Abstract
Traumatic brain injury (TBI) affects millions globally, with a majority of TBI cases being classified as mild, in which diffuse pathologies prevail. Two of the pathological hallmarks of TBI are diffuse axonal injury (DAI) and microglial activation. While progress has been made investigating the breadth of TBI-induced axonal injury and microglial changes in rodents, the neuroinflammatory progression and interaction between microglia and injured axons in humans is less well understood. Our group previously investigated microglial process convergence (MPC), in which processes of non-phagocytic microglia directly contact injured proximal axonal swellings, in rats and micropigs acutely following TBI. These studies demonstrated that MPC occurred on injured axons in the micropig, but not in the rat, following diffuse TBI. While it has been shown that microglia co-exist and interact with injured axons in humans post-TBI, the occurrence of MPC has not been quantitatively measured in the human brain. Therefore, in the current study we sought to validate our pig findings in human postmortem tissue. We investigated MPC onto injured axonal swellings and intact myelinated fibers in cases from individuals with confirmed DAI and control human brain tissue using multiplex immunofluorescent histochemistry. We found an increase in MPC onto injured axonal swellings, consistent with our previous findings in micropigs, indicating that MPC is a clinically relevant phenomenon that warrants further investigation.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) affects an estimated sixty-nine million people globally each year1. In 2022 alone, over twenty thousand United States service members from the Army, Navy, Air Force, and Marines, suffered from a TBI2. Approximately 80% of all TBI cases are classified as mild, in which diffuse pathologies that are difficult to discern via molecular imaging prevail. One of the pathological hallmarks of mild TBI is diffuse axonal injury (DAI), wherein axons are disrupted over time and progress to disconnection resulting in a proximal axonal swelling that is still connected to the neuronal soma and a distal axonal segment that degenerates via Wallerian degradation3. Additionally, microglia, the innate immune cell of the central nervous system, have been shown to be activated following TBI in both humans4,5,6,7,8,9 and animals10,11,12,13,14 and have been linked to cognitive changes following TBI5. Activated microglia fall on a spectrum from pro-inflammatory to anti-inflammatory with functions that can promote tissue neurodegeneration or neuroprotection15,16,17,18,19,20,21.
While previous studies have identified various pro and anti-inflammatory pathways upregulated following TBI, non-phagocytic physical interactions between activated microglia and adjacent neurons have only recently begun to be investigated10,22,23,24,25,26,27,28,29. Previous studies from our group using a micropig model of TBI found microglial processes converging onto the injured proximal axonal segment in a phenomenon called microglial process convergence (MPC)27,30. This MPC does not appear to involve phagocytosis27 and was not found in our rat model of TBI26. Specifically, in pigs, the number of activated microglial processes contacting injured proximal axonal swellings was nearly twice that observed for myelinated fibers at 6 h following a diffuse TBI generated using the central fluid percussion injury model27. This MPC significantly increased from 6 h to 1 day post injury26. However, in rats, there were far fewer microglial processes contacting injured axonal swellings compared to myelinated fibers following TBI, indicating that MPC might be a phenomenon associated with higher order gyrencephalic brains26. To investigate the potential that MPC onto injured axons occurs in the human brain, in the current study we quantitatively assessed the prevalence of MPC onto injured axonal swellings and intact axonal segments in human postmortem brain tissue. We hypothesized that human postmortem tissue would demonstrate significant microglial process convergence.
Results
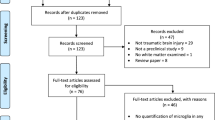
Microglial process convergence increases following axonal injury
To investigate the potential for microglial process convergence occurring on injured axonal swellings or intact myelinated fibers in the human brain, multiplexed immunohistochemistry against the anterogradely transported protein, amyloid precursor protein (APP) to visualize injured axons, myelin basic protein (MBP) to visualize intact myelinated axons, and ionized calcium-binding adaptor molecule 1 (Iba-1) to visualize microglia processes was done on human postmortem tissue from the DoD/USU tissue repository. When all fibers that were analyzed across all cases were collated as APP + injured axonal swelling or MBP + intact myelinated fibers, it was found that more Iba-1 + microglial processes/um of the perimeter were in direct contact with APP + axonal swellings compared to MBP + intact myelinated fibers (Fig. 1A; U = 32,240, p = 2.4 × 10–4). The paraffin sections were thin sections, precluding the ability to perform 3D reconstructions of the axonal swellings, as we had done for our previous studies26,27. As a single 2D image of the axonal segments is likely to be missing processes that are out of the plane of section, we also investigated the number of Iba-1 + microglial processes that were within 5um of the axonal segments. More microglial processes were found within 5um of APP + axonal swellings compared to MBP + intact myelinated fibers (Fig. 1B; U = 34,260, p = 2.99 × 10–6), indicating that more microglial processes are close to the injured axonal swellings.
After completing this initial analysis of the overall comparison between APP + swellings and MBP + myelinated fibers, the cases were un-blinded. Following case unblinding, it was discovered that some APP + axonal swellings were identified in control individuals and some MBP + myelinated fibers were analyzed from individuals that had DAI (Fig. 2). Therefore, the analyzed fibers were organized into four groups: (1) MBP + intact myelinated fibers in control tissue, (2) MBP + intact myelinated fibers in DAI tissue, (3) APP + axonal swellings in control tissue, and (4) APP + axonal swellings in DAI tissue. When the data was stratified by axonal injury and DAI cases we found more microglial process convergence occurring directly onto APP + injured axonal swellings, specifically within tissue with verified DAI (χ2(3) = 15.53, p = 0.001; Fig. 3A). There were also significantly more microglia processes within 5 μm of APP + injured swellings in both control and DAI tissue as compared to MBP + fibers in control postmortem samples (χ2(3) = 21.97, p = 6.61 × 10–5; Fig. 3B).
Representative fluorescent micrographs of microglial process interactions with either intact myelinated axonal fibers (first two columns) or injured axonal swellings (second two columns). Nuclei were labeled with Dapi in blue (top panel). Microglia were immunolabeled with Iba-1 which is pseudo colored green in the second panel. Intact myelinated fibers immunolabeled with MBP (first two columns of the third panel) or injured axonal swellings immunolabeled with APP (last two columns of the third panel) were pseudo colored in red. The last panel shows the full overlay for the multiplex immunohistochemical labeling. Scale bar is 20 μm.
Microglial processes appear to converge onto injured axons in control and DAI cases. Box and whisker plots of Iba-1 + microglial processes (A) in direct contact with or (B) within 5 μm of MBP + intact myelinated axonal fibers in either control cases (n = 161 fibers) or DAI cases (n = 36 fibers) and APP + injured axonal swellings in control cases (n = 105 swellings) or DAI cases (n = 173 swellings). Note that while the APP + axonal swellings within the control cases did not have significantly higher Iba-1 + microglial processes directly touching it (p = 0.053), both control cases and DAI cases had significantly more Iba-1 + microglial processes within 5 μm compared to the intact MBP + fiber counterparts. *p < 0.05.
The morphology between MBP + intact axonal segments and APP + axonal swellings was significantly different (χ2(3) = 12.2, p = 0.007; Fig. 4), with the APP + axonal swellings within DAI tissue having smaller perimeters compared to the MBP + intact axonal fibers within control tissue (p = 0.003; Fig. 4C). This is interesting as the number of Iba-1 + microglial processes in contact with the axonal segments or within 5 μm of the axonal segments were calculated as the number of contacts per μm of the perimeter for all axonal segments assessed. As expected, the APP + axonal swellings in both control and DAI tissue had significantly higher circularity indices compared to the MBP + axonal fibers in either control or TBI tissue (χ2(3) = 332.35, p ≤ 0.001; Fig. 4D). Specifically, while the MBP + intact axonal fibers in both control and DAI cases were more linear the APP + axonal swellings had a high degree of circularity (Fig. 4). There were no differences observed between control and DAI cases for either MBP + intact fibers (p = 0.25) or APP + injured axonal swellings (p = 0.83).
Injured axons have lower perimeters and are more circular than MBP + intact myelinated fibers. Low magnification micrographs of MBP + intact myelinated fibers (arrow heads) within and APP + axonal swellings (arrows) within (A) control tissue or (B) DAI tissue. Box and whisker plots of (C) the perimeter of axonal segments and D) the circularity of axonal segments of MBP + intact axonal fibers in either control cases (n = 161 fibers) or TBI cases (n = 36 fibers) and APP + injured axonal swellings in control cases (n = 105 swellings) or TBI cases (n = 173 swellings). Note that while there was no significant difference between APP + axonal swellings in control tissue compared to MBP + myelinated fibers in control tissue (p = 0.08), injured APP + axonal swellings within TBI tissue had significantly lower perimeters. Scale bar is 20 μm. *p < 0.05.
To validate the by eye counts of Iba-1 microglial process puncta onto the APP + axonal swellings, the integrated density/intensity of Iba-1 labeled microglial processes in the region of the APP + axonal swelling or MBP + myelinated fiber was assessed, in which a mask of the APP + axonal swelling or the MBP + myelinated fiber was made and the integrated density of Iba-1 labeling within those regions was assessed. The intensity of Iba-1 labeling was significantly higher in APP + injured axonal swellings compared to control MBP + axons (χ2(3) = 56.217, p = 3.78 × 10–12; Fig. 5). Specifically, there were no differences in the intensity of Iba-1 between APP + injured axons (p = 0.72) nor between MBP + axonal segments (p = 0.99) within control tissue compared to DAI tissue. There was significantly higher Iba-1 integrated density within APP + axonal swellings compared to MBP + intact axonal segments regardless of DAI status of the case (MBP + intact fiber in control cases vs. APP + swellings in control cases p < 0.001; MBP + intact fiber in DAI cases vs. APP + swellings in DAI cases p < 0.001; Fig. 5). This finding supported the counts of microglial process convergence onto injured axonal swellings depicted in Fig. 3, demonstrating increases in microglial process convergence onto APP + injured axonal swellings in the human brain.
Injured axons have higher Iba-1 + microglia fluorescent intensity than MBP + intact myelinated fibers. Box and whisker plots depicting the integrated density of Iba-1 + microglia within axonal segments of MBP + intact axonal fibers in either control cases (n = 161 fibers) or DAI cases (n = 36 fibers) and APP + injured axonal swellings in control cases (n = 105 swellings) or DAI cases (n = 173 swellings). Injured APP + axonal swellings in either control or DAI tissue had significantly higher Iba-1 + fluorescent intensity within the swellings compared to intact MBP + axonal fibers. *p < 0.05.
Discussion
The current study demonstrates that microglial processes converge onto injured axonal swellings in the human brain, supporting our hypothesis. The perimeters of the axonal segments were relatively consistent across MBP + myelinated fibers in both control and DAI tissue as well as APP + injured axonal swellings within control tissue. The APP + injured axonal swellings within TBI tissue had significantly lower perimeters than the MBP + intact myelinated axonal segments within control tissue. The number of Iba-1 + microglial processes in direct contact with the axonal segment, however, was significantly higher onto APP + axonal swellings compared to MBP + axonal segments, despite the lower perimeter available for contact. There were also significantly more microglial processes within 5 μm of the injured axons compared to the MBP + axonal segments. Our group previously observed MPC in the micropig brain acutely following a central fluid percussion diffuse TBI27. This phenomenon; however, was not recapitulated following TBI in the rat26, indicating that MPC onto injured axons might be species specific. The current findings that MPC onto injured axonal swellings occurs in human postmortem tissue, validates our previous findings in the micro pig and indicates that MPC following TBI might primarily manifest in higher order gyrencephalic brains. These findings show that MPC is a phenomenon that occurs in the human population, necessitating further investigation.
Diffuse axonal injury (DAI) or traumatic axonal injury (TAI) is one of the hallmark pathologies of mild TBI31,32,33,34,35,36. It was originally thought that DAI occurs following TBI due to the mechanical shearing of the axons. However, this is only true for a subset of axons that are observed to be injured within minutes of TBI, which is referred to as primary axotomy. Rather, secondary axotomy/axonal injury, which occurs sub-acutely after injury in rodent models of TBI is the phenomenon that is typically investigated. Secondary axonal injury involves cytoskeletal dysregulation and accumulation of organelles and proteins, such as APP within the injured axonal swelling37,38,39. Specifically, the tensile forces of TBI cause axonal alterations that allow an influx of calcium into the axon. This calcium influx leads to activation of cysteine protease pathways, which leads to degradation of neurofilaments. Microtubules are also impacted by calcium influx following TBI and ultimately lead to a reactive axonal swelling as anterogradely transported proteins and organelles pool at the end of the proximal axon38,39,40. In the early 1990s immunohistochemistry against the anterogradely transported protein, APP, was found to efficiently label the proximal injured axonal segment where it pooled41,42. Immunohistochemical labeling of APP has since become the gold standard for identifying DAI pathologically. Axonal injury is typically studied in rodents 6–24 h following TBI, when it is most prevalent43,44. Within higher order animals DAI appears to be prevalent starting hours following injury and peaking at 1w post-TBI13, however DAI has been shown to last up to 6 months in a pig model of TBI45 and has been observed in human postmortem tissue from people several years following a TBI46,47. While DAI is a hallmark of diffuse TBI-induced pathologies, DAI can also be present following hypoxia and in cases of substance use-related deaths, making the assessment of MPC on injured axonal swellings impactful beyond the TBI field.
Many recent studies have demonstrated the impact of inflammatory cascades in regulating behavioral morbidities, general pathology, and neuronal function in both the normal brain and in various disease states, including TBI21,48,49. Neuroinflammation has been demonstrated in various brain regions in the human population chronically following TBI5,9,20,50. Microglia, the innate immune cells of the brain, are critical mediators of these TBI-induced neuroinflammatory processes16,51,52,53,54,55,56,57. Microglia have been shown to contact specific areas of the axon in the mouse brain during homeostasis including, the nodes of Ranvier58, the axon initial segment10, synapses59, and neuronal soma60. Many studies using rodents have indicated that reduction or elimination of activated microglia and/or targeting various neuroinflammatory signaling pathways ameliorates downstream pathology and behavioral morbidity24,61,62,63,64. Conversely, other studies have also found that anti-inflammatory microglial activation is necessary and potentially advantageous17,54,65,66,67,68,69,70. These studies demonstrated activated microglia can secrete neurotrophic factors15,71,72,73, which would suggest a potential ameliorative effect of microglia following injury in some cases. Additionally, recent studies have shown that microglia physical contacts play a role in regulating neuronal activity, either increasing activity following anesthesia74,75 or decreasing activity following epileptiform activity60,67.
A study by Schirmer et al. investigating human post-mortem tissue found a significant positive correlation between the density of microglia and axonal outgrowth as well as the duration of patient survival following TBI, however, they did not quantitatively investigate the physical interactions between microglia and injured axons76. Another study done in vitro and in rats following a spinal cord injury found that exosomes from anti-inflammatory microglia increased neurite outgrowth in vitro and increased GAP43 expression in vivo, indicating that microglia could play a role in axonal outgrowth17.
Microglia have been observed within physical proximity to injured axonal swellings in human postmortem tissue76,77,78. Oehmichen et al. observed an increase in CD-68 + microglial cells areas of axonal injury in the white matter at least five days post-TBI in human postmortem tissue, however, they only observed limited physical interactions between the CD68 + cells and the APP + axonal segments77. Ryu et al. qualitatively identified areas in which Iba-1 + microglia were in proximity to APP + injured axons in postmortem tissue from individuals following both motor vehicle accident and blast induced TBI78. Although, these previous studies indicated that there could be direct physical interactions between microglia and injured axonal segments, our current study is the first to quantitatively show that MPC occurs onto injured proximal axonal segments in human brain tissue following TBI.
We do appreciate that there are limitations to the current study, mainly, that all cases were from male doners. There is evidence that males and females respond to TBI differently79. A recent study also found that the burden of axonal injury following a diffuse TBI in a pig model was significantly higher in females compared to age matched males80. Further, microglia have been shown to be different in males and females81,82,83,84,85. Therefore, investigations into MPC in both the male and female population should be done to fully appreciate the prevalence of MPC onto injury axons in the human brain. We further acknowledge that MBP + intact axonal segments might not be un-injured, rather could be pathological in a way in which there is no APP + axonal swelling present. Additionally, these sections were only 15 μm thick, precluding a 3D investigation of MPC, as was done in our previous micro pig studies26,27. It is likely that the numbers of microglial processes we found converging onto the axonal segments in the current study were artificially lower than they might actually be due to the section thickness. Therefore, investigations using thicker tissue in which 3D reconstructions could be done, would be warranted to glean a better appreciation of the degree of MPC onto injured axonal swellings in human postmortem tissue of both males and females. Despite these limitations, the current study is the first to quantitatively demonstrate MPC onto injured axons in the human brain. These findings indicate that MPC is a component of human DAI and that further studies exploring the phenotypes and overall roles of the microglia involved in MPC following DAI should be investigated.
Methods
Samples
Human brain samples were acquired from the Department of Defense (DoD)/Uniform Services University (USU) Tissue Repository. All cases were from males between 26 and 69 years old (median age of 36 years) with a maximum postmortem interval of 1 day (median of 19 h from death to fixation). A total of 11 human brain samples were used. All identifiers were removed from the samples. Tissue was paraffin embedded and sectioned at 15um. Slides containing areas demonstrating DAI were used for this study. Of these samples, 6 were cases with demonstrated areas of DAI and 5 were controls. Confirmation of DAI was defined as focal positive labeling of myelinated axons by APP. The etiology of DAI was varied with the cause of death for 3 cases being TBI, the cause of death for 2 cases being drug/alcohol abuse-related, and the cause of death for one case being glioblastoma. The cause of death for control cases was cardiac arrest for 3 cases, kidney failure for one case, and liver failure for one case. All but one case were taken from regions within the cingulate cortex with corpus callosum (one DAI case was harvested from an unclear brain region). All imaging was done in regions in which the axon fibers were running in parallel to the tissue section. All study staff were blinded to case group throughout the labeling, imaging, and analysis.
Immunohistochemistry
To visualize the interactions between microglia and injured or intact axonal segments in the human brain multiplexed fluorescent immunohistochemistry was performed. To identify injured axons, an antibody against amyloid precursor protein (APP) was used, which indicates axonal transport issues indicative of axonal injury 13,14,58. To visualize microglia, an antibody against ionized calcium-binding adaptor molecule 1 (Iba-1) was used. Intact axonal fibers were visualized using an antibody against myelin basic protein (MBP).
In this procedure, sections were deparaffinized by incubating slides in progressively more concentrated alcohols. Antigen retrieval was done by steaming the tissue in pH 6.0 citric acid buffer for 30 min. Tissue was then blocked and permeabilized at room temperature in 5% normal goat serum (NGS), 2% bovine serum albumin (BSA) and 1.5% triton in phosphate buffered saline for 2 h followed by overnight incubation with a rabbit antibody against microglial Iba-1 (1:200; Cat.#019-19741 Wako; Richmond, VA, USA) at 4C° in 5% NGS/2% BSA/0.5% triton. Tissue was washed with 1%NGS/1%BSA in PBS at least six times prior to secondary antibody incubation with Alexa Fluor 488-conjugated goat anti-rabbit IgG (1:700; Cat.# A-11008, Life Technologies, Carlsbad, CA, USA) in 1%NGS/1%BSA/PBS at room temperature for 2 h. Tissue was washed in PBS at least four times prior to overnight incubation with a mouse antibody against the 22C11 clone of APP (1:200; Cat.#14-9749-82, ThermoFisher Scientific, Waltham, MA, USA) in 5% NGS/2% BSA/0.5% triton at 4C°. Tissue was washed with 1%NGS/1%BSA in PBS at least six times prior to the next secondary antibody incubation with Alexa Fluor 647-conjugated goat anti-mouse IgG (1:700; Cat.# A-21237, Life Technologies, Carlsbad, CA, USA) in 1%NGS/1%BSA/PBS at room temperature for 2 h. Iba-1 and APP labeled tissue was washed in PBS at least four times prior to overnight incubation with a rat antibody against MBP (1:200; Novus) at 4C° in 5% NGS/2% BSA/0.5% triton. Tissue was washed with 1%NGS/1%BSA in PBS at least six times prior to the third secondary antibody incubation with Alexa Fluor 568-conjugated goat anti-rat IgG (1:700; Cat.# A-11077, Life Technologies, Carlsbad, CA, USA) in 1%NGS/1%BSA/PBS at room temperature for 2 h. Tissue was washed in PBS at least four times. Multiplex labeled tissue was coversliped with Vectashield hard-set mounting medium with Dapi (Cat.#H-1500; Vector Laboratories, Burlingame, CA, USA).
Microglial process convergence analysis
The fluorescently immunolabeled slides were imaged on the Keyence BZ-X800 microscope (Keyence Corporation of America, Itasca, IL, USA) at 40X magnification. One section was analyzed for each case by an investigator blinded to group. A navigation super-image was generated using the far-red channel in which the APP + injured axonal swellings could be visualized. APP + axonal swellings were differentiated from APP within the neuronal soma by the intensity of the axonal swelling, which were more intense than somatic APP labeling, by the absence of DAPI within APP + axonal swellings, and by the difference in size between the axonal swelling and neuronal soma. Images containing at least 1 APP + injured axonal swellings were captured or no APP + swellings but clean MBP labeling were captured. Fewer MBP only images were captured, as there were several analyzable MBP + intact myelinated fibers in each captured image, whereas there were few analyzable APP + axonal swellings in each captured image. At least 25 images were taken for most cases, however, only 13 images were captured for 1 case as no APP + swellings were identified. Across all samples a total of 161 MBP + intact axonal segments from controls, 36 MBP + intact axonal segments from injured samples, 105 injured axonal swellings from controls, and 173 injured axonal swellings from injured samples were analyzed for the current study. Fiji Image J software (National Institute of Health, Bethesda, MD, USA) was used to evaluate the 2D images. Image scales were set to 5.3 pixels/um.
To assess the interaction between microglia and injured axonal swellings, the APP + axonal swelling was traced using the freehand tool and measured for perimeter, area, shape descriptors (aspect ratio, circularity, round, solidity), integrated density, and mean grey value. The number of microglial processes and puncta that were directly touching the APP + axonal swelling was counted by hand. A microglial puncta was counted if the Iba-1 stain was bright and consisted of a cluster of at least 4 pixels. Then, the region encircling the APP + axonal swelling was enlarged by 5 um and the microglial processes and puncta within the enlarged region was counted by hand.
In order to visualize the interaction between microglia and intact axonal segments, a random number generator was used to generate x,y coordinates to choose a MBP + axonal segment on the image. The axonal segment was traced with the freehand tool and measured for perimeter, area, shape descriptors (aspect ratio, circularity, roundness, and solidity), integrated density, and mean grey value. The number of microglial processes and puncta that were directly touching the MBP + intact axonal segment was counted by eye. Then, the region encircling the axonal segment was enlarged by 5um and the number of microglial processes and puncta within the enlarged region were counted by eye.
Statistical analysis
The statistics were run using IBM SPSS software (IBM Corp., Armonk, NY). A Shapiro–Wilk test was conducted to test for normality of the data. As the data was not normally distributed, a Mann–Whitney U test was used to test differences between all APP + injured axonal swellings and all MBP + intact axonal segments. A Kruskal–Wallis test was run to assess differences across multiple groups. A Bonferroni post hoc was used to correct for multiple pairwise comparisons. Statistical significance was set to a p value of < 0.05. Data is presented as means and standard error of the mean. All raw data is included in Supplemental table 1.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files. Following publication these data will also be available on the Open Science Framework along with the analysis protocol.
References
Dewan, M. C. et al. Estimating the global incidence of traumatic brain injury. J. Neurosurg. 130, 1080–1097 (2018).
DOD TBI Worldwide Numbers [Internet]. Military Health System. [cited 2024 May 28]. Available from: https://www.health.mil/Military-Health-Topics/Centers-of-Excellence/Traumatic-Brain-Injury-Center-of-Excellence/DOD-TBI-Worldwide-Numbers.
Kelley, B. J., Farkas, O., Lifshitz, J. & Povlishock, J. T. Traumatic axonal injury in the perisomatic domain triggers ultrarapid secondary axotomy and Wallerian degeneration. Exp. Neurol. 198, 350–360 (2006).
Coughlin, J. M. et al. Imaging of glial cell activation and white matter integrity in brains of active and recently retired national football league players. JAMA Neurol. 74, 67–74 (2017).
Coughlin, J. M. et al. Neuroinflammation and brain atrophy in former NFL players: An in vivo multimodal imaging pilot study. Neurobiol. Dis. 74, 58–65 (2015).
Little, D. M. et al. Thalamic integrity underlies executive dysfunction in traumatic brain injury. Neurology 74, 558–564 (2010).
Boche, D., Perry, V. H. & Nicoll, J. R. Review: Activation patterns of microglia and their identification in the human brain. Neuropathol. Appl. Neurobiol. 39, 3–18 (2013).
Neumann, K. D. et al. Microglial activation persists beyond clinical recovery following sport concussion in collegiate athletes. Front. Neurol. https://doi.org/10.3389/fneur.2023.1127708/full (2023).
Velázquez, A., Ortega, M., Rojas, S., González-Oliván, F. J. & Rodríguez-Baeza, A. Widespread microglial activation in patients deceased from traumatic brain injury. Brain Inj. 29, 1126–1133 (2015).
Baalman, K. et al. Axon initial segment-associated microglia. J. Neurosci. 35, 2283–2292 (2015).
Cao, T., Thomas, T. C., Ziebell, J. M., Pauly, J. R. & Lifshitz, J. Morphological and genetic activation of microglia after diffuse traumatic brain injury in the rat. Neuroscience. 225, 65–75 (2012).
Chhor, V. et al. Role of microglia in a mouse model of paediatric traumatic brain injury. Brain Behav. Immun. 63, 197–209 (2017).
Grovola, M. R. et al. Diverse changes in microglia morphology and axonal pathology during the course of 1 year after mild traumatic brain injury in pigs. Brain Pathol. https://doi.org/10.1111/bpa.12953 (2021).
Witcher, K. G. et al. Traumatic brain injury-induced neuronal damage in the somatosensory cortex causes formation of rod-shaped microglia that promote astrogliosis and persistent neuroinflammation. Glia 66, 2719–2736 (2018).
Aldskogius, H. Microglia in neuroregeneration. Microsc. Res. Tech. 46, 40–46 (2001).
Neumann, H., Kotter, M. R. & Franklin, R. J. M. Debris clearance by microglia: An essential link between degeneration and regeneration. Brain J. Neurol. 132, 288–295 (2009).
Guan, P. et al. M2 microglia-derived exosome-loaded electroconductive hydrogel for enhancing neurological recovery after spinal cord injury. J. Nanobiotechnol. 22, 8 (2024).
Zhao, S., Umpierre, A. D. & Wu, L.-J. Tuning neural circuits and behaviors by microglia in the adult brain. Trends Neurosci. 47, 181–194 (2024).
Aguzzi, A., Barres, B. & Bennett, M. L. Microglia: Scapegoat, saboteur or something else?. Inflammation 339, 156–162 (2013).
Ramlackhansingh, A. F. et al. Inflammation after trauma: Microglial activation and traumatic brain injury. Ann. Neurol. 70, 374–383 (2011).
Nizamutdinov, D. & Shapiro, L. A. Overview of traumatic brain injury: An immunological context. Brain Sci. 7, 11 (2017).
Clark, K. C. et al. Compromised axon initial segment integrity in EAE is preceded by microglial reactivity and contact. Glia 64, 1190–1209 (2016).
Eyo, U. B. & Wu, L. J. Bidirectional microglia-neuron communication in the healthy brain. Neural Plast. 2013, 1–10 (2013).
Eyo, U. B. et al. Modulation of microglial process convergence toward neuronal dendrites by extracellular calcium. J. Neurosci. 35, 2417–2422 (2015).
Eyo, U. B. et al. The GluN2A subunit regulates neuronal NMDA receptor-induced microglia-neuron physical interactions. Sci. Rep. https://doi.org/10.1038/s41598-018-19205-4 (2018).
Gorse, K. M. & Lafrenaye, A. D. The importance of inter-species variation in traumatic brain injury-induced alterations of microglial-axonal interactions. Front. Neurol. 9, 778 (2018).
Lafrenaye, A. D., Todani, M., Walker, S. A. & Povlishock, J. T. Microglia processes associate with diffusely injured axons following mild traumatic brain injury in the micro pig. J. Neuroinflamm. 12, 186 (2015).
Lafrenaye, A. Physical interactions between activated microglia and injured axons: Do all contacts lead to phagocytosis?. Neural Regen. Res. 11, 538 (2016).
Hu, Y. & Tao, W. Current perspectives on microglia-neuron communication in the central nervous system: Direct and indirect modes of interaction. Journal of Advanced Research [Internet]. 2024 [cited 2024 May 1]; Available from: https://www.sciencedirect.com/science/article/pii/S2090123224000067.
Benusa, S. D. & Lafrenaye, A. D. Microglial process convergence on axonal segments in health and disease. Neuroimmunol. Neuroinflamm. 7, 23–39 (2020).
Mesfin, F. B., Gupta. N., Hays Shapshak. A. & Taylor, R. S. Diffuse axonal injury. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 May 10]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK448102/.
Graham, N. S. N. et al. Diffuse axonal injury predicts neurodegeneration after moderate–severe traumatic brain injury. Brain 143, 3685–3698 (2020).
Frati, A. et al. Diffuse axonal injury and oxidative stress: A comprehensive review. Int. J. Mol. Sci. 18, 2600 (2017).
Büki, A. & Povlishock, J. T. All roads lead to disconnection?—Traumatic axonal injury revisited. Acta Neurochir. 148, 181–193 (2006).
Smith, D. H., Meaney, D. F. & Shull, W. H. Diffuse axonal injury in head trauma. J. Head Trauma Rehabil. 18, 307–316 (2003).
Chen, Q. et al. Traumatic axonal injury: Neuropathological features, postmortem diagnostic methods, and strategies. Forensic Sci. Med. Pathol. 18, 530–544 (2022).
Maxwell, W. L., Watt, C., Graham, D. I. & Gennarelli, T. A. Ultrastructural evidence of axonal shearing as a result of lateral acceleration of the head in non-human primates. Acta Neuropathol. 86, 136–144 (1993).
Povlishock, J. T. Pathobiology of traumatically induced axonal injury in animals and man. Ann. Emerg. Med. 22, 980–986 (1993).
Christman, C. W., Grady, M. S., Walker, S. A., Holloway, K. L. & Povlishock, J. T. Ultrastructural studies of diffuse axonal injury in humans. J. Neurotrauma. 11, 173–186 (1994).
Stone, J. R. et al. Impaired axonal transport and altered axolemmal permeability occur in distinct populations of damaged axons following traumatic brain injury. Exp. Neurol. 190, 59–69 (2004).
Gentleman, S. M., Nash, M. J., Sweeting, C. J., Graham, D. I. & Roberts, G. W. β-Amyloid precursor protein (βAPP) as a marker for axonal injury after head injury. Neurosci. Lett. 160, 139–144 (1993).
Sherriff, F. E., Bridges, L. R. & Sivaloganathan, S. Early detection of axonal injury after human head trauma using immunocytochemistry for beta-amyloid precursor protein. Acta Neuropathol. 87, 55–62 (1994).
DiLeonardi, A. M., Huh, J. W. & Raghupathi, R. Impaired axonal transport and neurofilament compaction occur in separate populations of injured axons following diffuse brain injury in the immature rat. Brain Res. 1263, 174–182 (2009).
Bramlett, H. M., Kraydieh, S., Green, E. J. & Dietrich, W. D. Temporal and regional patterns of axonal damage following traumatic brain injury: A beta-amyloid precursor protein immunocytochemical study in rats. J. Neuropathol. Exp. Neurol. 56, 1132–1141 (1997).
Chen, X.-H. et al. Long-term accumulation of amyloid-beta, beta-secretase, presenilin-1, and caspase-3 in damaged axons following brain trauma. Am. J. Pathol. 165, 357–371 (2004).
Johnson, V. E., Stewart, W. & Smith, D. H. Widespread tau and amyloid-beta pathology many years after a single traumatic brain injury in humans. Brain Pathol. 22, 142–149 (2012).
Johnson, V. E., Stewart, W. & Smith, D. H. Axonal pathology in traumatic brain injury. Exp. Neurol. 246, 35–43 (2013).
Morganti-Kossmann, M. C., Satgunaseelan, L., Bye, N. & Kossmann, T. Modulation of immune response by head injury. Injury 38, 1392–1400 (2007).
Kelley, B. J., Lifshitz, J. & Povlishock, J. T. Neuroinflammatory responses after experimental diffuse traumatic brain injury. J. Neuropathol. Exp. Neurol. 66, 989–1001 (2007).
Zhou, Y. et al. Characterization of thalamocortical association using amplitude and connectivity of fMRI in mild traumatic brain injury. J. Magn. Reson. Imaging 39, 1558–1568 (2014).
Mannix, R. C. & Whalen, M. J. Traumatic brain injury, microglia, and Beta amyloid. Int. J. Alzheimer’s Dis. 2012, 608732 (2012).
Smith, C. Review: The long-term consequences of microglial activation following acute traumatic brain injury. Neuropathol. Appl. Neurobiol. 39, 35–44 (2013).
Ransohoff, R. M. & Perry, V. H. Microglial physiology: Unique stimuli, specialized responses. Annu. Rev. Immunol. 27, 119–145 (2009).
Karve, I. P., Taylor, J. M. & Crack, P. J. The contribution of astrocytes and microglia to traumatic brain injury. Br. J. Pharmacol. 173, 692–702 (2015).
Tay, T. L., Hagemeyer, N. & Prinz, M. The force awakens: Insights into the origin and formation of microglia. Curr. Opin. Neurobiol. 39, 30–37 (2016).
Loane, D. J. & Kumar, A. Microglia in the TBI brain: The good, the bad, and the dysregulated. Exp. Neurol. 275, 316–327 (2016).
Grovola, M. R., von Reyn, C., Loane, D. J. & Cullen, D. K. Understanding microglial responses in large animal models of traumatic brain injury: An underutilized resource for preclinical and translational research. J. Neuroinflamm. 20, 67 (2023).
Ronzano, R. et al. Microglia-neuron interaction at nodes of Ranvier depends on neuronal activity through potassium release and contributes to remyelination. Nat. Commun. 12, 5219 (2021).
Wake, H., Moorhouse, A. J., Jinno, S., Kohsaka, S. & Nabekura, J. Resting microglia directly monitor the functional state of synapses in vivo and determine the fate of ischemic terminals. J. Neurosci. Off. J. Soc. Neurosci. 29, 3974–3980 (2009).
Uweru, J. O. & Eyo, U. B. A decade of diverse microglial-neuronal physical interactions in the brain (2008–2018). Neurosci. Lett. 698, 33–38 (2019).
Weber, M. D. et al. The influence of microglial elimination and repopulation on stress sensitization induced by repeated social defeat. Biol. Psychiatry 85, 667–678 (2019).
d’Avila, J. C. et al. Microglial activation induced by brain trauma is suppressed by post-injury treatment with a PARP inhibitor. J. Neuroinflamm. 9, 31 (2012).
Siopi, E. et al. Evaluation of late cognitive impairment and anxiety states following traumatic brain injury in mice: The effect of minocycline. Neurosci. Lett. 511, 110–115 (2012).
Henry, R. J., Ritzel, R. M., Barrett, J. P., Doran, S. J., Jiao, Y., Leach, J. B. et al. Microglial depletion with CSF1R inhibitor during chronic phase of experimental traumatic brain injury reduces neurodegeneration and neurological deficits. bioRxiv 791871 (2019).
Swiatkowski, P. et al. Activation of microglial P2Y12 receptor is required for outward potassium currents in response to neuronal injury. Neuroscience 318, 22–33 (2016).
Dissing-Olesen, L. et al. Activation of neuronal NMDA receptors triggers transient ATP-mediated microglial process outgrowth. J. Neurosci. 34, 10511–10527 (2014).
Eyo, U. B. et al. Neuronal hyperactivity recruits microglial processes via neuronal NMDA receptors and microglial P2Y12 receptors after status epilepticus. J. Neurosci. Off. J. Soc. Neurosci. 34, 10528–10540 (2014).
Franco, E. C. S., Cardoso, M. M., Gouvêia, A., Pereira, A. & Gomes-Leal, W. Modulation of microglial activation enhances neuroprotection and functional recovery derived from bone marrow mononuclear cell transplantation after cortical ischemia. Neurosci. Res. 73, 122–132 (2012).
Hanlon, L. A., Raghupathi, R. & Huh, J. W. Depletion of microglia immediately following traumatic brain injury in the pediatric rat: Implications for cellular and behavioral pathology. Exp. Neurol. 316, 39–51 (2019).
Wang, C. et al. Increased level of exosomal miR-20b-5p derived from hypothermia-treated microglia promotes neurite outgrowth and synapse recovery after traumatic brain injury. Neurobiol. Dis. 179, 106042 (2023).
Batchelor, P. E. et al. Macrophages and microglia produce local trophic gradients that stimulate axonal sprouting toward but not beyond the wound edge. Mol. Cell. Neurosci. 21, 436–453 (2002).
Parkhurst, C. N. et al. Microglia promote learning-dependent synapse formation through brain-derived neurotrophic factor. Cell 155, 1596–1609 (2013).
Dougherty, K. D., Dreyfus, C. F. & Black, I. B. Brain-derived neurotrophic factor in astrocytes, oligodendrocytes, and microglia/macrophages after spinal cord injury. Neurobiol. Dis. 7, 574–585 (2000).
Liu, Y. U. et al. Neuronal network activity controls microglial process surveillance in awake mice via norepinephrine signaling. Nat. Neurosci. 22, 1771–1781 (2019).
Cao, K. et al. Microglia modulate general anesthesia through P2Y12 receptor. Curr. Biol. 33, 2187-2200.e6 (2023).
Schirmer, L., Merkler, D., König, F. B., Brück, W. & Stadelmann, C. Neuroaxonal regeneration is more pronounced in early multiple sclerosis than in traumatic brain injury lesions. Brain Pathol. 23, 2–12 (2013).
Oehmichen, M., Theuerkauf, I. & Meissner, C. Is traumatic axonal injury (AI) associated with an early microglial activation? Application of a double-labeling technique for simultaneous detection of microglia and AI. Acta neuropathologica. 97, 491–494 (1999).
Ryu, J. et al. The problem of axonal injury in the brains of veterans with histories of blast exposure. Acta Neuropathol. Commun. 2, 1–14 (2014).
Biegon, A. Considering biological sex in traumatic brain injury. Front. Neurol. 12, 576366 (2021).
Song, H. et al. Sex differences in the extent of acute axonal pathologies after experimental concussion. Acta Neuropathol. 147, 79 (2024).
Yanguas-Casás, N. Physiological sex differences in microglia and their relevance in neurological disorders. Neuroimmunol. Neuroinflamm. 7, 13–22 (2020).
Martinez-Muniz, G. A. & Wood, S. K. Special section on sexual dimorphism in neuroimmune cells sex differences in the inflammatory consequences of stress: Implications for pharmacotherapy. J. Pharmacol. Exp. Ther. 375, 161–174 (2020).
VanRyzin, J. W., Pickett, L. A. & McCarthy, M. M. Microglia: Driving critical periods and sexual differentiation of the brain. Dev. Neurobiol. 78, 580–592 (2018).
Schwarz, J. M., Sholar, P. W. & Bilbo, S. D. Sex differences in microglial colonization of the developing rat brain. J. Neurochem. 120, 948–963 (2012).
Doran, S. J. et al. Sex differences in acute neuroinflammation after experimental traumatic brain injury are mediated by infiltrating myeloid cells. J. Neurotrauma 36, 1040–1053 (2019).
Acknowledgements
This work would not have been possible without the tissue from the Department of Defense (DoD)/Uniform Services University (USU) Tissue Repository and Neuropathology Core, which is funded by the Department of Defense and is housed within the Center for Neuroscience and Regenerative Medicine.
Funding
This work was funded by NINDS Grants R21 NS126611 and R01 NS128104.
Author information
Authors and Affiliations
Contributions
A.L.W. performed quantitative analysis and wrote the first draft of the manuscript. K.G. captured images for analysis and performed quantitative analysis. A.L. captured images for analysis, organized the data, edited the manuscript, managed the project, and secured funding for the completion of this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Approval for human experiments
The current study was approved by the Virginia Commonwealth University Institutional Review Board under IRB ID HM20029279 and was determined not to be research involving human subjects as defined by DHHS and FDA regulations. The Department of Defense (DoD)/Uniform Services University (USU) Tissue Repository also approved the use of these tissues for this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Logan-Wesley, A.L., Gorse, K.M. & Lafrenaye, A.D. Microglial process convergence onto injured axonal swellings, a human postmortem brain tissue study. Sci Rep 14, 21369 (2024). https://doi.org/10.1038/s41598-024-71312-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71312-7
- Springer Nature Limited