Abstract
In recent years, increasing interest has been devoted to the susceptibility gene polymorphisms in type 1 diabetes (T1D) as well as in other autoimmune diseases. Among these, a nucleotide polymorphism of the gene encoding for the protein tyrosine phosphatase non-receptor type 22 (PTPN22) has been associated with T1D in several studies. The aim of this study is to define the frequency of the C1858T polymorphism in the PTPN22 gene in a cohort of 113 Caucasian patients (58 males and 55 females) with T1D, and to assess a possible correlation with a group of clinically relevant variables: age at onset, gender, diabetes-related autoantibodies, residual β-cell function and daily insulin requirement (IR) 6 months after diagnosis. Using a PCR-RFLP approach, we evidenced a 17.7% frequency of the PTPN22 C1858T polymorphism in diabetic patients, higher than the frequency showed in the general population. A statistically significant correlation between this polymorphism and higher levels of C-peptide at diagnosis and lower IR at 6 months from diagnosis was observed (P=0.001 and P=0.04). Moreover, 1858T variant carriers were more frequently positive for glutamic acid decarboxylase (GAD) autoantibodies at diagnosis than wild-type subjects (P=0.19). On the other hand, no significant difference regarding age at onset, gender distribution, insulinoma-associated 2 molecule (IA2) and islet cell antibodies (ICA) positivity was found. These findings, if adequately confirmed in the future and extended to larger samples, may characterize a subset of T1D patients with a defined genetic pattern, who may be eligible for trials aimed to preserve residual β-cell function in the coming years.
Similar content being viewed by others
Introduction
Type 1 diabetes (T1D) is an immune-mediated disease causing the destruction of pancreatic β-cell.1, 2 The extent of β-cell destruction and the resulting residual β-cell function are variable. Indeed, C-peptide secretion could be found at onset, during the so-called remission phase.3, 4 This endogenous insulin secretion could completely disappear soon after diagnosis or persist over a long period of time.3, 4
These findings suggest that in T1D, natural course of β-cell destruction may vary markedly, and it may be influenced by different genetic backgrounds.
A novel gene related to T1D has recently been described, namely the protein tyrosine phosphatase non-receptor type 22 (PTPN22).5 PTPN22 is located outside the HLA region, it maps to human chromosome 1p13.3-p13.1 and encodes for the lymphoid-specific tyrosine phosphatase (Lyp), which is expressed in immature and mature lymphocytes of type B and T, as well as in natural killer cells. This protein can be found in three isoforms, Lyp1–3, being Lyp1 the most abundant.6 Although the exact role of this protein remains unclear, studies have shown that Lyp may negatively regulate the proximal signaling pathway after T-cell receptor activation, thus affecting maturation and proliferation.7, 8 Even if data are lacking, it is likely that Lyp may have a similar role in B cells.9, 10 This single-nucleotide polymorphism PTPN22 C1858T, encoding Arg620Trp, was implicated in the disruption of the mechanism of T-cell deactivation, and it has been suggested to modify the thresholds of thymic selection, leading to an expansion of autoreactive T cells. This may explain recent reports about the association of PTPN22 and many autoimmune diseases, like T1D,5 rheumatoid arthritis,11 systemic lupus erythematosus,12 Graves’ disease13, 14 and Hashimoto thyroiditis (HT).15 The association between T1D and PTPN22 C1858T was confirmed in United States,5, 16, 17 German,18 Dutch,19 British,20 Finnish,21 Danish,22 Spanish,23 Italian,24, 25 Czech,26 Azeri,26 Ukrainian Caucasian27 and Colombian28 populations, but not in African-American,11 Asian29 or Japanese30 populations, likely due to the low frequency of the 1858T allele in these three populations.
In recent years, immunologists have tried to exploit immunotherapeutic strategies for treating and/or preventing autoimmune diseases.31 The goal of these strategies should be to eliminate autoimmune processes before the complete loss of ability of cells, that is, pancreatic β-cells in T1D, in order to ensure adequate blood glucose levels.
The aims of this study were (1) to evaluate the prevalence of the C1858T polymorphism in PTPN22 gene in a population of children and adolescents with T1D and (2) to investigate the association between the PTPN22 C1858T variant, gender distribution, age at onset, autoimmunity, residual β-cell function and insulin requirement (IR) at 6 months after diagnosis.
Materials and methods
This study was performed in a cohort of Caucasian children and adolescents (n=113 patients, 58 males and 55 females) with T1D, consecutively diagnosed from January 2003 to November 2013. Patients were recruited and followed up at the Pediatric Diabetes Outpatient Unit, Department of Pediatrics, Faculty of Medicine, ‘G. D’Annunzio’ University of Chieti.
Only patients with an initial diagnosis of T1D according to the ISPAD (International Society for Pediatric and Adolescent Diabetes) criteria were enrolled in the study while patients with suspected non-T1D (type 2 diabetes, maturity-onset diabetes of the young or secondary diabetes) were excluded.
For each subject, the following data were collected: gender, age at study entry, age at diagnosis, severity of onset (presence or absence of ketoacidosis, in particular pH, base excess and bicarbonate levels), evaluation of pancreatic autoimmunity, glycated hemoglobin (HbA1c), body mass index (BMI), personal history of HT and celiac disease (CD), and family history of T1D of at least one first-degree relative. Diabetes-related autoimmunity was assessed at diagnosis of the disease, while CD and thyroid-related autoimmunity were determined at diabetes onset and at annual intervals.
All the subjects were treated with an intensive insulin therapy consisting of three injections of rapid insulin (lispro or aspart) plus glargine insulin once a day. Periodical adjustments were made every 3 or 6 months.
To estimate the residual β-cell function, the C-peptide dosage was measured by immunoassay. The evaluation of pancreatic autoimmunity through the presence of glutamic acid decarboxylase-65 (GAD), insulinoma-associated 2 molecule (IA2) and islet cell antibodies (ICA) was determined at the time of disease onset using commercial kit radioimmunoassay (Bio-Rad, Milan, Italy).
Capillary HbA1C was determined by column assay at diagnosis and after 6 months. Moreover, daily IR 6 months after diagnosis was detected.
Additional information on the presence of other specific autoantibodies (thyroperoxidase autoantibodies and anti-gliadin and anti-transglutaminase IgA antibodies) and familial history of T1D was evaluated at diagnosis.
The C1858T variant (rs2476601) was investigated in a group of 113 patients by PCR amplification followed by PCR-RFLP and agarose gel electrophoresis.
Genomic DNA was extracted from Buccal Swabs using Chelex 100 Resin according to the manufacturer’s instructions (Bio-Rad Laboratories, Hercules, CA, USA) and stored at −20 °C.
PCR was performed in a final reaction volume of 25 μl containing 20–50 ng of genomic DNA template, standard PCR Buffer, 100 μm dNTPs, 1,5 mm MgCl2, 100 nm primers and 1.75U of AB Taq (AB Analitica, Padova, Italy). The amplification conditions consisted of an initial denaturation at 95 °C for 10 min, followed by 30 cycles of 95 °C for 30 s, 63 °C for 60 s, 72 °C for 60 s, and a final extension at 72 °C for 7 min.
The upstream primer 5′-ACCTCCTGGGTTTGTACCTT-3′ and the downstream primer 5′ACTTCTCAGGTCCTTTCAATGT-3′ were used to generate a 678-bp amplicon. The PCR-product size and purity were evaluated through agarose gel electrophoresis.
The PTPN22 genotypes were identified by CViQI restriction endonuclease digestion (Thermo Fisher Scientific, Waltham, MA, USA) which recognizes the G^TAC sites by making a blunt cut. Enzymatic digestion was performed at 37 °C for 2 h according to the manufacturer’s instructions, and the digested products were separated on a 3% agarose gel. The enzymatic digestion created two fragments of 391 bp and 232 bp for the CC variant, two fragments of 391 bp and 283 bp for the TT variant and three fragments of 391 bp, 283 bp and 232 bp for the CT variant.
Written informed consent was obtained from all parents or legal guardians of participating subjects. Statistical analysis was performed by using SPSS (Statistical Package for the Social Science), version 17.0 software for Windows (SPSS Inc, Chicago, IL, USA). A P-value of ⩽0.05 was considered as significant. The distribution of the study population was investigated by Kolmgorov–Smirnov Test.
Normal distribution variables (glycemia, HbA1c, BMI and age at onset; HbA1c and IR after 6 months) were analyzed by comparing the means of patients bearing the tested polymorphism with the means of patients with the normal nucleotide sequence using the Independent Samples T-Test.
Non-normal distribution variables (C-peptide at diagnosis) were analyzed using the Mann–Whitney test.
The prevalence of the studied polymorphism for dichotomous variables such as gender, first grade familiarity for T1D, presence of concomitant autoimmune diseases and the positivity for autoimmune antibodies (ICA, GAD and IA2) were studied using the Fisher’s exact test.
Results
The mean age at diagnosis was 98.5±49.6 s.d. months. BMI was 18.06±3.40 kg m−2 s.d. and HbA1c was 11.38±2.17% s.d. at the time of diagnosis (Table 1).
We found an association of the T allele with T1D, being this allele present in 17.7% of patients, frequency higher than the one previously reported in the general population.24 The C/T genotype was significantly more frequent in patients (14.2%) than T/T (3.5%). Because of the low frequency of 1858T allele, the C/T and T/T genotypes were grouped for statistical analysis.
We did not find statistically significant association of C1858T polymorphism with a positive family history of T1D; however, nearly 50% of C/T and T/T genotype carriers had a family history of T1D. The C1858T PTPN22 polymorphism was not associated with the age of diabetes onset (100.3±46.1 s.d. months for CT/TT versus 96.8±53.1 s.d. months for CC; P=0.77) (Table 1).
The frequency of C/T and T/T genotypes was 15.5% in males versus 20% in females (Table 1). The distribution of C/T and T/T genotypes carrying the predisposing allele did not differ significantly between males and females.
There were no significant differences with respect to gender distribution, age, anthropometric data, HbA1c at diagnosis, other metabolic parameters, family history of diabetes between patients with wild-type genotype and patient carriers of the C/T and T/T genotypes.
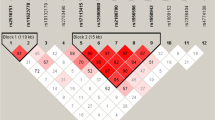
The C-peptide level was significantly higher for the T-allele carriers compared with C-allele (wild-type) carriers at disease onset (genotype C/T-T/T:C-peptide=0.60 ng ml−1 (0.32–0.84) versus genotype C/C:C-peptide=0.40 ng ml−1 (0.20–0.50); P=0.001) (Table 1 and Figure 1).
Children bearing the mutated allele of the investigated gene (PTPN22 C1858T) presented significantly higher levels of C-peptide at the diabetes onset. *P=0.001.
At 6 months, IR was lower in subjects carrying the PTPN22 polymorphism than in subjects homozygous for C allele. Means±s.d. for IR at 6 months were 0.59±0.23 and 0.48±0.19, respectively, in CC subjects and in CT/TT subjects, P=0.04 (Table 2 and Figure 2).
Children bearing the mutated allele of the investigated gene (PTPN22 C1858T) had a significant lower insulin requirement 6 months after the diabetes diagnosis. *P=0.04.
Metabolic control did not differ between the two patient groups during the first year after diabetes onset: genotype C/T-T/T:HbA1c=6.96±1.26% (s.d.) versus genotype C/C:HbA1c=7.19±1.27% (s.d.), n.s. (P=0.32).
The presence of GAD, IA2 and ICA autoantibodies was determined at the time of disease onset. Overall, the C1858T genotype was associated with GAD positivity (63% of CC subjects versus 80% of C/T-T/T subjects; P=0.19), although the result was not statistically significant (Table 3).
In contrast, no effect of C1858T genotype on ICA (32% of C/C subjects versus 21% of C/T-T/T subjects, P=0.32) and IA2 (77% of C/C subjects versus 85% of C/T-T/T subjects, P=0.53) positivity was found (Table 3).
Regarding other autoimmune diseases, among C/T and T/T genotype carriers, HT and CD were more frequent than wild-type carriers, but P-values were not statistical significant (T1D+HT: 17% of C/C subjects versus 25% of C/T-T/T subjects; P=0.21; T1D + CD: 8% of C/C subjects versus 15% of C/T-T/T subjects; P=0.30) (Table 3).
These results remain preliminary, due to the small number of patients.
Discussion
Recent researches have showed that PTPN22 gene is associated with the development of T1D and other autoimmune diseases.
Bottini et al.32 suggested that the risk-carrying allele 1858T suppresses T-cell receptor signaling more efficiently during thymic development, which results in the survival of autoreactive T cells.32
The first report by Bottini et al.5 of the association of PTPN22 C1858T polymorphism with T1D was confirmed by several other association studies.21, 33
This finding was reinforced by recently published meta-analyses, which suggest that the PTPN22 C1858T polymorphism may contribute to the predisposition of T1D, especially in populations of Europe and America.34
Our study provides another replication of the association of PTPN22 1858T allele with T1D. We confirmed the association of the 1858T allele with T1D, with a carrier frequency of 17.7%, compared with the frequency in healthy subjects as previously reported in other studies carried out in the same region (5.6% in the study of Saccucci et al.,24 6.7% in the study of Gloria-Bottini et al.35).
These findings support previous results. Gianchecchi et al.36 showed 17% heterozygosity for PTPN22 C1858T in T1D patients with a higher frequency than in the control group (8.75%).
Mainardi-Novo et al.37 have demonstrated a higher frequency of the C1858T PTPN22 gene polymorphism in T1D patients: C/T-T/T genotypes in 18.7 versus 10.6% of controls.
Also in the series by Kordonouri et al.,38 a higher frequency of the PTPN22 C1858T polymorphism in young T1D patients was found.
A recent study performed by Gloria-Bottini et al.,35 involving patients from continental Italy and Sardinia, demonstrated an association between PTPN22 and T1D (13.6% in T1D versus 6.7%) in patients from continental Italy.
The interaction of the PTPN22 C1858T polymorphism with gender in T1D was suggested.22, 39
Our series did not find a different distribution of the C/T and T/T genotypes between males and females, in agreement with the majority of reported studies.21, 24, 37, 39, 40
Genetic factors have been also reported to have a certain influence on age of diagnosis. However, in the present study the C1858T polymorphism was not associated with the age of diabetes onset, in agreement with a recent Italian study of Gloria-Bottini et al.35 and as previously reported by other researchers.16, 18, 20, 30, 40, 41
Regarding autoimmunity, in the present study we have shown an increased frequency of GAD positivity among PTPN22 polymorphism carriers, although our results are not statistically significant, most likely owing to the sample size. On the other hand, no effect of C1858T genotype on IA2 and ICA positivity (P=0.53 and P=0.32, respectively) was recorded.
An explanation for these findings could be that PTPN22 1858T is involved in two independent control processes from onset and during the following 12 months.42 In our series, T1D autoimmunity was detected only at diabetes onset.
These results are in agreement with the findings of Maziarz et al.,43 which found that the association between PTPN22 (C/T+T/T) and GAD-positive T1D was much stronger than the association between PTPN22 (C/T+T/T) and GAD-negative T1D. Also in the study of Mainardi-Novo et al.,37 the polymorphism was associated with a higher frequency of GAD.
The increased association we have found between 1858T allele in T1D patients with CG and familial history of T1D supports the concept that this genotype confers a general susceptibility to autoimmune diseases, which are known to occur with increased frequency in T1D patients. However, Rueda et al.44 did not observe any statistically significant deviation after comparing allele and genotypic frequencies of PTPN22 C1858T between patients with CD and controls.
In our series, C-peptide levels at onset were significantly higher in T1D subjects carrying the 1858T variant of the PTPN22 gene. According to this result, we also found lower IR after 6 months of disease in diabetic patients carrying the PTPN22 variant. This finding provides a further evidence of better residual β-cell function in C/T and T/T genotype carriers, mainly taking into account similar HbA1c values in the two patient groups. In our series, HbA1C values for the first year after diabetes onset were also similar in the two groups regardless of C-peptide values at diagnosis, probably due to our strict educational program for newly diagnosed patients. These results conflict with other studies. Indeed, Petrone et al.33 found an association between the T allele of the C1858T variant, low fasting C-peptide (as a surrogate marker of residual β-cell mass) and poorer glycemic control at diagnosis, while no differences were shown in IR. These findings were independent of age at onset, sex and HLA risk groups.
Andersen et al.45 showed an association between genetic pattern, including multiple numbers of risk alleles for T1D-associated nucleotide polymorphisms (INS and PTPN22 genes), β-cell function and glycemic control during the first year after diagnosis. They also demonstrated a similar trend between stimulated C-peptide and proinsulin.
Nielsen et al.42 suggested an association between carriers of the T allele and high proinsulin throughout the first year after disease onset. Interestingly, in this study of Hvidoere Study Group on Childhood Diabetes, C/T and T/T carriers presented significantly higher proinsulin (30%) levels at onset and over the 12-month study period compared with the C/C genotype group. Kaas et al.46 reported that proinsulin and C-peptide were positively associated with diabetes onset. Our series did not measure proinsulin levels, but we speculate that the results from the Hvidoere Study Group on Childhood Diabetes are in line with our findings.
In our patients, we found a relationship among C-peptide levels, GAD positivity at diabetes onset, IR at 6 months and PTPN22 1858T variant. These results indicate that the extension of β-cell destruction in T1D could be controlled in part by the PTPN22 gene. Indeed, this mutation is thought to allow T cells to remain activated for a longer period of time.43
Prevention of β-cell loss in T1D patients is expected to improve insulin secretion and disease management.47
The aim of tertiary prevention in T1D and one of the major goals of current research48 is delaying or even stopping β-cell destruction.49 A number of studies tried to develop and identify compounds able to counteract immunological response against pancreatic islets.48, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60
Identification of subset of T1D patients who will be eligible for tertiary prevention trials could encompass genetic markers as well as metabolic parameters. PTPN22 1858T is one of the most recognized T1D-associated allele and shows, in our patients, an association with a residual β-cell function.
Recentlty, a class of Lyp inhibitors able to counteract the gain-of-function mutation generated by the C1858T polymorphism have been identified.61, 62, 63, 64
Xie et al.62 reported a class of thiazolidine-2,4-diones and 2-thioxothiazolidin-4-ones acting as potent inhibitors of Lyp, suggesting a new approach to treatment of autoimmune diseases by inhibition of Lyp. Moreover, Vang et al.63 studied inhibition of Lyp by benzofuran salicylic acids.
This new approach may be a future benefit for tertiary prevention trials, aimed toward preventing the progression of β-cell loss. Our results provide further evidence of the heterogeneity of T1D.
Undoubtedly, a weakness of our study is represented by the lack of data on C-peptide at 6 months. However, our results show an IR of ⩽0.5 units per kg per day associated with HbA1C ⩽7.5 % in CT+TT carriers: these parameters have been used to define the partial remission period, that is obviously associated with residual β-cell function.65, 66
Moreover, our CT+TT carriers also showed a mean value of ‘insulin dose-adjusted A1C’ (IDDA1C, a qualitative measure of partial remission) of 5.22. This value fulfills the threshold (⩽9) established by Mortensen et al.67
A strength of our study is the evidence of higher C-peptide levels at onset, lower IR after 6 months of disease, in C/T and T/T carriers, suggesting that PTPN22 C1858T could be associated with slow disease progression.
Our results, once confirmed by further studies, may be useful in identifying a subset of patients who can potentially benefit from novel therapeutic approaches in the coming years.
References
Notkins AL, Lernmark A . Autoimmune type 1 diabetes: resolved and unresolved issues. J Clin Invest 2001; 108: 1247–1252.
Atkinson MA, Eisenbarth GS . Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet 2001; 358: 221–229.
Effects of age, duration and treatment of insulin-dependent diabetes mellitus on residual beta-cell function: observations during eligibility testing for the Diabetes Control and Complications Trial (DCCT). The DCCT Research Group. J Clin Endocrinol Metab 1987; 65: 30–36.
Schölin A, Björklund L, Borg H, Arnqvist H, Björk E, Blohmé G et al. Islet antibodies and remaining beta-cell function 8 years after diagnosis of diabetes in young adults: a prospective follow-up of the nationwide Diabetes Incidence Study in Sweden. J Intern Med 2004; 255: 384–391.
Bottini N, Musumeci L, Alonso A, Rahmouni S, Nika K, Rostamkhani M et al. A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes. Nat Genet 2004; 36: 337–338.
Wang S, Dong H, Han J, Ho WT, Fu X, Zhao ZJ . Identification of a variant form of tyrosine phosphatase LYP. BMC Mol Biol 2010; 11: 78.
Gjörloff-Wingren A, Saxena M, Williams S, Hammi D, Mustelin T . Characterization of TCR-induced receptor-proximal signaling events negatively regulated by the protein tyrosine phosphatase PEP. Eur J Immunol 1999; 29: 3845–3854.
Hill RJ, Zozulya S, Lu Y-L, Ward K, Gishizky M, Jallal B . The lymphoid protein tyrosine phosphatase Lyp interacts with the adaptor molecule Grb2 and functions as a negative regulator of T-cell activation. Exp Hematol 2002; 30: 237–244.
Burn GL, Svensson L, Sanchez-Blanco C, Saini M, Cope AP . Why is PTPN22 a good candidate susceptibility gene for autoimmune disease? FEBS Lett 2011; 585: 3689–3698.
Rieck M, Arechiga A, Onengut-Gumuscu S, Greenbaum C, Concannon P, Buckner JH . Genetic variation in PTPN22 corresponds to altered function of T and B lymphocytes. J Immunol 2007; 179: 4704–4710.
Begovich AB, Carlton VEH, Honigberg LA, Schrodi SJ, Chokkalingam AP, Alexander HC et al. A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am J Hum Genet 2004; 75: 330–337.
Lea WW, Lee YH . The association between the PTPN22 C1858T polymorphism and systemic lupus erythematosus: a meta-analysis update. Lupus 2011; 20: 51–57.
Velaga MR, Wilson V, Jennings CE, Owen CJ, Herington S, Donaldson PT et al. The codon 620 tryptophan allele of the lymphoid tyrosine phosphatase (LYP) gene is a major determinant of Graves’ disease. J Clin Endocrinol Metab 2004; 89: 5862–5865.
Skórka A, Bednarczuk T, Bar-Andziak E, Nauman J, Ploski R . Lymphoid tyrosine phosphatase (PTPN22/LYP) variant and Graves’ disease in a Polish population: association and gene dose-dependent correlation with age of onset. Clin Endocrinol (Oxf) 2005; 62: 679–682.
Criswell LA, Pfeiffer KA, Lum RF, Gonzales B, Novitzke J, Kern M et al. Analysis of families in the multiple autoimmune disease genetics consortium (MADGC) collection: the PTPN22 620W allele associates with multiple autoimmune phenotypes. Am J Hum Genet 2005; 76: 561–571.
Steck AK, Liu S-Y, McFann K, Barriga KJ, Babu SR, Eisenbarth GS et al. Association of the PTPN22/LYP gene with type 1 diabetes. Pediatr Diabetes 2006; 7: 274–278.
Ladner MB, Bottini N, Valdes AM, Noble JA . Association of the single nucleotide polymorphism C1858T of the PTPN22 gene with type 1 diabetes. Hum Immunol 2005; 66: 60–64.
Kahles H, Ramos-Lopez E, Lange B, Zwermann O, Reincke M, Badenhoop K . Sex-specific association of PTPN22 1858T with type 1 diabetes but not with Hashimoto’s thyroiditis or Addison's disease in the German population. Eur J Endocrinol 2005; 153: 895–899.
Zhernakova A, Eerligh P, Wijmenga C, Barrera P, Roep BO, Koeleman BPC . Differential association of the PTPN22 coding variant with autoimmune diseases in a Dutch population. Genes Immun 2005; 6: 459–461.
Smyth D, Cooper JD, Collins JE, Heward JM, Franklyn JA, Howson JMM et al. Replication of an association between the lymphoid tyrosine phosphatase locus (LYP/PTPN22) with type 1 diabetes, and evidence for its role as a general autoimmunity locus. Diabetes 2004; 53: 3020–3023.
Hermann R, Lipponen K, Kiviniemi M, Kakko T, Veijola R, Simell O et al. Lymphoid tyrosine phosphatase (LYP/PTPN22) Arg620Trp variant regulates insulin autoimmunity and progression to type 1 diabetes. Diabetologia 2006; 49: 1198–1208.
Nielsen C, Hansen D, Husby S, Lillevang ST . Sex-specific association of the human PTPN22 1858T-allele with type 1 diabetes. Int J Immunogenet 2007; 34: 469–473.
Santiago JL, Martínez A, de la Calle H, Fernández-Arquero M, Figueredo MA, de la Concha EG et al. Susceptibility to type 1 diabetes conferred by the PTPN22 C1858T polymorphism in the Spanish population. BMC Med Genet 2007; 8: 54.
Saccucci P, Del Duca E, Rapini N, Verrotti A, Piccinini S, Maccari et al. Association between PTPN22 C1858T and type 1 diabetes: a replication in continental Italy. Tissue Antigens 2008; 71: 234–237.
Gloria-Bottini F, Saccucci P, Manca-Bitti ML, Rapini N, Verrotti A, Neri et al. Type 1 diabetes mellitus. Comparison between the association with PTPN22 genotype and the association with ACP1-ADA1 joint genotype. Diabetes Res Clin Pract 2014; 106: 7–9.
Cinek O, Hradsky O, Ahmedov G, Slavcev A, Kolouskova S, Kulich M et al. No independent role of the -1123 G>C and+2740 A>G variants in the association of PTPN22 with type 1 diabetes and juvenile idiopathic arthritis in two Caucasian populations. Diabetes Res Clin Pract 2007; 76: 297–303.
Fedetz M, Matesanz F, Caro-Maldonado A, Smirnov II, Chvorostinka VN, Moiseenko TA et al. The 1858T PTPN22 gene variant contributes to a genetic risk of type 1 diabetes in a Ukrainian population. Tissue Antigens 2006; 67: 430–433.
Gomez LM, Anaya J-M, Gonzalez CI, Pineda-Tamayo R, Otero W, Arango et al. PTPN22 C1858T polymorphism in Colombian patients with autoimmune diseases. Genes Immun 2005; 6: 628–631.
Ikegami H, Kawabata Y, Noso S, Fujisawa T, Ogihara T . Genetics of type 1 diabetes in Asian and Caucasian populations. Diabetes Res Clin Pract 2007; 77: S116–S121.
Mori M, Yamada R, Kobayashi K, Kawaida R, Yamamoto K . Ethnic differences in allele frequency of autoimmune-disease-associated SNPs. J Hum Genet 2005; 50: 264–266.
Fierabracci A . Peptide immunotherapies in Type 1 diabetes: lessons from animal models. Curr Med Chem 2011; 18: 577–586.
Bottini N, Vang T, Cucca F, Mustelin T . Role of PTPN22 in type 1 diabetes and other autoimmune diseases. Semin Immunol 2006; 18: 207–213.
Petrone A, Spoletini M, Zampetti S, Capizzi M, Zavarella S, Osborn J et al. The PTPN22 1858T gene variant in type 1 diabetes is associated with reduced residual beta-cell function and worse metabolic control. Diabetes Care 2008; 31: 1214–1218.
Tang S, Peng W, Wang C, Tang H, Zhang Q . Association of the PTPN22 gene (+1858C/T, -1123G/C) polymorphisms with type 1 diabetes mellitus: a sistematic review and meta-analysis. Diabetes Res Clin Pract 2012; 97: 446–452.
Gloria-Bottini F, Saccucci P, Meloni GF, Manca-Bitti ML, Coppeta L, Neri et al. Study of factors influencing susceptibility and age at onset of type 1 diabetes: a review of data from Continental Italy and Sardinia. World J Diabetes 2014; 5: 557–561.
Gianchecchi E, Palombi M, Fierabracci A . The putative role of the C1858T polymorphism of protein tyrosine phosphatase PTPN22 gene in autoimmunity. Autoimmun Rev 2013; 12: 717–725.
Mainardi-Novo DTO, Santos AS, Fukui RT, Gamberini M, Correia MRS, Ruiz MO et al. The PTPN22 1858T allele but not variants in the proximal promoter region of IL-21 gene is associated with the susceptibility to type 1 diabetes and the presence of autoantibodies in a Brazilian cohort. Clin Exp Immunol 2013; 172: 16–22.
Kordonouri O, Hartmann R, Charpentier N, Knip M, Danne T, Ilonen J . Genetic risk markers related to diabetes-associated autoantibodies in young patients with type 1 diabetes in berlin, Germany. Exp Clin Endocrinol Diabetes 2010; 118: 245–249.
Giza S, Goulas A, Gbandi E, Effraimidou S, Papadopoulou-Alataki E, Eboriadou M et al. The role of PTPN22 C1858T gene polymorphism in diabetes mellitus type 1: first evaluation in Greek children and adolescents. Biomed Res Int 2013; 2013: 721604.
Chagastelles PC, Romitti M, Trein MR, Bandinelli E, Tschiedel B, Nardi NB . Association between the 1858T allele of the protein tyrosine phosphatase nonreceptor type 22 and type 1 diabetes in a Brazilian population. Tissue Antigens 2010; 76: 144–148.
Korolija M, Renar IP, Hadžija M, Medvidović EP, Pavković P, Jokić M et al. Association of PTPN22 C1858T and CTLA-4 A49G polymorphisms with type 1 diabetes in Croatians. Diabetes Res Clin Pract 2009; 86: e54–e57.
Nielsen LB, Pörksen S, Andersen MLM, Fredheim S, Svensson J, Hougaard P et al. The PTPN22 C1858T gene variant is associated with proinsulin in new-onset type 1 diabetes. BMC Med Genet 2011; 12: 41.
Maziarz M, Janer M, Roach JC, Hagopian W, Palmer JP, Deutsch K et al. The association between the PTPN22 1858C>T variant and type 1 diabetes depends on HLA risk and GAD65 autoantibodies. Genes Immun 2010; 11: 406–415.
Rueda B, Núñez C, Orozco G, López-Nevot MA, de la Concha EG, Martin J et al. C1858T functional variant of PTPN22 gene is not associated with celiac disease genetic predisposition. Hum Immunol 2005; 66: 848–852.
Andersen MLM, Rasmussen MA, Pörksen S, Svensson J, Vikre-Jørgensen J, Thomsen J et al. Complex multi-block analysis identifies new immunologic and genetic disease progression patterns associated with the residual β-cell function 1 year after diagnosis of type 1 diabetes. PLoS One 2013; 8: e64632.
Kaas A, Andersen MLM, Fredheim S, Hougaard P, Buschard K, Petersen JS et al. Proinsulin, GLP-1, and glucagon are associated with partial remission in children and adolescents with newly diagnosed type 1 diabetes. Pediatr Diabetes 2012; 13: 51–58.
Steffes MW, Sibley S, Jackson M, Thomas W . Beta-cell function and the development of diabetes-related complications in the diabetes control and complications trial. Diabetes Care 2003; 26: 832–836.
Cook JJ, Hudson I, Harrison LC, Dean B, Colman PG, Werther GA et al. Double-blind controlled trial of azathioprine in children with newly diagnosed type I diabetes. Diabetes 1989; 38: 779–783.
Wherrett DK, Daneman D . Prevention of type 1 diabetes. Endocrinol Metab Clin North Am 2009; 38: 777–790.
Buckingham BA, Sandborg CI . A randomized trial of methotrexate in newly diagnosed patients with type 1 diabetes mellitus. Clin Immunol 2000; 96: 86–90.
Silverstein J, Maclaren N, Riley W, Spillar R, Radjenovic D, Johnson S . Immunosuppression with azathioprine and prednisone in recent-onset insulin-dependent diabetes mellitus. N Engl J Med 1988; 319: 599–604.
Mastrandrea L, Yu J, Behrens T, Buchlis J, Albini C, Fourtner S et al. Etanercept treatment in children with new-onset type 1 diabetes: pilot randomized, placebo-controlled, double-blind study. Diabetes Care 2009; 32: 1244–1249.
Keymeulen B, Vandemeulebroucke E, Ziegler AG, Mathieu C, Kaufman L, Hale G et al. Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N Engl J Med 2005; 352: 2598–2608.
Coppieters KT, Harrison LC, von Herrath MG . Trials in type 1 diabetes: antigen-specific therapies. Clin Immunol 2013; 149: 345–355.
Hartemann A, Bensimon G, Payan CA, Jacqueminet S, Bourron O, Nicolas N et al. Low-dose interleukin 2 in patients with type 1 diabetes: a phase 1/2 randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2013; 1: 295–305.
Moran A, Bundy B, Becker DJ, DiMeglio LA, Gitelman SE, Goland R et al. Interleukin-1 antagonism in type 1 diabetes of recent onset: two multicentre, randomised, double-blind, placebo-controlled trials. Lancet 2013; 381: 1905–1915.
Yu A, Snowhite I, Vendrame F, Rosenzwajg M, Klatzmann D, Pugliese et al. Selective IL-2 responsiveness of regulatory T cells through multiple intrinsic mechanisms support the use of low-dose IL-2 therapy in Type-1 diabetes. Diabetes 2015; 64: 2172–2183.
Orban T, Bundy B, Becker DJ, DiMeglio LA, Gitelman SE, Goland R et al. Co-stimulation modulation with abatacept in patients with recent-onset type 1 diabetes: a randomised, double-blind, placebo-controlled trial. Lancet 2011; 378: 412–419.
Pozzilli P, Guglielmi C, Maggi D, Carlone A, Buzzetti R, Manfrini S . Clinical update on the use of immuno modulators (antiCD3, GAD, Diapep277, anti-IL1) in type 1 diabetes. Curr Pharm Des 2011; 17: 3224–3228.
Verrotti A, Chiuri RM, Blasetti A, Mohn A, Chiarelli F . Treatment options for paediatric diabetes. Expert Opin Pharmacother 2010; 11: 2483–2495.
Hou X, Li R, Li K, Yu X, Sun J-P, Fang H . Fast identification of novel lymphoid tyrosine phosphatase inhibitors using target–ligand interaction-based virtual screening. J Med Chem 2014; 57: 9309–9322.
Xie Y, Liu Y, Gong G, Rinderspacher A, Deng S-X, Smith DH et al. Discovery of a novel submicromolar inhibitor of the lymphoid specific tyrosine phosphatase. Bioorg Med Chem Lett 2008; 18: 2840–2844.
Vang T, Xie Y, Liu WH, Vidović D, Liu Y, Wu S et al. Inhibition of lymphoid tyrosine phosphatase by benzofuran salicylic acids. J Med Chem 2011; 54: 562–571.
He Y, Liu S, Menon A, Stanford S, Oppong E, Gunawan AM et al. A potent and selective small-molecule inhibitor for the lymphoid-specific tyrosine phosphatase (LYP), a target associated with autoimmune diseases. J Med Chem 2013; 56: 4990–5008.
Schölin A, Berne C, Schvarcz E, Karlsson FA, Björk E . Factors predicting clinical remission in adult patients with type 1 diabetes. J Intern Med 1999; 245: 155–162.
Ortqvist E, Falorni A, Scheynius A, Persson B, Lernmark A . Age governs gender-dependent islet cell autoreactivity and predicts the clinical course in childhood IDDM. Acta Paediatr 1997; 86: 1166–1171.
Mortensen HB, Hougaard P, Swift P, Hansen L, Holl RW, Bjoerndalen H et al. New definition for the partial remission period in children and adolescents with type 1 diabetes. Diabetes Care 2009; 32: 1384–1390.
Acknowledgements
We express our gratitude to patients and their families for participating in this study. We also thank Kelly Chuang, MHS, Johns Hopkins University for help with language revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Blasetti, A., Di Giulio, C., Tumini, S. et al. Role of the C1858T polymorphism of protein tyrosine phosphatase non-receptor type 22 (PTPN22) in children and adolescents with type 1 diabetes. Pharmacogenomics J 17, 186–191 (2017). https://doi.org/10.1038/tpj.2016.6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tpj.2016.6
- Springer Nature Limited