Abstract
This study aimed to investigate the correlation between ossific nucleus volume and avascular necrosis (AVN) in pediatric patients diagnosed with developmental dysplasia of the hip (DDH). Analyzing 211 cases, including 119 open reduction (OR) and 92 closed reduction (CR) procedures, we quantified ossific nucleus volume using magnetic resonance imaging (MRI). Categorizing the OR group based on ossific nucleus volume revealed no statistically significant difference in AVN incidence. Similarly, in the CR cohort, there was no significant discrepancy in AVN occurrence between subgroups with or without the ossific nucleus. Logistic regression in CR identified the international hip dysplasia institute (IHDI) grade as a significant AVN risk factor (p = 0.007). IHDI grades 3 and 4 exhibited a 6.94 times higher likelihood of AVN compared to grades 1 and 2. Across CR and OR, neither initial age nor ossific nucleus volume emerged as AVN risk factors. In conclusion, ossific nucleus volume does not pose a risk for AVN in DDH children undergoing CR or OR, emphasizing the clinical significance of IHDI grading in predicting AVN risk during CR and the importance of early intervention to prevent treatment delays.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Developmental dysplasia of the hip (DDH) refers to the morphological and positional abnormalities between the proximal femur and the acetabulum caused by various factors during the developmental process1. DDH may result in chronic pain, deformity, and impaired mobility in affected children, progressing to early-onset degenerative joint disease and ultimately leading to disability. Avascular necrosis (AVN) of the femoral head persists as a consequential complication following DDH treatments, exerting a substantial impact on the functional aspects of the hip joint2,3,4.
The ossific nucleus size of the femoral head has long been a focal point in DDH patients due to its close association with normal femoral head development. Some scholars believe that the appearance of the ossific nucleus of the femoral head can enhance its mechanical strength, thereby reducing the probability of postoperative AVN5,6,7. Conversely, other studies argue that the appearance of the ossific nucleus might not diminish the AVN incidence8,9,10.
Current research exhibits two main deficiencies. Firstly, most studies concentrate solely on the link between the presence of the ossific nucleus and AVN occurrence after closed reduction (CR), neglecting investigations on open reduction (OR). Secondly, existing studies frequently categorize the ossific nucleus based on its presence or absence, lacking precise measurements of its size. Consequently, this study aims to utilize preoperative magnetic resonance imaging (MRI) for precise measurements of the ossific nucleus, including the left and right diameters, as well as the anterior, posterior, upper, and lower diameters in the coronal and axial planes. The volume of the ossific nucleus will be calculated, allowing exploration of the relationship between its size and the occurrence of AVN after both CR and OR. This research aims to furnish more comprehensive information for the treatment of DDH patients and offer additional decision support for surgeons and medical teams in mitigating the risk of postoperative complications.
Material and methods
Study population and data collection
This study adhered to the principles of the Helsinki Declaration and obtained approval from the Ethics Committee of Honghui Hospital, Xi’an Jiaotong University (Approval No: 202205005). Informed consent was obtained from the parents/guardians of all participants. We included a total of 211 patients treated between May 2015 and July 2020 in this study. Among them, 119 patients underwent OR, 42 patients underwent OR combined with Salter pelvic osteotomy, and 77 patients underwent OR combined with Salter pelvic osteotomy and femoral shortening osteotomy. Additionally, 92 patients received CR treatment. Inclusion criteria were as follows: (1) DDH diagnosis confirmed by a pediatric orthopedic surgeon; (2) unilateral involvement; (3) age between 6 and 36 months; (4) preoperative MRI examination with complete imaging data; (5) follow-up of at least 2 years postoperatively; (6) obtained informed consent from both the child and legal guardian. The exclusion criteria were: (1) bilateral DDH; (2) exclude cases with cerebral palsy, multiple congenital joint contractures, spina bifida, tethered spinal cord syndrome, or other musculoskeletal disorders; (3) follow-up duration should be no less than 24 months; (4) cases lacking complete clinical and imaging data.
Treatment methods
CR: For children aged 6–18 months, CR is attempted as the initial approach. Intraoperatively, the adequacy of reduction is assessed based on joint imaging. If the adductor muscles are tense and affect reduction, adductor tenotomy is performed. After reduction, external rotation plaster is applied for 3 months to maintain the reduction, with a change every 6–7 weeks. After plaster removal, the patient wears an external rotation orthosis for an additional 3 months.
OR combined with pelvic osteotomy: for children aged 18 months and older who cannot achieve a stable reduction status through CR and have poor acetabular coverage, OR combined with pelvic osteotomy is performed.
OR combined with pelvic osteotomy and femoral shortening osteotomy: for patients with difficulty in femoral head reduction after OR and increased pressure on the femoral head after reduction, a combination of femoral shortening osteotomy is usually required to alleviate the pressure between the femoral head and the acetabulum, preventing the long-term occurrence of AVN.
Radiological evaluation
All patients underwent preoperative pelvic anteroposterior, external rotation internal rotation X-ray, frog-leg lateral X-ray, and bilateral hip joint MRI examinations. The selection of an appropriate treatment strategy was based on a comprehensive evaluation of the children’s imaging findings.
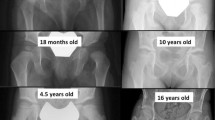
Measurement of ossific nucleus volume: measurement of the upper and lower diameters of the ossific nucleus: on coronal MRI images, the level with the maximum diameter of the ossific nucleus is selected (Fig. 1). Two lines parallel to the proximal femoral growth plate are drawn, tangential to the inner and outer boundaries of the ossific nucleus. The vertical distance between these two lines represents the upper and lower diameters of the ossific nucleus. Measurement of the anterior and posterior diameters of the ossific nucleus: on axial MRI images, the level with the maximum diameter of the ossific nucleus is selected. Two parallel lines tangential to the ossific nucleus are drawn. The longest distance between these two parallel lines is taken as the anterior and posterior diameters of the ossific nucleus. Measurement of the left and right diameters of the ossific nucleus: on axial MRI images, the level with the maximum diameter of the ossific nucleus is selected. Two parallel lines tangential to the ossific nucleus are drawn. The shortest distance between these two parallel lines is taken as the left and right diameters of the ossific nucleus.
Measurement of the ossific nucleus on different levels in preoperative MRI (a) measurement of the upper and lower diameters of the ossific nucleus: two perpendicular lines are drawn with the growth plate as a reference. The distance “A” between these two lines represents the upper and lower diameter of the ossific nucleus. (b) Measurement of the anterior and posterior diameter of the ossific nucleus: Two tangent lines to the ossific nucleus are drawn parallel to each other. The maximum distance between these two lines is taken as the anterior and posterior diameter “B” of the ossific nucleus. (c) Measurement of the left and right diameter of the ossific nucleus: Two tangent lines to the ossific nucleus are drawn parallel to each other. The minimum distance between these two lines is taken as the left and right diameter “C” of the ossific nucleus.
Calculation of the volume of the ossified nucleus: The ossific nucleus is approximated as an ellipsoid, and the volume is estimated using the ellipsoid volume formula: 4π * (a b c *1/2)/3 (where a, b, c represent half of the anterior–posterior diameter, left–right diameter and upper-lower diameter, and left–right diameter of the ossific nucleus, respectively). The volume of the ossific nucleus is calculated separately for both sides.
Assessment of AVN of the femoral head: In the X-rays of the last follow-up, the occurrence of AVN in the femoral head is determined based on anteroposterior pelvic X-rays and hip joint external rotation/internal rotation X-rays. The initial evaluation of femoral head osteonecrosis was conducted by two physicians. In cases of disagreement regarding the staging of AVN, the assessment was further discussed with two additional highly qualified orthopedic specialists. The Kalamchi–MacEwen classification method is used to grade AVN.
Statistical analysis
Statistical analysis was conducted using SPSS 17.0 software (SPSS Inc., Chicago, Illinois, USA). The data are grouped based on the ratio of the ossific nucleus between the affected and healthy sides. Normality tests are conducted, and if the data meet the criteria for a normal distribution, an independent samples t-test is used for the comparison of quantitative data between the two groups. For categorical data, chi-square tests and rank-sum tests are employed. When the data deviate from a normal distribution, non-parametric tests are employed to compare groups. Logistic regression analysis is conducted to explore the correlation between the volume of the ossific nucleus and the occurrence of AVN after surgery. A significance level of p < 0.05 is considered statistically significant.
Results
Radiographic measurements showed excellent interobserver reliability for the left and right diameter of the affected ossific nucleus (intraclass correlation coefficient (ICC) = 0.914), the upper and lower of the affected ossific nucleus (ICC) = 0.864, the anterior and posterior diameter of the affected ossific nucleus (ICC) = 0.939, the left and right diameter of the healthy ossific nucleus (ICC) = 0.933, the upper and lower of the healthy ossific nucleus (ICC) = 0.870, the anterior and posterior diameter of the healthy ossific nucleus (ICC) = 0.981.
The study comprised 211 pediatric patients diagnosed with unilateral DDH. Among them, 119 patients underwent OR, 42 patients underwent hip joint OR along with Salter pelvic osteotomy, and 77 patients underwent hip joint OR combined with Salter pelvic osteotomy and femoral shortening osteotomy. Of the total cases, 24 patients were diagnosed with AVN (Table 1).
Based on the ratio of the ossific nucleus on the affected side to the contralateral side, patients undergoing OR were divided into two groups: Group 1 with a ratio ≤ 0.15, and Group 2 with a ratio > 0.15. The results indicated that there was no statistically significant difference in the occurrence of AVN between the two groups after surgery (Table 2).
The research results indicate that age, IHDI grade, and the size of the ossific nucleus are not risk factors for the occurrence of AVN after OR (Table 3).
Ninety-two patients underwent CR treatment, comprising eight males and 84 females, with 60 cases on the left side and 32 on the right side. The average age was 10.97 ± 3.55 months. Postoperatively, during follow-up, 15 cases experienced AVN (Table 4).
Patients undergoing CR treatment were divided into two groups: Group 1 consisted of patients without an ossific nucleus, and Group 2 included patients with the presence of the ossific nucleus. The study revealed a significant age difference between the two groups (p < 0.001), while the incidence of AVN exhibited no statistical significance (Table 5).
The results indicate that the IHDI classification is a risk factor for the occurrence of AVN after CR (p = 0.007). The probability of AVN occurrence in IHDI grades 3 and 4 is 6.94 times higher than in IHDI grades 1 and 2. However, the volume of the ossific nucleus in patients is not a risk factor for the occurrence of AVN. (Table 6).
Discussion
This study indicates that, in patients undergoing CR treatment, the initial dislocation degree is a risk factor for the occurrence of AVN postoperatively, while the age at treatment initiation is not a risk factor for AVN. Additionally, regardless of whether OR or CR is performed, this study finds no correlation between the size of the ossific nucleus on the affected side and the occurrence of AVN. Our results align with previous studies, but our research uniquely includes measurements of the three-dimensional size of the ossific nucleus using MRI images. For the first time, we measured the left–right diameter, superior–inferior diameter, and anterior–posterior diameter of the ossific nucleus and calculated its approximate volume using the formula for the volume of an ellipsoid. Moreover, this study incorporated patients undergoing both open and closed procedures, exploring the correlation between the ossific nucleus size and subsequent AVN.
Currently, there is a debate surrounding the correlation between the age at the initiation of treatment and the incidence of AVN following CR. Some scholars believe that the probability of AVN occurring after CR increases with age11,12,13. On the contrary, some researchers suggest that the occurrence of postoperative AVN decreases as the age at treatment initiation increases14,15. They suggested that vessels in the proximal femur increase with age16. This study aligns with the majority of research indicating that the initial treatment age is not a risk factor for AVN after CR4,14,17,18,19. Some scholars’ research indicates that the initial higher dislocation grade is a significant risk factor for AVN, which is consistent with this study findings11,16,20. Our research reveals that the probability of AVN occurrence is 6.94 times higher in patients with IHDI 3 or 4 compared to those with IHDI classification 1 or 2.
The association between the presence of the ossific nucleus and the occurrence of AVN remains a matter of debate. Some authors propose a protective role of the ossific nucleus against AVN5,21,22,23. This potential protection is attributed to the vulnerability of the microcirculation supplied by terminal arteries to the cartilaginous epiphysis of the femoral head. The emergence of the secondary ossification center brings changes to the blood supply to the femoral head. The development of the ossific nucleus establishes an effective collateral circulation, potentially augmenting the femoral head's resistance to ischemic injury. Nevertheless, the majority of studies suggest that the presence of the ossific nucleus does not mitigate the incidence of AVN10,11,24,25.
Some previous studies have assessed the size of the ossific nucleus through radiographic imaging. Zhen et al.26 measured the diameter of the ossific nucleus and used the ratio of the diameter of the affected side's ossific nucleus to the diameter of the femoral neck as an indicator of ossific nucleus size. Wu et al.16 measured the diameter and height of the ossific nucleus using MRI and used the percentage reduction of the affected side’s diameter and height relative to the healthy side as an indicator of the size of the affected side’s ossific nucleus. However, their study solely assessed the size of the ossific nucleus in two-dimensional planes, overlooking the spatial volume of the ossific nucleus. Therefore, in this study, we measured the anterior–posterior diameter of the ossific nucleus on the MRI horizontal plane and used the formula for the volume of an ellipsoid to calculate the volume of the ossific nucleus. This study is the first to calculate the spatial volume of the ossific nucleus, using the ratio of the affected side’s ossific nucleus to the healthy side’s ossific nucleus as an indicator of ossific nucleus size. This study indicates that the size of the ossific nucleus on the affected side is not a significant risk factor for postoperative AVN, regardless of whether CR or OR is performed. This observation aligns with the predominant outcomes reported in prior studies.
Scholars have previously documented the correlation between the incidence of AVN following surgical procedures in children undergoing OR and the presence of ossific nucleus. Segal et al.5 retrospectively evaluated 49 patients with DDH, among 17 hips underwent OR. The study results suggested that the occurrence of the ossific nucleus might reduce the risk of AVN after either CR or OR. However, the study had limitations as it did not distinguish between AVN occurrences after CR and OR. Some researchers contend that the performance of OR increases the likelihood of AVN incidence27. This is attributed to the fact that OR is an invasive surgical intervention, and the primary blood supply to the femoral head, the medial circumflex artery, may undergo ligation or damage during the procedure28,29,30,31. Luhmann et al.9 demonstrated that the presence of the ossific nucleus did not reduce the rate of AVN in children undergoing CR or OR. However, this study, like many others, only compared the differences in AVN occurrence between groups with and without the presence of the ossific nucleus, without quantifying the size of the ossific nucleus or studying the overall size of the ossific nucleus in relation to AVN incidence. This study suggests that the ossific nucleus volume does not correlate with AVN occurrence after OR in children with DDH.
This study has two limitations as follows: firstly, the relatively small sample size and retrospective design, which did not involve sample size estimation. Future research could benefit from multicenter studies and larger cohorts to provide more meaningful clinical information. Additionally, the minimum follow-up time in this study was 26 months postoperatively, which might underestimate the incidence of femoral head necrosis. However, using a two-year follow-up period is acceptable for making reasonable inferences, as seen in previous studies32. In future research, extending the postoperative follow-up time could enhance the credibility of the study.
In conclusion, ossific nucleus volume does not pose a risk for AVN in DDH children undergoing CR or OR, emphasizing the clinical significance of IHDI grading in predicting AVN risk during CR and the importance of early intervention to prevent treatment delays. In the future, 3D reconstruction of MRI images is expected to offer a more precise evaluation of the volume of the ossified nucleus and the femoral head (Supplementary Tables).
Data availability
Data is provided within the manuscript or supplementary information files.
References
Yang, S., Zusman, N., Lieberman, E. & Goldstein, R. Y. Developmental dysplasia of the hip. Pediatrics https://doi.org/10.1542/peds.2018-1147 (2019).
Malvitz, T. A. & Weinstein, S. L. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J. Bone Jt. Surg. Am. 76, 1777–1792. https://doi.org/10.2106/00004623-199412000-00004 (1994).
Zionts, L. E. & MacEwen, G. D. Treatment of congenital dislocation of the hip in children between the ages of one and three years. J. Bone Jt. Surg. Am. 68, 829–846 (1986).
Gregosiewicz, A. & Wośko, I. Risk factors of avascular necrosis in the treatment of congenital dislocation of the hip. J. Pediatr. Orthop. 8, 17–19 (1988).
Segal, L. S. et al. Avascular necrosis after treatment of DDH: The protective influence of the ossific nucleus. J. Pediatr. Orthop. 19, 177–184. https://doi.org/10.1097/00004694-199903000-00008 (1999).
Tarassoli, P., Gargan, M. F., Atherton, W. G. & Thomas, S. R. The medial approach for the treatment of children with developmental dysplasia of the hip. Bone Jt. J. 96B, 406–413. https://doi.org/10.1302/0301-620x.96b3.32616 (2014).
Zamzam, M. M. et al. One-stage bilateral open reduction through a medial approach in developmental dysplasia of the hip. J. Bone Jt. Surg. Br. 91, 113–118 (2009).
Konigsberg, D. E., Karol, L. A., Colby, S. & O’Brien, S. Results of medial open reduction of the hip in infants with developmental dislocation of the hip. J. Pediatr. Orthop. 23, 1–9 (2003).
Luhmann, S. J., Schoenecker, P. L., Anderson, A. M. & Bassett, G. S. The prognostic importance of the ossific nucleus in the treatment of congenital dysplasia of the hip. J. Bone Jt. Surg. Am. 80, 1719–1727. https://doi.org/10.2106/00004623-199812000-00001 (1998).
Roposch, A., Odeh, O., Doria, A. S. & Wedge, J. H. The presence of an ossific nucleus does not protect against osteonecrosis after treatment of developmental dysplasia of the hip. Clin. Orthop. Relat. Res. 469, 2838–2845. https://doi.org/10.1007/s11999-011-1801-6 (2011).
Sibiński, M., Synder, M., Domzalski, M. & Grzegorzewski, A. Risk factors for avascular necrosis after closed hip reduction in developmental dysplasia of the hip. Ortop. Traumatol. Rehabil. 6, 60–66 (2004).
Weiner, D. S., Hoyt, W. A. & O’Dell, H. W. Congenital dislocation of the hip. The relationship of premanipulation traction and age to avascular necrosis of the femoral head. J. Bone Jt. Surg. Am. 59, 306–311 (1977).
Kruczynski, J. Avascular necrosis of the proximal femur in developmental dislocation of the hip: Incidence, risk factors, sequelae and MR imaging for diagnosis and prognosis. Acta Orthop. Scand. 67, 3–48 (1996).
Schur, M. D., Lee, C., Arkader, A., Catalano, A. & Choi, P. D. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. J. Child Orthop. 10, 185–192. https://doi.org/10.1007/s11832-016-0743-7 (2016).
Kalamchi, A. & MacEwen, G. D. Avascular necrosis following treatment of congenital dislocation of the hip. J. Bone Jt. Surg. Am. 62, 876–888 (1980).
Wu, J. et al. Does the size of the femoral head correlate with the incidence of avascular necrosis of the proximal femoral epiphysis in children with developmental dysplasia of the hip treated by closed reduction?. J. Child Orthop. 14, 175–183. https://doi.org/10.1302/1863-2548.14.190176 (2020).
Sankar, W. N. et al. Closed reduction for developmental dysplasia of the hip: Early-term results from a prospective multicenter cohort. J. Pediatr. Orthop. 39, 111–118. https://doi.org/10.1097/bpo.0000000000000895 (2019).
Brougham, D. I., Broughton, N. S., Cole, W. G. & Menelaus, M. B. Avascular necrosis following closed reduction of congenital dislocation of the hip. Review of influencing factors and long-term follow-up. J. Bone Jt. Surg. Br. 72, 557–562 (1990).
Cha, S. M., Shin, H. D. & Shin, B. K. Long-term results of closed reduction for developmental dislocation of the hip in children of walking age under eighteen months old. Int. Orthop. 42, 175–182. https://doi.org/10.1007/s00264-017-3685-x (2018).
Bozkurt, C. et al. Evaluation of avascular necrosis risk factors after closed reduction for developmental dysplasia of the hip before walking age. J. Pediatr. Orthop. B 31, 237–241 (2022).
Carney, B. T., Clark, D. & Minter, C. L. Is the absence of the ossific nucleus prognostic for avascular necrosis after closed reduction of developmental dysplasia of the hip?. J. Surg. Orthop. Adv. 13, 24–29 (2004).
Clarke, N. M., Jowett, A. J. & Parker, L. The surgical treatment of established congenital dislocation of the hip: Results of surgery after planned delayed intervention following the appearance of the capital femoral ossific nucleus. J. Pediatr. Orthop. 25, 434–439 (2005).
Morbi, A. H., Carsi, B., Gorianinov, V. & Clarke, N. M. Adverse outcomes in infantile bilateral developmental dysplasia of the hip. J. Pediatr. Orthop. 35, 490–495 (2015).
Cooke, S. J., Rees, R., Edwards, D. L., Kiely, N. T. & Evans, G. A. Ossification of the femoral head at closed reduction for developmental dysplasia of the hip and its influence on the long-term outcome. J. Pediatr. Orthop. B 19, 22–26. https://doi.org/10.1097/BPB.0b013e32832fc8ca (2010).
Madhu, T. S., Akula, M., Scott, B. W. & Templeton, P. A. Treatment of developmental dislocation of hip: Does changing the hip abduction angle in the hip spica affect the rate of avascular necrosis of the femoral head?. J. Pediatr. Orthop. B 22, 184–188 (2013).
Bian, Z. et al. Risk factors for avascular necrosis after closed reduction for developmental dysplasia of the hip. J. Pediatr. Orthop. 42, 467–473. https://doi.org/10.1097/bpo.0000000000002228 (2022).
Harris, N. H., Lloyd-Roberts, G. C. & Gallien, R. Acetabular development in congenital dislocation of the hip: With special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy. J. Bone Jt. Surg. Br. 57, 46–52 (1975).
Zlotorowicz, M., Szczodry, M., Czubak, J. & Ciszek, B. Anatomy of the medial femoral circumflex artery with respect to the vascularity of the femoral head. J. Bone Jt. Surg. Br. 93, 1471–1474. https://doi.org/10.1302/0301-620x.93b11.26993 (2011).
Bolland, B. J., Wahed, A., Al-Hallao, S., Culliford, D. J. & Clarke, N. M. Late reduction in congenital dislocation of the hip and the need for secondary surgery: Radiologic predictors and confounding variables. J. Pediatr. Orthop. 30, 676–682 (2010).
Wenger, D. R. & Bomar, J. D. Human hip dysplasia: Evolution of current treatment concepts. J. Orthop. Sci. 8, 264–271. https://doi.org/10.1007/s007760300046 (2003).
Tang, H. C., Lee, W. C., Kao, H. K., Yang, W. E. & Chang, C. H. Surgical outcomes of developmental dysplasia of the hip with or without prior failed closed reduction. J. Pediatr. Orthop. 35, 703–707. https://doi.org/10.1097/bpo.0000000000000374 (2015).
Roposch, A., Stöhr, K. K. & Dobson, M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip: A meta-analysis. J. Bone Jt. Surg. Am. 91, 911–918. https://doi.org/10.2106/jbjs.H.00096 (2009).
Author information
Authors and Affiliations
Contributions
P.H.T. and X.L.K. contributed to the study design and initial manuscript drafting, S.F. and L.M. participated in data analysis, D.Y.Z. and W.B. were involved in data collection and summarization, while J.Q. contributed to meticulous manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pang, H., Xu, L., Su, F. et al. Association between ossific nucleus volume changes and postoperative avascular necrosis risk in children with developmental dysplasia of the hip. Sci Rep 14, 21363 (2024). https://doi.org/10.1038/s41598-024-72445-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72445-5
- Springer Nature Limited