Abstract
As a common chemotherapy drug, methotrexate (MTX) has achieved remarkable clinical success. However, high inter-individual variability and unpredictable toxicity continue to challenge its use in clinical practices. Some studies suggest this variation is associated with a methylenetetrahydrofolate reductase (MTHFR) gene polymorphism, but results remain unclear. In this meta-analysis, we include 14 studies that focus on MTHFR C677T and A1298C polymorphisms in pediatric patients with malignancy. We found significant associations of the MTHFR C677T polymorphism with hepatotoxicity (grade ⩾2; CC vs CT/TT: risk ratio (RR): 0.82, 95% confidence interval (CI): 0.67–0.99; P=0.04), hematological toxicity (grade 3–4; CC vs CT/TT: RR: 0.65, 95% CI: 0.44–0.97; P=0.03) in a dominant genetic model and mucositis (grade ⩾3) in all models (CC vs CT/TT: RR: 0.18, 95% CI: 0.04–0.87; P=0.03; CC/CT vs TT: RR: 0.10, 95% CI: 0.03–0.32; P⩽0.0001; CC vs TT: RR: 0.10, 95% CI: 0.02–0.50; P=0.005). No significant association was found with the MTHFR A1298C polymorphism. For children with malignancy, genotyping of the MTHFR C677T polymorphism is expected to be a useful tool in reducing toxicity and improving outcome in personalized MTX therapy.
Similar content being viewed by others
Introduction
A folate antagonist, methotrexate (MTX) has been widely used for the treatment of a variety of adult and childhood cancers, including acute lymphoblastic leukemia (ALL) and lymphoma, and rheumatoid arthritis.1, 2 Although MTX has achieved remarkable clinical success, highly variable individual responses and unpredictable toxicity continue to challenge its clinical use.3 Intravenous infusion of MTX, especially high-dose MTX followed by leucovorin rescue is associated with several toxic responses in many patients, including myelosuppression, oral mucositis, hepatotoxicity, renal toxicity, and both transient and persistent neurotoxicity. Toxicity can result in the interruption or discontinuation of chemotherapy, thereby increasing relapse risk; it also affects patient quality of life.4 Studies on the key regulators in the MTX pathway seek to find a reliable biomarker to predict risk of MTX toxicities.
In the MTX pathway, the polymorphism of folate regulation genes is involved in the pharmacodynamics of MTX.5 Numerous pharmacogenetic studies have reported that single-nucleotide polymorphisms alter the activity or expression of folate pathway enzymes, which may influence the response and toxicity of MTX in various malignancies and autoimmune diseases.6, 7, 8 Among these key genes, the methylenetetrahydrofolate reductase (MTHFR) gene polymorphism has become a research focus due to its critical role in intracellular folate homeostasis and metabolism. Two well-characterized polymorphisms, MTHFR C677T (rs1801133) and MTHFR A1298C (rs1801131) have been reported in enzyme activity reduction.9 In MTHFR C677T, transition from a C to a T nucleobase encodes proteins with enzymatic activity that is decreased significantly, by about 30–40%, leading to an increased level of homocysteine and an altered distribution of folate.10 In MTHFR A1298C, a milder decrease in MTHFR activity is caused by a transition from an A to a C nucleobase.11
As high-dose MTX is more easily associated with toxic responses and dosage for malignancy is higher than those for rheumatoid arthritis, people with malignant cancer are more easily affected by toxicities than those with rheumatoid arthritis. Besides, in the chemotherapy regimens, MTX dosage for pediatric patients are usually higher than those for adults;12 and in the real clinical practice, the MTX response of children is often different from adults,3 which leads us to paying more attention to pediatric patients with malignant cancers.
So far, there exists three systematic reviews/meta-analyses13, 14, 15 (Table 1) and one umbrella review or systematic review of systematic reviews.16 Obviously, studies included in the three systematic reviews/meta-analyses were published before 2012 and the literature databases searched were limited, besides, Campbell et al.16 just synthesized the findings of all the three systematic reviews without including new studies, which means that the studies published nearly 5 years (2012–2016) and some studies in other databases need to be included and reanalyzed, so as to observe whether the results change.
What is more, only one meta-analysis focused on pediatric patients alone. In that study, Lopez-Lopez et al.14 focused on ALL and found no association between MTHFR C677T or A1298C polymorphisms and individual toxicity. However, five recent cohort studies using a total 601 subjects have found significant associations: one study in non-Hodgkin’s lymphoma (NHL) was conducted by D’Angelo et al.;17 one in osteosarcoma was conducted by Park and Shin;5 and three studies were in pediatric ALL (one in 2014 and two in 2015).18, 19, 20 Further, Hagleitner et al.15 showed that the effect of a germline genetic variant in a metabolizing gene can reasonably be expected to be independent of the type of malignancy present. In light of this information, we performed a meta-analysis in children with a childhood malignancy, including ALL, lymphoma and osteosarcoma, to assess the possible associations between two common MTHFR gene polymorphisms (C677T and A1298C) and MTX-induced toxicities.
Materials and methods
Search strategy
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement.21 Relevant literature published before 1 August 2016 in the Cochrane Library (Appendix 1), PubMed (Appendix 2), EMBASE (Appendix 3) and Web of Science (Appendix 4) were thoroughly searched, independently by two reviewers, for studies exploring the association between MTHFR polymorphisms and MTX-induced toxicities in children with malignancies. Only English language papers were searched, but no restrictions on the study design were imposed. We also hand-searched ClinicalTrials.gov and references of retrieved studies and reviews. The following keywords and subject terms were used: methotrexate; methylenetetrahydrofolate reductase; MTHFR; methotrexate; MTX; pediatric; children.
Study selection
Two reviewers (CZ and YWL) independently screened the literature search results for relevant papers. Studies in this meta-analysis met the following inclusion criteria: evaluation of the association between MTHFR polymorphism and MTX-induced toxicities was done in children with a malignancy; and sufficient data were provided regarding genotype distributions to calculate the risk ratio (RR) and its corresponding 95% confidence interval (CI). When a single group of subjects was involved in multiple studies, we included only one of the studies.
Data extraction
The following data from eligible studies were extracted in duplicate by two investigators (CZ and YWL) working independently: first author’s name, publication year, ethnicity or country of subjects, sample size, disease, age, gender, treatment protocol, MTX dosage, genotype, MTX-induced toxicities, Hardy–Weinberg equilibrium (HWE) values for gene polymorphisms, and toxicity criteria used to define and grade the toxicities noted during chemotherapy. For studies that did not provide graded genotyped toxicity data in their original published paper, the corresponding authors were contacted by e-mail or phone to obtain any available graded genotyped toxicity data. A third investigator (SZW) was consulted to reach a consensus decision where any discrepancy occurred in the data extracted.
Quality assessment
Two independent reviewers (CZ and SZW) applied the Newcastle–Ottawa Quality Assessment Scale to assess the selected studies, including case–control studies and cohort studies. Any disagreements that arose between the reviewers were resolved through discussion. A third reviewer (YWL) was available to settle disputes.
Data synthesis and analysis
Where two or more included studies reported the same toxicities, their results were combined in the meta-analysis if no significant heterogeneity was present. Statistical analysis was conducted using Revman 5.3 (Cochrane IMS) and we estimated the overall pooled RRs and their corresponding 95% CIs using Mantel-Haenszel’s method with random-effects model or fixed-effects model depending on I2 (if I2⩾50%, a random-effects model was used; otherwise, a fixed-effects model was used). I2 value statistical methods and Cochrane Q tests were used to assess heterogeneity across the included studies. A P-value below 0.05 for the Cochrane Q test indicates the presence of statistically significant heterogeneity and an I2 value >50% indicates moderate to extreme heterogeneity. For association evaluation, a Z-test was performed to determine the statistical significance of pooled RRs and a P-value <0.05 was considered to be statistically significant.22 Pooled RRs were used for the dominant model (C677T: CC vs CT/CT; A1298C: AA vs AC/CC), recessive model (C677T: CC/CT vs TT; A1298C: AA/AC vs CC) and homozygote models (C677T: CC vs TT; A1298C: AA vs CC). Meta-analyses for the association between genotype, non-hematological toxicity (hepatotoxicity and mucositis) and hematological toxicity were performed. When I2 was >50%, heterogeneity analysis was performed subsequently by sensitivity analysis and subgroup analysis if data permitted.
Results
Identification and characteristics of the studies
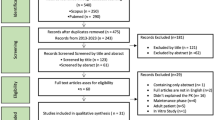
The literature selection process is summarized in Figure 1. A total of 1082 records were identified through our initial search. After removing 520 overlapping records and screening titles and abstracts, 130 records were considered potentially eligible and full texts were retrieved and read thoroughly for further evaluation. Subsequently, 116 studies were excluded: 26 were meeting abstracts with full data unavailable; four were letters; 34 were conducted using mixed age group (both pediatrics and adults); 23 did not provide sufficient toxicity data corresponding to each genotype for MTX-induced toxicity; and 25 expressed data in the form of mean±s.d., which could not be combined with dichotomous variables in this meta-analysis. Four of the remaining studies used the same data, and only the study with largest sample size was included. Thus, a total of 14 studies met the inclusion criteria and were included in our meta-analysis.
Flow diagram of study.
The characteristics of the included studies are summarized in Table 2. In these 14 studies, MTX dose ranged from 1 g m−2 to 12 g m−2. Eight studies examined both MTHFR C677T and A1298C polymorphisms4, 5, 17, 18, 20, 23, 24, 25 and six studies included only MTHFR C677T.19, 26, 27, 28, 29, 30 With regard to ethnicity, the 14 studies were divided into four ethnic groups: Caucasian,17, 18, 19, 20, 24, 25 Asian,4, 5, 27, 28, 29 African23 and mixed population,26, 30 with sample sizes of six, five, one and two studies, respectively. For disease type, there were nine studies of ALL,4, 18, 19, 20, 23, 24, 25, 26, 30 one of non-Hodgkin’s lymphoma,17 one of osteosarcoma5 and three of both ALL and lymphoma.27, 28, 29 MTX-induced toxicity of the included studies is summarized in Table 3; hematological toxicity, hepatotoxicity and mucositis were the dominant MTX-induced toxicities. Among the 14 studies, 50% mentioned that genotype distributions of samples were consistent with HWE.
Quality of studies
All the 14 included studies were cohort studies; the highest quality score was nine stars23, 24 and the lowest was seven stars4, 5, 17, 18, 19, 20, 25, 26, 27, 28, 29 (Table 4). Most of the cohort studies did well in sample selection and comparability, but failed in outcome due to the short or inadequate follow-up.
Association between MTHFR C677T polymorphism and MTX-induced toxicities
All fourteen studies measured the association between the MTHFR C677T polymorphism and MTX-induced toxicities. Detailed data of dominant, recessive and homozygote models regarding different toxicities are summarized in Table 5.
Seven studies (918 subjects in total)4, 5, 20, 23, 27, 29, 30 provided data on hepatotoxicity (grade ⩾2); the combined analysis found a significant association between the MTHFR C677T polymorphism and hepatotoxicity (grade ⩾2) only in the dominant genetic model (CC vs CT/TT: RR: 0.82, 95% CI: 0.67–0.99; P=0.04; Figure 2). A stratified analysis based on ethnicity was conducted to check whether ethnicity influences the association between C677T and risk of grade ⩾2 hepatotoxicity. The results revealed a statistically significant association between C677T and increased risk in the Asian in recessive model (CC/CT vs TT: RR: 0.72, 95% CI: 0.52–0.99; P=0.04) with no significant heterogeneity (Figure 3). While only one African study was included, the results suggest a statistically significant association in the recessive model of this ethnic group (RR: 0.05, 95% CI: 0.01–0.33; P=0.002) and homozygote model (RR: 0.09, 95% CI: 0.01–0.58; P=0.01). A tendency toward increased risk of hepatotoxicity was also present for ALL disease in the dominant model (CC vs CT/TT: RR: 0.81, 95% CI: 0.65–1.00; P=0.05; Figure 4). For hepatotoxicity, grades 1–4,25, 28 no pattern could be detected in the limited available data from the included studies and further stratified analysis based on ethnicity was not possible.
Meta-analysis of association between MTHFR C677T polymorphism and risk of hepatotoxicity (grade ⩾2) in pediatric patients with malignancies in dominant model. CI, confidence interval.
Subgroup analysis of association between MTHFR C677T polymorphism and risk of hepatotoxicity (grade ⩾2) in pediatric patients with malignancies based on ethnicity in recessive model. CI, confidence interval.
Meta-analysis of association between MTHFR C677T polymorphism and risk of hepatotoxicity (grade ⩾2) in pediatric patients with ALL in dominant model. CI, confidence interval.
Seven studies (855 subjects in total)4, 17, 18, 19, 20, 23, 24 were included, which mentioned risk of hematologic toxicity (grade 3–4), showing significant effect in the dominant model (CC vs CT/TT: RR: 0.65, 95% CI: 0.44–0.97; P=0.03; Figure 5). In the other two models, meta-analyses failed because of significant heterogeneity (CC+CT vs TT: I2=83%; CC vs TT: I2=78%). However, two studies, Africans with ALL23 and Caucasians with ALL24 showed a statistically significant association between C677T and hematologic toxicity (grade 3–4; Table 5). For grade 1–4 hematologic toxicity, no significant association was detected.
Meta-analysis of association between MTHFR C677T polymorphism and risk of hematologic toxicity (grade 3–4) in pediatric patients with malignancies in dominant model. CI, confidence interval.
A significant association between C677T and mucositis (grade ⩾3) was present in all genetic models (CC vs CT/TT: RR: 0.18, 95% CI: 0.04–0.87; P=0.03; CC/CT vs TT: RR: 0.10, 95% CI: 0.03–0.32; P⩽0.0001; CC vs TT: RR: 0.10, 95% CI: 0.02–0.50; P=0.005; Figure 6). However, no significant effect was observed in grade 1–4 mucositis toxicity in all genetic models.
Meta-analysis of association between MTHFR C677T polymorphism and risk of mucositis (grade ⩾3) in pediatric patients with malignancies in all three genetic models. CI, confidence interval.
Association between MTHFR A1298C polymorphism and MTX-induced toxicities
Seven studies included the MTHFR A1298C polymorphism, two in Asians,4, 5 one in Africans23 and four in Caucasians.17, 18, 20, 25 In these studies, five were in ALL,4, 18, 20, 23, 25 one was in NHL17 and one was in osteosarcoma.5 The evaluation of associations between the MTHFR A1298C polymorphism and various MTX-induced toxicities in children with malignancy are summarized in Table 5.
Four studies with 381 subjects included analysis of hepatotoxicity (grade ⩾ 2)4, 5, 20, 23 as shown in Table 5. There was no significant association found in any of the three genetic models. Similarly, no significant association was found between the MTHFR A1298C polymorphism and MTX-induced hematological toxicities4, 17, 18, 23, 25 or musositis4, 5, 20, 23, 25 in any of the genetic models. No further stratified analysis based on ethnicity was performed because few studies were available in each comparison. Mild-to-moderate heterogeneity was observed, mainly in the analysis of grade 1–4 mucositis4, 20, 25 and hematological toxicities4, 17, 18, 23, 25 under different genetic models. However, Shu-Guang Liu found a significant association between A1298C and grade 3–4 hematologic toxicity in Asians in all except the dominant genetic model4 (Table 5).
Heterogeneity analysis
Mild-to-moderate between-study heterogeneity was identified during some of the meta-analyses performed for the relationship between MTHFR polymorphisms and MTX toxicity. Therefore, a random-effects model was used and the source of heterogeneity assessed in subgroup analysis according to ethnicity (Table 5). Heterogeneity may also be due to diseases, MTX dose, sample size, HWE and/or the criteria used for toxicity assessment, so that sensitivity analysis was also conducted. One study with relatively small sample25 or no HWE20 or no dose20 was omitted and analyses re-done to test the stability of the final pooled results. Finally, in A1298C, I2 of all models in grade 1–4 mucositis were dramatically decreased to less than 50%; while in C677T, I2 of CC vs CT/TT in grade 3–4 hematologic toxicity was smoothly altered, but still more than 50% (Table 5), which indicated that all the factors above could be the recourses of heterogeneity.
Discussion
As an antifolate chemotherapeutic agent, MTX has been widely used in the treatment of childhood malignancies, such as ALL, lymphoma and osteosarcoma. Although many studies have analyzed MTHFR polymorphisms and their association with MTX-induced toxicities, definitive conclusions cannot be drawn. Considering the different study designs and low power of individual studies on pediatric patients, this meta-analysis was conducted in an attempt to provide a more comprehensive and reliable conclusion on the possible association, with less random errors and more precise estimates.
To the best of our knowledge, this meta-analysis is the first to evaluate the association between MTHFR C677T and A1298C polymorphisms and risk of MTX-induced toxicity in children with malignancy across a range of ethnic backgrounds. After pooling available data from included studies, the meta-analysis demonstrates that MTHFR C677T polymorphism is significantly associated with increased risk of mucositis (grade ⩾3). Moreover, the significant associations between MTHFR C677T polymorphism and increased risk of hepatotoxicity (grade ⩾2) and grade 3–4 hematological toxicity were found in dominant model. A subgroup analysis by ethnicity was conducted in recessive and homozygote models, which revealed a significant association between C677T and hepatotoxicity (grade ⩾2) in African, Asian. The protective effect of the heterozygous CC/CT genotype was more evident in Africans. However, the study number was limited and sample size was small in our meta-analysis; therefore, further studies are needed to verify the association in different ethnicities.
In the chemotherapy regimens for pediatric patients with childhood malignancy, MTX dosages adopted are typically high (higher than 1 g m−2), which is different from adult patients where a low-dose MTX regimen is also common.12 In our meta-analysis, toxicity data related to dosage were limited, so a subgroup analysis by MTX dosage to clarify whether MTX dosage influences the associations was not possible. Although Zhao, et al.3 conducted a meta-analysis in adult patients with hematological malignancies, including six studies with the final sample size of 409, and a subgroup analysis by MTX dosage was conducted to clarify whether MTX dosage may influence the association findings. The result revealed that MTHFR 677T allele increased risk of MTX-induced all-grade (G1–4) and severe (G3–4) hepatic and gastrointestinal toxicity in Caucasian independent of MTX dosage. However, the available data were also insufficient, which means that more new studies are necessary to validate this finding and reach a more robust conclusion. In real clinical practice, the treatment response of children to MTX is often much better than in adults.3 Some studies show that pediatric ALL patients typically have a much higher completion rate than adult ALL patients, and the 5-year event-free survival rate reaches nearly 80% for children but is only 40% for adults.1, 2 Therefore, the association between MTHFR variants and MTX-induced toxicity may be less obvious in children, which is also suggested by our meta-analysis results.
Our meta-analysis found no significant association between MTHFR A1298C polymorphism and hepatotoxicity, hematological toxicity or mucositis, which is in agreement with results reported in previous studies.3, 31, 32, 33, 34 However, a few studies have revealed that the MTHFR A1298C mutation can reduce enzyme activity and leave more substrate for thymidylate synthesis, subsequently resulting in more DNA synthesis and less toxiciy.4 Furthermore, some studies have shown that the A1298C polymorphism has a protective role.13, 22, 35 Overall, the MTHFR A1298C polymorphism does not seem to be a good predictor of MTX toxicity, although it may be a protective factor in children with childhood malignancy.
Besides the MTX-induced toxicity, MTHFR C677T and A1298C polymorphism also affect other aspects in MTX treatment, such as MTX dosage, event-free survival, relapse and mortality. Thus, it can give us information to optimize the protocol and predict the outcome. Salazar et al.36 found that children with a favorable MTHFR genotype treated with MTX doses of 5 g m−2 develop a similar or, in some cases, less toxicity than those children with an unfavorable genotype that were treated with the classical MTX dose of 3 g m−2. Krajinovic et al.37 showed that patients with the MTHFR T677A1298 haplotype had a poorer event-free survival. After controlling for known risk factors, Sepe et al.30 observed that polymorphisms in MTHFR (HR=1.61, P=0.034) significantly increased relapse risk. More recently, Moulik et al.20 indicated that folate deficiency in 26% at baseline was more common in children with MTHFR 677 mutations, and sepsis-related deaths were more frequent in folate-deficient children (P=0.02) during induction.
Heterogeneity in results was observed during our meta-analysis, some of which persisted even when subgroup analysis by ethnicity and disease type was performed. But sensitivity analysis led to a dramatic decrease in I2 (Table 5). This indicates that sample size and HWE are also the reasons for heterogeneity. In addition, to provide a relatively conservative estimate of the evaluated association, a random-effects model was used to accommodate diversity between studies. It is also possible that differences in MTX dose, length of follow-up, definition of toxicity grade and folate supplementation may be responsible for the observed heterogeneity; the true cause remains unclear.
Some limitations of our meta-analysis warrant consideration. First, the number of studies and sample sizes were relatively small, leading to potentially insufficient power to detect mild effects. Second, although our meta-analysis was conducted in across ethnicities, the African population was under-represented, with only one study that had a sample size of 40. Therefore, it is possible that our subgroup analysis by ethnicity may be unable to provide robust results. Third, the included studies used different chemotherapy regimens of MTX. Various MTX doses, duration of therapy and combined chemotherapy agents in different chemotherapy protocols may markedly influence MTX toxicity. Fourth, different studies had different toxicity grading scales, which might influence the accuracy of toxicity combination. Therefore, further studies with a larger sample size, multiple centers and more detailed information should be performed to better assess the effect of MTHFR polymorphism on the risk of MTX-induced toxicity in children with childhood malignancy.
Conclusion
In conclusion, our meta-analysis of published studies demonstrates that the MTHFR C677T polymorphism is associated with MTX-induced toxicity in children with malignancy, especially in mucositis (⩾ grade 3). The MTHFR A1298C polymorphism was not found to be useful in predicting the risk of MTX-induced toxicity. Therefore, for children with childhood malignancy, genotyping of the MTHFR C677T polymorphism is expected to be a useful tool in reducing toxicity and improving outcome in personalized MTX therapy. However, larger and better-designed studies and further evaluations are needed to verify our findings.
References
Johnston WT, Lightfoot TJ, Simpson J, Roman E . Childhood cancer survival: a report from the United Kingdom Childhood Cancer Study. Cancer Epidemiol 2010; 34: 659–666.
Pui CH . Genomic and pharmacogenetic studies of childhood acute lymphoblastic leukemia. Front Med 2015; 9: 1–9.
Zhao M, Liang L, Ji L, Chen D, Zhang Y, Zhu Y et al. MTHFR gene polymorphisms and methotrexate toxicity in adult patients with hematological malignancies: a meta-analysis. Pharmacogenomics 2016; 17: 1005–1017.
Liu SG, Li ZG, Cui L, Gao C, Li WJ, Zhao XX . Effects of methylenetetrahydrofolate reductase gene polymorphisms on toxicities during consolidation therapy in pediatric acute lymphoblastic leukemia in a Chinese population. Leuk Lymphoma 2011; 52: 1030–1040.
Park JA, Shin HY . Influence of genetic polymorphisms in the folate pathway on toxicity after high-dose methotrexate treatment in pediatric osteosarcoma. Blood Res 2016; 51: 50–57.
de Jonge R, Tissing WJ, Hooijberg JH, Jansen G, Kaspers GJ, Lindemans J et al. Polymorphisms in folate-related genes and risk of pediatric acute lymphoblastic leukemia. Blood 2009; 113: 2284–2289.
Gorlick R, Goker E, Trippett T, Waltham M, Banerjee D, Bertino JR . Intrinsic and acquired resistance to methotrexate in acute leukemia. N Engl J Med 1996; 335: 1041–1048.
Stamp LK, Roberts RL . Effect of genetic polymorphisms in the folate pathway on methotrexate therapy in rheumatic diseases. Pharmacogenomics 2011; 12: 1449–1463.
Bellampalli R, Phani NM, Bhat KG, Prasad K, Bhaskaranand N, Guruprasad KP et al. Significance of 5,10-methylenetetrahydrofolate reductase gene variants in acute lymphoblastic leukemia in Indian population: an experimental, computational and meta-analysis. Leuk Lymphoma 2015; 56: 1450–1459.
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 1995; 10: 111–113.
van der Put NM, Gabreels F, Stevens EM, Smeitink JA, Trijbels FJ, Eskes TK et al. A second common mutation in the methylenetetrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 1998; 62: 1044–1051.
Huang L, Tissing WJE, de Jonge R, van Zelst BD, Pieters R . Polymorphisms in folate-related genes: Association with side effects of high-dose methotrexate in childhood acute lymphoblastic leukemia. Leukemia 2008; 22: 1798–1800.
Yang L, Hu X, Xu L . Impact of methylenetetrahydrofolate reductase (MTHFR) polymorphisms on methotrexate-induced toxicities in acute lymphoblastic leukemia: a meta-analysis. Tumour Biol 2012; 33: 1445–1454.
Lopez-Lopez E, Martin-Guerrero I, Ballesteros J, Garcia-Orad A . A systematic review and meta-analysis of MTHFR polymorphisms in methotrexate toxicity prediction in pediatric acute lymphoblastic leukemia. Pharmacogenomics J 2013; 13: 498–506.
Hagleitner MM, Coenen MJ, Aplenc R, Patino-Garcia A, Chiusolo P, Gemmati D et al. The role of the MTHFR 677C>T polymorphism in methotrexate-induced liver toxicity: a meta-analysis in patients with cancer. Pharmacogenomics J 2014; 14: 115–119.
Campbell JM, Bateman E, Stephenson MD, Bowen JM, Keefe DM, Peters MD . Methotrexate-induced toxicity pharmacogenetics: an umbrella review of systematic reviews and meta-analyses. Cancer Chem Pharmacol 2016; 78: 27–39.
D'Angelo V, Ramaglia M, Iannotta A, Francese M, Pota E, Affinita MC et al. Influence of methylenetetrahydrofolate reductase gene polymorphisms on the outcome of pediatric patients with non-Hodgkin lymphoma treated with high-dose methotrexate. Leuk Lymphoma 2013; 54: 2639–2644.
Zgheib NK, Akra-Ismail M, Aridi C, Mahfouz R, Abboud MR, Solh H et al. Genetic polymorphisms in candidate genes predict increased toxicity with methotrexate therapy in Lebanese children with acute lymphoblastic leukemia. Pharmacogenet Genomics 2014; 24: 387–396.
Araoz HV, D'Aloi K, Foncuberta ME, Sanchez La Rosa CG, Alonso CN, Chertkoff L et al. Pharmacogenetic studies in children with acute lymphoblastic leukemia in Argentina. Leuk Lymphoma 2015; 56: 1370–1378.
Moulik NR, Kumar A, Agrawal S, Awasthi S, Mahdi AA, Kumar A . Role of folate status and methylenetetrahydrofolate reductase genotype on the toxicity and outcome of induction chemotherapy in children with acute lymphoblastic leukemia. Leuk Lymphoma 2015; 56: 1379–1384.
Moher D, Liberati A, Tetzlaff J, Altman DG . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8: 336–341.
DerSimonian R, Laird N . Meta-analysis in clinical trials revisited. Contemp Clin Trials 2015; 45 (Pt A): 139–145.
Tantawy AA, El-Bostany EA, Adly AA, Abou El Asrar M, El-Ghouroury EA, Abdulghaffar EE . Methylene tetrahydrofolate reductase gene polymorphism in Egyptian children with acute lymphoblastic leukemia. Blood Coagul Fibrinolysis 2010; 21: 28–34.
D'Angelo V, Ramaglia M, Iannotta A, Crisci S, Indolfi P, Francese M et al. Methotrexate toxicity and efficacy during the consolidation phase in paediatric acute lymphoblastic leukaemia and MTHFR polymorphisms as pharmacogenetic determinants. Cancer Chemother Pharmacol 2011; 68: 1339–1346.
Karathanasis NV, Stiakaki E, Goulielmos GN, Kalmanti M . The role of the methylenetetrahydrofolate reductase 677 and 1298 polymorphisms in Cretan children with acute lymphoblastic leukemia. Genet Test Mol Biomarkers 2011; 15: 5–10.
Kishi S, Griener J, Cheng C, Das S, Cook EH, Pei D et al. Homocysteine, pharmacogenetics, and neurotoxicity in children with leukemia. J Clin Oncol 2003; 21: 3084–3091.
Imanishi H, Okamura N, Yagi M, Noro Y, Moriya Y, Nakamura T et al. Genetic polymorphisms associated with adverse events and elimination of methotrexate in childhood acute lymphoblastic leukemia and malignant lymphoma. J Hum Genet 2007; 52: 166–171.
Shimasaki N, Mori T, Torii C, Sato R, Shimada H, Tanigawara Y et al. Influence of MTHFR and RFC1 polymorphisms on toxicities during maintenance chemotherapy for childhood acute lymphoblastic leukemia or lymphoma. J Pediatr Hematol Oncol 2008; 30: 347–352.
Horinouchi M, Yagi M, Imanishi H, Mori T, Yanai T, Hayakawa A et al. Association of genetic polymorphisms with hepatotoxicity in patients with childhood acute lymphoblastic leukemia or lymphoma. Pediatr Hematol Oncol 2010; 27: 344–354.
Sepe DM, McWilliams T, Chen J, Kershenbaum A, Zhao H, La M et al. Germline genetic variation and treatment response on CCG-1891. Pediatr Blood Cancer 2012; 58: 695–700.
Fisher MC, Cronstein BN . Metaanalysis of methylenetetrahydrofolate reductase (MTHFR) polymorphisms affecting methotrexate toxicity. J Rheumatol 2009; 36: 539–545.
Lee YH, Song GG . Associations between the C677T and A1298C polymorphisms of MTHFR and the efficacy and toxicity of methotrexate in rheumatoid arthritis: a meta-analysis. Clin Drug Invest 2010; 30: 101–108.
Spyridopoulou KP, Dimou NL, Hamodrakas SJ, Bagos PG . Methylene tetrahydrofolate reductase gene polymorphisms and their association with methotrexate toxicity: a meta-analysis. Pharmacogenet Genomics 2012; 22: 117–133.
Owen SA, Lunt M, Bowes J, Hider SL, Bruce IN, Thomson W et al. MTHFR gene polymorphisms and outcome of methotrexate treatment in patients with rheumatoid arthritis: analysis of key polymorphisms and meta-analysis of C677T and A1298C polymorphisms. Pharmacogenomics J 2013; 13: 137–147.
Song GG, Bae SC, Lee YH . Association of the MTHFR C677T and A1298C polymorphisms with methotrexate toxicity in rheumatoid arthritis: a meta-analysis. Clin Rheumatol 2014; 33: 1715–1724.
Salazar J, Altes A, del Rio E, Estella J, Rives S, Tasso M et al. Methotrexate consolidation treatment according to pharmacogenetics of MTHFR ameliorates event-free survival in childhood acute lymphoblastic leukaemia. Pharmacogenomics J 2012; 12: 379–385.
Krajinovic M, Lemieux-Blanchard E, Chiasson S, Primeau M, Costea I, Moghrabi A . Role of polymorphisms in MTHFR and MTHFD1 genes in the outcome of childhood acute lymphoblastic leukemia. Pharmacogenomics J 2004; 4: 66–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix 1
Appendix 1 Search strategy for Cochrane Library
The following text words were used:
methotrexate OR MTX OR mexate OR amethopterin
The search was performed in title, abstract or keywords
PowerPoint slides
Appendices
Appendix 2
Appendix 2 Search strategy for PubMed
-
1
For methotrexate the following MeSH headings and text words were used:methotrexate OR MTX OR mexate OR amethopterin
-
2
For children, the following MeSH headings and text words were used:infant OR infan* OR newborn OR newborn* OR new-born* OR baby OR baby* OR babies OR neonat* OR child OR child* OR schoolchild* OR schoolchild OR school child OR school child* OR kid OR kids OR toddler* OR adolescent OR adoles* OR teen* OR boy* OR girl* OR minors OR minors* OR underag* OR under ag* OR juvenil* OR youth* OR kindergar* OR puberty OR puber* OR pubescen* OR prepubescen* OR prepuberty* OR pediatrics OR pediatric* OR paediatric* OR peadiatric* OR schools OR nursery school* OR preschool* OR pre school* OR primary school* OR secondary school* OR elementary school* OR elementary school OR high school* OR highschool* OR school age OR schoolage OR school age* OR schoolage* OR infancy OR schools, nursery OR infant, newborn
-
3
For MTHFR, the following MeSH headings and text words were used:MTHFR OR methylenetetrahydrofolate reductase OR 5,10-methylenetetrahydrofolate reductase OR methylenetetrahydrofolate, reductase OR FADH OR FADH2 OR EC 1.1.1.171. OR NADPH OR NAD* OR NAD*H methylene-THF reductase OR NADPH2 OR methylene tetrahydrofolate reductase OR tetrahydrofolate reductase, methyleneFinal search: 1 AND 2 AND 3[*=zero or more characters]
Appendix 3
Appendix 3 Search strategy for Embase
-
1
For methotrexate, the following Emtree terms and text words were used:
-
a
Methotrexate/ or methotrexate.mp.
-
b
mexate or amethopterin.mp.
-
c
MTX.mp
-
d
or/1-3
-
a
-
2
For children, the following Emtree terms and text words were used:?
-
a
infant/ or infancy/ or newborn/ or baby/ or child/ or preschool child/ or school child/
-
b
adolescent/ or juvenile/ or boy/ or girl/ or puberty/ or prepuberty/ or pediatrics/
-
c
primary school/ or high school/ or kindergarten/ or nursery school/ or school/
-
d
or/1-3
-
e
(infant$ or (newborn$ or new born$) or (baby or baby$ or babies) or neonate$).mp.
-
f
(child$ or (school child$ or schoolchild$) or (school age$ or schoolage$) or (pre school$ or preschool$)).mp.
-
g
(kid or kids or toddler$ or adoles$ or teen$ or boy$ or girl$).mp.
-
h
(minors$ or (under ag$ or underage$) or juvenil$ or youth$).mp.
-
i
(puber$ or pubescen$ or prepubescen$ or prepubert$).mp.
-
j
(pediatric$ or paediatric$ or peadiatric$).mp.
-
k
(school or schools or (high school$ or highschool$) or primary school$ or nursery school$ or elementary school or secondary school$ or kindergar$).mp.
-
l
or/5-11
-
m
4 or 12
-
a
-
3
For MTHFR, the following Emtree terms and text words were used:
-
a
methylenetetrahydrofolate reductase.mp. or Methylenetetrahydrofolate Reductase/
-
b
(MTHFR or NADPH2).mp.
-
c
(methylene-THF reductase or methylene tetrahydrofolate reductase).mp.
-
d
EC 1.1.1.171.mp.
-
e
(NADPH or NAD$ or FADH2 or FADH$).mp.
-
f
or/1-5
-
a
Final search: 1 and 2 and 3 (Methotrexate AND Children AND MTHFR) [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name; /=Emtree term; $=zero or more characters]
Appendix 4
Search strategy for Web of Science
The following text words were used:
(Methotrexate OR MTX) AND (child* OR pediatric* OR p*diatric*) AND (MTHFR OR methylenetetrahydrofolate reductase)
The search was performed in subject headings
[*=zero or more characters]
Rights and permissions
About this article
Cite this article
Zhu, C., Liu, Y., Wang, S. et al. Associations between the C677T and A1298C polymorphisms of MTHFR and the toxicity of methotrexate in childhood malignancies: a meta-analysis. Pharmacogenomics J 18, 450–459 (2018). https://doi.org/10.1038/tpj.2017.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2017.34
- Springer Nature Limited
This article is cited by
-
Correlation between gene polymorphism and adverse reactions of high-dose methotrexate in osteosarcoma patients: a systematic review and meta-analysis
World Journal of Surgical Oncology (2024)
-
An interactive dose optimizer based on population pharmacokinetic study to guide dosing of methotrexate in Chinese patients with osteosarcoma
Cancer Chemotherapy and Pharmacology (2024)
-
Genetic markers in methotrexate treatments
The Pharmacogenomics Journal (2018)