Abstract
Psoriasis is characterized by keratinocyte (KC) hyperproliferation and inflammatory cell infiltration, but the mechanisms remain unclear. In an imiquimod-induced mouse psoriasiform model, p38 activity is significantly elevated in KCs and p38α specific deletion in KCs ameliorates skin inflammation. p38α signaling promotes KC proliferation and psoriasis-related proinflammatory gene expression during psoriasis development. Mechanistically, p38α enhances KC proliferation and production of inflammatory cytokines and chemokines by activating STAT3. While p38α signaling in KCs does not affect the expression of IL-23 and IL-17, it substantially amplifies the IL-23/IL-17 pathogenic axis in psoriasis. The therapeutic effect of IL-17 neutralization is associated with decreased p38 and STAT3 activities in KCs and targeting the p38α-STAT3 axis in KCs ameliorates the severity of psoriasis. As IL-17 also highly activates p38 and STAT3 in KCs, our findings reveal a sustained signaling circuit important for psoriasis development, highlighting p38α-STAT3 axis as an important target for psoriasis treatment.
Similar content being viewed by others
Introduction
Psoriasis is a chronic inflammatory skin disease characterized by epidermis hyperproliferation and the infiltration of multiple inflammatory cells in the dermis, which affects ~125 million people globally and ~2–3% of the population worldwide1,2,3,4. Although the pathogenesis of psoriasis is still unclear, much progress has been made to uncover this disease pathogenesis by using imiquimod (IMQ)-5 or interleukin-23 (IL-23)-6 induced psoriatic mouse models. Currently, it is appreciated that the dysregulated interaction between keratinocytes (KCs) and immune cells is critical for psoriasis development2,7.
KCs are the primary cell type in the epidermis, forming a barrier against environmental damage8. Various insults act on KCs to induce them to produce multiple inflammatory cytokines and chemokines, which further recruit and activate immune cells to initiate the inflammatory immune response7. One of recent pioneer studies demonstrates that triggers-stimulated KCs can secrete LL-37, binding with self-nucleic acids from these cells to form complexes9,10. These complexes further stimulate dendritic cells (DCs) to release polarized cytokines, such as IL-6 and IL-23, thereby activating the differentiation and/or expansion of IL-17-producing T cells (T17)5. T17 produce inflammatory molecules such as IL-17 and TNFα, acting on KCs and leading to their abnormal differentiation and hyperproliferation. The stimulated KCs can produce multiple chemokines to recruit various immune cells such as neutrophils into inflamed psoriatic plaques11. Moreover, these stimulated KCs can also synthesize and release certain cytokines, antimicrobial peptides, and growth factors, further enhancing the vicious cycles of inflammatory response12,13. Thus, targeting KCs is a promising therapeutic strategy for the treatment of psoriasis, highlighting an essential step to explore the signaling pathways that regulate the proliferation and inflammatory responses of KCs.
p38 mitogen-activated protein kinase (MAPK) is one of the most important signaling pathways to regulate the inflammatory immune responses14,15. Increased activation of p38 kinase in lesional compared to nonlesional psoriatic skin16,17,18, as well as in CD45+ immune cells in the skins in an IMQ-induced mouse psoriasiform model19 has been reported. Improved psoriasis severity is accompanied with decreased activation of p38 kinase in Adalimumab therapy18. Accordingly, the expression of mitogen-activated protein kinase phosphatase 1 (MKP-1), the negative regulator of p38α, is decreased in mouse skin upon IMQ treatment20 as well as in lesional psoriatic skin21. Our previous study indicates that MKP-1-deficient mice have severe skin inflammation upon IMQ-treatment20. Inhibition of p38 kinase suppresses the development of psoriasis-like lesions in a human skin transplant model of psoriasis22. Cutaneous activation of p38 kinase is sufficient to induce psoriasiform inflammation including epidermal thickening, neutrophil infiltration and proinflammatory cytokine expression in mice23. Our previous study has shown that p38α signaling in Langerhans cells (LCs), but not in other DCs or T cells, is essential for IMQ-induced psoriasiform19, demonstrating the cell-type specific role of p38α in psoriasis pathogenesis. However, the role of p38α in KCs in vivo is still not well known.
In the current study, we found an increased p38 activity in KCs of IMQ-treated mice. To further examine the role of p38α in KCs in psoriasis in vivo, we crossed Mapk14flox/flox mice with K14-Cre transgenic mice, which have a human keratin 14 promoter/enhancer sequence, to obtain the mice with specific deletion of p38α in KCs. In the IMQ- or IL-23-induced mouse psoriasiform model, we found that p38α-signal transducer and activator of transcription 3 (STAT3) signaling axis in KCs significantly aggravated psoriasis severity by promoting KC proliferation and the production of proinflammatory cytokines and chemokines. Our study suggests that p38α-STAT3 axis is an important target for developing therapies for the treatment of skin inflammatory diseases.
Results
Deletion of p38α in KCs largely ameliorates IMQ-induced psoriasiform disease
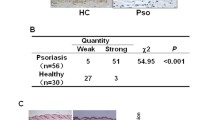
An increased p38 activity has been reported in lesional psoriatic skin16,17,18, but the role and underlying mechanisms of p38 in psoriasis pathogenesis are still unclear. In an IMQ-induced mouse psoriasiform model, we found that p38 activity was significantly elevated in epidermal tissue either by immunofluorescence (IF) staining (Fig. 1a). Further Western blot and flow cytometry analyses showed that the phosphorylation level of p38 was higher in KCs from IMQ-treated mice than control cream-treated mice (Fig. 1b, c and Supplementary Fig. 1a). These findings suggest an important role of p38 signaling in KCs during psoriasis pathogenesis. Considering that p38α is the main subunit of p38 MAPK in the regulation of inflammation, to delineate the specific role of KC-intrinsic p38 signaling in the pathogenesis of psoriasis in vivo, we generated Mapk14flox/floxK14-Cre mice (referred to as “p38αΔKC mice” here). In p38αΔKC mice, we observed an efficient deletion of p38α in skin KCs both at mRNA level and protein level (Supplementary Fig. 1b, c). Notably, KC-specific ablation of p38α did not compromise mouse skin development and homeostasis (Supplementary Fig. 1d, e). In the IMQ-induced psoriasiform model, p38αΔKC mice had significantly decreased ear thickness and disease severity score compared with wild-type mice (Fig. 1d, e). Histological analysis showed less epidermal hyperplasia and inflammation in IMQ-treated skin of p38αΔKC mice than wild-type mice (Fig. 1f). In addition, the percentages and cell numbers of neutrophils and macrophages were largely reduced in skin tissues of p38αΔKC mice compared with wild-type control mice. However, the percentages and cell numbers of dendritic epidermal T cells (DETCs), γδ T cells, TCRβ+ T cells and DCs were comparable in skin tissues of IMQ-treated wild-type mice and p38αΔKC mice (Fig. 1g). Collectively, these findings indicate a key role for KC p38α signaling in IMQ-induced psoriasiform skin disease.
a–c Wild-type (WT) mice were topically treated with imiquimod (IMQ)-containing or control cream for three consecutive days. The phosphorylation (p) of p38 in skin sections was examined by immunofluorescence staining (a). Scale bar: 50 μm. The abundance of p38 and p-p38 in keratinocytes (KCs) was analyzed by Western blot and the relative expression was normalized with GAPDH (b, n = 3). The activity of p38 in KCs was detected by flow cytometry (c, n = 5). d–g WT and p38αΔKC mice were topically treated with IMQ for six consecutive days (n = 6). Changes in ear thickness (d) and disease severity score (e) were recorded. Histopathological changes in skin sections were examined by hematoxylin and eosin (H&E) staining (f). Scale bar: 50 μm. The percentages and cell numbers of neutrophils, macrophages, dendritic epidermal T cells (DETCs), γδ T cells, TCRβ+ T cells, and dendritic cells (DCs) in skin tissue were analyzed (g). All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-tailed Student’s t tests (b, c, e, g) and two-way analysis of variance (ANOVA) (d) were performed. *P < 0.05; **P < 0.01; ***P < 0.001; ns not significant.
p38α signaling in KCs promotes psoriasis-related inflammatory gene expression upon IMQ treatment
Consistent with the decreased disease severity in p38αΔKC mice after IMQ treatment, the skin tissues of IMQ-treated p38αΔKC mice had significantly reduced transcript levels of various psoriasis-related inflammatory cytokines and chemokines, such as Tnfa, Il1a, Il1b, Cxcl1, and Cxcl2 (Fig. 2a). The mRNA expression of several genes encoding antimicrobial peptides such as S100a7a, S100a8, and S100a9 was also decreased in IMQ-treated p38αΔKC mice compared with wild-type mice (Fig. 2a). Furthermore, the mRNA expression of Krt6, Krt16, and Krt17, encoding the keratins related to excessive KC proliferation, was significantly reduced in IMQ-treated p38αΔKC mice (Fig. 2a). However, the mRNA levels of Il6, Il19, Il20, Il24, Il36a, Il36b, Il36g, Ifng, Cxcl5, Cxcl9, Cxcl10, Ccl20, Lcn2, Reg3g, Defb2, Krt1, Krt10, and Krt14 were comparable between wild-type mice and p38αΔKC mice (Fig. 2a and Supplementary Fig. 2a). Among these molecules, KRT14 is a basal layer-specific keratin and will be replaced by KRT1/KRT10 in suprabasal layers during KC differentiation24, indicating that p38α might not be required for KC differentiation. IL-36α, IL-36β and IL-36γ secreted by KCs have been shown to be upregulated in human psoriatic skin and mouse models of psoriasiform skin disease and can activate DCs and neutrophils25,26. Notably, although IL-23/IL-17 axis and IL-17 family of cytokines play pivotal roles in the pathogenesis of psoriasis5,27,28,29,30, the transcript levels of Il23p19, Il22, Il17a, Il17c, Il17d, Il17e, and Il17f, and the production of IL-17A from γδ T cells and CD4+ T cells were comparable between IMQ-treated wild-type mice and p38αΔKC mice (Fig. 2a and Supplementary Figs. 2a, b and 3a). The percentages of γδ T cells, CD4+ T cells, CD8+ T cells, Th1 cells, Th2 cells, Treg cells, and IFNγ+CD8+ T cells were also similar in IMQ-treated wild-type mice and p38αΔKC mice (Supplementary Fig. 3a). Moreover, wild-type mice and p38αΔKC mice had comparable proportions of naïve γδ T cells, effector γδ T cells, naïve CD4+ T cells and effector CD4+ T cells upon IMQ treatment (Supplementary Fig. 3b, c). In line with these findings, there were no significant differences in the frequencies of total DCs, LCs, and dermal DCs, and the expression of activation markers CD40, CD80, and CD86 on LCs and dermal DCs in skin tissues of IMQ-treated wild-type mice and p38αΔKC mice (Supplementary Fig. 4a−c). In addition, the proportions of migratory DCs and resident DCs were also similar in draining lymph nodes of IMQ-treated wild-type mice and p38αΔKC mice (Supplementary Fig. 4d).
WT and p38αΔKC mice were topically treated with IMQ for six consecutive days. a Relative mRNA expression of inflammatory cytokines, chemokines, antimicrobial peptides, and keratins was measured in skin tissue (n = 5). b KCs were sorted from skin tissue at days 0, 1, 3, and 6 to examine the relative mRNA levels of inflammation-related genes (n = 5). All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-tailed Student’s t tests were performed (a, each time point of b). *P < 0.05; **P < 0.01; ***P < 0.001; ns not significant.
To explore the potential mechanism by which KC p38α regulates the pathogenesis of IMQ-induced psoriasiform skin disease, we purified KCs from IMQ-treated skin tissues at different time points and analyzed the related gene expression. The results showed that IMQ treatment significantly increased the mRNA expression of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Ccl20, S100a7a, S100a8, S100a9, Krt6, Krt16, Krt17, Il36a, Il36b, and Il36g in KCs (Fig. 2b and Supplementary Fig. 2c). Although the expression of Ccl20, Il36a, Il36b, and Il36g mRNA in KCs was comparable between IMQ-treated wild-type mice and p38αΔKC mice, p38α deletion in KCs largely reduced the transcript levels of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, S100a7a, S100a8, S100a9, Krt6, Krt16, and Krt17 in KCs upon IMQ treatment (Fig. 2b and Supplementary Fig. 2c). These results collectively demonstrate that deletion of p38α in KCs ameliorates psoriasis-related inflammatory gene expression, but does not affect IL-23/IL-17 axis during IMQ-treatment.
p38α signaling promotes KC hyperproliferation and psoriasis severity in a STAT3-dependent manner
KC hyperproliferation is a major pathogenic factor in psoriasis13. The decreased expression of keratin genes such as Krt6, Krt16, and Krt17 in p38αΔKC mice, which mediate the abnormal proliferation of epidermal cells, prompted us to further examine whether p38α signaling can regulate KC hyperproliferation during psoriasis development. Immunohistochemical analysis showed reduced Ki-67 staining levels in epidermal cells of p38αΔKC mice treated with IMQ for 3 days (Fig. 3a) and 6 days (Fig. 3b) compared with wild-type mice. While the BrdU incorporation (indicating as cell proliferation) in KCs was similar in wild-type mice and p38αΔKC mice under steady state, there was significantly lower BrdU incorporation in KCs of p38αΔKC mice than that in wild-type mice upon IMQ treatment (Fig. 3c). The apoptosis of KCs has been shown to contribute to psoriasis pathogenesis31. Notably, active caspase-3 staining showed comparable apoptosis of KCs in both wild-type mice and p38αΔKC mice with or without IMQ treatment (Fig. 3d). These results demonstrate that p38α signaling promotes KC proliferation, but does not affect KC apoptosis during psoriasis development.
a, b Immunohistochemistry analysis of Ki-67 in skin sections of WT and p38αΔKC mice treated with IMQ for 3 days (a, n = 4) and 6 days (b, n = 4). Scale bar: 100 μm. c, d The frequencies of BrdU+ KCs (c) and active caspase-3+ KCs (d) in skin tissue of IMQ-treated wild-type mice and p38αΔKC mice at indicated time points (n = 5). All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-way ANOVA with Bonferroni post-tests (c, d) were performed. **P < 0.01; ns not significant.
To explore the potential molecular mechanisms for p38α signaling in regulating KC proliferation and psoriasis-related inflammatory gene expression, we treated primary KCs with R848, an IMQ analog, for further analysis. Upon R848 stimulation, primary p38α-deficient KCs had significantly decreased percentages of Edu+ cells compared with primary wild-type KCs, indicating a reduced proliferation of primary p38α-deficient KCs (Fig. 4a). Moreover, deletion of p38α in KCs substantially decreased the mRNA levels of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, S100a7a, S100a8, S100a9, Krt6, Krt16, and Krt17 in primary KCs stimulated with R848 (Fig. 4b), similar to the phenotype we obtained in vivo (Fig. 2b). Further Western blot analysis showed that p38α deficiency reduced the phosphorylation level of STAT3 but did not affect the activities of JNK, ERK, p65 and Akt in primary KCs stimulated with R848 (Fig. 4c and Supplementary Fig. 5a). IF analysis also demonstrated lower phosphorylation level of STAT3 in epidermis of IMQ-treated p38αΔKC mice (Fig. 4d).
a–c Primary KCs of WT and p38αΔKC mice were stimulated with R848. R848 stimulation for 24 h to perform 5-ethynyl-2’-deoxyuridine (Edu) incorporation assay and calculate the frequency of Edu+ cells (a, n = 5-6). Scale bar: 100 μm. R848 stimulation for 5 h to determine the mRNA levels of inflammation-related genes and the relative expression was normalized with unstimulated KCs (b, n = 4). R848 stimulation for indicated times to examine the activities of STAT3, p38, JNK, ERK, p65 and Akt (c). The numbers below the lanes indicate the band intensity relative to total protein. d Immunofluorescence staining of p-STAT3 in skin sections of WT and p38αΔKC mice treated with IMQ for 3 days (n = 4). Scale bar: 50 μm. e–j WT and p38αΔKC mice topically treated with IMQ were intradermally injected with STAT3 activator Colivelin (Col) or control vehicle (Veh) (n = 6): changes in ear thickness (e); disease severity score (f); histopathological changes in skin sections (g); infiltration of neutrophils (h); and relative expression of inflammation-related genes (i) in skin tissue; the frequencies of BrdU+ KCs (j). Scale bar: 100 μm. All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-way ANOVA with Bonferroni post-tests (a, f, h–j), two-tailed Student’s t tests (b), and two-way ANOVA (e) were performed. *P < 0.05; **P < 0.01; ***P < 0.001; ns not significant.
To examine whether the decreased activity of STAT3 in primary p38α-deficient KCs contributed to the less psoriasiform disease severity in p38αΔKC mice, we treated wild-type mice and p38αΔKC mice with IMQ to induce psoriasiform skin disease and then intradermally injected STAT3 activator Colivelin or control vehicle. As expected, activation of STAT3 signaling significantly enhanced psoriasiform skin disease severity in both wild-type mice and p38αΔKC mice, indicated by ear swelling, disease severity score, epidermal hyperplasia, and neutrophil infiltration (Fig. 4e−h). More importantly, the activation of STAT3 signaling fully restored the less psoriasiform disease severity in p38αΔKC mice compared with wild-type mice (Fig. 4e−h). The decreased mRNA levels of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, S100a7a, S100a8, S100a9, Krt6, Krt16, and Krt17 in skin tissues and reduced proliferation in KCs of p38αΔKC mice were also completely reached to the levels of wild-type mice (Fig. 4i, j). Collectively, p38α signaling in KCs promotes mouse psoriasiform skin disease in a STAT3-dependent manner.
Deletion of p38α in KCs protects mice from IL-23-induced psoriasiform skin disease
To examine whether the critical role of p38α signaling in KCs in promoting mouse psoriasiform skin disease was unique to IMQ stimulation, we performed an IL-23-induced psoriasiform mouse model32 and found that p38 activity was significantly elevated in KCs of IL-23-treated mice (Fig. 5a). Furthermore, we introduced IL-23 to wild-type mice and p38αΔKC mice and analyzed disease severity. Compared with IL-23-treated wild-type mice, IL-23-treated p38αΔKC mice had significantly less skin disease severity as indicated by ear swelling, disease severity score, epidermal hyperplasia, and neutrophil infiltration (Fig. 5b−e). In addition, the mRNA levels of inflammation-related genes, such as Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Krt6, Krt16, and Krt17, were also significantly decreased in IL-23-treated p38αΔKC mice compared with wild-type mice (Fig. 5f). However, Il6, Il17a, Il17f, Ifng, Il36a, Cxcl5, Ccl20, and Krt10 levels were comparable between wild-type mice and p38αΔKC mice upon IL-23 treatment (Fig. 5f). These results demonstrate that p38α signaling in KCs is also crucial for the regulation of IL-23-induced mouse psoriasiform skin disease.
a The activity of p38 in KCs of WT mice intradermally injected with IL-23 or PBS every other day for two times. b–f WT and p38αΔKC mice were intradermally injected with IL-23 every other day for four times (n = 6): changes in ear thickness (b); disease severity score (c); histopathological changes in skin sections (d); infiltration of neutrophils (e); and relative expression of inflammation-related genes (f) in skin tissue. Scale bar: 200 μm. All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-way ANOVA (b) and two-tailed Student’s t tests (c, e, f) were performed. *P < 0.05; **P < 0.01; ***P < 0.001; ns not significant.
p38α-STAT3 axis mediates IL-17 signaling in KCs
IL-17A plays an essential role in psoriasis pathogenesis, mainly through inducing the proliferation and secretion of inflammatory cytokines by KCs, further amplifying psoriasiform inflammation33. p38 activity in KCs was increased upon stimulation with IL-17A, which was associated with the increased phosphorylation of STAT3 (Fig. 6a and Supplementary Fig. 5b). However, upon deletion of p38α in KCs, the phosphorylation level of STAT3 was substantially reduced, without affecting the activities of JNK, ERK, p65 and Akt upon stimulation with IL-17A (Fig. 6a and Supplementary Fig. 5b). At the same line, IL-17A could largely induce KC proliferation, indicated by Edu+ cells, however, the percentage of Edu+ cells was significantly decreased in primary p38α-deficient KCs compared with primary wild-type KCs upon IL-17A treatment (Fig. 6b). We then explored whether certain psoriasis-related inflammatory cytokines in KCs would be affected by p38α signaling once stimulated with IL-17A. Our results showed that deletion of p38α in KCs significantly decreased the mRNA levels of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Krt6, Krt16, and Krt17 in primary KCs stimulated with IL-17A, but did not affect the mRNA level of Ccl20 (Fig. 6c). Notably, STAT3 activator largely increased the proliferation and expression of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Ccl20, Krt6, Krt10, Krt16, and Krt17 in primary KCs and abolished the differences in proliferation and psoriasis-related inflammatory cytokine production between primary wild-type and p38α-deficient KCs upon IL-17A treatment (Fig. 6b, c).
a The activities of STAT3, p38, JNK, ERK, p65, and Akt were determined in WT and p38αΔKC primary KCs stimulated with IL-17A for indicated times. The numbers below the lanes indicate the band intensity relative to total protein. b, c Primary KCs of WT and p38αΔKC mice were pretreated with or without STAT3 activator Colivelin followed with or without stimulation of IL-17A. IL-17A stimulation for 24 h to perform the Edu incorporation assay and calculate the percentages of Edu+ cells (b, n = 5). Scale bar: 100 μm. IL-17A stimulation for 5 h to analyze the production of inflammation-related genes (c, n = 4). d–g WT and p38αΔKC mice were intradermally injected with IL-17A (n = 6): changes in ear thickness (d); disease severity score (e); infiltration of neutrophils (f) and relative expression of inflammation-related genes (g) in skin tissue. All the assays were replicated three times with consistent results. Data represent mean ± SEM. Two-way ANOVA with Bonferroni post-tests (b, c), two-way ANOVA (d) and two-tailed Student’s t tests (e–g) were performed. *P < 0.05; **P < 0.01; ***P < 0.001; ns not significant.
To examine whether p38α signaling in KCs mediates the effector phase of IL-17-induced mouse psoriasiform inflammation in vivo, we intradermally injected IL-17A into the ear skin of wild-type mice and p38αΔKC mice to induce psoriasiform skin inflammation34. Upon IL-17A treatment, p38αΔKC mice had less ear swelling, disease severity score, and neutrophil infiltration than wild-type mice (Fig. 6d−f). Although the mRNA levels of Ccl20 and Krt10 were comparable between wild-type mice and p38αΔKC mice, the expression of Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Krt6, Krt16, and Krt17 in p38αΔKC mice was lower than that in wild-type mice (Fig. 6g). These results indicate that p38α deficiency in KCs significantly reduces the disease severity in the IL-17A-induced mouse psoriasiform disease. Taken together, p38α-STAT3 axis in KCs is important for amplifying the effector function of IL-17A during psoriasis development.
p38α-STAT3 axis in KCs is an important therapeutic target for the treatment of psoriasiform skin disease
IL-17A antagonist has been approved for psoriasis treatment since 20201. To further determinate whether the p38α-STAT3 axis is a good target during IL-17A antagonist treatment in psoriasis, we intraperitoneally injected IMQ-treated wild-type mice with the antibody against IL-17A. Blockade of IL-17A largely reduced ear swelling, disease severity score and neutrophil infiltration in IMQ-treated wild-type mice (Supplementary Fig. 6a−c). More importantly, blockade of IL-17A suppressed the phosphorylation level of p38 and STAT3 in KCs (Fig. 7a).
a WT mice topically treated with IMQ for six consecutive days were intraperitoneally administered with the antibody against IL-17A (anti-IL-17A) or control IgG 4 h after IMQ treatment and the activities of p38 and STAT3 in KCs were analyzed by Western blot. b–f WT and p38αΔKC mice topically treated with IMQ for six consecutive days were intradermally injected with STAT3 inhibitor S3I-201 or control vehicle at days 1, 3, and 5 (n = 6): changes in ear thickness (b), disease severity score (c); histopathological changes in skin sections (d); infiltration of neutrophils (e) and relative expression of inflammation-related genes (f) in skin tissue. Scale bar: 100 μm. All the assays were replicated two times with consistent results. Data represent mean ± SEM. Two-way ANOVA (b) and two-way ANOVA with Bonferroni post-tests (c, e, f) were performed. **P < 0.01; ***P < 0.001; ns not significant.
Considering that p38α-STAT3 axis mediated IL-17 signaling in KCs (Fig. 6) and blockade of IL-17 largely reduced the activities of p38α and STAT3 (Fig. 7a), we then assessed whether p38α-STAT3 axis could be a good therapeutic target for the treatment of psoriasis. We intradermally injected STAT3 inhibitor S3I-201 or control vehicle to IMQ-treated wild-type mice and p38αΔKC mice. The results showed that inhibition of STAT3 signaling largely alleviated ear swelling and disease severity of IMQ-treated mice (Fig. 7b, c). Furthermore, histological and flow cytometry analyses showed that inhibition of STAT3 signaling significantly reduced the epidermal hyperplasia and infiltration of neutrophils in skin tissue of IMQ-treated mice (Fig. 7d, e). Moreover, inhibition of STAT3 signaling also markedly decreased the relative expression of proinflammatory cytokines, chemokines, antimicrobial peptides and keratins, such as Tnfa, Il1a, Il1b, Cxcl1, Cxcl2, Ccl20, S100a7a, S100a8, Krt6, Krt16, and Krt17, in skin tissue of IMQ-treated mice (Fig. 7f). In addition, upon STAT3 inhibitor treatment, p38αΔKC mice exhibited similar psoriasiform skin disease severity as wild-type mice, including ear swelling, disease score, epidermal hyperplasia, and neutrophil infiltration (Fig. 7b−e). The mRNA levels of inflammation-related genes were also comparable between wild-type mice and p38αΔKC mice treated with STAT3 inhibitor (Fig. 7f).
Next, we evaluated whether inhibition of p38 activity can attenuate psoriasis. In our previous study, we intraperitoneally injected p38 inhibitor SB203580 into the psoriatic mice and found this treatment could ameliorate psoriasiform inflammation19. In the current study, we intradermally injected SB203580 or control vehicle to wild-type mice pretreated with IMQ and analyzed disease severity. The results showed that the ear swelling and disease severity score were significantly alleviated in SB203580-treated mice compared with vehicle-treated mice (Supplementary Fig. 7a, b). We further observed decreased epidermal hyperplasia and infiltration of neutrophils in skin tissue of SB203580-treated mice (Supplementary Fig. 7c, d). Moreover, p38 inhibitor SB203580 reduced the relative expression of multiple key psoriasis-related cytokines, such as Tnfa, Il1a, Il1b, Il17a, I17f, Cxcl1, Cxcl2, S100a7a, S100a8, S100a9, Krt6, Krt16, and Krt17, but had no effect on the mRNA levels of Il10, Tgfb1, or Ccl20 (Supplementary Fig. 7e). Collectively, these findings suggest that p38α-STAT3 axis could serve as a good target for the treatment of psoriasis.
Discussion
Although mounting evidence demonstrates an essential role of KCs in psoriasis pathogenesis, the underlying mechanisms by which KCs regulate the initiation and maintenance of skin inflammation remain incompletely understood. In this study, we identified the p38α-STAT3 axis as a key pathogenic factor in regulating the proliferation and inflammation-related cytokine production of KCs during psoriasis development. Selective deletion of p38α in KCs or inhibition of STAT3 signaling greatly alleviated the key features of disease severity. While p38α signaling in KCs did not affect the expression of IL-23 and IL-17, it substantially amplified the IL-23/IL-17 pathogenic axis in psoriasis. Our results thus establish a critical role of p38α-STAT3 axis in the pathogenesis of psoriasis.
Psoriasis is featured with KC hyperproliferation, abnormal differentiation and dysregulated DC-T cell interaction. The reduced expression of certain genes involved in excessive KC proliferation, such as Krt6, Krt16, and Krt17, in skin tissues, lower Ki-67 staining levels in epidermal cells and less BrdU positive KCs in IMQ-treated p38αΔKC mice reveal a critical role of p38α signaling in regulating KC proliferation. However, the comparable expression of certain genes regulating KC differentiation, such as Krt1, Krt10, and Krt14, between IMQ-treated wild-type mice and p38αΔKC mice indicates that p38α signaling might not be required for KC differentiation. Furthermore, p38α has no effect on KC apoptosis in psoriasis despite it participates in apoptosis in sunitinib-treated primary oral KCs35. In the current study, we show that during the initial phase of psoriasis, exogenous stimuli can activate p38-STAT3 axis in KCs to produce proinflammatory cytokines and chemokines, as well as damage-associated molecular patterns, which further promote the infiltration and activation of LCs and other immune cells. Moreover, exogenous stimuli can also directly activate p38 activity in LCs to produce IL-23 and IL-6, which promoting the secretion of IL-17 from T17 cells19. In the maintenance phase of psoriasis, IL-17 further activates p38-STAT3 axis in KCs to produce proinflammatory cytokines and chemokines, thereby amplifying the inflammatory response of psoriasis. Thus, p38α-mediated cross-talk between KCs and LCs generates the inflammatory and immune circuits responsible for the initiation, progression and persistence of the psoriasiform diseases.
The IL-23/IL-17 axis has been well studied in psoriasis pathogenesis and clinical application1,5,33. Biologics targeting IL-23, IL-17 and IL-17RA have been approved and widely used in the clinical treatment of psoriasis, which benefit most of psoriasis patients in the past decade1,36. Although the therapeutics have obtained excellent efficacy, there are still some unavoidable side effects, including nasopharyngitis, upper respiratory tract or systemic infections, injection-site reaction, and headache1,36. These side effects are largely due to the widespread expression of IL-17R in multiple cell types and the protective roles of IL-17 in other tissues and diseases. Therefore, it is necessary to develop drugs with higher specificity. Although IL-17 significantly influences phenotype determination in the IMQ-induced psoriasis model5, p38α signaling in KCs does not affect the expression of IL-23 and IL-17 family cytokines, as well as the differentiation and recruitment of T17 cells. However, it specifically mediates the downstream inflammatory signals of IL-23/IL-17 axis in KCs in a STAT3-dependent manner. Inhibition of STAT3 signaling could alleviate disease severity and decrease neutrophil and macrophage recruitment, as well as IL-17 expression. Thus, it will be very interesting to elucidate the direct targets of p38α in KCs during psoriasis pathogenesis in future study. Moreover, certain chemokines such as CXCL1 and CXCL2, which critically guide neutrophil and macrophage recruitment, are regulated by p38α-STAT3 axis in KCs. Published papers have shown that p38 MAPK in other cell types can also controls neutrophil trafficking in different mechanisms37,38,39,40,41,42. Whether p38-STAT3 axis in KCs will take advantage of these mechanisms to mediate the pathogenesis of psoriasis will need further in-depth study in the future. Notably, although Ccl20 is known as a factor upregulated by IL-17 and STAT3 in KCs43, p38α signaling does not affect the gene expression of Ccl20. It has been shown that Ccl20 promoter region contains AP-1 binding sites44 and AP-1 activity can promote Ccl20 production in human neonatal foreskin KCs45 and primary normal human epidermal KCs46. Considering that p38α deficiency can upregulate the phosphorylation of c-Jun and thereby enhancing the transcriptional activity of AP-1 binding site47, which might counteract the role of STAT3 in regulating the expression of Ccl20. All these data highlight a central role of the p38-STAT3 axis in KCs in the regulation of psoriasis pathogenesis and p38α-STAT3 axis in KCs might be as an effective therapeutic target to treat psoriasis.
Certain published papers have shown the activation of the epidermal p38 pathway by IMQ models or IL-17A is involved in psoriasis48,49,50. As the epidermal cells include many cell types such as KCs and immune cells, they might play different roles in psoriasis pathogenesis. Our previous study has demonstrated that p38α signaling in LCs, but not in dermal DCs or T cells, is critical for disease development19, highlighting to further define the specific cell types of p38α in the pathogenesis of psoriasis is important. Considering that KCs is the predominant cells in epidermis and the cells expressing K14 can more accurately represent KCs than epidermis, in the current study, we have used the genetic model of Mapk14flox/floxK14-Cre mice to better elucidate the cellular mechanism of p38α in psoriasis pathogenesis.
The activity of p38α is markedly increased in lesional psoriatic skin and animal models16,17,18,19. Inhibition of p38 can reduce the symptoms of psoriasis by either intraperitoneally injected p38 inhibitor prior to IMQ treatment or applied p38 inhibitor along with IMQ treatment23,51. To further examine whether p38 inhibitors would have a therapeutic effect on IMQ-induced psoriasis, we have intraperitoneally injected p38 inhibitor into the mice after the onset of diseases (3 days after IMQ treatment) and found that this treatment could alleviate the ongoing psoriasis development19. However, considering the potential liver toxicity caused by systemic application of SB203580, in the current study, we intradermally injection of lower doses of SB203580 into the mice after the onset of diseases (3 days after IMQ treatment) and found that this treatment can also achieve a good therapeutic effect, which is more in line with clinical application.
Until now, clinical application of p38 inhibitors is limited52. In addition to the liver toxicity, its cellular specificity is also a significant factor. The cell type-specific inflammatory function of p38α can coordinate pro- and anti-inflammatory gene expression in sodium dodecyl sulfate-induced chronic skin inflammation53.Considering that KCs are the main cell type in skin tissues and the roles of KC p38α signaling in promoting inflammatory response and KC hyperproliferation both in initiation phase and in maintenance phase of psoriasis, inhibiting of p38α signaling pathway in KCs is a promising new approach to prevent psoriasis aggravation.
Methods
Experimental animals
Mapk14flox mice have been described previously54,55. K14-Cre mice were kindly provided by Dr. Gang Ma (Shanghai Jiao Tong University, China)56. We purchased C57BL/6 mice from Shanghai SLAC Laboratory Animal Co., Ltd (Shanghai, China) and SPF Biotechnology Co., Ltd (Beijing, China). All mice were backcrossed to C57BL/6 background for at least 9 generations. Age- and sex-matched mice at 6 to 10 weeks of age were used for all experiments. Male and female were used in all experiments, as we have not observed sex difference in any of the measured endpoints. Wild-type or Cre+ littermate control mice were used as control. No adverse effects due to Cre expression itself were observed in these studies. All mice were bred and maintained in specific pathogen-free condition. This study was approved by the Experimental Animal Center of Guangdong Medical University and the Institutional Animal Care and Use Committee of Shanghai Jiao Tong University School of Medicine. We have complied with all relevant ethical regulations for animal use.
Psoriasis mouse model
IMQ-induced mouse psoriasiform skin disease model was indued by topically treating both sides of the ear of each mouse with 25 mg IMQ cream (5%) (3 M Pharmaceuticals or MedShine) daily for six consecutive days from day 0 to day 5. IL-23-induced experimental psoriasis model was established by intradermally injecting 500 ng IL-23 (eBioscience) to the ear of each mouse every other day on days 0, 2, 4, and 6. IL-17A-induced experimental psoriasis model was established by intradermally injecting 500 ng IL-17A (R&D) to the ear of each mouse daily for four consecutive days from day 0 to day 3. Ear thickness was measured daily by a micrometer. The severity of erythema, scaling, and thickening were independently scored as follows: 0 = none, 1 = slight, 2 = moderate, 3 = marked, and 4 = very marked, and their cumulative score served as the disease severity score (scale, 0 to 12). In some experiments, IMQ-treated mice were intradermally injected with STAT3 activator Colivelin (Selleck) at a dose of 0.1 mg/kg body weight or STAT3 inhibitor S3I-201 (Selleck) at a dose of 0.5 mg/kg body weight on days 1, 3 and 5. For pharmacological inhibition of p38, IMQ-treated mice were intradermally injected with p38 inhibitor SB203580 (Merck Calbiochem) at a dose of 30 μg/kg body weight on days 3-5. Liquid Colivelin dissolved in water, and liquid S3I-201 and liquid SB203580 dissolved in dimethyl sulfoxide (DMSO) were diluted with phosphate-buffered saline (PBS) for injection into mice. Control mice were injected with same volume of water or DMSO diluted with PBS on the same schedule. For IL-17A blockade, antibody against IL-17A (2 mg/kg body weight, Bio-X-Cell) or control IgG was diluted with PBS and intraperitoneally administered to mice 4 h after IMQ treatment.
Skin cell isolation
Skin cells were isolated as described previously with minor modification19. Briefly, mouse ears were collected from euthanized mice and divided into dorsal and ventral halves. After carefully removing cartilage and fat tissue, the ear tissue was spread on the surface of 0.5% trypsin (w/v) (Gibco) and incubated at 37°C for 45 min for separating the epidermal and dermal tissues. The separated epidermal and dermal tissues were cut into pieces and digested respectively in 1 mg/ml and 1.5 mg/ml type IV Collagenase (Gibco) for 90 min, respectively. Then the cells were thoroughly mixed with a pipette and filtered through a nylon membrane to obtain single-cell suspension.
Primary keratinocyte (KC) culture and analysis
Neonatal mice were euthanized for isolating the entire skin to be divided into four parts and suspended on 1 mg/ml Dispase II (Sigma-Aldrich) at 4 °C overnight in dark. Gently the epidermis was separated and placed on 0.05% Tryspin-EDTA (w/v) (Gibco) at 37 °C for 10 min. Then the cells were mix thoroughly and filtered through a 40 μm cell strainer. After centrifugation, the cells were resuspended with 154CF medium (Gibco) containing Human Keratinocyte Growth Supplement (Gibco) and cultured in the culture plate pretreated with rat tail collagen. The primary KCs were stimulated with 10 μM R848 (Invivogen) or 100 ng/ml IL-17A (R&D system) for indicated time points for protein analysis and 5 h for mRNA analysis. In Western blot analysis, the band intensity of phosphorylated protein relative to total protein was calculated by ImageJ. In 5-ethynyl-2’-deoxyuridine (Edu) incorporation assay, primary KCs were stimulated with 10 μM R848 (Invivogen) or 100 ng/ml IL-17A (R&D system) for 24 h and subjected to Edu at last 2 h with further staining by EdU Cell Proliferation Kit (Beyotime) according to the manufacturer’s instructions. Cells were observed under a fluorescence microscope and Edu+ positive cells were counted.
Flow cytometry and cell purification
For analysis of surface markers, cells were stained with surface marker antibodies in PBS with 2% fetal bovine serum for 30 min on ice. For intracellular cytokine staining (ICS), cells were pre-stimulated with 1 μM ionomycin (Sigma-Aldrich) and 50 ng/ml phorbol 12-myristate 13-acetate (Sigma-Aldrich) in the presence of GolgiStop (BD Biosciences) and GolgiPlug (BD Biosciences) for 5 h and ICS was performed with Intracellular Fixation & Permeabilization Buffer Set (eBioscience). Intracellular phosphorylation antibody staining was performed with Lyse/Fix Buffer and Perm Buffer III (BD Biosciences). Staining of transcriptional factor, active caspase-3 and BrdU was performed with Foxp3/Transcription Factor Staining Buffer Set (eBioscience), APC BrdU Flow Kit (BD Biosciences, Cat No. 552598, used at 1 μl/test), and PE Active Caspase-3 Apoptosis Kit (BD Biosciences, Cat No. 550914, used at 10 μl/test), respectively. Antibodies used in this study include: Fixable Viability Dye (FVD, eBioscience, Cat No. 65-0865-18, 1:1000), anti-CD45 (clone: 30-F11, eBioscience, Cat No. 48-0451-82, used at 1 μg/ml; BD Biosciences, Cat No. 564279, used at 0.5 μg/ml), anti-EpCAM (clone: G8.8, eBioscience, Cat No. 12-5791-82 or 17-5791-82, used at 0.5 μg/ml), anti-CD11b (clone: M1/70, eBioscience, Cat No. 48-0112-82, used at 1 μg/ml; BD Biosciences, Cat No. 563015, used at 0.5 μg/ml), anti-F4/80 (clone: BM8, eBioscience, Cat No. 17-4801-82, used at 0.5 μg/ml), anti-γδTCR (clone: eBioGL3, eBioscience, Cat No. 17-5711-82 or 25-5711-82, used at 0.5 μg/ml), anti-TCRβ (clone: H57-597, eBioscience, Cat No. 12-5961-82 or 45-5961-82, used at 0.5 μg/ml), anti-CD4 (clone: RM4-5, eBioscience, Cat No. 48-0042-82, used at 1 μg/ml), anti-CD8α (clone: 53-6.7, BD Biosciences, Cat No. 563152, used at 0.5 μg/ml), anti-CD11c (clone: N418, eBioscience, Cat No. 25-0114-82, used at 0.5 μg/ml), anti-MHC II (clone: M5/114.15.2, eBioscience, Cat No. 11-5321-85, used at 1 μg/ml), anti-CD40 (clone: 1C10, eBioscience, Cat No. 17-0401-81, used at 0.5 μg/ml), anti-CD80 (clone: 16-10A1, BD Biosciences, Cat No. 740888, used at 0.5 μg/ml), anti-CD86 (clone: GL1, eBioscience, Cat No. 48-0862-82, used at 1 μg/ml), anti-CD44 (clone: IM7, eBioscience, Cat No. 17-0441-82, used at 0.5 μg/ml), anti-CD62L (clone: MEL-14, eBioscience, Cat No. 12-0621-82, used at 0.5 μg/ml), anti-IL-17 (clone: eBio17B7, eBioscience, Cat No. 25-7177-82, used at 2 μg/ml), anti-IFNγ (clone: XMG1.2e, eBioscience, Cat No. 11-7311-82, used at 2 μg/ml), anti-IL-4 (clone: 11B11, eBioscience, Cat No. 12-7041-82, used at 2 μg/ml), anti-Foxps3 (clone: FJK-165, eBioscience, Cat No. 12-5773-82, used at 2 μg/ml), anti-Gr1 (clone: 1A8, BD Biosciences, Cat No. 560602, used at 0.5 μg/ml); anti-CD64 (clone: X54-5/7.1, Biolegend, Cat No. 139309, used at 0.5 μg/ml); anti-phospho-p38 (clone: 28B10, CST, Cat No. 4551, 1:50). Flow cytometry was performed with BD LSR Fortessa X-20 and analyzed with FlowJo-v10. FVD− cells were gated as live cells. CD45−EpCAM+ cells of skin cells were gated as KCs57 (Supplementary Fig. 1a). KCs of skin tissue were sorted with Beckman MoFlo XDP.
Hematoxylin and eosin, immunohistochemistry, and immunofluorescence staining
Skin issues were fixed in formalin, embedded in paraffin, and cut into 6 μm thickness longitudinal sections of for histological studies. The mouse skin paraffin sections were stained with hematoxylin and eosin (Beyotime) for hematoxylin and eosin assay, and anti-Ki-67 (clone: Sp6, Abcam, Cat No. ab1667, 1:200) for immunohistochemistry assay according to standard procedures. The histological images were taken with Leica ICC50 W Microscope. For IF analysis, skin tissue was frozen and embedded in Neg-50 (Epredia). The mouse skin frozen sections were prepared as 8 μm thickness and stained with anti-phospho (p)-p38 (clone: D3F9, CST, Cat No. 4511, 1:1000) and anti-p-STAT3 (clone: D3A7, CST, Cat No. 9145, 1:200) according to standard procedures. Samples were observed using a Leica TCS SP8 Laser Confocal Microscope.
Protein and RNA analyses
Skin tissue and cells were lysed and quantified as described previously. Western blot analysis was performed with the following primary antibodies: p38 (clone: D13E1, CST, Cat No. 8690, 1:1000), p-p38 (clone: D3F9, CST, Cat No. 4511, 1:1000), STAT3 (clone: D3Z2G, CST, Cat No. 12640, 1:1000), p-STAT3 (clone: D3A7, CST, Cat No. 9145, 1:2000), JNK (clone: 56G8, CST, Cat No. 9258, 1:1000), p-JNK (clone: 81E11, CST, Cat No. 4668, 1:1000), ERK (clone:137F5, CST, Cat No. 4695, 1:1000), p-ERK (clone: D13.14.4E, CST, Cat No. 4370, 1:2000), p65 (clone: D14E12, CST, Cat No. 8242, 1:1000), p-p65 (clone: 93H1, CST, Cat No. 3033, 1:1000), Akt (clone: 11E7, CST, Cat No. 4685, 1:1000), p-Akt (clone: D9E, CST, Cat No. 4060, 1:2000), GAPDH (clone: 14C10, CST, Cat No. 2118, 1:1000), and β-Tubulin (clone: 9F3, CST, Cat No. 2128, 1:1000). The relative expression in Western blot analysis was calculated with IntDen in Image J. RNA isolation and reverse transcription were performed as described previously19. Quantitative real-time PCR (qRT-PCR) analysis was performed by using Hieff qPCR SYBR Green Master Mix (Yeasen) in a QuantStudio 5 Real time fluorescence quantitative PCR system (Applied Biosystems) with the primers listed in Supplementary Table 1.
Statistics and reproducibility
Data were analyzed with Graph Prism 8 and presented as mean ± SEM from at least three repeats. Two-way analysis of variance (ANOVA) with Bonferroni post-tests was used for multiple comparisons, and two-tailed Student’s t test was used when two conditions were compared. The number of experimental and technical replicates are specified in the figure legends. P values were indicated and P < 0.05 was considered significant. *P < 0.05; **P < 0.01; ***P < 0.001; ns, not significant. “n” indicates biological replicates for in vitro experiments and number of mice for in vivo studies.
Data availability
All data are available in the paper and its supplementary information files. All source data in this study are available upon reasonable request and the source data for graphs in figures are provided in Supplementary Data file. Uncropped blots are shown in Supplementary Fig. 8.
References
Ghoreschi, K., Balato, A., Enerback, C. & Sabat, R. Therapeutics targeting the IL-23 and IL-17 pathway in psoriasis. Lancet 397, 754–766 (2021).
Zhou, X., Chen, Y., Cui, L., Shi, Y. & Guo, C. Advances in the pathogenesis of psoriasis: from keratinocyte perspective. Cell Death Dis. 13, 81 (2022).
Lowes, M. A., Suarez-Farinas, M. & Krueger, J. G. Immunology of psoriasis. Annu. Rev. Immunol. 32, 227–255 (2014).
Dainichi, T. et al. The epithelial immune microenvironment (EIME) in atopic dermatitis and psoriasis. Nat. Immunol. 19, 1286–1298 (2018).
van der Fits, L. et al. Imiquimod-induced psoriasis-like skin inflammation in mice is mediated via the IL-23/IL-17 axis. J. Immunol. 182, 5836–5845 (2009).
Zheng, Y. et al. Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature 445, 648–651 (2007).
Albanesi, C., Madonna, S., Gisondi, P. & Girolomoni, G. The interplay between keratinocytes and immune cells in the pathogenesis of psoriasis. Front. Immunol. 9, 1549 (2018).
Trompette, A. & Ubags, N. D. Skin barrier immunology from early life to adulthood. Mucosal Immunol. 16, 194–207 (2023).
Lande, R. et al. Plasmacytoid dendritic cells sense self-DNA coupled with antimicrobial peptide. Nature 449, 564–569 (2007).
Ganguly, D. et al. Self-RNA-antimicrobial peptide complexes activate human dendritic cells through TLR7 and TLR8. J. Exp. Med. 206, 1983–1994 (2009).
Hawkes, J. E., Chan, T. C. & Krueger, J. G. Psoriasis pathogenesis and the development of novel targeted immune therapies. J. Allergy Clin. Immunol. 140, 645–653 (2017).
Morizane, S. & Gallo, R. L. Antimicrobial peptides in the pathogenesis of psoriasis. J. Dermatol. 39, 225–230 (2012).
Greb, J. E. et al. Psoriasis. Nat. Rev. Dis. Prim. 2, 16082 (2016).
Arthur, J. S. & Ley, S. C. Mitogen-activated protein kinases in innate immunity. Nat. Rev. Immunol. 13, 679–692 (2013).
Mavropoulos, A., Rigopoulou, E. I., Liaskos, C., Bogdanos, D. P. & Sakkas, L. I. The role of p38 MAPK in the aetiopathogenesis of psoriasis and psoriatic arthritis. Clin. Dev. Immunol. 2013, 569751 (2013).
Johansen, C. et al. The mitogen-activated protein kinases p38 and ERK1/2 are increased in lesional psoriatic skin. Br. J. Dermatol. 152, 37–42 (2005).
Yu, X. J. et al. Expression and localization of the activated mitogen-activated protein kinase in lesional psoriatic skin. Exp. Mol. Pathol. 83, 413–418 (2007).
Soegaard-Madsen, L., Johansen, C., Iversen, L. & Kragballe, K. Adalimumab therapy rapidly inhibits p38 mitogen-activated protein kinase activity in lesional psoriatic skin preceding clinical improvement. Br. J. Dermatol 162, 1216–1223 (2010).
Zheng, T. et al. p38alpha signaling in Langerhans cells promotes the development of IL-17-producing T cells and psoriasiform skin inflammation. Sci. Signal. 11, eaao1685 (2018).
Zhao, W. et al. MAPK phosphatase-1 deficiency exacerbates the severity of imiquimod-induced psoriasiform skin disease. Front. Immunol. 9, 569 (2018).
Kjellerup, R. B., Johansen, C., Kragballe, K. & Iversen, L. The expression of dual-specificity phosphatase 1 mRNA is downregulated in lesional psoriatic skin. Br. J. Dermatol. 168, 339–345 (2013).
Mihara, K., Elliott, G. R., Boots, A. M. & Nelissen, R. L. Inhibition of p38 kinase suppresses the development of psoriasis-like lesions in a human skin transplant model of psoriasis. Br. J. Dermatol. 167, 455–457 (2012).
Sakurai, K. et al. Cutaneous p38 mitogen-activated protein kinase activation triggers psoriatic dermatitis. J. Allergy Clin. Immunol. 144, 1036–1049 (2019).
Sumer, C., Boz Er, A. B. & Dincer, T. Keratin 14 is a novel interaction partner of keratinocyte differentiation regulator: receptor-interacting protein kinase 4. Turk. J. Biol. 43, 225–234 (2019).
Tortola, L. et al. Psoriasiform dermatitis is driven by IL-36-mediated DC-keratinocyte crosstalk. J. Clin. Invest. 122, 3965–3976 (2012).
Sugiura, K. Role of interleukin 36 in generalised pustular psoriasis and beyond. Dermatol. Ther. (Heidelb.) 12, 315–328 (2022).
Watanabe, H. et al. Functional characterization of IL-17F as a selective neutrophil attractant in psoriasis. J. Invest. Dermatol. 129, 650–656 (2009).
Johnston, A. et al. Keratinocyte overexpression of IL-17C promotes psoriasiform skin inflammation. J. Immunol. 190, 2252–2262 (2013).
Senra, L. et al. Keratinocyte-derived IL-17E contributes to inflammation in psoriasis. J. Invest. Dermatol. 136, 1970–1980 (2016).
Ni, X. et al. IL-17D-induced inhibition of DDX5 expression in keratinocytes amplifies IL-36R-mediated skin inflammation. Nat. Immunol. 23, 1577–1587 (2022).
Kastelan, M., Prpic-Massari, L. & Brajac, I. Apoptosis in psoriasis. Acta Dermatovenerol. Croat. 17, 182–186 (2009).
Singh, T. P., Zhang, H. H., Hwang, S. T. & Farber, J. M. IL-23- and imiquimod-induced models of experimental psoriasis in mice. Curr. Protoc. Immunol. 125, e71 (2019).
Martin, D. A. et al. The emerging role of IL-17 in the pathogenesis of psoriasis: preclinical and clinical findings. J. Invest. Dermatol. 133, 17–26 (2013).
Veras, F. P. et al. Pyruvate kinase M2 mediates IL-17 signaling in keratinocytes driving psoriatic skin inflammation. Cell Rep. 41, 111897 (2022).
Fukada, S. et al. Sunitinib promotes apoptosis via p38 MAPK activation and STAT3 downregulation in oral keratinocytes. Oral Dis. 30, 639–649 (2022).
Kolli, S. S., Kepley, A. L., Cline, A. & Feldman, S. R. A safety review of recent advancements in the treatment of psoriasis: analysis of clinical trial safety data. Expert Opin. Drug Saf. 18, 523–536 (2019).
Smolen, J. E. et al. L-selectin signaling of neutrophil adhesion and degranulation involves p38 mitogen-activated protein kinase. J. Biol. Chem. 275, 15876–15884 (2000).
Tandon, R., Sha’afi, R. I. & Thrall, R. S. Neutrophil beta2-integrin upregulation is blocked by a p38 MAP kinase inhibitor. Biochem. Biophys. Res. Commun. 270, 858–862 (2000).
Yan, W. et al. Role of p38 MAPK in ICAM-1 expression of vascular endothelial cells induced by lipopolysaccharide. Shock 17, 433–438 (2002).
Hidalgo, A., Peired, A. J., Wild, M., Vestweber, D. & Frenette, P. S. Complete identification of E-selectin ligands on neutrophils reveals distinct functions of PSGL-1, ESL-1, and CD44. Immunity 26, 477–489 (2007).
Liu, X. et al. Bidirectional regulation of neutrophil migration by mitogen-activated protein kinases. Nat. Immunol. 13, 457–464 (2012).
Molinar-Inglis, O. et al. Phosphoproteomic analysis of thrombin- and p38 MAPK-regulated signaling networks in endothelial cells. J. Biol. Chem. 298, 101801 (2022).
Bae, H. C. et al. RIP4 upregulates CCL20 expression through STAT3 signalling in cultured keratinocytes. Exp. Dermatol. 27, 1126–1133 (2018).
Zhao, L., Xia, J., Wang, X. & Xu, F. Transcriptional regulation of CCL20 expression. Microbes Infect. 16, 864–870 (2014).
Kanda, N. et al. Prolactin enhances basal and IL-17-induced CCL20 production by human keratinocytes. Eur. J. Immunol. 39, 996–1006 (2009).
Li, H. et al. Cyr61/CCN1 induces CCL20 production by keratinocyte via activating p38 and JNK/AP-1 pathway in psoriasis. J. Dermatol. Sci. 88, 46–56 (2017).
Zheng, T. et al. Protein kinase p38alpha signaling in dendritic cells regulates colon inflammation and tumorigenesis. Proc. Natl Acad. Sci. USA 115, E12313–E12322 (2018).
Kanemaru, K. et al. Phospholipase Cdelta1 regulates p38 MAPK activity and skin barrier integrity. Cell Death Differ. 24, 1079–1090 (2017).
Mose, M., Kang, Z., Raaby, L., Iversen, L. & Johansen, C. TNFalpha- and IL-17A-mediated S100A8 expression is regulated by p38 MAPK. Exp. Dermatol. 22, 476–481 (2013).
Johansen, C., Bertelsen, T., Ljungberg, C., Mose, M. & Iversen, L. Characterization of TNF-alpha- and IL-17A-mediated synergistic induction of DEFB4 gene expression in human keratinocytes through IkappaBzeta. J. Invest. Dermatol. 136, 1608–1616 (2016).
Lee, J. H. et al. NJK14047 inhibition of p38 MAPK ameliorates inflammatory immune diseases by suppressing T cell differentiation. Int. Immunopharmacol. 130, 111800 (2024).
Schindler, J. F., Monahan, J. B. & Smith, W. G. p38 pathway kinases as anti-inflammatory drug targets. J. Dent. Res. 86, 800–811 (2007).
Kim, C. et al. The kinase p38 alpha serves cell type-specific inflammatory functions in skin injury and coordinates pro- and anti-inflammatory gene expression. Nat. Immunol. 9, 1019–1027 (2008).
Nishida, K. et al. p38alpha mitogen-activated protein kinase plays a critical role in cardiomyocyte survival but not in cardiac hypertrophic growth in response to pressure overload. Mol. Cell. Biol. 24, 10611–10620 (2004).
Huang, G. et al. Signaling via the kinase p38alpha programs dendritic cells to drive TH17 differentiation and autoimmune inflammation. Nat. Immunol. 13, 152–161 (2012).
Huang, S. et al. Involvement of epithelial Wntless in the regulation of postnatal hair follicle morphogenesis. Arch. Dermatol. Res. 307, 835–839 (2015).
Sakamoto, K., Goel, S., Funakoshi, A., Honda, T. & Nagao, K. Flow cytometry analysis of the subpopulations of mouse keratinocytes and skin immune cells. STAR Protoc. 3, 101052 (2022).
Acknowledgements
The authors would like to thank Dr. G. Ma (Shanghai Jiao Tong University, China) for kindly providing the K14-Cre mice. This work was supported by National Natural Science Foundation of China and Guangdong Basic and Applied Basic Research Foundation, under grant no 82001702 (T.Z.), 32341004 (G.H.), 82371758 (G.H.), 31670897 (G.H.), 81971329 (X.L.), 82200821 (M.Y.), 2021B1515130004 (G.H.), 2022A1515140062 (T.Z.), 2021B1515140021 (Y.W.), 2022A1515140075 (S.O.), 2021A1515011045 (S.O.), and 2023A1515012838 (M.Y.).
Author information
Authors and Affiliations
Contributions
T.Z. performed experiments, analyzed the data, prepared figures, and drafted the manuscript. J.D., J.W., S.X., H.H., J.S., L.Z., H.C., and J.L. performed experiments. Y.W., S.O., and M.Y. contributed to data analysis and manuscript revising. K.O. provided mouse models. X.L. provided reagents. G.H. designed experiments, analyzed the data, revised the manuscript, and provided overall direction. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks John Lukens, Scott Simon and the other, anonymous, reviewer for their contribution to the peer review of this work. Primary Handling Editor:Christina Karlsson Rosenthal. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zheng, T., Deng, J., Wen, J. et al. p38α deficiency ameliorates psoriasis development by downregulating STAT3-mediated keratinocyte proliferation and cytokine production. Commun Biol 7, 999 (2024). https://doi.org/10.1038/s42003-024-06700-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s42003-024-06700-w
- Springer Nature Limited