Abstract
The objective of this study was to evaluate the biological activities of chrysin (CRY), curcumin (CUR), and ellagic acid (EA) by comparing the anti-proliferative, anti-migration effects, and apoptotic gene expressions between the three human cancer cell lines: lung (A549), liver (HEP3B), and breast (MCF-7) compared to normal human fibroblast cell line (L929). Antiproliferative effects of certain phenolic compounds were determined by the MTS assay. Cells were treated with different concentrations of the compounds for two consecutive days. Their effect on cell migration was evaluated using the wound-healing assay. Apoptosis was evaluated by Bax, Bcl-2, Cas-3, Cas-8, Cas-9, Cas-10, CDK 2, CDK4, CDK6, CCNB1, and CCND2 gene expressions. The MTS assay showed that the compounds had antiproliferative effects on A549, HEP3B, and MCF-7 cell lines in a dose- and time-dependent manner. All three compounds also suppressed the migration of the tumor cell lines, significantly increased the levels of apoptotic gene expression, and induced apoptotic cell death. This study shows that chrysin, curcumin, and ellagic acid could be considered promising chemotherapeutic agents in the treatment of lung, liver, and breast cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Cancer is a very complex disease, and the formation and progression of cancer cells are strongly associated with an abnormal intracellular signaling system. One of the most important strategies of novel cancer treatments is chemotherapy [1]. However, common anticancer agents currently used to treat various types of cancer have serious side effects. Thus, recent research has focused mainly on medicinal plants, as they are non-toxic, and natural, and have been found effective in the treatment and prevention of various types of cancer. Therefore, screening natural products is important to identify potential anticancer compounds [2]. More than 60% of recently used anticancer drugs are produced from natural resources, including marine organisms, plants, and microorganisms. There is considerable interest in the function of dietary antioxidants that can scavenge free radicals and oxidants responsible for the development and initiation of various diseases. Confirmed data that antioxidants have preventive effects against various conditions such as coronary diseases, cancer, neurological degeneration, inflammatory disorders, and aging has led to the exploration of foods containing antioxidants [3].
Natural flavonoids are a broad class of plant pigments, and a structurally diverse class of polyphenolic compounds, that can be found in all parts of plants, as are their secondary metabolites. Flavonoids and their derivatives have several biochemical and pharmacological activities such as anti-inflammatory, antiallergic, neuroprotective, cardioprotective, antimicrobial, antioxidant, antibacterial, antiviral, antithrombotic, antimutagenic, and antineoplastic actions. The antioxidant properties of flavonoids are due to their potential activity as oxidative stress-preventing and reducing agents [4, 5].
Chrysin (5,7 dihydroxyflavone) (CRY), is a natural flavonoid of the Oroxylum inducum plant and can be found in various plant extracts as well as in honey and propolis. Chrysin is a herbal medicine mostly used in China and other East Asian countries and has been officially on the list in the Chinese Pharmacopoeia for a long time. Chrysin was shown to have potent antioxidant, anti-inflammatory, and anticancer activities. However, its mechanism of action is not fully known. These beneficial effects of chrysin are believed to be due to free radical scavenging properties [6].
Like chrysin, curcumin (CUR) found in Curcuma longa is one of the naturally occurring phytochemicals that is widely used as a food additive. Its natural polyphenol derivatives, giving turmeric the yellow color, have antioxidant, immunomodulatory, anti-inflammatory, antiviral, antimicrobial, antifungal, and apoptosis-inducing properties. In addition, curcumin was shown to have anticarcinogenic and antiproliferative effects in experimental animals and cell culture studies [7].
Ellagic acid (EA), which has a polyphenolic structure, is a natural antioxidant found in 46 kinds of fruits and nuts such as pomegranate, raspberry, blackberry, grape, walnut, tea, and strawberry. The antioxidant and antiproliferative properties of ellagic acid encourage the exploration of its potential benefits. It is widely used because of its ability to prevent and treat many diseases, including cancer. However, its molecular mechanisms have not been fully clarified [8].
Although the antitumoral properties of all these dietary compounds are known, it is still unclear how they inhibit the complex tumorigenic pathways characterized by uncontrolled cell proliferation, angiogenesis, invasion, and metastasis. It is suggested that these effects are achieved by inhibiting transcription and growth factors, blocking the receptor, inactivating the kinase enzyme system, and inhibiting the release of cytokines that cause tumor formation [9].
In the present study, we examined the effects of chrysin, curcumin, and ellagic acid administration on human lung cancer (A549), human liver (HEP3B), and human breast cancer (MCF-7) cell lines compared to a healthy human fibroblast cell line (L929). To the best of our knowledge, our study is the first to compare the anticancer activities of these three phenolic compounds together.
MATERIALS AND METHODS
Cell line and culture
Cancer cell lines A549 (lung), HEP3B (liver), MCF-7 (breast), and normal fibroblast cell line L929 were from the American Type Culture Collection (ATCC). Dulbecco’s Modified Eagles Medium (DMEM, Sigma) containing 1% penicillin-streptomycin and 10% fetal bovine serum was used as a cell medium. The cells were incubated in a CO2 incubator at 37°C, 5% partial pressure of CO2, and a humid environment in a single-beam, dual detector humidified incubator (Z10.EC 160, NUVE, Turkey) and passaged 2–3 times per week using trypsin-EDTA (0.25%) and washed with phosphate-buffered saline (PBS). The cells were pelleted by centrifugation at 1 500 rpm for 5 min and resuspended in DMEM to the desired concentration.
Chemicals
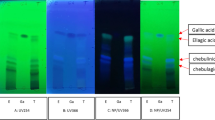
Chrysin, curcumin, and ellagic acid were from Sigma-Aldrich (Cas no: 458-37-7), MP Biomedicals (Lot no: #5096K), Alfa Aesar (Cas no: 476–66-4) respectively, and their stock solutions were prepared in dimethyl sulfoxide (DMSO) to a concentration of 10 mM. Subsequently, stock solutions were diluted for use at 1 µM, 10 µM, 20 µM, 40 µM, 80 µM, 160 µM, 200 µM, 300 µM, and 400 µM concentrations.
Cell viability
Cell viability was tested quantitatively and colorimetrically using the MTS (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) method (The CellTiter 96® AQueous One Solution Cell Proliferation Assay, Promega). The MTS assay protocol is based on the reduction of the MTS tetrazolium compound by viable mammalian cells (and cells from other species) to generate a colored formazan dye that is soluble in cell culture media. A549, HEP3B, MCF-7, and L929 cells were seeded into 96-well plates at 5 × 103 cells per well in 100 µL of the medium. After 24 hours of incubation, cells were treated with chrysin, curcumin, and ellagic acid at different concentrations (1 µM, 10 µM, 20 µM, 40 µM, 80 µM, 160 µM, 200 µM, 300 µM, and 400 µM) and incubated for 24 and 48 hours. The MTS solution was prepared according to the manufacturer’s instructions. For stock solution, 0.084 g of MTS was taken into a sterile foil-wrapped falcon tube and 43 ml of PBS was added. The pH of the prepared solution was adjusted to 6.0–6.5. In a separate sterile falcon tube, 0.02 g of phenazine methosulfate (PMS) was dissolved in 2.1 ml of sterile PBS and, after mixing with a vortex mixer for 10 min, combined with the MTS solution. The combined solution was then mixed by vortexing for 3–5 minutes, passed through a 0.2 µm filter, aliquoted into 2 ml tubes, and stored wrapped in aluminum foil at –20°C. In the plates, with cell lines that have completed the 24 h or 48 h incubation period with the tested compounds, the media were removed from the wells with the help of an aspirator without touching the bottom of the well, and MTS reagent dissolved in DMEM (100 mL DMEM + 10 µL MTS reagent) was added to each well and the plates were returned to the incubator. The intensity of the developed product was measured at 450 nm with a microplate reader (Synergy H1 Hybrid Multi-Mode Reader, BioTek, USA) after 1.5 or 2 h incubation. The absorbance values obtained from the negative controls (cells incubated without the tested compounds) were calculated and taken as 100% cell viability. The MTS trials were repeated four times for each concentration at 24 and 48 hours (n = 4). IC50 concentrations were calculated in the GraphPad Prism (GraphPad Software, Version 8) program using the cell viability results.
Wound healing (scratch) assay
A549, HEP3B, MCF-7, and L929 cell lines were cultured in 12-well microplates at final concentrations of 1 × 105 cells/well. They were subjected to a 24 h standard incubation (5% CO2, 37°C). A straight line was drawn by using a 200 µL sterile plastic pipette, detached cells were removed by DMEM and the remained attached cells were treated with indicated concentrations of chrysin, curcumin, and ellagic acid in 100 µL of DMEM. The wound-healing rate was evaluated with an inverted light microscope after 0, 24, and 48 hours of incubation, and the ImageJ program was used to analyze the wound healing gap area (n = 3) [10].
Apoptosis analysis with Annexin V
Apoptotic cell death rate after treatment with chrysin, curcumin, and ellagic acid was analyzed using the Muse Annexin V and Dead Cell Reagent kit (Luminex Corporation, Texas, USA) according to the manufacturer’s instructions. L929, A549, HEP3B and MCF-7 cell lines were cultured in 6-well microplates at final concentrations of 1 × 106 cells/well and a total volume of 3 mL of medium. They were subjected to a 24 h standard incubation (5% CO2, 37°C). Chrysin, curcumin, and ellagic acid were applied at IC50 concentrations and incubated for a further 48 h. Only cell medium (without the tested compounds) was applied to the control group, which was used to determine the control cell population. To prepare cell suspension for analysis, the upper media were transferred to separate falcon tubes and cells were harvested by adding 500 µL of 0,25% Trypsin in PBS buffer containing 1 mM EDTA (pH 7.2), and the contents of each well were transferred to the corresponding falcon tube containing the medium. To inhibit the effect of trypsin PBS containing 2% FBS (total volume 250 µL) was added to the cell pellet obtained after centrifugation at 1500 rpm for 5 min. From each tube 100 µL of cell suspension was taken and after addition to it of 100 µL of Annexin V-Dead Cell kit solution incubated in the dark for 20 minutes. At the end of the incubation period, analysis of each sample was performed in triplicate using the Muse Cell Analyzer (Luminex Corporation, Texas, USA).
Gene expression analysis by RT-PCR
Chrysin, curcumin, and ellagic acid were applied at IC50 concentrations to A549, HEP3B, and MCF-7 cells seeded in 6-well plates. At the end of 48 h incubation time, total RNA isolation, cDNA synthesis, and RT-PCR analysis were performed to evaluate the expression of genes of interest. The control groups used in the comparison of the results are the A549, HEP3B, and MCF-7 cells, which were treated with cell medium only. Total RNA isolation from cells was performed using One Step RNA Reagent (BS410A, Bio Basic, Toronto, Canada) according to the manufacturer’s protocol. According to the protocol, One Step RNA Reagent was added at 1 mL per well and the cells were removed with a scraper and centrifuged after adding 200 µL of chloroform (Cas no: 67-66-3, ISOLAB, Germany) and 500 µL of isopropyl alcohol (Cas no: 24137, Honeywell, Germany), respectively. The cell pellet obtained was washed with 1 mL of ethanol (Cas no: 32221, Honeywell, Germany) and then dissolved with 30 µL of RNase-DNase-free water. The concentration and purity of the isolated total RNAs were measured with a Nanodrop spectrophotometer (Thermo Fisher Sci., Canada). As a result of the measurements, the expected purity value at the rate of 260/280 was around 2.0. cDNA synthesis was performed according to the manufacturer's protocol (OneScript Plus cDNA synthesis kit for mRNAs, Cat no: G236, Applied Biological Materials, Richmond, Canada), using equal amounts (2 µg) of total RNA in each sample. The synthesized cDNAs were stored at –80°C until real-time polymerase chain reaction (RT-PCR) analysis. mRNA expression analyzes were performed using StepOnePlus RT-PCR (Applied Biosystems, Massachusetts, USA) according to the BlasTaq 2X qPCR MasterMix kit (Cat no: G891, Applied Biological Materials, Richmond, Canada) protocol. The RT-PCR conditions for the genes were: pre-denaturation at 95°C for 3 min, followed by 40 cycles of denaturation at 95°C for 15 s and 60°C for 60 s GADPH was used as a reference housekeeping gene in the analysis of Bcl-2-associated X protein (Bax), B-cell lymphoma 2 (Bcl-2), caspases (Cas)-3, Cas-8, Cas-9, Cas-10, cyclin-dependent kinases (CDK) 2 (CDK2), CDK4, CDK6, cyclin (CCN)B1 and CCND2 mRNA expressions (Table 1). In the analysis of PCR data, quantitation was performed using the ∆CT method. Volcano Plot analyses in the ‘RT² Profiler™ PCR Array Data Analysis’ program on the Internet-based Gene Globe platform were used (https://geneglobe.qiagen.com/us/analyze).
Statistical analysis
Two-way ANOVA with post-hoc Tukey test was performed using the GraphPad Prism program (Version 8) for cell viability data analyses. ImageJ program was used to analyze wound healing. The wound area was expressed as a percentage of the whole area. Descriptive data were analyzed using the SPSS 22.0 package program (SPSS Inc., Chicago, IL, United States). Statistical differences in wound healing were calculated using Two-way variance analysis. In cases where gene expression was compared, the expression values of the relevant genes were determined relatively between the control and different concentrations. In the comparison of the groups, statistical significance was evaluated with the Student’s t-test analysis. In all analyzes, the significance value was determined as p < 0.05.
RESULTS
Cell viability
Cell viability results for chrysin, curcumin, and ellagic acid treatment in the cell lines are given in Fig. 1. Cell viability was decreased in a dose-dependent manner in both cancer and normal cell lines.
The optimal IC50 concentrations to be applied to A549, HEP3B, and MCF-7 cells at all subsequent stages were determined for 48 h (Table 2). Accordingly, it was found that all three therapeutic compounds showed cytotoxic effects at lower concentrations in cancer cell lines compared to normal non-transformed cells. When the three phenolic compounds were compared, ellagic acid was found most effective for the A549 and MCF-7 cell lines, while chrysin was for the HEP3B cells.
Wound healing (scratch)
A wound-healing assay was used to determine the cell migration effect of chrysin, curcumin, and ellagic acid in normal and cancer cell lines. According to the results of the wound-healing assay in normal fibroblast cells, the clefts remained open for 24 and 48 hours and healed at the lowest level with the migration ability of the cells being restricted. The phenolic compound treatment improved cellular migration, which significantly accelerated wound closure in L929 cells.
Comparative analysis has shown that all three phenolic compounds markedly inhibited the migration ability of A549 cell lines after 48 h incubation with wound healing being inhibited by chrysin by 422 ± 26 %, curcumin by 360 ± 8%, and ellagic acid by 477 ± 38 %. In the HEP3B cell line there was also an inhibitory effect of chrysin (145 ± 4 %), and curcumin (128 ± 9 %) after 48 h. In the MCF-7 cell line an inhibiting effect of chrysin (97 ± 2 %), curcumin (85 ± 3 %), and ellagic acid (98 ± 6%) after 24 h, and of chrysin (253 ± 8 %), curcumin (223 ± 7 %), and ellagic acid (153 ± 6 %) after 48 h was also observed. The wound-healing assay results for chrysin (CRY), curcumin (CUR), and ellagic acid (EA) effects on L929, A549, HEP3B, and MCF-7 cell lines are given in Fig. 2.
Effects of chrysin, curcumin, and ellagic acid on the number of live, apoptotic and dead cells
Apoptotic cell death after treatment of the cells with chrysin, curcumin, and ellagic acid are shown in Fig. 3. In cell lines where chrysin, curcumin, and ellagic acid were applied at IC50 concentrations, compared to the control it was found that the rate of live cells is significantly decreased and the rate of apoptotic cells significantly increased.
Effects of chrysin, curcumin, and ellagic acid on expression of genes involved in the apoptosis pathway and cell cycle
In the A549 cell line, mRNA expression of Bcl-2, Cas-3, Cas-8, Cas-10, CDK2, CDK4, and CDK6 was significantly increased after chrysin treatment compared to the control group whereas the expression level of Cas-9 and CCND2 genes was decreased. Treatment with curcumin significantly increased mRNA levels of Bax, Cas-3, Cas-9, Cas-10, CDK2, CDK4, and CDK6 whereas levels of Cas-8 and CCND2 expression were decreased. Ellagic acid treatment led to upregulation of Bax, Cas-3, Cas-8, Cas-9, Cas-10, CDK2, CDK4, CDK6, and CCND2 compared to the untreated control group whereas levels of Bcl2, CCNB1, and CCND2 were not changed (Table 3).
In HEP3B cells after chrysin treatment the levels of Bax, Bcl-2, Cas-3, Cas-10, CDK2, and CDK6 were significantly increased, whereas the levels of CDK4 and CCND2 were decreased compared to the control group. After treatment with curcumin, the levels of Bcl-2, Cas-3, Cas-9, Cas-10, CDK2, CDK4, and CDK6 were significantly increased, while the levels of CCND2 were decreased compared to the control group. Finally, in ellagic acid treatment led to increased levels of Bax, Cas-8, Cas-9, Cas-10, CDK2, CDK4, and CDK6 while the level of CCND2 was decreased compared to the control group (Table 4).
In MCF-7 cells after chrysin treatment levels of expression of mRNA of Bax, Cas-3, Cas-8, Cas-9, Cas-10, CDK2, CDK4, and CCND2 were significantly increased compared to the control group. After curcumin treatment mRNA expressions of Bcl-2, Cas-3, Cas-8, and CDK2 were increased whereas the expression level of Cas-10 was decreased compared to the controls. Ellagic acid treatment led to increased expressions of Bax, Bcl-2, Cas-3, Cas-8, Cas-9, Cas-10, CDK2, CDK6, CCNB1, and CCND2 compared to the control group on MCF-7 cells whereas CDK4 has not changed (Table 5).
Analysis of cell migration. Wound-healing assays were performed at 0, 24, and 48 h in L929, A549, HEP3B, and MCF-7 cells after treatment with IC50 concentrations of the compounds (chrysin—CRY, curcumin—CUR, and ellagic acid—EA) compared to untreated cells used as controls. Representative phase-contrast microscope images showing the area covered by the cells at 0, 24, and 48 h after wounding. Original magnification 10X. Graphic presentation of the data. *—Significant differences from control after 24 h, p < 0.05; #—significant differences from control after 48 h, p < 0.05, (n = 3).
The results of Annexin V-test after treatment of L929, A549, HEP3B, and MCF-7 cell lines with chrysin (CRY), curcumin (CUR), and ellagic acid (EA). *—Significantly reduced number of live cells compared to the control group taken as 100%. #—significantly increased number of apoptotic and dead cells compared to the control group, p < 0.05 (n = 3).
DISCUSSION
Many genetic mutations in cancer cells transform healthy cells into malignant ones, leading to excessive proliferation or decreased resistance to apoptosis. Uncontrolled proliferation and escape from apoptotic cell death are among the common features of all cancer types. For this reason, alternative approaches are sought in studies with potential antitumor agents, especially by targeting inhibition of proliferation and induction of apoptosis. For example, reactive oxygen species (ROS) or antioxidant inhibitors can selectively kill tumor cells or are likely to reduce tumor development and growth in several cancer cell lines. Therefore, ROS manipulation strategies that involve approaches to eliminate or generate ROS in cancer cells may be potentially effective treatments. ROS-mediated cancer cell proliferation was identified in the liver, lung, breast, and many other types of cancer [11, 12].
Curcumin (CUR) affects the activities of cytokines, enzymes, and transcription factors associated with inflammation and has also tumor growth inhibitory effects by promoting degradation of hypoxia-inducible factors (HIF) which have a central role in the adaptation and response to low oxygen levels in metazoan cells. Moreover, curcumin is also an iron chelator, showing the potential to inhibit HIF-α prolyl hydroxylase (PHD) activity [13]. Curcumin can inhibit the initiation of carcinogenesis by increasing glutathione S-transferase, induce cell cycle arrest at the S and G2/M phases, induce apoptosis, and inhibit metastasis by reducing the expression of CD31, vascular endothelial growth factor (VEGF), interleukin 8(IL-8), and miR-21 [14]. In a previous study on the HEP3B cell line, curcumin exhibited antiproliferative, anticancer, and anti-inflammatory activities [15]. Curcumin was shown to induce apoptosis through multiple signaling pathways; in particular, through inhibition of the Wnt pathway. Thus, developing a curcumin therapy was suggested as a new strategy for inhibiting cell proliferation and survival in hepatocellular carcinoma [15]. In the present study apoptotic gene expression as well as cell viability and migration were evaluated in liver cancer (HEP3B), lung (A549), and breast (MCF-7) cell lines. We found that curcumin exhibits cytotoxic effects on the A549, MCF-7, and HEP3B cell lines at lower doses compared to healthy fibroblasts. The cytotoxic effect of curcumin was found to be less effective in liver cancer cells HEP3B than in other cell lines (lung, breast cancer, and normal fibroblasts) when compared with each other. Moreover, curcumin inhibited the migration of all cancer cells analyzed. Similar to the cytotoxic effect, cell migration was less inhibited in HEP3B cells than in the other two cancer types.
In the apoptotic signaling pathway, the initiator caspases Cas-8, Cas-9, and Cas-10 are activated as a result of apoptotic signals from endogenous and extrinsic sources. Activation of Cas-9 in the intrinsic pathway causes increased expression of effector caspase Cas-3 and activation of Cas-8 causes increased expression of Cas-7 [16] which both further activate cell death machinery [17]. Activation of the proapoptotic gene Bax supports the increase of Cas-3/7-9 expressions together with the deterioration of mitochondrial membrane potential and causes caspase-dependent apoptotic cell death [18]. However, the specific binding of the anti-apoptotic Bcl-2 to Bax may cause the Bax/Bcl-2 balance to be disrupted and the cells to escape from apoptotic cell death [19]. As shown by Horn and colleagues Cas-10 is a negative regulator of Cas-8-mediated cell death and instead promotes CD95-induced gene induction [20]. Thus far, Cas-10 was reported to be a pro-apoptotic initiator caspase, similar to Cas-8 [21, 22]. Horn and colleagues argued the pro-apoptotic function of Cas-10, regardless of the cell line or the experimental setting used (siRNA-/shRNA-mediated knockout or gene knockout). Significantly, their reconstituted DISC approach clearly demonstrated the negative impact of Cas-10 on Cas-8 in a cell-free system [20]. A more complex role of Cas-10 has been proposed in a recent study demonstrating a pro-survival function of endogenous Cas-10 since it was shown to inhibit autophagic cell death in multiple myeloma cell lines [23]. In our study, Cas-10 and Cas-8 gene expression levels increased in all cancer cell lines treated with chrysin, while in hepatoma Cas-8 gene expression at mRNA levels did not change. Whereas Cas-10 gene expression was increased in all cancer cell lines treated with ellagic acid, Cas-8 gene expression was increased only in hepatoma and breast cancer cells but decreased in the lung cancer cells. When curcumin was applied, it was found that Cas-10 mRNA levels increased in hepatoma and lung cancer cells but decreased in breast cancer cells, whereas Cas-8, on the contrary, decreased in hepatoma and lung cancer cells and increased in breast cancer cells. As the carboxy-terminal half of Cas-10 that is involved in substrate recognition and binding to death-receptor-bound FADD (the adaptor protein of Fas-associated death domain) differs greatly from that of Cas-8, different roles for both caspases in death receptor-induced apoptosis are conceivable [24]. In the cell lines studied in this work, the ratio between the expression of Cas-10 and Cas-8 genes was different and to a different extent affected by the tested compounds. In our work, no changes were found in expression levels of cyclinB1 (CCNB1) which is a member of a highly conserved family of cyclins that are detected in nearly all human tissues and many cancer types.
A previous study examining chrysin (CRY) as a potential anticancer agent assessed its possible mechanisms of action in the human lung adenocarcinoma epithelial cell line and it was shown that it inhibits the growth of lung cancer cells by inducing apoptosis and inhibiting the activation of Cas-3 and Cas-9 through regulation of the Bcl-2 family [25]. In a study examining bladder cancer, chrysin was found to selectively inhibit the growth of bladder cancer cells T-24 and 5637 in a dose-dependent manner, but not to reduce the viability of normal immortalized urothelial SV-HUC-1 cells [26]. Similarly, non-transformed cells of different origins such as fibroblasts and epithelial cells were reported to be much more resistant to the cytotoxic effect of chrysin compared to malignant cells [26–28]. These findings indicate a selective antitumor effect of chrysin on targeting malignant cells and protecting non-cancerous cells. The antitumor effects of chrysin and the underlying potential mechanisms may be listed as the inhibition of cell viability and induction of the intrinsic pathway of apoptosis, activation of ER stress, and modulation of signal transducer and activator of transcription 3 (STAT3) expression, with the antitumor effects of chrysin being dependent on ROS formation [26]. A study of lung cancer cell line L132 demonstrated a loss of cell viability after treatment with chrysin in a time- and dose-dependent manner. Chrysin was also reported to induce apoptosis in several cancer cell lines such as cervical cancer HeLa cells, U937, HL-60, and L1210 leukemia cells, OE33 esophageal adenocarcinoma cells, and KYSE-510 esophageal squamous carcinoma cells [5]. Chrysin was found to have potential cytotoxicity and apoptotic properties in the breast cancer MCF-7 cell line [25]. In their study, Parajuli and colleagues found that chrysin at a concentration of 100 µM significantly inhibited the growth of aggressive breast cancer MDA-MB-231 cells after four days of treatment [29]. Our study has also demonstrated that chrysin exhibits cytotoxic effects on the lung (A549), liver (HEP3B), and breast (MCF-7) cancer cell lines at lower doses compared to healthy cells with the most pronounced effect being in the hepatoma cells. Chrysin also inhibited the migration of all cancer cells. No cell-type-specific differences were found between the apoptotic gene expression levels of chrysin administration in different types of cancer cells. Similar to curcumin administration, no change was found in CCNB1 gene expression levels in all three cell types after chrysin administration.
Antitumor activity of ellagic acid (EA) was first suggested after aromatase, a key enzyme that converts androgens to estrogens in breast cancer development was found to be inhibited by polyphenols derived from fresh pomegranate juice [30]. Liu and colleagues examined the inhibitory effect of ellagic acid on the viability of lung A549 cell lines and found that 48-hour treatment with ellagic acid significantly inhibited cell viability and induced apoptosis in a dose-dependent manner [31]. The analysis of the effect of ellagic acid on breast cancer cells demonstrated that it can significantly reduce the growth of human breast cancer cells in the submicromolar concentration range. In addition, colony formation and apoptosis showed that ellagic acid was a potent compound that could reduce the colonization of selected breast cancer cells and induce apoptosis [32]. Data on apoptosis are also in close agreement with some previous studies suggesting that ellagic acid induces apoptosis in lung A549 cells via the phosphoinositide 3-kinase/protein kinase B pathway [33]. Ellagic acid was shown to cause apoptosis and cell cycle arrest, and has a strong anti-proliferative potential against cancer and is thus considered a promising therapeutic anticancer compound. Dahiya and colleagues investigated the cytotoxicity and antiproliferative potential of ellagic acid on HepG2, A549, and HEK293 cells and reported that it significantly inhibited the growth of cancer cells in a dose-dependent manner. This effect was also CDK6-dependent [34]. Therefore, it is believed that ellagic acid may be a therapeutic agent for CDK6-targeted therapies in cancer cells with high CDK6 expression [35]. A study examining the efficacy of ellagic acid in reducing hepatocarcinogenesis in rats found that it also had a chemo-preventive function [36]. Another study found ellagic acid to inhibit the proliferation of breast MCF-7 cells, mainly by stopping the cell cycle at the G0/G1 phase [37]. In our study ellagic acid was found to exhibit cytotoxic effects on the A549 and MCF-7 cell lines at lower doses than in healthy fibroblast cells. In this regard, ellagic acid exhibited a similar cytotoxic profile to curcumin. Ellagic acid inhibited the migration of A549 and MCF-7 cells but had no anti-migration effects on HEP3B cells.
In our study, it was found that ellagic acid increased the levels of Bax and Bcl-2 expressions in the HEP3B cancer cell line. However, considering the Bax/Bcl-2 (29.79/3.41) ratio, it can be concluded that a positive shift toward Bax leads to apoptotic cell death. Similarly, curcumin treatment showed the same effect on the A549 cell line. Also, all of the phenolic compounds promoted apoptotic cell death with a significant increase in Bax expression in the MCF-7 cell line. Because there were increases in caspase expression levels (Cas-3, Cas-8, Cas-9, and Cas-10) after treatment with chrysin, curcumin, and ellagic acid in the studied cancer cell lines compared with controls it can be concluded that apoptotic cell death occurs by a caspase-dependent mechanism. The decreased expression level of Bcl-2 and increased expression level of Bax can induce apoptotic cell death and eliminate cancer cells. It has been stated that if the ratio of Bax/Bcl-2 shows a positive increasing value, it causes cell death as a result of disruption of the mitochondrial membrane potential. This can be explained by the activation of Cas-9, one of the pro-apoptotic caspase genes, as a result of decreased Bcl-2 inhibitory effect on Bax [38].
Numerous studies have reported that some anti-cancer agents stimulate the cell cycle arrest checkpoint, thereby inducing apoptotic cell death. The central machinery driving cell cycle progression is regulated by cell cycle-specific cyclins and CDKs modulated by interactions with CDK inhibitors. Compounds that activate CDK2 induce apoptosis by arresting the cell cycle. Inhibition of CCND2, a cyclin that functions in the cell cycle, specifically the G1/S transition, can suppress proliferation and metastasis in cancer cells. Inhibition of CCNB1 can cause the cell cycle to arrest in the G2/M phase. The increased expression of other cell cycle components may be due to increased translation efficiency or protein stability [39].
Chrysin and curcumin can arrest the cell cycle at the G1/S phase by inhibiting CCDN2 expression as it was found in the A549 cell line. Similarly; chrysin, curcumin, and ellagic acid can stop the cell cycle at the G1/S phase in the HEP3B cell line. Finally, in the MCF-7 cell line, chrysin and curcumin can inhibit CCNB1 expression, and arrest the cell cycle at the G2/M phase.
CONCLUSIONS
Analysis of the antiproliferative and anti-migration effects of chrysin, curcumin, and ellagic acid on the human cancer cell lines A549, HEP3B, and MCF-7 demonstrated that polyphenolic compounds have cell type-dependent effects on cellular metabolism. Our data suggest that although these compounds do not have a single target of action in particular cancer cells, they affect the migration and proliferation of cancer cells. Our study found that the cytotoxic and anti-tumoral effects of chrysin, curcumin, and ellagic acid in cancer cell lines involve inhibition of cell cycle G1/S or G2/M checkpoints and induction of apoptotic cell death via a caspase-dependent pathway. Therefore, we confirm that this group of compounds may serve as important therapeutic measures for cancer treatment.
REFERENCES
Falzone L, Salomone S, Libra M (2018) Evolution of Cancer Pharmacological Treatments at the Turn of the Third Millennium. Front pharmacol 9: 1300. https://doi.org/10.3389/fphar.2018.01300
Khan T, Ali M, Khan A, Nisar P, Jan SA, Afridi S, Shinwari ZK (2019) Anticancer Plants: A Review of the Active Phytochemicals, Applications in Animal Models, and Regulatory Aspects. Biomolecules 10: 47. https://doi.org/10.3390/biom10010047
Samarghandian S, Azimi-Nezhad M, Borji A, Hasanzadeh M, Jabbari F, Farkhondeh T, Samini M (2016) Inhibitory and cytotoxic activities of chrysin on human breast adenocarcinoma cells by induction of apoptosis. Pharmacogn Mag 12: 436–440. https://doi.org/10.4103/0973-1296.191453
Panche AN, Diwan AD, Chandra SR (2016) Flavonoids: an overview. J Nutr Sci 5: e47. https://doi.org/10.1017/jns.2016.41
Mehdi SH, Zafaryab M, Nafees S, Khan A, Ahmad I, Hafeez ZB, Rizvi MA (2019) Chrysin sensitizes human lung cancer cells to tumour necrosis factor related apoptosis-inducing ligand (TRAIL) mediated apoptosis. Asia Pac J Clin Oncol 4(2): 27–33. DOI 10.31557/APJCB.2019.4.2.27-33
Zhang H, Li X, Wu K, Wang M, Liu P, Wang X, Deng R (2017) Antioxidant Activities and Chemical Constituents of Flavonoids from the Flower of Paeonia ostii. Molecules 22: 5. https://doi.org/10.3390/molecules22010005
Stanić Z (2017) Curcumin, a Compound from Natural Sources, a True Scientific Challenge-A Review. Plant Foods Hum Nutr 72(1): 1–12. https://doi.org/10.1007/s11130-016-0590-1
Alfei S, Marengo B, Zuccarı G (2020) Oxidative stress, antioxidant capabilities, and bioavailability: Ellagic acid or urolithins? Antioxidants 9(8): 707. https://doi.org/10.3390/antiox9080707
Abotaleb M, Samuel SM, Varghese E, Varghese S, Kubatka P, Liskova A, Büsselberg D (2018) Flavonoids in Cancer and Apoptosis. Cancers (Basel) 11(1): 28. https://doi.org/10.3390/cancers11010028
Liang Cc, Park Ay, Guan JL (2007) In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nat Protoc 2: 329–333. https://doi.org/10.1038/nprot.2007.30
Glasauer A, Chandel NS (2014) Targeting antioxidants for cancer therapy. Biochem Pharmacol 92: 90–101. https://doi.org/10.1016/j.bcp.2014.07.017
Carrasco-Torres G, Baltıérrez-Hoyos R, Andrade-Jorge E, Vılla-Treviño S, Trujillo-Ferrara JG, Vásquez-Garzón VR (2017) Cytotoxicity, oxidative stress, cell cycle arrest, and mitochondrial apoptosis after combined treatment of hepatocarcinoma cells with maleic anhydride derivatives and quercetin. Oxid Med Cell Longev 2017: 2734976. https://doi.org/10.1155/2017/2734976
Ströfer M, Jelkmann W, Depping R (2011) Curcumin decreases survival of Hep3B liver and MCF-7 breast cancer cells: the role of HIF. Strahlenther Onkol 187: 393–400. https://doi.org/10.1007/s00066-011-2248-0
Alam MN, Almoyad M, Huq F (2018) Polyphenols in colorectal cancer: current state of knowledge including clinical trials and molecular mechanism of action. Biomed Res Int 2018: 4154185. https://doi.org/10.1155/2018/4154185
Kim HJ, Park SY, Park OJ, Kim YM (2013) Curcumin suppresses migration and proliferation of Hep3B hepatocarcinoma cells through inhibition of the Wnt signaling pathway. Mol Med Rep 8: 282–286. https://doi.org/10.3892/mmr.2013.1497
Boatright KM, Renatus M, Scott FL, Sperandio S, Shin H, Pedersen IM, Ricci JE, Edris WA, Sutherlin DP, Green DR, Salvesen GS (2003) A unified model for apical caspase activation. Mol Cell 11: 529–541. https://doi.org/10.1016/S1097-2765(03)00051-0
Singh N (2007) Apoptosis in health and disease and modulation of apoptosis for therapy: An overview. Indian J Clin Biochem 222: 6–16. https://doi.org/10.1007/BF02913307
Kim EJ, Kim GT, Kim BM, Lim EG, Kim SY, Kim YM (2017) Apoptosis-induced effects of extract from Artemisia annua Linné by modulating PTEN/p53/PDK1/Akt/ signal pathways through PTEN/p53-independent manner in HCT116 colon cancer cells. BMC Complement Altern Med 17: 1–12. https://doi.org/10.1186/S12906-017-1702-7/FIGURES/7
Anantram A, Degani M (2019) Targeting cancer’s Achilles’ heel: role of BCL-2 inhibitors in cellular senescence and apoptosis. 11: 2287–2312. https://doi.org/10.4155/FMC-2018-0366
Horn S, Hughes MA, Schilling R, Sticht C, Tenev T, Ploesser M, Meier P, Sprick MR, MacFarlane M, Leverkus M (2017) Caspase-10 negatively regulates caspase-8-mediated cell death, switching the response to CD95L in favor of NF-κB activation and cell surv Cell Rep 19: 785–797. https://doi.org/10.1016/j.celrep.2017.04.010
Engels IH, Totzke G, Fischer U, Schulze-Osthoff K, Jänicke RU (2005) Caspase-10 sensitizes breast carcinoma cells to TRAIL-induced but not tumor necrosis factor-induced apoptosis in a caspase-3-dependent manner. Mol Cell Biol 25: 2808–2818. https://doi.org/10.1128/MCB.25.7.2808-2818.2005
Fischer U, Stroh C, Schulze-Osthoff K (2006) Unique and overlapping substrate specificities of caspase-8 and caspase-10. Oncogene 25: 152–159. https://doi.org/10.1038/sj.onc.1209015
Lamy L, Ngo VN, Emre NCT, Shaffer AL 3rd, Yang Y, Tian E, Nair V, Kruhlak MJ, Zingone A, Landgren O, Staudt LM (2013) Control of autophagic cell death by caspase-10 in multiple myeloma. Cancer Cell 23: 435–449. https://doi.org/10.1016/j.ccr.2013.02.017
Fernandes-Alnemri TRC, Armstrong J, Krebs SM, Srinivasula L, Wang F, Bullrich LC, Fritz JA, Trapani KJ, Tomaselli G, Litwack ES (1996) In vitro activation of CPP32 and Mch3 by Mch4, a novel human apoptotic cysteine protease containing two FADD-like domains. Proc Natl Acad Sci 93: 7464–7469. https://doi.org/10.1073/pnas.93.15.7464
Samarghandian S, Nezhad MA, Mohammadi G (2014) Role of caspases, Bax and Bcl-2 in chrysin-induced apoptosis in the A549 human lung adenocarcinoma epithelial cells. Anticancer Agents Med Chem 14: 901–909. https://doi.org/10.2174/1871520614666140209144042
Xu Y, Tong Y, Ying J, Lei Z, Wan L, Zhu X, Ye F, Mao P, Wu X, Pan R, Peng B, Liu Y, Zhu J (2018) Chrysin induces cell growth arrest, apoptosis, and ER stress and inhibits the activation of STAT3 through the generation of ROS in bladder cancer cells. Oncol Lett 15: 9117–9125. https://doi.org/10.3892/ol.2018.8522
Zhang H, Li X, Wu K, Wang M, Liu P, Wang X, Deng R (2016) Antioxidant activities and chemical constituents of flavonoids from the flower of paeonia ostii. Molecules 22: 5. https://doi.org/10.3390/molecules22010005
Cárdenas M, Marder M, Blank VC, Roguın LP (2006) Antitumor activity of some natural flavonoids and synthetic derivatives on various human and murine cancer cell lines. Bioorg Med Chem 14: 2966–2971. https://doi.org/10.1016/j.bmc.2005.12.021
Parajuli P, Joshee N, Rimando AM, Mittal S, Yadav AK (2009) In vitro antitumor mechanisms of various Scutellaria extracts and constituent flavonoids. Planta medica75: 41–48. https://doi.org/10.1055/s-0028-1088364
Kim ND, Mehta R, Yu W, Neeman I, Livney T, Amichay A, Poirier D, Nicholls P, Kirby A, Jiang W, Mansel R, Ramachandran C, Rabi T, Kaplan B, Lansky E (2002) Chemopreventive and adjuvant therapeutic potential of pomegranate (Punica granatum) for human breast cancer. Breast Cancer Res Treat 71: 203–217. https://doi.org/10.1023/a:1014405730585
Liu Q, Liang X, Niu C, Wang X (2018) Ellagic acid promotes A549 cell apoptosis via regulating the phosphoinositide 3-kinase/protein kinase B pathway. Exp Ther Med 16: 347–352. https://doi.org/10.3892/etm.2018.6193.
Yousuf M, Shamsi A, Khan P, Shahbaaz M, AlAjmi MF, Hussain A, Hassan GM, Islam A, Rizwanul Haque QM, Hassan MI (2020) Ellagic Acid Controls Cell Proliferation and Induces Apoptosis in Breast Cancer Cells via Inhibition of Cyclin-Dependent Kinase 6. Int J Mol Sci. 21: 3526. https://doi.org/10.3390/ijms21103526
Liu Q, Liang X, Niu C, Wang X (2018) Ellagic acid promotes A549 cell apoptosis via regulating the phosphoinositide 3-kinase/protein kinase B pathway. Exp Ther Med. 16: 347–352. https://doi.org/10.3892/etm.2018.6193
Dahiya R, Mohammad T, Gupta P, Haque A, Alajmi MF, Hussain A, Hassan MI (2019) Molecular interaction studies on ellagic acid for its anticancer potential targeting pyruvate dehydrogenase kinase 3. RSC Adv 9: 3302–23315. https://doi.org/10.1039/c9ra02864a
Gupta P, Mohammad T, Khan P, Alajmi MF, Hussain A, Rehman MT, Hassan MI (2019) Evaluation of ellagic acid as an inhibitor of sphingosine kinase 1: A targeted approach towards anticancer therapy. Biomed Pharmacother 118: 109245. https://doi.org/10.1016/j.biopha.2019.109245
Ceci C, Lacal PM, Tentori L, De Martino MG, Miano R, Graziani G (2018) Experimental evidence of the antitumor, antimetastatic and antiangiogenic activity of ellagic acid. Nutrients 10: 1756. https://doi.org/10.3390/nu10111756
Chen HS, Bai MH, Zhang T, Li GD, Liu M (2015) Ellagic acid induces cell cycle arrest and apoptosis through TGF-β/Smad3 signaling pathway in human breast cancer MCF-7 cells. Int J Oncol 46: 1730–1738. https://doi.org/10.3892/ijo.2015.2870
Ramadan MA, Shawkey AE, Rabeh MA, Abdellatif AO (2019) Expression of P53, BAX, and BCL-2 in human malignant melanoma and squamous cell carcinoma cells after tea tree oil treatment in vitro. Cytotechnology 71: 461–473. https://doi.org/10.1007/s10616-018-0287-4
Chen J (2016) The Cell-cycle arrest and apoptotic functions of p53 in tumor ınitiation and progression. Cold Spring Harb Perspect Med 6: a026104. https://doi.org/10.1101/cshperspect.a026104
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Concept: Songül Ünüvar, Neşe Başak Türkmen, Hande Yüce; Design: Songül Ünüvar, Neşe Başak Türkmen, Dilan Aşkın Özek; Materials: Neşe Başak Türkmen, HandeYüce; Analysis and/or interpretation: Yasemin Şahin, Osman Çiftçi; Literature review: Songül Ünüvar, Neşe Başak Türkmen, Hande Yüce; Writing the article: Songül Ünüvar, Hande Yüce.
Corresponding author
Ethics declarations
CONFLICT OF INTEREST
The authors declare that they have no conflict of interests.
Rights and permissions
About this article
Cite this article
Yüce, H., Şahin, Y., Türkmen, N.B. et al. Apoptotic, Cytotoxic and Antimigratory Activities of Phenolic Compounds. J Evol Biochem Phys 58, 1819–1833 (2022). https://doi.org/10.1134/S0022093022060138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0022093022060138