Abstract
Calcium phosphate composite cements for bone grafting containing an X-ray contrast agent, (BiO)2CO3, were obtained. Its presence in cement will make it possible to track the process of bone-tissue regeneration. Due to the multicomponent composition of the cement, in which some of the phases are resorbed slowly and others quickly, a prolonged supply of the material involved in osteogenesis is achieved. The resulting cement paste can be injected through the needle of a syringe with an internal diameter of 2 mm, without delamination, due to the introduction of polyethylene glycol as a thixotropic additive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The development of methods for producing X-ray contrast cements with improved properties for closing small cavities in bone tissues, as well as treating traumatic genesis cracks, is a popular area of modern medicine. In traumatology and maxillofacial surgery, composite calcium-phosphate cements are used as bone-substituting materials. Bone-tissue regeneration during their use occurs as a result of the gradual resorption of calcium orthophosphates with the involvement of mineral components in osteogenesis. The important advantages of such materials include biocompatibility and low invasiveness of surgical procedures, as well as the possibility of introduction by syringe. To visualize the processes of material introduction and subsequent restoration of bone tissue, cements containing X-ray contrast substances (XCSs) are used.
Among XCSs widely used in radiological practice for contrasting vascular formations or closed cavities, iodine-containing substances are widely used. However, the introduction of these compounds is accompanied by a number of side effects. Their toxic effect on blood, kidneys, liver, and thyroid gland has been noted [1, 2]. Bismuth, tantalum, strontium, bromine, fluorine, etc., are studied as elements acting as an XCS [3–7]. Due to its relevance to medicine, the search for effective and safe XCS continues.
Bismuth-containing compounds have attractive characteristics. Bismuth compounds have disinfecting, drying, astringent, and antiseptic properties. They treat many nonspecific inflammatory processes. Many medical preparations based on gallate, tartrate, carbonate, tribromophenolate, bismuth subcitrate, and subsalicylate have been developed [8]. Bismuth-containing drugs reduce the toxic effect that occurs during anticancer chemotherapy [9]. Bismuth preparations are believed to have moderate toxicity. Long-term introduction and high concentrations cause complications. The chronic intake of bismuth in amounts of 1–1.5 g per day is considered dangerous. Chronic bismuth poisoning leads to a change in lipid, protein, and carbohydrate metabolism in the body; a decrease in hemoglobin in the blood; and other disorders.
Bi3+-doped hydroxyapatite samples were obtained and studied in [10, 11]. It has been established that Bi-doped hydroxyapatite has a slower dissolution rate than undoped hydroxyapatite. The antimicrobial activity of the samples was noted. The use of bismuth salicylate as an X-ray contrast agent in cement is proposed in [12, 13]. It was noted that bismuth salicylate has a retarding effect on the curing rate of cement, but its addition reduces the viscosity and yield strength of the cement paste, which increases its ability to be injected. The results show that the composition has a good in vitro X-ray contrast ability, high injectability, and potent antimicrobial activity.
The aim of this work was to obtain calcium phosphate composite cements for bone restoration, with (BiO)2CO3 acting as an XCS and polyethylene glycol as a plasticizer for the cement paste.
EXPERIMENTAL
Tricalcium phosphate (TCF) and monocalcium phosphate monohydrate (MCPM) with a molar ratio of 1.5 : 1 were used as starting components. (BiO)2CO3 was added to the samples in amounts from 0 to 20%. All chemical reagents have the “pure” brand. Samples of calcium phosphate cements were obtained by the mechanical mixing of the components and the subsequent addition of a mixing liquid. A 30% colloidal silicate suspension in water (CSW) (SIGMA-ALDRICH, LUDOX AM-30) with the addition of 5% polyethylene glycol (PEG-35 (1500)) as a plasticizer was used. The solid and liquid phases were mixed with a metal spatula on the glass until they were smooth, after which the cement paste was placed in a cylindrical mold with a diameter of 1.2 cm and a height of 0.7 cm and then dried at room temperature for 24 h. The curing process took place at a temperature of 25°C and relative humidity of 70%. After 24 h, the molded sample was taken out and examined.
The composition of the samples was controlled by X-ray diffraction using the EVA software with a PDF-2 powder database. The mechanical strength of samples was determined by compressing them at a rate of 0.5 mm/min using an Autograph AG-X plus 100 kN Shimadzu tensile testing machine (Japan). Images of the structure of materials were obtained by scanning electron microscopy using Hitachi S 5500 devices (Japan) with an add-on for energy dispersive analysis. The X-ray contrast properties of samples was determined in Hounsfield units (Hu) using an Optima CT580GE computer tomograph. X-ray contrast properties of the samples were calculated as an average value of ten measurements obtained in randomly selected points.
RESULTS AND DISCUSSION
The obtainment of calcium phosphate cement by tricalcium phosphate mixing with monocalcium phosphate monohydrate and water is described by the reaction
The final product of the reaction is dicalcium phosphate dihydrate (brushite). It is known that the rate of resorption of brushite cements compared with, for example, apatite is higher [14]. As shown by in vivo studies [15], it is so high that the growing bone tissue does not have time to fill the cavities that form. That is why such compounds are not suitable for independent use as bone-tissue substitutes, but they are used only as components of calcium phosphate cement mixtures. In order to restore bone tissue, the biodegradation rate of implanted materials should maximally coincide with the growth rate of new bone.
The presence of tricalcium phosphate that is excessive with respect to the stoichiometric amount of calcium in the composition of the initial cement increases the Ca/P ratio and increases the pH of the hardening solution that should lead to a decrease in the solubility of final cement composition in the body. Changing the amount of TCP in the mixture will make it possible to control the final composition of the implanted materials and, therefore, affect the rate of resorption. To obtain calcium phosphate cement, the TCP and MCPM were taken in a molar ratio of 1.5 : 1. The mixing liquid was chosen to be 30% CSW, since the strength of the samples diluted with this suspension is one and a half times higher than that of the samples sealed with water [16].
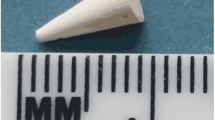
When passing through the needle, calcium phosphate-based cements tend to delamination. To improve the properties of cement paste, as well as to prolong the time of its curing, polyethylene glycol was introduced into the dilution fluid. Polyethylene glycol is a neutral, water-soluble polyester that has a relatively low toxicity to body tissues [17, 18]. It is widely used as a thixotropic additive that improves the injectability of biocement [19, 20], and it is also used in drug delivery [21, 22]. Due to its introduction, most of the samples have acceptable plasticity and do not separate. Acceptable plasticity was taken as plasticity in which the cement paste can be injected through a needle with an inner diameter of 2 mm.
X-ray diffraction showed that the final compounds 24 h after mixing the solid and liquid phases are as follows: for 0% XCS, a mixture of brushite (CaHPO4 ⋅ 2H2O) and hydroxyapatite (Ca10(PO4)6(OH)2); for 5% XCS, a mixture of brushite, hydroxyapatite, and bismuthyl carbonate ((BiO)2CO3); and, for 20% XCS, a mixture of brushite, hydroxyapatite, monetite (CaHPO4), and bismuthyl carbonate (Fig. 1).
The strength of the samples was investigated at variable S/L values in the cement paste and a constant content of (BiO)2CO3 of 5%. The range 1.52 > S/L > 1 was investigated. The strength of the samples in this interval linearly decreases from 2.3 to 0.8 MPa. Outside this interval, the characteristics of the cement paste are unsatisfactory: at S/L > 1.52, it was not possible to inject the paste through a syringe and, at S/L < 1, the curing time of the samples is more than 40 min. Thus, there are optimal S/L ratios at which the maximum compressive strength of cement is achieved, while maintaining acceptable ductility of the cement paste and satisfactory curing time. The range 1.2 < S/L < 1.4 satisfies these conditions. For further research, we chose the ratio S/L = 1.3. Table 1 shows the characteristics of samples of calcium phosphate cements obtained in the work.
The curing time of the studied samples ranges from 5 to 15 min. The time of complete solidification of the cement was 2–3 h. The strength of the samples is affected by the content of XCS in the mixture of components: an increase in XCS reduces the strength of the cement (Table 1). As is known, bone defects must be filled with materials with mechanical characteristics similar to bone, and the compressive strength of trabecular bone tissue ranges within 2–12 MPa [23]. Thus, the strength of the materials becomes unsatisfactory when the content of (BiO)2CO3 is more than 7%.
Bone tissues have their own X-ray contrast properties, which, according to C. Mish classification, varies from 350 to 1250 Hu (Hounsfield units), depending on shape, structure, function, and development. Table1 shows that, for visualization of the implant, the content of (BiO)2CO3 in the amount of 3.5–4% will be sufficient. Studies show that the most durable cements that satisfy the required plasticity and X-ray contrast are obtained when several conditions are met simultaneously 5% < PEG < 10%; 1.2 < S/L < 1.4; 3.5 < (BiO)2CO3 < 5. In these cases, the curing time of cement maximally fits to carry out the surgical manipulations.
Figure 2 shows fragments of the fracture in the samples. They have a similar structure and a well-developed microrelief. The samples are characterized by particles that are stuck together, resembling plates, with average sizes of 3 × 3 × 1 μm. The higher the percentage of XCS in the sample, the more blurred the sample looks.
Table 2 shown the compositions of cement samples containing 0% (BiO)2CO3 (nos. 1–3), 5% (BiO)2CO3 (nos. 4–6), and 20% (BiO)2CO3 (nos. 7–9). The dots shown in Figure 2 correspond to the numbers shown in Table 2. The Ca/P ratio in the sample ranges from 0.9 to 2. The particles in the shape of platelets mainly consist of calcium phosphates.
The purpose of the composite calcium phosphate cements is to close small cavities in bone tissues, as well as treat traumatic genesis cracks exclusively in places where bone tissue does not carry a significant load. The advantage of the materials is their biocompatibility. Calcium phosphate-based cement can resorb and be replaced with bone tissue over time, which allows the biological restoration of its own bone tissue and eliminates thermal and toxic effects that are inevitable when using, for example, the injection of acrylic cement, which is widely used in surgery. In particular, injecting acrylic X-ray contrast cement was proposed in [13]. Its main components are polymethyl methacrylate (PMMA) and methyl methacrylate. The polymerization reaction of PMMA is exothermic. The temperature can reach 122°C. In addition, it is necessary to take into account that the curing of the monomer phase is not fully realized and a certain amount of methyl methacrylate remains in the system, which is able to penetrate into the surrounding tissues, exerting a toxic effect [24].
In [12], the composition of calcium phosphate cement was proposed in which the basic bismuth salicylate was used as the X-ray contrast component. All calcium phosphates used in the cement preparation method [12] underwent a laborious and lengthy preparation process: tetracalcium phosphate was obtained by a solid phase reaction between calcium phosphate and calcium carbonate at a temperature of 1500°C for 8 h. Dicalcium phosphate dihydrate was obtained from diammonium phosphate and calcium nitrate in an acidic medium, and anhydrous dicalcium phosphate by removing crystallization water from dicalcium phosphate at 120°C. The solid phase for cement paste was obtained by dry mixing the required amount of each of the components and grinding the mixture for 24 h in a ball mill.
The preparation process of cement paste that is proposed is simple and does not require special equipment for the preparation of its components.
CONCLUSIONS
Calcium phosphate composite cements for bone grafting, which can provide the body with a prolonged supply of material involved in osteogenesis, have been obtained. This is due to the fact that one of the phases (hydroxyapatite) is resorbed slowly and the other (breaks, monetizes) is resorbed quickly.
The introduction of polyethylene glycol makes the cement paste more plastic, which makes it possible to adjust the curing time of the paste and use it for injection through a syringe.
The presence of an X-ray contrast substance, bismuthyl carbonate, in the cement composition makes it possible to control the processes of filling and regeneration of bone-tissue defects.
REFERENCES
Domaradskaya, A.I., What should we know about adverse reactions on contrast media?, Russ. Electron. J. Radiol., 2012, vol. 2, no. 1, pp. 71–73.
Fominyh, V.P., Fineshin, I.N., and Sharikov, P.V., Roentgen contrast media: View of resuscitator, Russ. Electron. J. Radiol., 2012, vol. 2, no. 1, pp. 35–43.
Webster, T.J., Massa-Schlueter, E.A., Smith, J.L., and Slamovich, E.B., Osteoblast response to hydroxyapatite doped with divalent and trivalent cations, Biomaterials, 2004, vol. 25, no. 11, pp. 2111–2121. https://doi.org/10.1016/j.biomaterials.2003.09.001
Deb, S., Abdulghani, S., and Behiri, J.C., Radiopacity in bone cements using an organo-bismuth compound, Biomaterials, 2002, vol. 23, no. 16, pp. 3387–3393. https://doi.org/10.1016/S0142-9612(02)00039-X
Åberg, J., Pankotai, E., Billström, G.H., Weszl, M., Larsson, S., Forster-Horváth, C., Lacza, Z., and Engqvist, H., In vivo evaluation of an injectable premixed radiopaque calcium phosphate cement, Int. J. Biomater., 2011, vol. 2011, article no. 232574. https://doi.org/10.1155/2011/232574
Wang, X., Ye, J., and Wang, Y., Influence of a novel radiopacifier on the properties of an injectable calcium phosphate cement, Acta Biomater., 2007, vol. 3, no. 5, pp. 757–763. https://doi.org/10.1016/j.actbio.2007.01.004
Åberg, J., Henriksson, H.B., Engqvist, H., Palmquist, A., Brantsing, C., Lindahl, A., Thomsen, P., and Brisby, H., Biocompatibility and resorption of a radiopaque premixed calcium phosphate cement, J. Biomed. Mater. Res., Part A, 2012, vol. 100, no. 5, pp. 1269–1278. https://doi.org/10.1002/jbm.a.34065
Yang, N. and Sun, H., Biocoordination chemistry of bismuth: Recent advances, Coord. Chem. Rev., 2007, vol. 251, pp. 2354–2366. https://doi.org/10.1016/j.ccr.2007.03.003
Imam, S.K., Advancements in cancer therapy with alpha-emitters: A review, Int. J. Radiat. Oncol., Biol., Phys., 2001, vol. 51, no. 1, pp. 271–278. https://doi.org/10.1016/S0360-3016(01)01585-1
Webster, T.J., Massa-Schlueter, E.A., Smith, J.L., and Slamovich, E.B., Osteoblast response to hydroxyapatite doped with divalent and trivalent cations, Biomaterials, 2004, vol. 25, no. 11, pp. 2111–2121. https://doi.org/10.1016/j.biomaterials.2003.09.001
Ciobanu, G., Bargan, A.M., and Luca, C., New bismuth-substituted hydroxyapatite nanoparticles for bone tissue engineering, JOM, 2015, vol. 67, no. 11, pp. 2534–2542. https://doi.org/10.1007/s11837-015-1467-8
Chen, F., Liu, C., and Mao, Y., Bismuth-doped injectable calcium phosphate cement with improved radiopacity and potent antimicrobial activity for root canal filling, Acta Biomater., 2010, vol. 6, no. 8, pp. 3199–3207. https://doi.org/10.1016/j.actbio.2010.02.049
Hernández, L., Fernández, M., Collía, F., Gurruchaga, M., and Goñi, I., Preparation of acrylic bone cements for vertebroplasty with bismuth salicylate as radiopaque agent, Biomaterials, 2006, vol. 27, no. 1, pp. 100–107. https://doi.org/10.1016/j.biomaterials.2005.05.074
Safronova, T.V. and Putlyaev, V.I., Medical inorganic materials science in Russia: Calcium phosphate materials, Nanosist.: Fiz., Khim.,Mat., 2013, vol. 4, no. 1, pp. 24–47.
Veresov, A.G., Putlyaev, V.I., and Tret’yakov, Yu.D., The chemistry of inorganic biomaterials based on calcium phosphates, Ross. Khim. Zh., 2004, vol. 48, no. 4, pp. 52–64.
Medkov, M.A., Grishchenko, D.N., Nedozorov, P.M., and Rudnev, V.S., Calcium phosphate cements for bone tissue engineering, Khim. Tekhnol., 2015, vol. 16, no. 1, pp. 12–17.
Zharkova, I.I., Bonartsev, A.P., Boskhomdzhiev, A.P., et al., The effect of poly(3-hydroxybutyrate) modification by poly(ethylene glycol) on the viability of cells grown on the polymer films, Biomed. Khim., 2012, vol. 58, no. 5, pp. 579–591.
Timashev, P.S., Bardakova, K.N., Demina, T.S., Pudovkina, G.I., Novikov, M.M., Markov, M.A., Asyutin, D.S., Pimenova, L.F., Svidchenko, E.A., Ermakov, A.M., Selezneva, I.I., Popov, V.K., Konovalov, N.A., Akopova, T.A., Solovieva, A.B., Panchenko, V.Ya., and Bagratashvili, V.N., Novel biocompatible material based on solid-state modified chitosan for laser stereolithography, Sovrem. Tekhnol. Med., 2015, vol. 7, no. 3, pp. 20–31. https://doi.org/10.17691/stm2015.7.3.03
Hesaraki, S., Borhan, S., Zamanian, A., and Hafezi-Ardakan, M., Rheological properties and injectability of β-tricalcium phosphate-hyaluronic acid / polyethylene glycol composites used for the treatment of vesicouretheral reflux, Adv. Biomed. Eng. Res., 2013, vol. 1, no. 3, pp. 40–44.
Rabiee, S.M. and Baseri, H., Prediction of the setting properties of calcium phosphate bone cement, Comput. Intell. Neurosci., 2012, vol. 2012, article no. 809235. https://doi.org/10.1155/2012/809235
Jo, S. and Park, K., Surface modification using silanated poly(ethylene glycol)s, Biomaterials, 2000, vol. 21, no. 6, pp. 605–616. https://doi.org/10.1016/S0142-9612(99)00224-0
Liu, S., Weng, W., Li, Z., Pan, L., Cheng, K., Song, C., Du, P., Shen, G., and Han, G., Effect of PEG amount in amorphous calcium phosphate on its crystallized products, J. Mater. Sci.: Mater. Med., 2009, vol. 20, no. 1, pp. 359–363. https://doi.org/10.1007/s10856-008-3584-1
Barinov, S.M., Calcium phosphate-based ceramic and composite materials for medicine, Russ. Chem. Rev., 2010, vol. 79, no. 1, pp. 13–30. https://doi.org/10.1070/RC2010v079n01ABEH004098
Shtil’man, M.I., Polimery mediko-biologicheskogo naznacheniya (Polymers for Biomedical Applications), Moscow: Akademkniga, 2006.
Funding
This work was partially supported by the “Far East” grant of the Basic Research Program of the Far Eastern Branch, Russian Academy of Sciences (project no. 18-3-042), as part of the state task of the Institute of Chemistry, Far Eastern Branch, Russian Academy of Sciences (topic no. 0265- 2018-0002).
Author information
Authors and Affiliations
Corresponding author
Additional information
Translated by A. Bannov
Rights and permissions
About this article
Cite this article
Medkov, M.A., Grishchenko, D.N., Klimov, M.A. et al. Calcium-Phosphate X-ray Contrast Cements for Bone Repair. Theor Found Chem Eng 54, 693–698 (2020). https://doi.org/10.1134/S0040579520040107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0040579520040107