768-5
Hacke, W., Kaste, M., Bluhmki, E., et al., Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke, N. Engl. J. Med., 2008, vol. 359, pp. 1317–1329. PMID 18815396. http://dx.doi.org/10.1056/NEJMoa0804656.
Shamalov, N.A., Optimization of reperfusion therapy in patients with ischemic stroke, Extended Abstract of Doctoral (Med.) Dissertation, Moscow, 2012.
Lansberg, M.G., Thijs, V.N., Bammer, R., et al., Risk factors of symptomatic intracerebral hemorrhage after tPA therapy for acute stroke, Stroke, 2007, vol. 38, pp. 2275–2278. PMID 17569874. https://doi.org/ 10.1161/STROKEAHA.106.480475.
Urbach, H., Hartmann, A., Pohl, C., et al., Local intra-arterial thrombolysis in the carotid territory: does recanalization depend on the thromboembolus type? Neuroradiology, 2002, vol. 44, pp. 695–699. PMID 12185548. http://dx.doi.org/10.1007/s00234-002-0762-6.
Bhatia, R., Hill, M.D., Shobha, N., et al., Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action, Stroke, 2010, vol. 41, no. 10, pp. 2254–2258. PMID 20829513. http://dx.doi.org/10.1161/STROKEAHA.110.592535.
Broderick, J.P., Palesch, Y.Y., Demchuk, A.M., et al., Endovascular therapy after intravenous t-PA versus t-PA alone for stroke, N. Engl. J. Med., 2013, vol. 368, no. 10, pp. 893–903. PMID 23390923. http://dx. doi.org/10.1056/NEJMoa1214300.
Riedel, C.H., Zimmermann, P., Jensen-Kondering, U., et al., The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length, Stroke, 2011, vol. 42, no. 6, pp. 1775–1777. PMID 21474810. http://dx.doi.org/10.1161/STROKEAHA.110.609693
Del Zoppo, C.J., Poeck, K., Pessin, M.S., et al., Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke, Ann. Neurol., 1992, vol. 32, pp. 78–86. PMID 1642475. http://dx.doi.org/ 10.1002/ana.410320113.
Mori, E., Yoneda, Y., Tabuchi, M., et al., Intravenous recombinant tissue plasminogen activator in acute carotid territory stroke, Neurology, 1992, vol. 42, pp. 976–982. PMID 1579252
Adams, H., Del Zoppo, G., Alberts, M., et al., Guidelines for the management of adults with ischemic stroke, Stroke, 2007, vol. 38, pp. 1655–1711. PMID 17431204. doi 10.1161/STROKEAHA.107.181486
Cucchiara, B., Tanne, D., Levine, S.R., et al., A risk score to predict intracranial hemorrhage after recombinant tissue plasminogen activator for acute ischemic stroke, J. Stroke Cerebrovasc. Dis., 2008, vol. 17, pp. 331–333. PMID 18984422. http://dx.doi.org/ 10.1016/j.jstrokecerebrovasdis.2008.03.012.
Saqqur, M., Shuaib, A., Alexandrov, A.V., et al., The correlation between admission blood glucose and intravenous rt-PA-induced arterial recanalization in acute ischemic stroke: a multi-centre TCD study, Int. J. Stroke, 2015, vol. 10, no. 7, pp. 1087–1092. PMID 26332252. doi 10.1111/ijs.12517
Vanacker, P., Heldner, M.R., Seiffge, D., et al., ASTRAL-R score predicts non-recanalisation after intravenous thrombolysis in acute ischemic stroke, Thromb. Haemostasis, 2015, vol. 113, no. 5, pp. 911–917. PMID 25854290. http://dx.doi.org/10.1160/TH14-06-0482.
Demchuk, A.M., Morgenstern, L.B., Krieger, D.W., et al., Serum glucose level, and diabetes predict tissue plasminogen activator-related intracerebral hemorrhage in acute ischemic stroke, Stroke, 1999, vol. 30, no. 1, pp. 34–39. PMID 9880385. http:// dx.doi.org/10.1161/01.STR.30.1.34.
Whiteley, W.N., Slot, K.B., Fernandes, P., et al., Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator: a systematic review and meta-analysis of 55 studies, Stroke, 2012, vol. 43, no. 11, pp. 2904–2909. PMID 22996959. http://dx.doi. org/10.1161/STROKEAHA.112.665331.
Rocco, A., Heuschmann, P.U., Schellinger, P.D., et al., Glycosylated hemoglobin A1 predicts risk for symptomatic hemorrhage after thrombolysis for acute stroke, Stroke, 2013, vol. 44, no. 8, pp. 2134–2138. PMID 23715962. https://doi.org/10.1161/ STROKEAHA.111.675918.
Masrur, S., Cox, M., Bhatt, D.L., et al., Association of acute and chronic hyperglycemia with acute ischemic stroke outcomes post thrombolysis: findings from get with the guidelines stroke, J. Am. Heart Assoc., 2015, vol. 4, no. 10, p. e002193. PMID 26408015. https://doi.org/10.1161/JAHA.115.002193/
Tanashyan, M.M., Suslina, Z.A., Ionova, V.G., et al., Endothelial function in patients with ischemic stroke at different degrees carotid artery atherosclerosis, Nevrol. Vestn. Zh. im. V.M. Bekhtereva, 2007, vol. 29, no. 1, pp. 12–16.
Author information
Authors and Affiliations
Corresponding author
Additional information
The article is published in the original.
Rights and permissions
About this article
Cite this article
Domashenko, M.A., Maksimova, M.Y., Gafarova, M.E. et al. Personified Approaches to Reperfusion Therapy of Ischemic Stroke. Hum Physiol 44, 869–874 (2018). https://doi.org/10.1134/S0362119718080030
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119718080030