Abstract
Skeletal muscles mainly contribute to the emergence of insulin resistance, impaired glucose tolerance and the development of type 2 diabetes. Molecular mechanisms that regulate glucose uptake are diverse, including the insulin-dependent as most important, and others as also significant. They involve a wide range of proteins that control intracellular traffic and exposure of glucose transporters on the cell surface to create an extensive regulatory network. Here, we highlight advantages of the omics approaches to explore the insulin-regulated proteins and genes in human skeletal muscle with varying degrees of metabolic disorders. We discuss methodological aspects of the assessment of metabolic dysregulation and molecular responses of human skeletal muscle to insulin. The known molecular mechanisms of glucose uptake regulation and the first results of phosphoproteomic and transcriptomic studies are reviewed, which unveiled a large-scale array of insulin targets in muscle cells. They demonstrate that a clear depiction of changes that occur during metabolic dysfunction requires systemic and combined analysis at different levels of regulation, including signaling pathways, transcription factors, and gene expression. Such analysis seems promising to explore yet undescribed regulatory mechanisms of glucose uptake by skeletal muscle and identify the key regulators as potential therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Currently, 15-25% of adult population are diagnosed with obesity in most of the European countries. According to WHO estimates, more than 40% of their population will have excessive body weight by 2030. Obesity is the main risk factor for emergence of insulin resistance (IR), which leads to the development of hyperglycemia and type 2 diabetes (T2DM), vascular dysfunction, kidney and vision impairments, cardiovascular and oncological complications [1, 2]. This underlies the systemic and interrelated nature of metabolic disorders, imposing restrictions on their studies directly in humans. IR is manifested as an impaired capacity of tissues to absorb glucose from the blood in response to insulin. In terms of plasma glucose regulation, the main targets of insulin are the liver, fat, and skeletal muscle tissues. Normally skeletal muscles make up 30-40% of the body mass. Even at rest they account for up to 80% of insulin-dependent glucose uptake [3]. This indicates the exclusive role of skeletal muscle in the development of metabolic disorders and emphasizes importance of studying the molecular mechanisms of IR development in this tissue.
Studying differences in metabolic parameters in skeletal muscle biopsies taken from individuals with different levels of metabolic disorders allows identifying the most pronounced changes in the expression and/or activity of enzymes and signaling proteins. Animal models including gene knockout and transgenic animals allow to expand experimental capabilities and compare dynamics of molecular and pathophysiological changes [4, 5]. However, increasing evidence reveals differences in metabolism between rodents and humans. In addition, animals are resistant to T2DM development. In particular, the lifespan of rodents is too short to reach the end stages of T2DM. Therefore, the results obtained in animal models must be cautiously translated to humans [6]. Finally, cell models are very useful for studying the dynamics of intracellular responses, including signal responses to insulin and other stimuli [7, 8]. They are convenient for modeling individual stages of T2DM pathogenesis (such as hyperlipidemia, hyperinsulinemia, or hyperglycemia) [9-11] and to explore epigenetic changes that occur in obesity and T2DM [12-15].
It became recently clear that insulin activates a large number of signaling molecules in cells that are integrated into an extended network [7, 8]. Also became apparent a large-scale pattern of molecular changes that accompany IR appearance and progression of T2DM [16, 17]. The omics approaches grow important for studying multicomponent signaling systems in cells. They allow simultaneous monitoring of thousands of molecular events associated with changes in the content of proteins and metabolites, their modification, gene expression, epigenome, and metabolome. Comprehensive bioinformatic processing of these “big data” allows to track down causative relationships and clue in the key molecular mechanisms and regulators, which altered function is associated with the development of metabolic disorders.
This review focuses on the results of only a few studies so far that have attempted to link the molecular changes in skeletal muscle to progression of systemic metabolic disorders in the humans and animals. We first discuss the means for assessment of systemic IR and comparative analysis of the changes associated with the development of IR and T2DM. To highlight the large scale of these changes even at the primary molecular level, intracellular pathways of glucose uptake regulation are discussed. Finally, we review the current high-throughput results and their potential to create comprehensive framework of these changes, which could help identify the relevant therapeutic targets.
ASSESSEMENT OF SYSTEMIC INSULIN SENSITIVITY
There is still no clear picture of the molecular changes, including in skeletal muscle, during T2DM development. This is because these changes are many and interconnected, do not occur discretely, but develop gradually with time and vary according to individual characteristics of a person. Studying their dynamics involves analysis of biopsy samples from volunteers stratified by the degree of metabolic alterations. For this purpose, reference indicators have been determined and generally accepted, based on the data from many clinical studies [18-20]. They are the fasting levels of insulin or glucose in the blood plasma (i.e., before the start of glucose tolerance test), the blood glucose after 2 h of glucose tolerance test, and glycated hemoglobin (A1C). Patients are stratified based on these indicators or their combinations (see below).
Obesity associated with accumulation of mostly visceral fat is the main risk factor for the development of metabolic disorders, IR and T2DM [18]. This condition is associated with chronic excessive food intake (so-called Western diet) and reduced energy expenditure because of a sedentary lifestyle. Clinical manifestations are usually long absent [21, 22]. Progressive obesity leads to impaired fat metabolism, development of latent inflammation in adipose tissues, and adipocyte dysfunction [23, 24]. This includes decreased secretion of adiponectin, which sensitizes cells to insulin, while secretion of pro-inflammatory cytokines and lipolysis in adipose tissue increase. As a result, levels of free fatty acids and triglyceride-rich lipoproteins in the blood plasma increase, leading to accumulation of ectopic fat in visceral tissues including skeletal muscle [21, 25, 26]. These factors are considered as the main triggers of IR in skeletal muscle [16, 27].
IR can persist for years in a latent form without clinical manifestations. This is because the increased secretion of insulin compensates for reduced cell responses thus maintaining carbohydrate and fat metabolism at proper level [22]. The first signs of uncompensated IR manifest as slight increases in fasting blood glucose from 5.6 to 7.8 mM (IFG, impaired fasting glucose) and/or as systemic impairment of glucose tolerance (IGT, impaired glucose tolerance) [18-20] (Fig. 1, a and b). The individual or combined manifestation of these parameters reflects the heterogeneity of T2DM pathogenesis and can also be used for stratification of patients [19]. IGT is determined by glucose tolerance test as an increased concentration of blood glucose (7.8-11 mM) 2 h after consumption of 75 g of glucose after the overnight fast [18]. In pre-diabetes state the fasting insulin levels are elevated only sometimes, but they are always higher in response to glucose load (Fig. 1, a and c). Thus, IFG reflects the defects of both insulin-dependent and insulin-independent mechanisms of glucose utilization [28], whereas IGT reflects impaired glucose uptake by tissues is response to stimulation with endogenous insulin.
Reference values (a) and changes in the blood levels of glucose (b) or insulin (c) during oral glucose tolerance test (OGTT) commonly used to assess the severity of carbohydrate metabolism disorder. The curves in (b) and (c) were compiled based on the results obtained in more than 5000 volunteers [20]. In the table and on the y-axes of the graphs the reference indicator values for impaired fasting glucose (IFG), impaired glucose tolerance (IGT), and type 2 diabetes mellitus (T2DM) are shown. The arrow indicates shift of the indicator value during long-term T2DM. The insulin level is traditionally expressed in international units (milliequivalents, ME) that quantitatively define therapeutic effect of insulin without taking into account its molecular mass (c). One insulin unit is equivalent to 0.0347 mg of insulin, and 100 µME/ml corresponds to insulin concentration of 0.6 pM.
T2DM is characterized by a steady increase in fasting glucose level (>7 mM) and that after 2 h of glucose tolerance test (>11 mM) (Fig. 1, a and b) [18]. In the early stages of T2DM the fasting blood insulin level is often increased (>9 µME/ml), but the peak insulin concentration in the blood does not change during the glucose tolerance test and decreases in the late stages of the disease (Fig. 1c). This is due to progressive dysfunction of pancreatic β-cells and impaired insulin secretion. As a result, the insulin-dependent tissues decrease glucose uptake after a meal, and stable hyperglycemia develops. At this stage the pathology of T2DM becomes virtually irreversible, combining the main features of type 1 and 2 diabetes, and treatment becomes symptomatic.
Absence of clinically relevant markers of molecular changes in skeletal muscle during IR and of the markers of β-cell dysfunction complicates tracking progression of the disease, stratification of patients for obtaining the biopsy samples, and interpretation of the results of its comparative analysis. To resolve the problem, the reference values for blood glucose and insulin levels being obtained during glucose tolerance test are used (Fig. 1a). They enable stratification and comparison of subject groups [18] including in large cohorts [19, 20].
Glucose tolerance test is rather simple and routinely used to acquire the indicators of carbohydrate metabolism (including IFG and IGT). It reports on the initial (fasting) state and the systemic response to an increase in endogenous insulin (the changes in plasma glucose/insulin levels). Since the latter itself depends on how far the pathology has progressed, exact quantification of insulin sensitivity using glucose tolerance test is not possible. It is important that this test uses a standard dose of glucose (75 g) for all subjects, which complicates comparison and interpretation of the results for individuals who differ significantly in body mass.
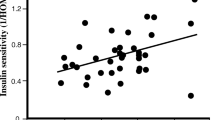
The hyperinsulinemic euglycemic clamp test is used as a “gold standard” for quantification of systemic IR [29]. Insulin and glucose are simultaneously infused into the blood, with the rate of insulin infusion gradually adjusted in such a way that its level (100 µME/ml) becomes comparable with the maximum physiological response to a meal. The rate of glucose infusion is adjusted to maintain its blood level constant. After 2-3 h an equilibrium is reached between the rate of glucose administration and utilization by tissues. This balance is further maintained for 1-2 h, and the M-index of systemic insulin sensitivity is calculated from the amount of glucose injected (and utilized) during this period. The use of several such tests with different target insulin concentrations allowed to evaluate the relationship between insulin concentration and glucose utilization [30] (Fig. 2). This relationship shifts to the right with IR development reflecting a decrease in tissue sensitivity to insulin (presence of IFG and/or IGT). In the later stages of T2DM not only the sensitivity to insulin, but also the maximum response to insulin decreases, which reflects dysfunction of β-cells. The relationship shown in Fig. 2 shifts to the right and down.
Changes in the relationship between the rate of glucose utilization and concentration of exogenous insulin during progression of IR and T2DM. Summarized results of several euglycemic clamp tests with different equilibrium insulin concentrations [30] are presented schematically. The vertical line corresponds to the steady-state insulin concentration of 100 µME/ml used in the standard clamp test. Abbreviations are as in Fig. 1.
The decrease in systemic insulin sensitivity measured using standard hyperinsulinemic euglycemic clamp test reflects a decrease in tissue glucose utilization at the most indicative concentration of blood insulin, 100 µME/ml (the vertical dotted line in Fig. 2). At the same time, this test does not allow to estimate either the maximum response to insulin or the response to its single administration. During the clamp test the high insulin level is long maintained, after which a biopsy is usually taken. However, such a prolonged and pronounced increase in blood insulin (~100 µME/ml) is not observed after a meal in healthy individuals and even in patients with IR [22]. Therefore, changes in intracellular signaling and gene expression after clamp test should be interpreted with caution. In addition, cell studies have shown that insulin induces fast (several minutes) and dynamically changing signaling responses [7, 12, 13, 31, 32], while significant time is spent to reach steady-state in the clamp test. This implies that the clamp test is not ideal for studying the full spectrum of skeletal muscle molecular responses to insulin.
A helpful alternative in studying molecular responses to insulin in vivo is measuring them under conditions as close to physiological as possible, such as after a meal that is normalized to the body mass or basal rate of metabolism [22]. Similar approach was used to study diurnal changes in skeletal muscle phosphoproteome in rodents [33]. It also appears promising for human studies while using glucose or a mixed meal normalized to the body mass or basal rate of metabolism. Insulin secretion after a meal is much higher in obese individuals, which is not simply due to the presence of IR, but also to a larger quantity of consumed meal. Thus, such normalization allows to better represent the differences in molecular muscle responses to insulin in people with IR and normal metabolism. This approach has not been yet used to investigate the molecular responses in human skeletal muscle.
MOLECULAR MECHANISMS OF GLUCOSE UPTAKE ARE MULTIPLE
The molecular mechanisms of IR have been linked to impaired intracellular regulation of glucose uptake by muscle and fat cells [34]. The defects may occur in direct regulators of glucose transport [27, 35] and be sensitive to signaling molecules of different cascades that control their activity, such as insulin signalling [16, 17] and other cascades [36]. They are closely associated with the imbalance of metabolic fluxes that occur in obesity [23, 25, 27]. Activation of glucose uptake occurs in several steps; each requires its own regulators that act combinatorially [37-39]. In the resting state the principal insulin-dependent glucose transporter Glut4 is stored in cells in special vesicles (Glut4 storage vesicles, GSV) [40]. These are the stationary vesicles kept in the cytosol and released after binding a set of regulators [37]. Then they translocate to the cell periphery, pass through the cortical cytoskeleton beneath cell membrane, get positioned, and fuse thus exposing the functional Glut4 on the cell surface (Fig. 3). So far there is no clear perception of those molecules which function is crumpled in IR and T2DM. These can be both elements of the signaling cascades and their final targets that directly control the translocation and exposure of glucose transporters, or their combinations.
Signaling regulatory mechanisms of glucose uptake linked to GLUT4 in muscle cells. In addition to the canonical insulin cascade (highlighted in red), which mainly regulates translocation of the GLUT4-containing vesicles from the cytosol to the cell membrane, the putative noncanonical insulin cascade (shown in green) regulates the approach, positioning, and fusion of the vesicles with the membrane, ensuring exposure of GLUT4 on the cell surface. The insulin-independent mechanism involving AMPK/NUAK2 (highlighted in blue) is responsible for GLUT4 exposure and glucose uptake in response to contraction and increase in intracellular AMP level. The dashed lines show the coupling of these cascades to activation of transcription factors (TF) and gene expression.
The canonical insulin cascade (receptor→protein IRS→PI3-kinase (PI3K)→Akt→TBC1D4 (AS160)→Rab GTPase→Glut4) is considered as the main signaling pathway to activation of glucose uptake by insulin in animals and humans (Fig. 3). It largely regulates the translocation step of GSV to the cell periphery via the GAP-protein TBC1D4 (aka AS160) and GTPases Rab8a and Rab13 (in muscle cells) or Rab10 (in adipocytes) [38, 39]. However, a large body of evidence is accumulated that in humans with systemic IR the activity of this cascade as measured at the level of Akt is not always reduced or not to the same extent as the insulin-stimulated glucose uptake [27, 41, 42]. There could be few reasons for this phenomenon. First, the canonical insulin signaling can be most altered within its distal part, downstream of Akt [27]. Second, altered may be activities of the direct regulators of GSV activation in the near-membrane compartment [38] or of the vesicle exocytosis [39], which are controlled via branches of the canonical cascade or other insulin receptor signaling pathways collectively shown as a putative non-canonical insulin cascade in Fig. 3. Finally, additional activation of Akt can be achieved from other receptors associated with the PI3-kinase cascade but not intended to target GSV. In this regard the key role of the Akt2 isoform in regulation of glucose uptake may merit attention [43]. The question remains as to whether Akt1 and Akt2 can be differently activated by different receptors such as the insulin receptor or the insulin-like growth factor (IGF-1) receptor.
The need of simultaneous involvement of several different regulators at each step of GSV traffic, differences in mechanisms of their activation and combinatorial pattern of their action render the regulation of GSV traffic an extensive network organization. It is depicted in an aggregate form in Fig. 3 as a non-canonical insulin cascade. Whereas its details are beyond the scope of this review and are highlighted by others [35, 37-40], two mechanisms are worth mentioning. Both are required and both regulate the exposure of glucose transporters independently of Akt or distal targets of the canonical insulin cascade. One involves activation of Rac1 GTPase by PI3-kinase; this causes rearrangement of cortical cytoskeleton to enable approach of GSV to the cell membrane. Another mechanism is initiated directly from the insulin receptor; it requires Ca2+ ions and involves the classic complex of SNARE proteins that mediate GSV fusion with cell membrane and transporter exposure.
Many regulators of vesicle traffic, including TBC1D4/AS160 and Rab GTPases, control not only one traffic step, but are also critical for other steps acting in concert with other regulators. Thus, the transporter exposure and glucose uptake are under multiple control of both the canonical and non-canonical insulin targets, many of which are still unknown [35]. It is plausible that the decrease in insulin sensitivity of glucose uptake is not only due to the loss of one of them, but is a result of coordinated dysfunction in a group of such targets.
Alternative mechanisms may regulate fasting glucose homeostasis (when insulin level is very low) and especially in response to contractile (physical) activity. They include AMP-activated protein kinase (AMPK) [44] and related kinases (Fig. 3). The latter comprise a group of 12 enzymes [45], which functions are still poorly understood. However, at least two of them, the AMPK-related kinases NUAK1 [46] and NUAK2 [47], are involved in regulation of blood glucose levels. Similar to AMPK, NUAK2 mediates the insulin-independent mechanism of glucose uptake aided by AMP and LKB1 kinase. Unlike the insulin-dependent mechanism, it is mediated mainly by the Rab14 GTPase and its regulator TBC1D1 [38]. Significance of the alternative mechanisms stems from the results of selective skeletal muscle knockout of insulin and IGF-1 receptors [48], or Akt1/2 isoforms [49], or overexpression of Akt2 in skeletal muscle [33]. The insulin sensitivity was not altered in these mice even after a high-fat diet [33]. In addition, AMPK is activated by physical exercise and improves glucose uptake from the blood by skeletal muscle [28], whereas AMPK activity is decreased in individuals with obesity and IR [50, 51].
The presence of several mechanisms that regulate Glut4 traffic and glucose uptake in skeletal muscle expands the list of signaling proteins which disturbed activity can be causative of IR. They are not only of the fundamental interest, but are also potential targets for antidiabetic therapeutics. Changes in their activity in individuals with obesity, IR, or T2DM can be caused both by changes in their posttranslational modifications (mainly phosphorylation) and by their altered intracellular content. Considering the long progression of IR and diversity of the molecules involved, it is plausible that these changes are associated with altered activities of a number of transcription factors (TF) and gene expression (Fig. 3) which strengthen the IR state and subsequent diabetic phenotype.
SKELETAL MUSCLE PROTEOME CHANGES IN IR AND T2DM
It is recognized that up to 10,000 proteins are expressed in each tissue regardless of their isoforms [52]. It is hardly possible to detect even one third of them in skeletal muscle samples, and those detected are mostly abundant sarcomeric proteins. They limit significantly the depth of proteomic analysis by mass-spectrometry.
The skeletal muscle proteome of individuals with metabolic disorders has been explored in a number of studies. The most detailed study with 148 volunteers (healthy individuals, patients with IR, with or without T2DM) evaluated changes in the content of more than 2000 proteins [53]. While only less than 100 proteins changed their expression in IR, much larger changes were found in T2DM patients. Of more than 400 proteins that changed the content, only a few have increased. They were primarily sarcomeric proteins typical for the fast twitch muscle fibers (isoforms of myosin heavy and light chains, troponin, tropomyosin). In contrast, many proteins reduced the content. These were mitochondrial enzymes and transporters, regulators of amino acid metabolism and protein synthesis [the mechanistic target of rapamycin (MTOR), elongation factor 2, ribosomal proteins], proteasomal and heat shock proteins, as well as a number of protein kinases (the myosin light chain kinase SPEG, CAMK2G, MAPK12, etc.). Interestingly, in the T2DM group these changes overlapped with changes in protein phosphorylation (see below). However, the proteome analysis does not suggest mechanism of the changes, implying importance of a more specific analysis of transcriptome and post-translational modifications, especially of the phosphoproteome.
SKELETAL MUSCLE PHOSPHOPROTEOME CHANGES IN IR AND T2DM
Phosphorylation is one of the major means of signal transduction in cells. There are hundreds of the kinases capable of phosphorylating several substrates each, and the total number of phosphorylation sites may reach 100,000 [54]. Immunoblotting allows only about a dozen different phosphorylation sites to be assessed in a study, depending on antibody availability and specificity. In contrast, the mass-spectrometry analysis of phosphoproteome allows to simultaneously detect more than 10,000 different phosphorylated sites in several thousand different proteins and, based on these data, to predict the kinases that changed the activity. In skeletal muscle samples, phosphosites are mainly detected in most abundant proteins, while the low abundant are detected much less. However, the latter make up the majority of the kinases and regulatory proteins. Even the most advanced modern phosphoproteome techniques may only detect about 10% of all phosphosites [54]. Nonetheless, phosphoproteomic analysis allows much broader coverage of changes in phosphorylation spectrum of many skeletal muscle proteins caused by IR and T2DM both in the basal (fasting) state and in response to insulin.
Basal state. No dramatic differences in basal phosphorylation level (fasting state) of the canonical insulin cascade proteins were found in skeletal muscle between healthy subjects and T2DM patients either by classic immunoblotting [55-64] or by targeted mass-spectrometry [65]. Other studies have demonstrated, by mass-spectrometry, only slight changes of individual phosphorylation sites in the proximal (IRS1) [66] or distal (TBC1D4) [53] parts of the cascade. The absence of marked changes in the insulin cascade at the basal state in T2DM patients is in agreement with studies in rat skeletal muscle after several weeks of high-fat diet that induced IR [33, 67].
On the other hand, a phosphoproteomic study involving 148 subjects with different degrees of metabolic disorders revealed progressive changes brought by IR (IFG or IGT) or T2DM [53]. As evaluated by altered substrate phosphorylation, the kinase activities were mainly decreased outside of insulin signaling. These included kinases of PKC family, casein kinases CK1/2, calcium/calmodulin-dependent kinase type II (CAMK2), cyclin-dependent kinases CDK, myotonic dystrophy protein kinase (DMPK), CDC2-like dual specificity kinase, mitogen-activated kinases (MAP-kinases, MAPK), and others. Also, the changes in phosphorylation of the contractile and structural proteins (myosin heavy chain isoforms, troponin, nebulin, titin, desmin, etc.) were observed. Whereas association of PKC with metabolic dysfunction could be anticipated [16], involvement of casein kinase type I/II (CK1/2) is rather unexpected. CK1/2 phosphorylate hundreds of substrates [54] being involved in many events such as phosphorylation of glycogen synthase and regulation of glycogen metabolism [68]. These human phosphoproteome data [53] are consistent with the results of high-fat diet in rodents [33, 67] that also revealed its effect on phosphorylation of proteins that regulate fat metabolism, inflammation, and protein degradation.
Summing up, the effects of IR and T2DM on basal (fasting) skeletal muscle phosphoproteome remains poorly understood. The available data suggest no marked changes in the basal activity of the canonical insulin cascade in T2DM. This implies that such changes are also absent in IR, and the main differences between healthy individuals and T2DM patients are most likely associated with the response to insulin. Large changes in the T2DM skeletal muscle are also detected in phosphorylation of signaling intermediates that control carbohydrate, lipid, and protein metabolism, as well as the inflammatory responses, all of which are not directly linked to the canonical insulin cascade, at least in its proximal part.
Insulin stimulation. Hyperinsulinemic euglycemic clamp test is commonly used to study molecular responses of human skeletal muscle to insulin. The blood insulin concentration is usually maintained at a relatively high level (~100 µME/ml) for several hours. As expected, a number of studies have found a lower phosphorylation and/or activity response to insulin of the canonical insulin cascade proteins in patients with T2DM as compared to healthy individuals [55-62]. However, no differences were found in other studies [63, 64, 69]. Phosphoproteome analysis by targeted mass-spectrometry revealed relatively minor changes in phosphorylation level of only a few out of two dozen sites in IRS1 after 0.5, 1, or 4 h of clamp test in skeletal muscle samples from T2DM patients as compared to healthy volunteers [65, 66].
Global phosphoproteome analysis of healthy human skeletal muscle after 2-h insulin stimulation during clamp test revealed ~700 phosphosites in more than 400 proteins that altered phosphorylation level. These changes were mostly observed in AKT, MTOR, and MAPK mediated signaling cascades, as well as in various TFs [70]. Considering that these molecules are insulin targets, this result is expected. To the best of our knowledge, there are no studies so far that have compared the effects of insulin on skeletal muscle phosphoproteome in individuals with or without IR or T2DM.
The skeletal muscle phosphoproteome of rats during the period of nocturnal activity, when the animals were actively feeding, was compared to that during the daytime rest [33]. In the animals on high-fat diet an increase in blood insulin after the food intake was more than 2-fold higher than in the control rats, indicative of IR presence. However, phosphorylation of the canonical insulin cascade proteins did not much differ. This suggests that the decrease in insulin sensitivity induced by the high-fat diet was effectively compensated by increased secretion of insulin.
Thus, only a few studies reported individual, not always pronounced and reproducible differences in phosphorylation/activity of the canonical insulin cascade proteins in response to insulin in skeletal muscle from subjects with metabolic disorders. This prompted to analyze the relationship between phosphorylation level of these proteins and insulin concentration. It appeared that, in adipocytes, even a small increase in phosphorylation of the key kinase of the proximal part of the cascade (Akt) was sufficient for full activation of its distal targets (such as Glut4 or transcription factor Foxo1) [41, 42]. It was hypothesized that the proximal part of the cascade in the cell (i.e., insulin receptor, IRS, PI3-kinase, and Akt) is redundant and selectively transmits signals toward the less-abundant targets [27]. This “spareness” hypothesis explains why the impairments associated with IR manifest and should be more pronounced in the distal part of the cascade at the level of GSV translocation, but not in the proximal part, where they are usually looked for, but not found. The exact mechanism of the “distal” disorders is still unknown [27].
In the abovementioned model [33] the increase in endogenous insulin in response to food consumption caused large changes in phosphorylation of more than 2500 phosphosites in skeletal muscle of the control rats and animals on high-fat diet. Despite the different insulin levels in the animals of these two groups, the relative increases in phosphorylation level of Akt, mTOR, or p70S6K1 (all insulin targets) and decrease in that of PKA were similar. The differences were observed only in proteins that regulate glycogen metabolism. Larger differences between the groups were observed after food intake and phosphorylation level altered in more than ~3000 phosphosites. Bioinformatic analysis predicted that the kinase activities of CaMK2, ribosomal p70S6K1 and p90S6K are upregulated in the animals with metabolic disorders, but the activity of casein kinase CK2 is reduced [33]. Since the basal activity of CK2 is also reduced in skeletal muscle of T2DM individuals and activity of CAMK2 is also altered [53], these results imply that CK2 and CAMK2 may contribute to changes in intracellular signaling in skeletal muscle during progression of IR and, possibly, T2DM.
Thus, changes in skeletal muscle phosphoproteome in response to insulin in the patients with IR and T2DM markedly differ from those in healthy individuals. One possible explanation is that insulin can bind to IGF-1 receptors and hybrid IGF-1/insulin receptors under IR conditions [71]. The insulin affinity to these receptors is an order of magnitude lower than the affinity of IGF-1, and normally insulin does not bind and activate them. However, in compensatory hyperinsulinemia typical for IR the insulin levels increase significantly, and the probability of activation of IGF-1 or hybrid receptors increases [72]. The level of IGF-1 also increases in IR, as long as the blood glucose levels remain normal, but normalizes in IFG and further decreases in T2DM, while the content of hybrid receptors in skeletal muscle increases in T2DM and correlates with the body mass index [71]. Despite that all these receptors activate the same proximal elements (PI3-kinase→Akt and Erk MAP-kinases; see Fig. 3), the distal targets may differ, leading to non-identical responses [73]. How big are these differences remains a question, but the scale of IR-associated changes in phosphoproteome suggests they are not solitary and therefore may just contribute.
Summing up, the impaired activation of the canonical insulin cascade by insulin is not always observed in IR and T2DM. This may be due to the majority of such events occurring in the distal part of the cascade, at the level of least abundant regulators of vesicle traffic, or in the non-canonical, or other regulatory pathways of glucose uptake. The effects of IR and T2DM on skeletal muscle phosphoproteome remain largely unexplored. The only study examined responses to exogenous insulin after feeding in the rodent model of high-fat diet. It demonstrated that the skeletal muscle phosphoproteome is altered in IR far beyond the canonical insulin cascade and marked changes are in the activities of CaMK2, ribosomal S6-kinases p70S6K1 and p90S6K, and CK2 [33]. Other targets still require identification and verification at least in different models.
SKELETAL MUSCLE TRANSCRIPTOME CHANGES IN IR AND T2DM
Multiple kinases alter their phosphorylation level in skeletal muscle both in the basal state [33, 53] and in response to insulin [33, 70] in metabolic disorders. These kinases regulate activity of hundreds of proteins including transcription factors. It is logical to assume that metabolic disorders also cause significant changes in gene expression.
Basal state. Changes in basal transcriptome of human skeletal muscle in T2DM were examined in many studies and revealed significant differences as compared to healthy controls. One of the first meta-analyses based on 6 studies showed that more than 100 genes alter expression in T2DM [74]. The most pronounced changes were in decreased expression of the genes encoding enzymes of the Krebs cycle and oxidative phosphorylation, β-oxidation of fatty acids, and regulators of amino acid metabolism. With regard to the genes of oxidative metabolism this is consistent with the results of subsequent large transcriptome studies [75, 76] and further confirmed by proteomic analysis of skeletal muscle from the patients with T2DM [53]. However, another meta-analysis did not find reduced expression of these genes in the patients with IR [77]. It is possible that reduced oxidative capacity of skeletal muscle is not associated only with IR, but also with other factors (age, the level of physical activity, etc.). Impaired expression of genes that regulate the amino acid metabolism in T2DM was confirmed in a number of studies [75-78], as well as the activation of proinflammatory genes and genes of ubiquitylation regulators [75, 76]. This is in agreement with elevated plasma amino acid levels [79] and latent inflammation in adipose tissues in obesity [23, 24, 26]. A lower mRNA expression was found in T2DM for the genes of the canonical insulin cascade [IRS2, PIK3CB, PIK3CA, PIK3R1, SLC2A4 (GLUT4)], receptors of insulin (INSR) and IGF-1 (IGF1R), and of the tyrosine kinase receptor adapter protein (GRB14) [77]. Although the degree of reduction in INSR and IRS2 expression correlated with the severity of metabolic disorders, it was far too small [80].
What factors are responsible for changes in gene expression in IR and T2DM? An unambiguous answer is hardly possible because of complexity of changes in the content of different substrates, metabolites, hormones, and regulatory factors in the blood and in skeletal muscle. Several studies used bioinformatics to predict the transcriptional regulators associated with genes that altered their expression in metabolic disorders [78, 80]. However, these studies aimed at the regulators of genes coding for insulin cascade proteins, whereas other regulators associated with larger changes in transcriptome were not tackled.
Insulin stimulation. Changes in insulin-dependent skeletal muscle transcriptome in metabolic disorders have been explored only in a few studies. Therefore, first we consider the effects of insulin in the cells and skeletal muscle of healthy humans.
In primary human myotubes, the transcriptome dynamics (0.5, 1, 2, 4, 8, and 24 h) was assessed in one of the early studies with an excess insulin concentration (1 µM) [81]. Very prompt response was observed (mostly an increase) in gene expression of the early response TFs (FOS, SRF, EGR1/2, JUNB, IER3, ATF3, and ID1), proinflammatory cytokines, and angiogenesis regulators. Later, the expression of genes for growth factors and metabolic enzymes also increased, and by 24 h the changes were virtually absent. The results of this study should be interpreted with caution because of the very high insulin level, which was maintained throughout the experiment, whereas the physiological insulin concentrations do not exceed 1 nM and last for short periods [22]. Nonetheless, similar to various stress stimuli in other cell cultures [82], insulin rapidly activates the early response TF genes in myotubes.
In human skeletal muscle with normal insulin sensitivity, the transcriptome changes were examined at only two time points after insulin stimulation during clamp test. While after 30 min of stimulation no changes in gene expression were observed [83], in 3-4 h the expression of hundreds of gene changed [83-85]. As in the myotube study cited above [81], insulin induced gene expression of proinflammatory cytokines (IL17D, CCL2, CCL8, CXCL2), their receptors (IL1R1, IL13R), a growth factor (TGFB2), and also of several dozen TF genes. Among the latter again were the early response TFs (EGR1/3, IER2), AP-1 family factors (JUNB, FOS, FOSB), regulators of glycolysis and oxidative phosphorylation (NR4A1 and NR4A3), fat metabolism (SREBF1), transcription initiation factors (TBPL1, BTF3), and others [83-85]. Decreased expression was found for myogenic factors (MEF2B, MYF6), a key regulator of fat metabolism (PPARG), hepatocyte nuclear factors (HNF1/2), and thyroid hormone receptor (THRA) [85]. The large-scale change in TF gene expression suggests that expression of many gene targets should also change during recovery after insulin stimulation. The key effects of insulin in human skeletal muscle (activation of glucose uptake, glycogen synthesis, and MTOR-dependent protein synthesis) are mediated by post-translational regulation. Apparently, insulin can also affect these events at the transcription level, for example, by upregulating expression of hexokinase-2 (HK2) and ribosomal protein genes, as well as a number of factors that control translation [84, 85].
In skeletal muscle of individuals with metabolic disorders, the direction of changes in gene expression in response to insulin stimulation during clamp test was similar to the healthy controls [86, 87]. Bioinformatic analysis linked these changes to interleukins, PPAR, and retinoid receptors [86]. In the single study that compared responses to insulin in metabolic disorders the expression of less genes altered after 5 h of clamp test in patients with IR than in healthy controls [87]. In particular, in IR patients insulin did not affect gene expression of the key enzymes of carbohydrate catabolism [pyruvate dehydrogenase kinase 4, hexokinase-2 (HK2), and others]. At the same time, insulin caused more pronounced gene activation of those TFs in IR patients that regulate fat metabolism (CEBPA and SREBF1).
Summing up, insulin stimulation induces massive changes in skeletal muscle transcriptome including increased gene expression of various TFs, cytokines, regulators of protein synthesis, carbohydrate and fat metabolism. However, their dynamics and signaling pathways that control these changes remain understudied, as well as the insulin-induced changes in transcriptome during development of metabolic disorders.
CONCLUSIONS AND PERSPECTIVES
The development of IR and T2DM is closely associated with reduced insulin-stimulated glucose uptake by skeletal muscles, however, molecular mechanisms of this disorder remain poorly understood. Changes in activation and phosphorylation level of signaling proteins of the proximal part of the canonical insulin cascade (from insulin receptor to AKT, Fig. 3) are not always detected in T2DM. Hypotheses are discussed that explain the decrease in insulin-stimulated glucose uptake by the defects in the distal part of the cascade or in the non-canonical insulin signalling at the level of regulation of GSV traffic and fusion with plasma membrane [27]. The rapid development of the methods of quantitative shotgun phosphoproteomics significantly expanded the understanding of signaling responses to insulin. It became clear that activation of many kinases and TFs is far beyond the framework of the canonical insulin cascade. Insufficient capability of detecting proteins of low abundance, which often play a key role in intracellular signal transduction, remains the major limitation of the shotgun phosphoproteome analysis [54]. Improvement of the hardware and sample preparation techniques should be helpful to increase the depth of phosphoproteome analysis and expand the list of insulin signaling targets. These proteins are of fundamental interest because of their potential as new therapeutic targets.
Changes in skeletal muscle transcriptome in the patients with IR and T2DM have been fairly well characterized in the basal state. They are likely due to a number of factors including the circulating in the blood and located in muscle tissues, also closely linked to physical inactivity. However, the signaling mechanisms and TFs responsible for these changes in muscle cells are almost unexplored. Gene expression responses to acute insulin stimulation are impaired in T2DM. These changes are still poorly characterized, as well as the mechanisms they are controlled by.
The increase of endogenous insulin caused by the food intake is significantly higher in IR than in healthy humans [22] or animals [33]. At the same time, the blood levels of glucose and free fatty acids are the same in IR versus healthy individuals [22], whereas in control animals and animals on a high-fat diet the detected differences in the proximal part of the canonical insulin cascade are minimal, if any [33]. This implies that the ability of signaling system to respond to insulin is maintained at the molecular level by a compensatory increase in insulin levels. The increased insulin secretion may be due to more food consumed by the overweight people. This means that in order to understand the molecular differences in insulin signaling it is important to study responses to normalized food intake thereby modeling the real-life scenario. There have been no such studies yet.
Metabolic disorders cause complex changes in skeletal muscle including the activation of signaling proteins and TFs, mRNA expression, the content of their protein products and various metabolites. They occur both in the basal state and in response to insulin stimulation. However, there is no clear understanding of the relationship between insulin-induced changes that occur at different levels of regulation in cells. For this purpose, a “trans-omics” approach has been recently proposed, which uses a combination of the phosphoproteomic, proteomic, transcriptomic, and metabolomic techniques with bioinformatic analysis. The advantage of the trans-omics approach is its potential to reconstruct molecular networks consisting of interconnected cascades, rather than individual signaling cascades. Such an approach has already allowed identifying molecular networks in rat hepatoma cells that are activated by pico- and nanomolar insulin concentrations typical for the basal state and response to a food intake, respectively [88]. It appeared that at low concentrations insulin mainly affects phosphorylation of translation factors, Akt and p38 MAPK thereby changing activity of TFs (Foxo1, Creb1, and others). These TFs regulate, in different directions, expression of mRNA of glycolytic enzymes, regulators of lipid and amino acid metabolism, thus altering levels of the respective metabolites. In contrast, at high concentrations insulin stimulates mainly Akt and Erk1/2 MAPK that in turn activate the early response TFs (Egr1, Hes1, and others) and increase expression of their target genes including a number of other TFs. Similar approach has been recently used experimentally to reconstruct the molecular networks (signaling proteins →TFs → target genes → metabolism regulators → metabolites) responsible for insulin-stimulated growth of embryonic Drosophila melanogaster S2R+ cells [89]. In another study the dynamics of phosphoproteome, transcriptome, and proteomes was simultaneously studied [90]. The molecular networks that regulate the levels of various metabolites in mouse liver over 6 h after insulin injection were reconstructed. This allowed to comprehend that the fast responses (changes of carbohydrate and fat metabolism) are regulated at the level of phosphorylation of signaling proteins, while the later responses (metabolism of amino acids and nucleotides) are additionally controlled by the expression of specific regulators. The changes in the content of these regulators are mainly due to the changes in their translation, but not at the mRNA level.
Regulation of carbohydrate and fat metabolism in animals and humans is different, therefore, the use of trans-omics analysis to study the mechanisms of IR in humans seems very promising. Considering the key role of skeletal muscle in the development of metabolic disorders, the efforts should be made to join the omics techniques in order to explore the molecular basis of IR and T2DM development in human skeletal muscle.
Abbreviations
- Akt (AKT for human protein):
-
kinase encoded by the retroviral oncogene from the AKT-8 cell line isolated from stock A strain k of the AKR mouse thymoma
- AMPK:
-
AMP-activated protein kinase
- CaMK2 (CAMK2 for human protein):
-
calcium/calmodulin-dependent type II kinase
- CK1/2:
-
casein kinases type I/II
- Glut4 (GLUT4 for human protein):
-
type 4 glucose transporter
- GSV:
-
GLUT4 storage vesicles
- IFG:
-
impaired fasting glucose
- IGF-1:
-
insulin-like growth factor-1
- IGT:
-
impaired glucose tolerance
- IR:
-
insulin resistance
- IRS:
-
insulin receptor substrate
- mTOR (MTOR for human protein):
-
mechanistic target of rapamycin
- T2DM:
-
type 2 diabetes mellitus
- TBC1D1 and TBC1D4 (AS160):
-
proteins containing TBC-domain
- TF:
-
transcription factors
References
Di Pino, A., and DeFronzo, R. A. (2019) Insulin resistance and atherosclerosis: implications for insulin-sensitizing agents, Endocr. Rev., 40, 1447-1467, https://doi.org/10.1210/er.2018-00141.
Nencioni, A., Caffa, I., Cortellino, S., and Longo, V. D. (2018) Fasting and cancer: molecular mechanisms and clinical application, Nat. Rev. Cancer, 18, 707-719, https://doi.org/10.1038/s41568-018-0061-0.
DeFronzo, R. A., Gunnarsson, R., Bjorkman, O., Olsson, M., and Wahren, J. (1985) Effects of insulin on peripheral and splanchnic glucose metabolism in noninsulin-dependent (type II) diabetes mellitus, J. Clin. Invest., 76, 149-155, https://doi.org/10.1172/JCI111938.
Deer, J., Koska, J., Ozias, M., and Reaven, P. (2015) Dietary models of insulin resistance, Metabolism, 64, 163-171, https://doi.org/10.1016/j.metabol.2014.08.013.
Nandi, A., Kitamura, Y., Kahn, C. R., and Accili, D. (2004) Mouse models of insulin resistance, Physiol. Rev., 84, 623-647, https://doi.org/10.1152/physrev.00032.2003.
Kowalski, G. M., and Bruce, C. R. (2014) The regulation of glucose metabolism: implications and considerations for the assessment of glucose homeostasis in rodents, Am. J. Physiol. Endocrinol. Metab., 307, E859-871, https://doi.org/10.1152/ajpendo.00165.2014.
Humphrey, S. J., Yang, G., Yang, P., Fazakerley, D. J., Stockli, J., et al. (2013) Dynamic adipocyte phosphoproteome reveals that Akt directly regulates mTORC2, Cell Metab., 17, 1009-1020, https://doi.org/10.1016/j.cmet.2013.04.010.
Ohno, S., Quek, L. E., Krycer, J. R., Yugi, K., Hirayama, A., et al. (2020) Kinetic trans-omic analysis reveals key regulatory mechanisms for insulin-regulated glucose metabolism in adipocytes, iScience, 23, 101479, https://doi.org/10.1016/j.isci.2020.101479.
Krako Jakovljevic, N., Pavlovic, K., Zujovic, T., Kravic-Stevovic, T., Jotic, A., et al. (2021) In vitro models of insulin resistance: Mitochondrial coupling is differently affected in liver and muscle cells, Mitochondrion, 61, 165-173, https://doi.org/10.1016/j.mito.2021.10.001.
Li, Z., Lai, Z. W., Christiano, R., Gazos-Lopes, F., Walther, T. C., et al. (2018) Global analyses of selective insulin resistance in hepatocytes caused by palmitate lipotoxicity, Mol. Cell. Proteomics, 17, 836-849, https://doi.org/10.1074/mcp.RA117.000560.
Samsonov, M. V., Podkuychenko, N. V., Khapchaev, A. Y., Efremov, E. E., Yanushevskaya, E. V., et al. (2021) AICAR protects vascular endothelial cells from oxidative injury induced by the long-term palmitate excess, Int. J. Mol. Sci., 23, 211, https://doi.org/10.3390/ijms23010211.
Batista, T. M., Jayavelu, A. K., Wewer Albrechtsen, N. J., Iovino, S., Lebastchi, J., et al. (2020) A cell-autonomous signature of dysregulated protein phosphorylation underlies muscle insulin resistance in type 2 diabetes, Cell Metab., 32, 844-859.e845, https://doi.org/10.1016/j.cmet.2020.08.007.
Haider, N., Lebastchi, J., Jayavelu, A. K., Batista, T. M., Pan, H., et al. (2021) Signaling defects associated with insulin resistance in nondiabetic and diabetic individuals and modification by sex, J. Clin. Invest., 131, e151818, https://doi.org/10.1172/JCI151818.
Gaster, M. (2019) The diabetic phenotype is preserved in myotubes established from type 2 diabetic subjects: a critical appraisal, APMIS, 127, 3-26, https://doi.org/10.1111/apm.12908.
Varemo, L., Henriksen, T. I., Scheele, C., Broholm, C., Pedersen, M., et al. (2017) Type 2 diabetes and obesity induce similar transcriptional reprogramming in human myocytes, Genome Med., 9, 47, https://doi.org/10.1186/s13073-017-0432-2.
Petersen, M. C., and Shulman, G. I. (2018) Mechanisms of insulin action and insulin resistance, Physiol. Rev., 98, 2133-2223, https://doi.org/10.1152/physrev.00063.2017.
White, M. F., and Kahn, C. R. (2021) Insulin action at a molecular level – 100 years of progress, Mol. Metab., 52, 101304, https://doi.org/10.1016/j.molmet.2021.101304.
American Diabetes Association Professional Practice (2022) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022, Diabetes Care, 45, S17-S38, https://doi.org/10.2337/dc22-S002.
Liu, Y., Li, J., Wu, Y., Zhang, H., Lv, Q., et al. (2022) Evidence from a systematic review and meta-analysis: Classical impaired glucose tolerance should be divided into subgroups of isolated impaired glucose tolerance and impaired glucose tolerance combined with impaired fasting glucose, according to the risk of progression to diabetes, Front. Endocrinol. (Lausanne), 13, 835460, https://doi.org/10.3389/fendo.2022.835460.
Wang, Q., Jokelainen, J., Auvinen, J., Puukka, K., Keinanen-Kiukaanniemi, S., et al. (2019) Insulin resistance and systemic metabolic changes in oral glucose tolerance test in 5340 individuals: an interventional study, BMC Med., 17, 217, https://doi.org/10.1186/s12916-019-1440-4.
Frayn, K. N. (2019) Turning over our fat stores: the key to metabolic health Blaxter Award Lecture 2018, Proc. Nutr. Soc., 78, 398-406, https://doi.org/10.1017/S0029665118002598.
McQuaid, S. E., Hodson, L., Neville, M. J., Dennis, A. L., Cheeseman, J., et al. (2011) Downregulation of adipose tissue fatty acid trafficking in obesity: a driver for ectopic fat deposition? Diabetes, 60, 47-55, https://doi.org/10.2337/db10-0867.
Vorotnikov, A. V., Stafeev, I. S., Menshikov, M. Y., Shestakova, M. V., and Parfyonova, Y. V. (2019) Latent inflammation and defect in adipocyte renewal as a mechanism of obesity-associated insulin resistance, Biochemistry (Moscow), 84, 1329-1345, https://doi.org/10.1134/S0006297919110099.
Stafeev, I. S., Vorotnikov, A. V., Ratner, E. I., Menshikov, M. Y., and Parfyonova, Y. V. (2017) Latent inflammation and insulin resistance in adipose tissue, Int. J. Endocrinol., 2017, 5076732, https://doi.org/10.1155/2017/5076732.
Samuel, V. T., and Shulman, G. I. (2016) The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux, J. Clin. Invest., 126, 12-22, https://doi.org/10.1172/JCI77812.
Sakers, A., De Siqueira, M. K., Seale, P., and Villanueva, C. J. (2022) Adipose-tissue plasticity in health and disease, Cell, 185, 419-446, https://doi.org/10.1016/j.cell.2021.12.016.
James, D. E., Stockli, J., and Birnbaum, M. J. (2021) The aetiology and molecular landscape of insulin resistance, Nat. Rev. Mol. Cell Biol., 22, 751-771, https://doi.org/10.1038/s41580-021-00390-6.
Sylow, L., Kleinert, M., Richter, E. A., and Jensen, T. E. (2017) Exercise-stimulated glucose uptake - regulation and implications for glycaemic control, Nat. Rev. Endocrinol., 13, 133-148, https://doi.org/10.1038/nrendo.2016.162.
DeFronzo, R. A., Tobin, J. D., and Andres, R. (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance, Am. J. Physiol., 237, E214-E223, https://doi.org/10.1152/ajpendo.1979.237.3.E214.
Kolterman, O. G., Insel, J., Saekow, M., and Olefsky, J. M. (1980) Mechanisms of insulin resistance in human obesity: evidence for receptor and postreceptor defects, J. Clin. Invest., 65, 1272-1284, https://doi.org/10.1172/JCI109790.
Humphrey, S. J., Azimifar, S. B., and Mann, M. (2015) High-throughput phosphoproteomics reveals in vivo insulin signaling dynamics, Nat. Biotechnol., 33, 990-995, https://doi.org/10.1038/nbt.3327.
Minard, A. Y., Tan, S. X., Yang, P., Fazakerley, D. J., Domanova, W., et al. (2016) mTORC1 is a major regulatory node in the FGF21 signaling network in adipocytes, Cell Rep., 17, 29-36, https://doi.org/10.1016/j.celrep.2016.08.086.
Small, L., Brandon, A. E., Parker, B. L., Deshpande, V., Samsudeen, A. F., et al. (2019) Reduced insulin action in muscle of high fat diet rats over the diurnal cycle is not associated with defective insulin signaling, Mol. Metab., 25, 107-118, https://doi.org/10.1016/j.molmet.2019.04.006.
Samuel, V. T., Petersen, K. F., and Shulman, G. I. (2010) Lipid-induced insulin resistance: unravelling the mechanism, Lancet, 375, 2267-2277, https://doi.org/10.1016/S0140-6736(10)60408-4.
Klip, A., McGraw, T. E., and James, D. E. (2019) Thirty sweet years of GLUT4, J. Biol. Chem., 294, 11369-11381, https://doi.org/10.1074/jbc.REV119.008351.
Deshmukh, A. S. (2016) Insulin-stimulated glucose uptake in healthy and insulin-resistant skeletal muscle, Horm. Mol. Biol. Clin. Invest., 26, 13-24, https://doi.org/10.1515/hmbci-2015-0041.
Bogan, J. S. (2012) Regulation of glucose transporter translocation in health and diabetes, Annu. Rev. Biochem., 81, 507-532, https://doi.org/10.1146/annurev-biochem-060109-094246.
Jaldin-Fincati, J. R., Pavarotti, M., Frendo-Cumbo, S., Bilan, P. J., and Klip, A. (2017) Update on GLUT4 vesicle traffic: A cornerstone of insulin action, Trends Endocrinol. Metab., 28, 597-611, https://doi.org/10.1016/j.tem.2017.05.002.
Leney, S. E., and Tavare, J. M. (2009) The molecular basis of insulin-stimulated glucose uptake: signalling, trafficking and potential drug targets, J. Endocrinol., 203, 1-18, https://doi.org/10.1677/JOE-09-0037.
Stockli, J., Fazakerley, D. J., and James, D. E. (2011) GLUT4 exocytosis, J. Cell Sci., 124, 4147-4159, https://doi.org/10.1242/jcs.097063.
Ng, Y., Ramm, G., Burchfield, J. G., Coster, A. C., Stockli, J., et al. (2010) Cluster analysis of insulin action in adipocytes reveals a key role for Akt at the plasma membrane, J. Biol. Chem., 285, 2245-2257, https://doi.org/10.1074/jbc.M109.060236.
Tan, S. X., Ng, Y., Meoli, C. C., Kumar, A., Khoo, P. S., et al. (2012) Amplification and demultiplexing in insulin-regulated Akt protein kinase pathway in adipocytes, J. Biol. Chem., 287, 6128-6138, https://doi.org/10.1074/jbc.M111.318238.
Dummler, B., and Hemmings, B. A. (2007) Physiological roles of PKB/Akt isoforms in development and disease, Biochem. Soc. Trans., 35, 231-235, https://doi.org/10.1042/BST0350231.
Hayashi, T., Hirshman, M. F., Kurth, E. J., Winder, W. W., and Goodyear, L. J. (1998) Evidence for 5′ AMP-activated protein kinase mediation of the effect of muscle contraction on glucose transport, Diabetes, 47, 1369-1373, https://doi.org/10.2337/diab.47.8.1369.
Lizcano, J. M., Goransson, O., Toth, R., Deak, M., Morrice, N. A., et al. (2004) LKB1 is a master kinase that activates 13 kinases of the AMPK subfamily, including MARK/PAR-1, EMBO J., 23, 833-843, https://doi.org/10.1038/sj.emboj.7600110.
Inazuka, F., Sugiyama, N., Tomita, M., Abe, T., Shioi, G., et al. (2012) Muscle-specific knock-out of NUAK family SNF1-like kinase 1 (NUAK1) prevents high fat diet-induced glucose intolerance, J. Biol. Chem., 287, 16379-16389, https://doi.org/10.1074/jbc.M111.302687.
Koh, H. J., Toyoda, T., Fujii, N., Jung, M. M., Rathod, A., et al. (2010) Sucrose nonfermenting AMPK-related kinase (SNARK) mediates contraction-stimulated glucose transport in mouse skeletal muscle, Proc. Natl. Acad. Sci. USA, 107, 15541-15546, https://doi.org/10.1073/pnas.1008131107.
O’Neill, B. T., Lauritzen, H. P., Hirshman, M. F., Smyth, G., Goodyear, L. J., et al. (2015) Differential role of insulin/IGF-1 receptor signaling in muscle growth and glucose homeostasis, Cell Rep., 11, 1220-1235, https://doi.org/10.1016/j.celrep.2015.04.037.
Jaiswal, N., Gavin, M. G., Quinn, W. J., III, Luongo, T. S., Gelfer, R. G., et al. (2019) The role of skeletal muscle Akt in the regulation of muscle mass and glucose homeostasis, Mol. Metab., 28, 1-13, https://doi.org/10.1016/j.molmet.2019.08.001.
Gauthier, M. S., O’Brien, E. L., Bigornia, S., Mott, M., Cacicedo, J. M., et al. (2011) Decreased AMP-activated protein kinase activity is associated with increased inflammation in visceral adipose tissue and with whole-body insulin resistance in morbidly obese humans, Biochem. Biophys. Res. Commun., 404, 382-387, https://doi.org/10.1016/j.bbrc.2010.11.127.
Xu, X. J., Gauthier, M. S., Hess, D. T., Apovian, C. M., Cacicedo, J. M., et al. (2012) Insulin sensitive and resistant obesity in humans: AMPK activity, oxidative stress, and depot-specific changes in gene expression in adipose tissue, J. Lipid Res., 53, 792-801, https://doi.org/10.1194/jlr.P022905.
Wang, D., Eraslan, B., Wieland, T., Hallstrom, B., Hopf, T., et al. (2019) A deep proteome and transcriptome abundance atlas of 29 healthy human tissues, Mol. Syst. Biol., 15, e8503, https://doi.org/10.15252/msb.20188503.
Ohman, T., Teppo, J., Datta, N., Makinen, S., Varjosalo, M., et al. (2021) Skeletal muscle proteomes reveal downregulation of mitochondrial proteins in transition from prediabetes into type 2 diabetes, iScience, 24, 102712, https://doi.org/10.1016/j.isci.2021.102712.
Needham, E. J., Parker, B. L., Burykin, T., James, D. E., and Humphrey, S. J. (2019) Illuminating the dark phosphoproteome, Sci. Signal., 12, https://doi.org/10.1126/scisignal.aau8645.
Krook, A., Roth, R. A., Jiang, X. J., Zierath, J. R., and Wallberg-Henriksson, H. (1998) Insulin-stimulated Akt kinase activity is reduced in skeletal muscle from NIDDM subjects, Diabetes, 47, 1281-1286, https://doi.org/10.2337/diab.47.8.1281.
Tonks, K. T., Ng, Y., Miller, S., Coster, A. C., Samocha-Bonet, D., et al. (2013) Impaired Akt phosphorylation in insulin-resistant human muscle is accompanied by selective and heterogeneous downstream defects, Diabetologia, 56, 875-885, https://doi.org/10.1007/s00125-012-2811-y.
Albers, P. H., Pedersen, A. J., Birk, J. B., Kristensen, D. E., Vind, B. F., et al. (2015) Human muscle fiber type-specific insulin signaling: impact of obesity and type 2 diabetes, Diabetes, 64, 485-497, https://doi.org/10.2337/db14-0590.
Vind, B. F., Birk, J. B., Vienberg, S. G., Andersen, B., Beck-Nielsen, H., et al. (2012) Hyperglycaemia normalises insulin action on glucose metabolism but not the impaired activation of AKT and glycogen synthase in the skeletal muscle of patients with type 2 diabetes, Diabetologia, 55, 1435-1445, https://doi.org/10.1007/s00125-012-2482-8.
Kim, Y. B., Kotani, K., Ciaraldi, T. P., Henry, R. R., and Kahn, B. B. (2003) Insulin-stimulated protein kinase C lambda/zeta activity is reduced in skeletal muscle of humans with obesity and type 2 diabetes: reversal with weight reduction, Diabetes, 52, 1935-1942, https://doi.org/10.2337/diabetes.52.8.1935.
Kim, Y. B., Nikoulina, S. E., Ciaraldi, T. P., Henry, R. R., and Kahn, B. B. (1999) Normal insulin-dependent activation of Akt/protein kinase B, with diminished activation of phosphoinositide 3-kinase, in muscle in type 2 diabetes, J. Clin. Invest., 104, 733-741, https://doi.org/10.1172/JCI6928.
Bandyopadhyay, G. K., Yu, J. G., Ofrecio, J., and Olefsky, J. M. (2005) Increased p85/55/50 expression and decreased phosphotidylinositol 3-kinase activity in insulin-resistant human skeletal muscle, Diabetes, 54, 2351-2359, https://doi.org/10.2337/diabetes.54.8.2351.
Karlsson, H. K., Zierath, J. R., Kane, S., Krook, A., Lienhard, G. E., et al. (2005) Insulin-stimulated phosphorylation of the Akt substrate AS160 is impaired in skeletal muscle of type 2 diabetic subjects, Diabetes, 54, 1692-1697, https://doi.org/10.2337/diabetes.54.6.1692.
Hojlund, K., Staehr, P., Hansen, B. F., Green, K. A., Hardie, D. G., et al. (2003) Increased phosphorylation of skeletal muscle glycogen synthase at NH2-terminal sites during physiological hyperinsulinemia in type 2 diabetes, Diabetes, 52, 1393-1402, https://doi.org/10.2337/diabetes.52.6.1393.
Beeson, M., Sajan, M. P., Dizon, M., Grebenev, D., Gomez-Daspet, J., et al. (2003) Activation of protein kinase C-zeta by insulin and phosphatidylinositol-3,4,5-(PO4)3 is defective in muscle in type 2 diabetes and impaired glucose tolerance: amelioration by rosiglitazone and exercise, Diabetes, 52, 1926-1934, https://doi.org/10.2337/diabetes.52.8.1926.
Karlsson, H. K. R., Kasahara, A., Ikeda, M., Chibalin, A. V., Harada, J., et al. (2021) Quantitative phosphoproteomic analysis of IRS1 in skeletal muscle from men with normal glucose tolerance or type 2 diabetes: A case-control study, Metabolism, 118, 154726, https://doi.org/10.1016/j.metabol.2021.154726.
Langlais, P., Yi, Z., Finlayson, J., Luo, M., Mapes, R., De Filippis, E., et al. (2011) Global IRS-1 phosphorylation analysis in insulin resistance, Diabetologia, 54, 2878-2889, https://doi.org/10.1007/s00125-011-2271-9.
Sun, Y. N., Huang, J. Q., Chen, Z. Z., Du, M., Ren, F. Z., et al. (2020) Amyotrophy induced by a high-fat diet is closely related to inflammation and protein degradation determined by quantitative phosphoproteomic analysis in skeletal muscle of C57BL/6 J mice, J. Nutr., 150, 294-302, https://doi.org/10.1093/jn/nxz236.
Roach, P. J., Depaoli-Roach, A. A., Hurley, T. D., and Tagliabracci, V. S. (2012) Glycogen and its metabolism: some new developments and old themes, Biochem. J., 441, 763-787, https://doi.org/10.1042/BJ20111416.
Meyer, M. M., Levin, K., Grimmsmann, T., Beck-Nielsen, H., and Klein, H. H. (2002) Insulin signalling in skeletal muscle of subjects with or without Type II-diabetes and first degree relatives of patients with the disease, Diabetologia, 45, 813-822, https://doi.org/10.1007/s00125-002-0830-9.
Needham, E. J., Hingst, J. R., Parker, B. L., Morrison, K. R., Yang, G., et al. (2022) Personalized phosphoproteomics identifies functional signaling, Nat. Biotechnol., 40, 576-584, https://doi.org/10.1038/s41587-021-01099-9.
Haywood, N. J., Slater, T. A., Matthews, C. J., and Wheatcroft, S. B. (2019) The insulin like growth factor and binding protein family: Novel therapeutic targets in obesity & diabetes, Mol. Metab., 19, 86-96, https://doi.org/10.1016/j.molmet.2018.10.008.
Belfiore, A., Frasca, F., Pandini, G., Sciacca, L., and Vigneri, R. (2009) Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease, Endocr. Rev., 30, 586-623, https://doi.org/10.1210/er.2008-0047.
Hakuno, F., and Takahashi, S. I. (2018) IGF1 receptor signaling pathways, J. Mol. Endocrinol., 61, T69-T86, https://doi.org/10.1530/JME-17-0311.
Varemo, L., Scheele, C., Broholm, C., Mardinoglu, A., Kampf, C., et al. (2015) Proteome- and transcriptome-driven reconstruction of the human myocyte metabolic network and its use for identification of markers for diabetes, Cell Rep., 11, 921-933, https://doi.org/10.1016/j.celrep.2015.04.010.
Scott, L. J., Erdos, M. R., Huyghe, J. R., Welch, R. P., Beck, A. T., et al. (2016) The genetic regulatory signature of type 2 diabetes in human skeletal muscle, Nat. Commun., 7, 11764, https://doi.org/10.1038/ncomms11764.
Wu, C., Xu, G., Tsai, S. A., Freed, W. J., and Lee, C. T. (2017) Transcriptional profiles of type 2 diabetes in human skeletal muscle reveal insulin resistance, metabolic defects, apoptosis, and molecular signatures of immune activation in response to infections, Biochem. Biophys. Res. Commun., 482, 282-288, https://doi.org/10.1016/j.bbrc.2016.11.055.
Timmons, J. A., Atherton, P. J., Larsson, O., Sood, S., Blokhin, I. O., et al. (2018) A coding and non-coding transcriptomic perspective on the genomics of human metabolic disease, Nucleic Acids Res., 46, 7772-7792, https://doi.org/10.1093/nar/gky570.
Chaudhuri, R., Khoo, P. S., Tonks, K., Junutula, J. R., Kolumam, G., et al. (2015) Cross-species gene expression analysis identifies a novel set of genes implicated in human insulin sensitivity, NPJ Syst. Biol. Appl., 1, 15010, https://doi.org/10.1038/npjsba.2015.10.
Caballero, B., Finer, N., and Wurtman, R. J. (1988) Plasma amino acids and insulin levels in obesity: response to carbohydrate intake and tryptophan supplements, Metabolism, 37, 672-676, https://doi.org/10.1016/0026-0495(88)90089-3.
Cen, H. H., Hussein, B., Botezelli, J. D., Wang, S., Zhang, J. A., et al. (2022) Human and mouse muscle transcriptomic analyses identify insulin receptor mRNA downregulation in hyperinsulinemia-associated insulin resistance, FASEB J., 36, e22088, https://doi.org/10.1096/fj.202100497RR.
Hansen, L., Gaster, M., Oakeley, E. J., Brusgaard, K., Damsgaard Nielsen, E. M., et al. (2004) Expression profiling of insulin action in human myotubes: induction of inflammatory and pro-angiogenic pathways in relationship with glycogen synthesis and type 2 diabetes, Biochem. Biophys. Res. Commun., 323, 685-695, https://doi.org/10.1016/j.bbrc.2004.08.146.
Arner, E., Daub, C. O., Vitting-Seerup, K., Andersson, R., Lilje, B., et al. (2015) Transcribed enhancers lead waves of coordinated transcription in transitioning mammalian cells, Science, 347, 1010-1014, https://doi.org/10.1126/science.1259418.
Coletta, D. K., Balas, B., Chavez, A. O., Baig, M., Abdul-Ghani, M., et al. (2008) Effect of acute physiological hyperinsulinemia on gene expression in human skeletal muscle in vivo, Am. J. Physiol. Endocrinol. Metab., 294, E910-E917, https://doi.org/10.1152/ajpendo.00607.2007.
Rome, S., Clement, K., Rabasa-Lhoret, R., Loizon, E., Poitou, C., et al. (2003) Microarray profiling of human skeletal muscle reveals that insulin regulates approximately 800 genes during a hyperinsulinemic clamp, J. Biol. Chem., 278, 18063-18068, https://doi.org/10.1074/jbc.M300293200.
Wu, X., Wang, J., Cui, X., Maianu, L., Rhees, B., et al. (2007) The effect of insulin on expression of genes and biochemical pathways in human skeletal muscle, Endocrine, 31, 5-17, https://doi.org/10.1007/s12020-007-0007-x.
Rudkowska, I., Jacques, H., Weisnagel, S. J., Marette, A., and Vohl, M. C. (2013) Transcriptomic profiles of skeletal muscle tissue following an euglycemic-hyperinsulinemic clamp in insulin-resistant obese subjects, Genes Nutr., 8, 91-98, https://doi.org/10.1007/s12263-012-0298-2.
Sears, D. D., Hsiao, G., Hsiao, A., Yu, J. G., Courtney, C. H., Ofrecio, J. M., et al. (2009) Mechanisms of human insulin resistance and thiazolidinedione-mediated insulin sensitization, Proc. Natl. Acad. Sci. USA, 106, 18745-18750, https://doi.org/10.1073/pnas.0903032106.
Kawata, K., Hatano, A., Yugi, K., Kubota, H., Sano, T., et al. (2018) Trans-omic analysis reveals selective responses to induced and basal insulin across signaling, transcriptional, and metabolic networks, iScience, 7, 212-229, https://doi.org/10.1016/j.isci.2018.07.022.
Terakawa, A., Hu, Y., Kokaji, T., Yugi, K., Morita, K., et al. (2022) Trans-omics analysis of insulin action reveals a cell growth subnetwork which co-regulates anabolic processes, iScience, 25, 104231, https://doi.org/10.1016/j.isci.2022.104231.
Matsuzaki, F., Uda, S., Yamauchi, Y., Matsumoto, M., Soga, T., et al. (2021) An extensive and dynamic trans-omic network illustrating prominent regulatory mechanisms in response to insulin in the liver, Cell Rep., 36, 109569, https://doi.org/10.1016/j.celrep.2021.109569.
Funding
The study was financially supported by the Russian Science Foundation (project no. 21-75-10146).
Author information
Authors and Affiliations
Contributions
D. V. Popov, A. V. Vorotnikov – concept of the review; D. V. Popov, P. A. Makhnovsky, A. V. Vorotnikov – gathering information, discussion of the results of the studies, writing and editing of the review.
Corresponding authors
Ethics declarations
Authors declare no conflict of interest in financial or any other sphere. This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Vorotnikov, A.V., Popov, D.V. & Makhnovskii, P.A. Signaling and Gene Expression in Skeletal Muscles in Type 2 Diabetes: Current Results and OMICS Perspectives. Biochemistry Moscow 87, 1021–1034 (2022). https://doi.org/10.1134/S0006297922090139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0006297922090139