Abstract
Vitamin A plays a critical role in various biological functions, including vision, cellular differentiation, and immune regulation. However, accurately assessing its status, particularly in obese individuals, presents challenges due to potential alterations in metabolism and distribution. This study utilized Liquid Chromatography–Tandem Mass Spectrometry (LC–MS/MS) methodology to precisely measure serum vitamin A concentrations in population of UAE. The methodology's reliability and precision, as demonstrated through validation procedures, underscore its potential utility in clinical settings. Employing the Multiple Reaction Monitoring mode of positive ion electrospray ionization, the LC–MS/MS system achieves a limit of detection (LOD) of 0.48 ng/mL in serum, while adhering to FDA-US regulations for accuracy and compliance. A key aspect of this study was the application of LC–MS/MS to assess vitamin A status in an obese population within UAE. By employing a diverse cohort of 452 Emirati participants, including 277 individuals from a randomized controlled trial who were assessed at baseline and at 6th month, and 175 healthy individuals aged 18–82 assessed at baseline, this study explores the relationship between obesity and vitamin A levels, shedding light on potential implications for health and well-being. It was an observational study based on a new vitamin A method and participants were asked to eat vitamin A rich foods. The robust performance of the LC–MS/MS methodology positions it as a valuable tool for clinical research. By accurately quantifying vitamin A levels in human serum, this methodology opens avenues for advancing our understanding of vitamin A physiology and its implications for health, particularly in obese populations. In summary, this LC–MS/MS methodology presents a potent tool for clinical studies, providing reliable, specific, and robust detection of vitamin A in human serum, thus, opening a new frontier for advancing our understanding of vitamin A related physiology and health in the obese population.
Similar content being viewed by others
Introduction
Vitamin A is a fat-soluble essential nutrient that plays a crucial role in maintaining various physiological functions within the human body. Retinal, retinol, and retinoic acid are the most active and biologically related substances that comprise vitamin A1. These forms are collectively known as retinoids. Vitamin A is mainly obtained from dietary sources, including animal products like liver, fish, and dairy, as well as from certain plant-based sources in the form of provitamin A carotenoids. β-Carotene, a plant-based precursor to vitamin A that is abundant in carrots, is found in all living things. An enzyme known as β-carotenoid-15,15'-dioxygenase in the body converts β-carotene, which has antioxidant properties, into vitamin A. A proper intake of vitamin A is essential for several body processes, including erythropoiesis, gene expression, immunological function, reproduction, physical development, growth, and eyesight2. Vitamin A also plays a significant role in maintaining healthy vision. Moreover, vitamin A also participates in the regulation of glucose and fat metabolism. Deficiencies in vitamin A could potentially contribute to the development of metabolic disorders like diabetes and obesity3.
The required amount of vitamin A varies based on age, gender, health status, and pregnancy. The Recommended Dietary Allowance (RDA) set by the Food and Nutrition Board of the Institute of Medicine ranges from 0.3 to 0.9 mg per day. To ensure sufficient vitamin A intake, it is advisable to consume a balanced diet rich in fruits, and vegetables, particularly those with vibrant colours like carrots, sweet potatoes, and leafy greens.
Retinol levels within the body are influenced by various factors. Increased levels of retinol are associated with advancing age and high body mass index4,5. The association between BMI and vitamin A levels may be influenced by several factors, including dietary intake, adipose tissue distribution, and metabolic processes. While adipose tissue can serve as a reservoir for fat-soluble vitamins such as vitamin A, the relationship between BMI and vitamin A status is complex and may be influenced by various confounding variables. These changes could be attributed to enhanced absorption in the intestines and reduced elimination. Retinol levels in blood are a measure of vitamin A status in the body. Normal levels of vitamin A range from 200 to 600 ng/mL. Retinol levels may vary slightly among different laboratories and test methods6,7,8.
Obesity can bring about alterations in the absorption and metabolism of nutrients, including vitamin A. The digestive process and metabolic functions can be disrupted by obesity, thereby affecting the body's ability to effectively absorb and utilize certain nutrients9. Factors such as inflammation, oxidative stress, and metabolic dysfunction commonly associated with obesity can impact the utilization and metabolism of vitamin A within the body, potentially leading to suboptimal health despite elevated levels10. These factors can potentially deplete vitamin A, along with other essential antioxidant nutrients, thereby further exacerbating the lower levels of vitamin A in obese individuals.
Regarding the impact of vitamin A on obesity itself, the relationship is intricate and multi-faceted. As obesity leads to an increase in adipose tissue, it may result in the sequestration of more vitamin A within the fat stores. Consequently, this trapped vitamin A becomes less bioavailable for the rest of the body to utilize. Vitamin A itself can impact obesity through its involvement in adipose tissue development, regulation of satiety, and modulation of glucose and fat metabolism11. By comparing the levels of vitamin A in the blood of obese individuals and normal weight (healthy) individuals, this research aims to investigate whether there is a significant difference between the groups or not.
There has been a lot of research done on measuring vitamin A levels in the human body. The most widely used techniques to assess vitamin A status are serum concentrations of retinol, retinyl esters, and carotenoids12,13. Numerous analytical techniques can be employed for the preprocessing and analysis of vitamins. There are several preprocessing techniques, including liquid–liquid extraction, dispersive liquid–liquid microextraction, solid-phase extraction, ultrasonic-assisted extraction. Various approaches, such as chromatography techniques, microbiological assays, biosensors, immunoassays, electrophoretic methods, and other techniques, are utilized for the determination analysis14,15,16,17,18,19. In a variety of matrices, liquid chromatography (LC) provides a wide range of both qualitative as well as quantitative analytical advantages20. LC–MS/MS methods enable the separation of samples based on their polarity and mass-to-charge (m/z) ratios. Additionally, this method offers low limits of quantitation (LOQ), resulting in heightened sensitivity. Midttun et al.7 successfully quantified three types of vitamins in a small volume of human plasma simultaneously using HPLC–MS/MS, demonstrating its applicability for analyzing vitamins in biological preparations19,21,22.
However, while numerous studies have employed LC–MS/MS methods for quantifying vitamin A in human serum, there remains a need to apply these methods specifically to populations where obesity is prevalent, such as in the UAE. The study was initiated in the UAE population to address a gap in understanding how obesity affects vitamin A metabolism and distribution, which are crucial for various biological functions. Given the global rise in obesity rates and its association with nutrient malabsorption and alteration in metabolism, it became imperative to investigate vitamin A status in this demographic. Additionally, considering the significant role of vitamin A in immune regulation, vision, and cellular differentiation, assessing its status in obese patients could offer insights into potential implications for health and well-being, particularly in a population with increasing obesity rates. Hence, the aim of this study was to develop and validate a sensitive, and easy LC–MS/MS-based assay with a simplified liquid–liquid extraction method for measuring vitamin A in human serum and use this method to measure vitamin A in healthy and obese Emirati individuals. This approach ensured that our study could effectively address the research questions regarding vitamin A status in different population groups, contributing valuable insights to the field of nutritional research and clinical practice.
Chemicals and reagents
Retinol, deuterated 25-hydroxyvitamin D3 (6, 19, 19-d3) (Internal standard), and albumin derived from human serum were obtained from Green Oasis Medical Equipment Installation and Maintenance (Gomet). The necessary chemicals and solvents, such as phosphate-buffered saline, methanol, deionized water, hexane, ethyl acetate, formic acid, ammonium format, LC–MS-grade water, and LC–MS-grade methanol, were acquired from Emirates Scientific and Technical Supplies L.L.C in Abu Dhabi (ESTS). To conduct the analysis, an Ascentis Express F5 column measuring 150 mm × 2.1 mm × 2.7 um was purchased from LABCO LLC.
Preparation of standard solutions
To prepare the standard solution of retinol and 25-hydroxyvitamin D3 (6, 19, 19-d3) (internal standard), ethanol was employed to dissolve the standards to obtain 1 mg/mL concentration of standard solution. The decision for using deuterated 25-hydroxyvitamin D3 (6, 19, 19-d3) rather than a stable isotope of retinol as the internal standard, was primarily influenced by considerations of availability and cost-effectiveness. The stock solutions were then stored in amber vials at − 20 °C to prevent degradation. For the subsequent preparation of the working solutions, the stock solutions were diluted and mixed with methanol solvent, ensuring the desired concentration was attained for analysis. During the laboratory procedure, measures were taken to ensure the integrity of the working solutions. All processing steps were performed under ice-cold conditions and monochromatic light, effectively preventing decomposition and preserving the stability of the samples throughout the preparation process23,24,25.
Samples collection
Blood samples were collected from 277 Emirati individuals identified as obese patients at baseline and follow-up. Using WHO cut-off points for BMI, the baseline group included 65 individuals (25%) with normal BMI, 92 individuals (35%) who were overweight, and 106 individuals (40%) with obesity, resulting in 277 baseline samples and 277 follow-up samples. Additionally, 175 healthy control volunteers participated in the study, comprising 73 males aged between 18 and 82 years and 204 females aged between 18 and 65 years. This was an observational study, and the objective was the newly developed method for vitamin A analysis. Participants were also advised to incorporate Vitamin A-rich foods into their diets, such as carrots, sweet potatoes, spinach, and kale. Whereas healthy participants were not given any supplements and served as a reference group.
The blood samples from the study group were collected in vacutainer tubes and individually labelled. Subsequently, they underwent centrifugation at 1500×g to separate the serum, which was then extracted. Following extraction, the serum samples were individually aliquoted into labelled plastic amber vials and stored at − 80 °C for further analysis. The Research Ethics Committee, UAEU granted and approved the ethics of the study under Protocol number AAHEC-3-17-055 for the recent study samples. All included participants gave informed consent. All methods have been carried out in accordance with the guidelines provided by the US Food and Drug Administration (FDA) for method validation26. We recruited participants through local press advertisements, community health centres, and hospital outpatient clinics. Exclusion criteria encompassed renal disease, hypercalcaemia, intake of calcium and/or vitamin D supplements, bisphosphonates, steroid medications, hormones or diuretics, and inability to give informed consent. This study did not include a placebo control group. It was designed as a preliminary investigation to assess the effects of the multivitamin supplement containing Vitamin A. The primary aim was to gather initial data, which will inform the design of a more comprehensive, placebo-controlled trial in the future.
Post-consent, we collected blood samples from eligible participants for Vitamin A metabolite measurements and detection of inflammatory and metabolic risk markers. Participants completed a face-to-face questionnaire about lifestyle and health factors relevant to vitamin A deficiency implications in UAE citizens. The questionnaire captured education and socio-economic status, employment history, previous illnesses or surgeries, smoking and drinking habits, physical activity, reproductive history, use of herbal medicine, vitamin supplements, and exogenous hormones for contraception and post-menopause. We obtained anthropometric data (body weight, height, and BMI) using a Tanita body composition analyser. Using the World Health Organization's sex-adjusted BMI cut-off points, we classified participants with a BMI of 18.5–24.9 as normal, 25–29.9 as overweight, and 30 or above as obese.
Method of extraction
The extraction procedure was developed through a simplified liquid–liquid extraction method, carefully designed to ensure efficiency and effectiveness in isolating vitamin A from human serum samples. The human serum samples were stored at a temperature of − 80 °C in a deep freezer. They were allowed to defrost at room temperature for the analysis to be commenced. In order to process the samples, 500 µl of serum samples were placed in a borosilicate glass culture tube measuring 16 × 100 mm, with a capacity of 14 mL. Then, a solution containing 20 µl of internal standard at a concentration of 1 µg/mL was added to spike the samples. Subsequently, the internal standard and a portion of the serum sample solution were mixed vigorously for 1 min using a vortex mixer. Next, a mixture of hexane and ethyl acetate in a ratio of 9:1, totalling 3.0 mL, was added to extract vitamin A and internal standard from the plasma samples. The resulting mixture was vortexed briefly and then subjected to centrifugation at 4000 rpm for 20 min at 4 °C. Following centrifugation, the 2.5 mL of supernatant was carefully separated and dried using a sample concentrator at 40 °C for 15 min with a continuous flow of Nitrogen. In order to reconstitute the dried samples, 100 µl of methanol graded for LC–MS/MS was added. The samples were then put into amber vials designed especially for LC–MS/MS, which were then put in an autosampler that was set at 4 °C. For the LC–MS/MS analysis, a volume of 5 µl from the sample extract was injected into the instrument27. The optimization of this procedure was driven by the goal of achieving high recovery rates and precise quantification of vitamin A levels. This was accomplished by thorough validation procedures that demonstrated the reliability of the LC–MS/MS methodology. The validation procedure includes a series of experiments designed to ensure the accuracy, precision, sensitivity, and reproducibility of our LC–MS/MS method. The selection of solvents and conditions were tailored to maximize the yield of vitamin A while minimizing potential interference or degradation. The final optimized conditions were validated through repeated extractions and quantifications to confirm their effectiveness.
LC–MS/MS analysis
The vitamin A chromatogram was obtained using Nexera ultra-high-pressure liquid chromatography (UHPLC) system manufactured by Shimadzu in Japan. The chromatogram was conducted on a reversed-phase C18 Ascentis Express column, which had the following specifications: a particle size of 2.7 µm and dimensions of 15 cm in length and 2.1 mm in inner diameter. To ensure optimal performance, a guard column was connected to the C18 column for physical filtration. Throughout the analysis, the column temperature was maintained at 30 °C, and the mobile phase flowed through the UHPLC system at a rate of 0.5 mL/min27.
For the analysis, two distinct mobile phases were employed. The mobile phase A consisted of 0.1% formic acid in 5 mM ammonium formate. Mobile phase B consisted of 0.1% formic acid in methanol. Various combinations of mobile phases were tested to optimize the separation and detection of vitamin A. The chosen composition provided the best balance of resolution, peak shape, and sensitivity. The gradient for the mobile phase was established in the following manner: Initially, the mobile phase B was set at 75% for a duration of 11 min, while the mobile phase A remained at 25%. Subsequently, between 11 and 15 min, the mobile phase B was raised to 100% and maintained at that level until the 16th minute. During this time, the mobile phase A decreased to 0%. From 16:00 to 16:10 min, the percentage of mobile phase A increased to 25% while the percentage of mobile phase B decreased to 75%. These percentages were maintained until the 20th minute, marking the conclusion of the mobile phase gradient (Fig. S1)27. The extended run time was implemented to ensure thorough separation and elution of all potential interfering substances, as well as to maintain the robustness and reproducibility of the method. This approach was critical to prevent carry-over effects and to guarantee the high quality and reliability of our results.
The Shimadzu model 8060, equipped with a triple quadrupole mass spectrometry system, was employed to perform the analysis. The mass spectrometer operated in positive electrospray ionization (ESI) mode, which offers advantages over negative ESI mode and other ionization techniques, such as atmospheric pressure chemical ionization (APCI). Specifically, positive ESI mode provides improved ion signal intensity and reduced noise for vitamin A analysis, which is critical for detecting low concentrations with high accuracy28,29. The data obtained were analyzed using Shimadzu's Lab Solutions software27. The MS parameters and conditions utilized in this study were carefully optimized to ensure accurate and reliable measurements. During the drying process, the nebulizing gas flow rate was set at 2 L/min, while the drying and heating gas flow was maintained at 8 L/min with an interface temperature of 300 °C. The heating block temperature was set to 400 °C during the analysis. These parameters were chosen to maximize sensitivity and precision in the detection of vitamin A concentrations in human serum.
Method validation
The validation process has been carried out in accordance with the guidelines provided by the US Food and Drug Administration (FDA) for method validation. The purpose of this validation was to assess the stability, recovery, accuracy, specificity, precision, and linearity26. To prepare the calibration curves and quality control (QC) samples, a blank serum was prepared using a published recipe that involved mixing human serum albumin with phosphate-buffered saline at a concentration of 50 g/L27. Four control limits, known as QCs, were established at different concentrations: a higher quality control limit (QCH) at 800 ng/mL, a medium quality control limit (QCM) at 400 ng/mL, a lower quality control limit (QCL) at 200 ng/mL, and a lower limit of quantification (LLOQ) at 100 ng/mL by spiking the retinol into serum. These QC’s were analyzed to determine the linearity, intra-day and inter-day precision, and accuracy of the vitamin A assays. Each validation included six controls at each concentration level (QCH, QCM, QCL, and LLOQ), along with a calibration curve.
The recovery experiment involved spiking the six quality control samples at the three different concentrations (800 ng/mL, 400 ng/mL, and 200 ng/mL) with mobile phase followed by extraction experiment conducted using blank serum samples spiked with quality controls at the same concentrations, and the recovery was calculated and compared using the peak area results (or area under the normal curve). Additionally, a stability experiment was conducted by subjecting the spiked quality controls to three freeze/thaw cycles at 0 h, 24 h, 48 h, and 72 h, and examining six controls at each concentration level. The standards were utilized to evaluate the average, intra/inter-day accuracy, specificity, recovery, and intra/inter-day precision. The values for these parameters were calculated using approved equations. The percentage of intra/inter-day accuracy of the assay for QC values was calculated using the equation [(mean value/nominal value) × 100]. The percentage of intra/inter-day precision (% CV) values from QC values was calculated using the equation [(standard deviation/mean) × 100]. The percentage of absolute recoveries was calculated using the equation [(mean unextracted QC values/mean extracted QC values) × 100]. The lower limit of detection (LOD) refers to the lowest concentration of an analyte that can be reliably detected, determined by correlating the signal-to-noise ratio with the analyte's lowest concentration. The LOD was calculated using the signal-to-noise (S/N) approach, reducing the analyte concentrations until a response equivalent to three times the detected background level was achieved. The generally accepted detection limit for the signal-to-noise ratio is three.
Results and discussion
Validation results
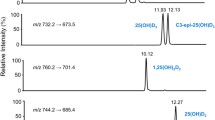
To ensure reliable outcomes, we employed a total of eight blank serum quality control (QC) samples in our study. These included six normal serum lots, one haemolyzed lot, and one lipemic lot. The use of these varied QC samples was aimed at assessing potential interference at the analyte retention time (RT). The inclusion of hemolyzedo99o and lipemic samples, in addition to normal serum, allowed for a comprehensive evaluation of the method's robustness under different physiological conditions. No interference was observed at the analyte RT for any of these eight lots, confirming the method's reliability and specificity. This validation step ensures that LC–MS/MS method provides accurate and reproducible measurements of vitamin A in human serum, irrespective of sample variability. The chromatograms in Fig. 1 represent the chromatograms of analyte and internal standard 25-hydroxyvitamin D3 (6, 19, 19-d3) and includes essential information such as the retention time and the application of multiple reaction monitoring (MRM). To detect vitamin A and the internal standard, specific m/z values and fragmentation patterns were targeted. The precursor ion for vitamin A ([M–H2O + H]+) was monitored at m/z 269.25, while the internal standard 25-hydroxyvitamin D3 (6, 19, 19-d3) was monitored at m/z 386.35. The targeted m/z values, fragmentation patterns, and daughter ions are summarized in Table 1. These distinct fragmentation patterns were essential for ensuring the accurate and specific detection of each compound in the LC–MS/MS analysis.
The MRM mode was employed to monitor precursor ions that exhibited the highest sensitivity. These ions were primarily observed when the retinol Vitamin molecule underwent the loss of a water molecule, along with the most sensitive product ions. In order to optimize the MRM parameters for each analyte, a direct infusion technique was utilized, involving both standard compound mixtures and individual solutions. The precursor ions were identified by infusing standards into the mass spectrometer and monitoring for the most intense ion signals. Fragmentation patterns were determined by adjusting the collision energy to produce the most abundant and distinct product ions. The validity of the selected MRM transitions was confirmed using Shimadzu's Lab Solutions Optimizer software. Table 1 provides a comprehensive illustration of the collision energies, precursor ions, and product ions for both vitamin A and the internal standard.
The specificity of the validation has been determined by utilizing numerous blank serum QC samples. Extraction and analysis of the blank serum QC sample were performed to carry out this evaluation. The overlay of peaks from the analysis was conducted to examine the presence of any interfering or co-eluting peaks at the specific retention times of the analytes (Fig. S2). Notably, no interfering co-eluting peaks were observed for vitamin A.
Calibration curve
To establish the calibration curve and ensure quality control, a blank serum was employed. Phosphate-buffered saline was combined with human serum albumin at a specific concentration of 50 g/mL. The analytes exhibited a favourable linear range spanning from 7.8125 to 1000 ng/mL, with an excellent regression value of (R2 = 0.999) (Fig. S3). The quantification of vitamin A was based on the standard practice of using the ratio of the peak areas of the analyte to the peak areas of internal standards. This approach ensured robust and accurate measurement of vitamin A concentrations in the analyzed samples, thereby enhancing the reliability and validity of our findings.
Table 2 provides information of concentrations, and criteria at different quality control levels. It includes intra-day and inter-day precision and accuracy results, limit of detection (LOD) values, and linear range in ng/mL. It summarizes the MRM transitions and their corresponding parameters. The validation method parameters meet the acceptable range for three QC levels. Accuracy and precision indicate that the method used for vitamin A metabolite analysis is highly reliable, with accuracy close to 100% and precision ranging from 0.07 to 0.29 for all concentrations. The recovery percentage demonstrates the efficiency of the extraction method for extracting vitamin A metabolites from serum samples.
Various studies have reported different LOD and LOQ values. For instance, Plozza et al. reported LOQ values of 0.1 μg/100 mL for all-trans-retinol. Midttun and Uelan reported an LOD of 0.1 μM for all-trans-retinol16. Santos et al. reported LOD and LOQ values of 0.07–170 ng/mL and 0.2–520 ng/mL, respectively17. Gentili et al. reported LOD values of 0.9–15.6 μg/L and LOQ values of 2.7–46.8 μg/L20.
Figure 2 illustrates stability tests conducted over different time periods (24 h, 48 h, and 72 h) incorporating three freeze–thaw cycles in comparison to the initial time point. The graph presents the percentage of change for four concentration levels (800 ng/mL, 400 ng/mL, 200 ng/mL, and 100 ng/mL) used to assess vitamin A stability in serum. The stability of vitamin A exhibited a percentage change ranging from 0 to 3%. Vitamin A exhibited a maximum percentage change of 0.08% after 24 h of the third freeze cycle. The error bars displayed on the graph illustrate the standard errors of the mean. This comprehensive analysis allows for a thorough examination of the sample's stability under different time intervals, providing valuable insights into the robustness and reliability of the experimental procedures employed in the study.
Results of obese Emirati samples
Vitamin A concentrations for clinical interpretation are categorized into several groups based on the literature30. Concentrations of Vitamin A falling below 200 ng/mL are classified as deficient, while the range of 200–600 ng/mL is considered optimal. Concentrations ranging from 600 to below 1000 ng/mL are identified as high, whereas levels equal to or surpassing 1000 ng/mL indicate hypervitaminosis A. The designed classification schema offers a precise framework for analyzing and interpreting vitamin A levels in our study group. Throughout the analysis and discussion, these benchmarks were utilized to evaluate the obtained results.
The analysis of serum samples using validated LC–MS/MS method from the Emirati population in the UAE is presented in Fig. 3A,B. These figures focus on female and male patients respectively highlighting the obese baseline and follow-up samples, as well as healthy controls. It should be noted that the baseline and follow-up samples had a female-to-male ratio of 2.8:1, due to a higher proportion of female patients returning for follow-up sessions.
Figures 3 present the box and whisker plots for vitamin A concentrations among female and male participants, respectively. The data show the distribution of vitamin A levels, including the median, quartiles, and potential outliers, providing a comprehensive view of the variability within each group. Figure 3A displays the vitamin A concentrations in obese female participants at baseline (N = 204), follow-up (N = 204), and healthy volunteers (N = 175). The box and whisker plots illustrate that the median vitamin A levels increased significantly from baseline to follow-up after supplementation. Appropriate statistical analysis was carried out based on the characteristics of our data for male and female combined. One way analysis of variance (ANOVA) was carried out for comparing the three groups. Statistical analysis indicates a significant difference among the means of the three groups (p < 0.0001), confirming the effectiveness of the supplementation in raising vitamin A levels. The Brown-Forsythe and Bartlett's tests confirmed homogeneity of variances (P > 0.05). Similarly, Fig. 3B shows the vitamin A concentrations in obese male participants at baseline (N = 73), follow-up (N = 73), and healthy volunteers (N = 175). Similar to the female participants, the male participants also exhibited a significant increase in vitamin A levels from baseline to follow-up. The one-way ANOVA results (P < 0.0001) indicate a significant difference among the groups. Tukey’s post hoc test was carried out which shows that there is a significant difference between specific baseline and follow up groups. This means that there is a significant difference in vitamin A levels before and after supplementation.
Upon examining the baseline volunteers, it becomes evident that the baseline female samples exhibited lower average concentrations of vitamin A, as compared to that of male samples. The vitamin A levels in baseline female samples had an average of 372 ng/mL. However, a significant number of individual samples fell below the acceptable lower limit of 200 ng/mL, indicating a high prevalence of deficiency within the cohort. However, after undergoing vitamin A supplementation, the follow-up samples (N = 204) demonstrated an increase to average concentration of vitamin A of 440 ng/mL. In contrast, the male sample (N = 73) results remained within the acceptable upper and lower limits, with average concentration ranging from 438 to 600 ng/mL for baseline and follow-up samples. Among the healthy participants aged between 18 and 65 years, the sample size was smaller compared to the baseline and follow-up samples, consisting of 175 individuals. Notably, the male participants achieved an exceptionally high vitamin A level of 1045 ng/mL, while the corresponding value for females was 702 ng/mL. These findings clearly indicate that both female and male vitamin A concentrations increased after supplementation (372–440 ng/mL for female sample and 438–540 ng/mL for male sample), reaching a satisfactory level in the participants.
Figure 4 provides a comparative overview of vitamin A concentrations at baseline, follow-up, and in healthy samples for both male and female participants combined. The combined data emphasize the substantial increase in vitamin A levels post-supplementation, highlighting the intervention's effectiveness. A comparative overview of vitamin A concentrations reveals distinct levels across baseline, follow-up, and healthy samples. In the baseline group, comprising 277 samples, the mean concentration of vitamin A was 389 ng/mL with a standard deviation of 215. In contrast, follow-up samples, also comprised of 277, exhibited a higher mean concentration of 466 ng/mL, with a standard deviation of 232. Notably, healthy individuals, represented by 175 samples, demonstrated substantially elevated levels of vitamin A, with a mean concentration of 717 ng/mL and a standard deviation of 344.
These findings suggest that the variations in vitamin A status observed among individuals over time and between healthy and obese populations are primarily due to the supplementation. This highlights the importance of investigating factors influencing vitamin A levels and their health implications. We have established through our detailed analysis that vitamin A levels significantly increase post-supplementation in obese patients on individual level (Fig. S4). This finding underscores the potential efficacy of Vitamin A supplementation in rectifying inadequacies within this demographic, particularly considering obesity's known impact on nutrient metabolism. While our study observed increased vitamin A levels post-supplementation, further research is needed to consider whole health outcomes and individual-level impacts.
In doing so, we hope to refine dietary recommendations and supplementation strategies, ensuring they cater to the specific needs of individuals, thereby enhancing public health strategies and clinical practices related to nutritional management. Intervention studies should be conducted to assess the effectiveness of vitamin A supplementation in improving health outcomes by randomly assigning participants to control and intervention groups.
Conclusion
In summary, the aim of the current study was to validate an LC–MS/MS-based method for accurately measuring vitamin A levels in the serum of both healthy and obese individuals in the Emirati population. The findings indicate that the LC–MS/MS method used was suitable and reliable for quantifying of vitamin A in human serum. The stability of vitamin A In serum ranged from 0 to 3%, and the optimal MS/MS parameters, including precursor and product ions, were determined to ensure precision in measurement. A total of 277 Emirati patients (75% were obese or overweight) were sampled for the baseline and followed up over time. The vitamin A levels in baseline female samples were below the acceptable lower limit of 200 ng/mL for many individuals, with an overall average level of 372 ng/mL. While the average was above 200 ng/mL, a significant number of samples still fell below this threshold. On average, the vitamin A levels in both male and female samples remained within the acceptable range, although individual variations were observed. The combined healthy sample, including both males and females, showed an average vitamin A level of 718 ng/mL. The statistical analysis affirms the robustness and reliability of the observed differences, underscoring the importance of addressing vitamin A deficiency through targeted interventions. This method is suitable for clinical studies involving vitamin A analysis in human serum, which can help assess the vitamin A status and nutritional needs of different populations and groups.
This research is not merely a routine application of an established method but a deliberate choice to fill a gap in nutritional research within a population where obesity is a growing concern. We specifically focused on the obese Emirati population; a demographic often underrepresented in nutritional research. This focus allowed us to address the unique challenges faced by this group, providing valuable data that can inform public health strategies in the UAE and similar regions. Our research involved assessment of vitamin A levels before and after supplementation, highlighting the potential for tailored nutritional interventions to address deficiencies. By demonstrating the efficacy of vitamin A supplementation in increasing serum retinol levels among obese individuals, our study provides a foundation for developing targeted nutritional guidelines. These guidelines can help mitigate the risk of deficiency and improve overall health outcomes in obese populations.
Future perspectives
In addition to examining the variations in vitamin A levels between healthy individuals and those with specific diseases or health conditions. Future research endeavours can explore the broader functional outcomes associated with vitamin A levels. Exploring the functional outcomes, such as immune function and vision health, linked to vitamin A levels can provide valuable insights into its physiological effects and overall impact on health. Conducting comparative studies in the future could investigate variations in vitamin A levels between healthy individuals and those with specific diseases or health conditions. By expanding the scope of our method to encompass a broader range of metabolites, future research endeavours could provide a more comprehensive understanding of metabolic profiles and their associations with various health outcomes.
Data availability
Samples of data and materials are available upon request to the corresponding author.
References
Herschel Conaway, H., Henning, P. & Lerner, U. H. Vitamin a metabolism, action, and role in skeletal homeostasis. Endocrine Rev. 34, 766–797. https://doi.org/10.1210/er.2012-1071 (2013).
Dror, D. K. & Allen, L. H. Retinol-to-fat ratio and retinol concentration in human milk show similar time trends and associations with maternal factors at the population level: A systematic review and meta-analysis. Adv. Nutr. 9, 332S-346S (2018).
Zhang, Y., Wang, T., Hu, X. & Chen, G. Vitamin A and Diabetes. https://home.liebertpub.com/jmf. 24, 775–785 (2021).
Ballew, C., Bowman, B. A., Sowell, A. L. & Gillespie, C. Serum retinol distributions in residents of the United States: third National Health and Nutrition Examination Survey, 1988–1994. Am. J. Clin. Nutr. 73, 586–593 (2001).
Gillespie, C., Ballew, C., Bowman, B. A., Donehoo, R. & Serdula, M. K. Intraindividual variation in serum retinol concentrations among participants in the third National Health and Nutrition Examination Survey, 1988–1994. Am. J. Clin. Nutr. 79, 625–632 (2004).
Penniston, K. L. & Tanumihardjo, S. A. The acute and chronic toxic effects of vitamin A. Am. J. Clin. Nutr. 83, 191–201 (2006).
Kraskinski, S. D. et al. Relationship of vitamin A and vitamin E intake to fasting plasma retinol, retinol-binding protein, retinyl esters, carotene, alpha-tocopherol, and cholesterol among elderly people and young adults: Increased plasma retinyl esters among vitamin A-supplement users. Am. J. Clin. Nutr. 49, 112–120 (1989).
Olson, J. A. Hypovitaminosis A: Contemporary scientific issues. J. Nutr. 124, 1461S-1466S (1994).
Sundaram, S. & Borthakur, A. Altered intestinal epithelial nutrient transport: an underappreciated factor in obesity modulated by diet and microbiota. Biochem. J. 478, 975–995 (2021).
Brahma, M. K. et al. Oxidative stress in obesity-associated hepatocellular carcinoma: sources, signaling and therapeutic challenges. Oncogene 40, 5155–5167 (2021).
Coronel, J., Pinos, I. & Amengual, J. β-carotene in obesity research: Technical considerations and current status of the field. Nutrients 11, 842 (2019).
Blaner, W. S. Vitamin A and provitamin A carotenoids. Present Knowl. Nutr. 1, 73–91. https://doi.org/10.1016/B978-0-323-66162-1.00005-6 (2020).
Sombié, O. O. et al. A comparative study on indicators of vitamin A status and risk factors for sensitivity and specificity of the methods to detect vitamin A deficiency. Nutr. Metab. (Lond) 20, 1–11 (2023).
Zhang, Y. et al. A review of the extraction and determination methods of thirteen essential vitamins to the human body: An update from 2010. Molecules 23, 1484 (2018).
Albarhani, A. A. et al. Vitamins D and A can be successfully measured by LC–MS/MS in cord blood diluted plasma. Clin. Biochem. 48, 1105–1112 (2015).
Midttun, Ø. & Ueland, P. M. Determination of vitamins A, D and E in a small volume of human plasma by a high-throughput method based on liquid chromatography/tandem mass spectrometry. Rapid Commun. Mass Spectrom. 25, 1942–1948 (2011).
Santos, J., Mendiola, J. A., Oliveira, M. B. P. P., Ibáñez, E. & Herrero, M. Sequential determination of fat- and water-soluble vitamins in green leafy vegetables during storage. J. Chromatogr. A 1261, 179–188 (2012).
Liu, Z., Kang, X. & Fang, F. Solid phase extraction with electrospun nanofibers for determination of retinol and α-tocopherol in plasma. Microchim. Acta 168, 59–64 (2010).
Viñas, P., Bravo-Bravo, M., López-García, I. & Hernández-Córdoba, M. Dispersive liquid–liquid microextraction for the determination of vitamins D and K in foods by liquid chromatography with diode-array and atmospheric pressure chemical ionization-mass spectrometry detection. Talanta 115, 806–813 (2013).
Gentili, A. et al. Comprehensive profiling of carotenoids and fat-soluble vitamins in milk from different animal species by LC-DAD-MS/MS hyphenation. J. Agric. Food Chem. 61, 1628–1639 (2013).
Plozza, T., Craige Trenerry, V. & Caridi, D. The simultaneous determination of vitamins A, E and β-carotene in bovine milk by high performance liquid chromatography–ion trap mass spectrometry (HPLC–MSn). Food Chem. 134, 559–563 (2012).
Tai, S. S. C., Bedner, M. & Phinney, K. W. Development of a candidate reference measurement procedure for the determination of 25-hydroxyvitamin D3 and 25-hydroxyvitamin D 2 in human serum using isotope-dilution liquid chromatography tandem mass spectrometry. Anal. Chem. 82, 1942–1948 (2010).
Fu, P. P. et al. Photodecomposition of Vitamin A and Photobiological Implications for the Skin†. Photochem. Photobiol. 83, 409–424 (2007).
Allwood, M. C. The influence of light on vitamin A degradation during administration. Clin. Nutr. 1, 63–70 (1982).
Allwood, M. C. & Martin, H. J. The photodegradation of vitamins A and E in parenteral nutrition mixtures during infusion. Clin. Nutr. 19, 339–342 (2000).
Bower, J. et al. 8th GCC: Consolidated feedback to US FDA on the 2013 draft FDA guidance on bioanalytical method validation. Bioanalysis 6, 2957–2963. https://doi.org/10.4155/bio.14.287 (2014).
Schoenaker, D. A. J. M., Simon, D., Chaturvedi, N., Fuller, J. H. & Soedamah-Muthu, S. S. Glycemic control and all-cause mortality risk in type 1 diabetes patients: The EURODIAB prospective complications study. J. Clin. Endocrinol. Metab. 99, 800–807 (2014).
Bruins, A. P. Mechanistic aspects of electrospray ionization. J. Chromatogr. A 794, 345–357 (1998).
Nasiri, A. et al. Overview, consequences, and strategies for overcoming matrix effects in LC-MS analysis: A critical review. Analyst 146, 6049–6063 (2021).
Olsen, K. et al. Serum retinyl esters are positively correlated with analyzed total liver vitamin A reserves collected from US adults at time of death. Am. J. Clin. Nutr. 108, 997–1005 (2018).
Acknowledgements
We offer our Special thanks to UAEU for sponsoring this research and further thanks to Sampathkumar Elangovan for his technical help.
Funding
The research was funded by Start-Up UAE University, grant number 12S091, SURE UAE University grant number G00003117 to Iltaf Shah and Project Grant from United Arab Emirates University to Salah Gariballa.
Author information
Authors and Affiliations
Contributions
I.S. SG presented the idea, secured the grant, supervised students, and provided the facility. M.K.H. and I.E.K. wrote the first draft and did the practical work along with B.A., J.Y, IS and, S.G. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Research Ethics Committee, UAEU granted and approved the ethics of the study under Protocol number AAHEC-3-17-055 for the recent study samples. All the participants signed the consent form to take part in this study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hakeem, M.K., El-Konaissi, I., Alzohily, B. et al. Evaluating a novel method for vitamin A analysis in an observational study of the UAE's obese population. Sci Rep 14, 20373 (2024). https://doi.org/10.1038/s41598-024-71145-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71145-4
- Springer Nature Limited