Abstract
The exploration of traumatic spinal fractures (TSFs) within the senior demographic has not been thoroughly scrutinized, particularly with respect to variations across genders, age groups, seasonal periods, and causative factors. This retrospective analysis aimed to dissect differences in the prevalence and characteristics of TSFs among the elderly, factoring in gender, age, seasonal timing, and causation. A retrospective analysis was conducted on the medical and imaging records of 1,415 patients, all aged 60 years or older, who were diagnosed with TSFs from 2013 to 2019. This study categorized the data by gender, age groups (60–70, 70–80, and 80 years or older), seasons, and the cause of injuries, including road traffic crashes (RTCs), falls from low heights (LHF), falls from high heights (HHF), and injuries incurred during everyday activities and agricultural labor (DFI). Male patients exhibited notably higher incidences of RTCs, high-height falls (HHFs), outdoor incidents, comas post-injury, fractures of the lower limbs (LLFs), pelvic fractures (PFs), rib fractures (RFs), intra-thoracic injuries (ITIs), intra-abdominal injuries (IAIs), cervical fractures, and spinal cord injuries (SCIs). With advancing age, there was a marked decline in occurrences of RTCs, HHFs, outdoor incidents, RFs, craniocerebral injuries (CCIs), ITIs, cervical fractures, and SCIs, while the incidences of DFIs, indoor incidents, and thoracic and lumbar (T + L) fractures notably increased. During autumn, LLF occurrences were significantly reduced, whereas the winter season saw an increase in thoracic fractures. Spring time was associated with a higher frequency of lumbar fractures and noncontiguous spinal fractures (NSFs). Significant distinctions were observed in the age distribution, injury circumstances, associated injuries, and SCIs between high-energy impacts (RTCs and HHFs) and low-energy traumas (LHFs and DFIs). In the elderly demographic, TSFs exhibited discernible distinctions based on gender, age, seasonal variations, and etiological factors, impacting the nature and circumstances of injuries, associated traumas, complications, fracture sites, and the occurrence of SCIs.
Similar content being viewed by others
Introduction
Aging leads to biomechanical alterations in bone structure, elevating the risk of fractures from falls, whether from standing or sitting heights, among the elderly. The prevalence of such fragility fractures is escalating, heralding significant health repercussions including fractures, mobility reduction, functional impairment, and in severe scenarios, fatality1,2,3,4. Scholarly discourse has recently highlighted traumatic spinal fractures (TSFs) across various populations, encompassing studies from the United States, Switzerland, Ontario, Saudi Arabia, Japan, Finland, and the Netherlands5,6,7,8,9,10,11, with a noted scarcity of data pertaining to China12,13. The discourse extends to examining variances across genders14, the incidence of osteoporosis15, fracture rates amid the COVID-19 pandemic16 and strategies for managing elderly patients with spine trauma17,18,19,20. Research delineates the distinct clinical manifestations of spinal fractures in adults aged 16 to 100, revealing a pronounced correlation between age, gender, fracture localization, and the complexity of spinal fractures21,22.
Research on the disparities in TSFs among the elderly in China, categorized by gender, age, seasonal impacts, and causative factors, remains limited. These fractures represent a significant health burden globally, leading to substantial morbidity and mortality rates. The main global contributors to TSFs include preventable incidents such as traffic collisions and falls. There exists a pressing need for comprehensive studies aimed at mapping the occurrence and determinants of TSFs across various geographical and socio-economic settings, particularly in countries with lower and middle income levels23. A detailed examination of the variations in associated injuries, complications, and spinal cord injuries (SCIs) based on demographic characteristics can enhance our understanding of the necessity for rapid, accurate diagnosis and treatment. Moreover, it underscores the importance of developing strategies for the prevention and management of complications and SCIs. Such insights are crucial for optimizing the allocation of healthcare resources and improving patient outcomes.
This investigation examined and analyzed cases from multiple tertiary hospitals in Chongqing and Shenyang, spanning January 2013 to December 2019. The primary objective was to explore the variances in gender, age, seasonal timing, and causative factors, with a particular focus on the patterns of concomitant injuries, SCIs, and complications in TSFs among individuals aged 60 years and above.
Materials and methods
Study population
Utilizing data from the Military Hospital Information Registry Database, this research was a retrospective cross-sectional analysis covering the period from January 1, 2013, to December 31, 2019. Conducted in alignment with the Declaration of Helsinki, the Northern Theater Command General Hospital's Ethics Committee granted approval for this study. Due to its retrospective and observational nature, and with the assurance that all data were collected and analyzed anonymously, the requirement for informed consent was exempted by the same Ethics Committee.
Patients eligible for this analysis were identified based on the following criteria: (i) evidence of spinal fractures via X-ray, computed tomography (CT), or magnetic resonance imaging (MRI); (ii) admission for spinal fracture treatment during the period from January 1, 2013, to December 31, 2019; and (iii) being aged 60 years or older. Exclusions were made for (i) individuals with fractures caused by pathological conditions such as tumors, tuberculosis, or infections; (ii) those readmitted due to complications at the same fracture site; and (iii) cases with missing data. A retrospective review identified 1,462 elderly patients with spinal fractures presented to our facilities. Of these, 47 were excluded, resulting in 1,415 patients ultimately being incorporated into the research, patients caused by injuries sustained during everyday activities and agricultural labor (DFI) without clear causes maybe suffering from traumatic fractures caused by osteoporosis were included in the current study (Fig. 1).
Evaluation of clinical and radiographic data
Clinical and radiological data of the patients were meticulously examined to document a variety of information, including demographic details, etiology of injuries such as road traffic accidents (RTAs), falls from heights above two meters (HHF), falls from heights below two meters (LHF), and injuries sustained during everyday activities and agricultural labor (DFI) that involved fractures without a clear cause maybe traumatic fractures caused by osteoporosis. Additionally, the season of the injury (spring, summer, autumn, winter), location of the incident (indoor or outdoor), concurrent injuries including fractures of lower limbs (LLFs), upper limbs (ULFs), pelvic fractures (PFs), ribs (RFs) and craniocerebral injuries (CCIs), intra-thoracic injuries (ITIs), and intra-abdominal injuries (IAIs), chronic conditions (heart disease, lung disease, diabetes mellitus), states of unconsciousness post-injury, lifestyle factors (smoking and alcohol consumption), complications such as deep vein thrombosis (DVT), pneumonia, pressure ulcers, urinary infections, and fatalities, site of the fracture, SCIs, and the treatments administered were all recorded.
Statistical analysis
The dataset underwent analysis using SPSS software (version 24.0, SPSS Inc., USA). The decision to use the chi-square test or Fisher's exact test for categorical data hinged on the configuration of the data. A P-value below 0.05 was considered indicative of statistical significance.
Ethical approval
All procedures were in accordance with the ethical standards of the Institutional Research Committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study protocol was approved by the Ethics Committee of the General Hospital of the Northern Theater Command of the Chinese PLA.
Results
General demographic data
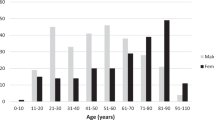
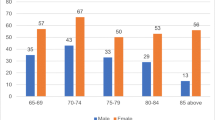
A detailed review of patient files from 2013 to 2019 revealed insights into 1,415 cases of TSFs in the elderly demographic. Analysis showed a gender distribution of 471 males (33.3%) and 944 females (66.7%), with a comprehensive count of 2,172 vertebral fractures. The mean age of patients affected by these spinal fractures was determined to be 70.7 years, with a range from 60 to 94 years old. The data indicated a predominance of spinal fractures in individuals aged between 60 and 70 years, making up 48.5% of the cases. Seasonal analysis revealed that fractures were most frequently reported during the autumn and winter months, with incidences at 26.3% and 26.2%, respectively. The leading causes of these fractures were identified as falls from a low height (40.0%), with the majority of these incidents (52.2%) occurring in outdoor environments. Among the patients, 27 (1.9%) experienced coma subsequent to their injuries, and 157 (11.1%) had additional injuries, with ITIs being the most common at 77 cases (5.4%), followed by CCIs at 48 cases (3.4%). Surgical treatment was administered to 1,027 patients (72.6%), among which percutaneous kyphoplasty (PKP) or percutaneous vertebroplasty (PVP) emerged as the most utilized techniques, accounting for 58.3% of the interventions (Table 1).
Differences according to different genders, ages, seasons and causes
In the male patient group, there was a notably higher occurrence of RTCs, HHFs, outdoor incidents, coma post-injury, LLFs, PFs, RFs, ITIs, IAIs, cervical fracture locations, and SCIs, with statistical significance achieved across these categories (P < 0.001 for most, P = 0.005 for PFs, and P = 0.011 for IAIs) (Table 1, Fig. 2). Age progression showed a marked decrease in the incidences of RTCs, HHFs, outdoor events, RFs, craniocerebral injuries (CCIs), ITIs, cervical fractures, and SCIs. Conversely, there was a significant increase in daily life and DFIs, indoor occurrences, and T + L fracture locations (Table 2, Fig. 3). In the autumn cohort, a lower frequency of LLFs was observed, whereas the winter group saw a rise in thoracic fracture locations. The spring cohort experienced an increase in lumbar fracture locations and NSFs (Table 3, Fig. 4). A distinct variation was evident between the incidences of high-energy (RTCs and HHFs) and low-energy (LHFs and DFIs) damage across different age groups, injury settings, associated injuries, and SCIs (Table 4, Fig. 5).
Distribution of SCI and fractured levels
Out of the total, 221 patients (15.6%) experienced SCIs. According to the American Spinal Injury Association (ASIA) classification, a subset of 51 patients (3.6% of the overall cohort) had complete motor and sensory loss (ASIA A). Furthermore, there were ten individuals (0.7%) who had complete motor loss but retained some sensory functions (ASIA B), 27 patients (1.9%) who had limited motor functionality (ASIA C), 133 patients (9.4%) who maintained useful motor functionality (ASIA D), and a large majority, 1,194 patients (84.4%), who showed no neurological deficits. Notably, SCI occurrences, particularly ASIA A injuries, were significantly more frequent among male patients, those aged between 60 and 70, and those who sustained injuries from high-energy impacts (Fig. 6). The study encompassed 1,415 participants, presenting with a total of 2,172 vertebral fractures, which were distributed across five anatomical regions: cervical (C1-C7) in 153 vertebrae, thoracic (T1-T10) in 365 vertebrae, thoracolumbar (T11-L2) in 1,317 vertebrae, and lumbar (L3-L5) in 337 vertebrae. A higher incidence of cervical vertebra fractures was observed in male patients and those injured due to high-energy impacts, compared to their female counterparts and those with low-energy-related injuries (Fig. 7).
Discussion
In the current study, we utilized data from the Military Hospital Information Registry Database to do this research. The Military Hospital Information Registry Database is the electronic medical record system used in the military hospitals, and the patients treated in the hospitals came from society. The roles of patients and types of disease admitted to military hospitals and non-military hospitals were basically the same. The highest incidence of spinal fractures among elderly patients was observed in the 60–70 year age group, representing 48.5% of cases. As the demographic continues to age, an upward trend in the incidence of spinal fractures among elderly individuals, particularly in older women, is anticipated. The male subgroup showed a markedly higher incidence of injuries from high-energy impacts, including LLFs, PFs, RFs, ITIs, IAIs, cervical fractures, and SCIs. With the population's aging, there was a significant reduction in the frequency of high-energy injuries, outdoor incidents, RFs, craniocerebral injuries CCIs, ITIs, cervical fractures, and SCIs. Conversely, the occurrence of daily life and DFIs, indoor incidents, and T + L fracture locations saw a significant increase.
Age-related morphological and functional alterations in the musculoskeletal system might affect the mechanical loading on vertebral bodies, thereby increasing the likelihood of fractures, especially among older women14,15,24. This trend could be linked to observed differences in age-related patterns and bone mineral density between genders25, with females experiencing more significant bone loss than males26. Male patients were significantly younger and more likely to sustain a traumatic fracture, while female patients more commonly presented with osteoporotic fractures6. Our findings are in line with the secular trends observed in minimal trauma hip, proximal humerus, and distal humerus fractures among elderly patients27,28,29,30,31. Fall was found to be the commonest mechanism of TSI7,9,10,11. In Catalonia, female sex, older age was associated with a higher incidence of major osteoporotic fractures27. Female patients had greater rates of traumatic spinal injury (TSI). Older patients had greater rates of TSI, especially related to falls7. Elderly patients (≥ 65 years of age) made up 42% of all patients in the Netherlands11. Therefore, it's imperative to implement strategies for fall prevention in the elderly to manage the growing burden of these age-related fractures effectively. With the aging of the population, the prevalence of osteoporosis and fracture is anticipated to continue to increase in China. Current policies regarding osteoporotic fracture prevention in many countries have mainly focused on postmenopausal women, but our data highlighted the importance of early recognition of high risk of fracture in both men and women based on risk factors and not just BMD15.
This research indicated seasonal fluctuations in the incidence of spinal fractures among elderly patients. Specifically, a decreased occurrence of LLFs was observed in the autumn cohort. In contrast, the winter cohort saw a marked increase in thoracic fractures, while the spring cohort experienced a rise in lumbar fractures and NSFs. The autumn (26.3%) and winter (26.2%) seasons recorded the highest frequencies of spinal fractures in this demographic. The underlying causes for these seasonal patterns are not fully understood, yet several hypotheses32,33,34,35,36 have been proposed, including the adverse conditions of winter, characterized by longer periods of darkness and colder temperatures34, and the risk of slipping on ice and snow35. Additionally, hypothermia in older individuals, restricted mobility, and the awkwardness associated with wearing multiple layers of clothing during colder months could increase the likelihood of falls36. Consequently, modifying environmental factors to minimize tripping or slipping hazards, coupled with enhanced education on home safety and fall prevention for the elderly, could potentially lower the rate of spinal fractures, aligning with observed seasonal trends.
Differences were notably observed between injuries from high-energy impacts, such as RTCs and HHFs, versus those from low-energy sources, like low-height falls (LHFs) and daily life and DFIs, in terms of age distribution, circumstances of injury, associated injuries, and SCIs. Approximately 20.7% of elderly individuals presenting with TSFs displayed neurological deficits14. In our study, neurological deficits were present in 15.6% of elderly patients with spinal fractures, with a higher prevalence found in RTCs (21.1%) and HHFs (43.2%), as compared to LHFs (15.0%) and DFIs (9.1%). Furthermore, associated injuries were reported in 11.5% of all elderly patients with TSFs14 with this study observing a 15.7% occurrence, and ITIs emerging as the most common associated injury. Significant variance in the distribution of associated injuries between high-energy damage (RTCs and HHFs) and low-energy damage (LHFs and DFIs) highlights the necessity for prompt, precise diagnosis and intervention, especially for injuries resulting from high-energy impacts. Predominant subsequent comorbidities were pneumonia (1.5%) and deep venous thrombosis (1.0%). Hence, implementing aggressive chest-protective measures is advocated to reduce respiratory complications related to spinal fractures in elderly patients, particularly for those affected by RTCs and HHFs.
Strengths and limitations
This investigation was a multicentre retrospective analysis aimed at discerning the differences in gender, age, seasonal occurrence, and causative factors in the characteristics of TSFs within the elderly demographic. Such insights are crucial for the optimal allocation of public health resources, the crafting of preventive strategies, and the enhancement of diagnosis and treatment methodologies. There were some limitations in the study. The study's retrospective nature and cases from military hospitals introduces potential for selection bias. Additionally, the absence of data on bone mineral density, serum calcium, and vitamin D levels was noted as a limitation. Furthermore, the often silent progression of osteoporosis and the resultant fractures are predominantly under diagnosed and undermanaged within China37. Despite these constraints, the gathered epidemiological data offers valuable guidance for the prevention of TSFs among the elderly.
Conclusions
Within the elderly demographic, TSFs exhibited distinct variations based on gender, age, seasonal patterns, and causative factors, influencing the nature of injuries, their circumstances, accompanying injuries, subsequent complications, fracture locations, and the occurrence of SCIs. These disparities highlight the need for tailored approaches in prevention, diagnosis, and management of TSFs among older adults.
Data availability
The data that support the findings of this study are available from the corresponding author upon special request.
References
Hadji, P. et al. Estimated epidemiology of osteoporosis diagnoses and osteoporosis-related high fracture risk in Germany: A German claims data analysis. Arch. Osteoporos. 15(1), 127 (2020).
Iihara, N. et al. Fragility fractures in older people in Japan based on the national health insurance claims database. Biol. Pharm. Bull. 42(5), 778–785 (2019).
Bouyer, B., Leroy, F., Rudant, J., Weill, A. & Coste, J. Burden of fractures in France: Incidence and severity by age, gender, and site in 2016. Int. Orthop. 44(5), 947–955 (2020).
Wu, S. C., Rau, C. S., Kuo, S. C. H., Chien, P. C. & Hsieh, C. H. The influence of ageing on the incidence and site of trauma femoral fractures: A cross-sectional analysis. BMC Musculoskelet. Disord. 20(1), 413 (2019).
Sun, J. et al. Traumatic spinal injury-related hospitalizations in the United States, 2016–2019: A retrospective study. Int. J. Surg. 109(12), 3827–3835 (2023).
Bigdon, S. F. et al. Epidemiologic analysis of 8000 acute vertebral fractures: Evolution of treatment and complications at 10-year follow-up. J. Orthop. Surg. Res. 17(1), 270 (2022).
Algahtany, M. et al. The changing etiology and epidemiology of traumatic spinal injury: A population-based study. World Neurosurg. 149, e116–e127 (2021).
Alawad, M. O. et al. Traumatic spinal injuries in Saudi Arabia: A retrospective single-centre medical record review. BMJ Open. 10(11), e039768 (2020).
Tafida, M. A., Wagatsuma, Y., Ma, E., Mizutani, T. & Abe, T. Descriptive epidemiology of traumatic spinal injury in Japan. J. Orthop. Sci. 23(2), 273–276 (2018).
Niemi-Nikkola, V. et al. Traumatic spinal injuries in Northern Finland. Spine (Phila Pa 1976). 43(1), E45–E51 (2018).
Smits AJ, Ouden LPD, Deunk J, Bloemers FW; LNAZ Research Group. Incidence of Traumatic Spinal Fractures in the Netherlands: Analysis of a Nationwide Database. Spine (Phila Pa 1976). 2020;45(23):1639–1648.
Chen, W. et al. National incidence of traumatic fractures in China: A retrospective survey of 512 187 individuals. Lancet Glob. Health. 5(8), e807–e817 (2017).
Lv, H. et al. Epidemiologic characteristics of traumatic fractures during the outbreak of coronavirus disease 2019 (COVID-19) in China: A retrospective & comparative multi-center study. Injury. 51(8), 1698–1704 (2020).
Wang, H., Xiang, L., Liu, J., Zhou, Y. & Ou, L. Gender differences in the clinical characteristics of traumatic spinal fractures among the elderly. Arch. Gerontol. Geriatr. 59(3), 657–664 (2014).
Wang, L. et al. Prevalence of osteoporosis and fracture in China: The China osteoporosis prevalence study. JAMA Netw. Open. 4(8), e2121106 (2021).
Zhu, Y. et al. Epidemiologic characteristics of traumatic fractures in elderly patients during the outbreak of coronavirus disease 2019 in China. Int. Orthop. 44(8), 1565–1570 (2020).
Barmparas, G. et al. The elderly patient with spinal injury: Treat or transfer?. J. Surg. Res. 202(1), 58–65 (2016).
Uehara, M. et al. Factors affecting the waiting time from injury to surgery in elderly patients with a cervical spine injury: A Japanese multicenter survey. World Neurosurg. 166, e815–e822 (2022).
Carlile CR, Rees AB, Schultz JD, Steinle AM, Nian H, Smith MD, et al. Predicting Mortality in Elderly Spine Trauma Patients. Spine (Phila Pa 1976). 2022;47(14):977–985.
Benchetrit, S. et al. Emergency management of older people with cervical spine injuries: An expert practice review. Emerg. Med. J. 39(4), 331–336 (2022).
Sidon, E. et al. Gender differences in spinal injuries: Causes and location of injury. J. Womens Health (Larchmt). 27(7), 946–951 (2018).
Tian, Y. et al. Age- and gender-specific clinical characteristics of acute adult spine fractures in China. Int. Orthop. 40(2), 347–353 (2016).
Kumar, R. et al. Traumatic spinal injury: Global epidemiology and worldwide volume. World Neurosurg. 113, e345–e363 (2018).
Ning, H. T. et al. Racial and gender differences in the relationship between sarcopenia and bone mineral density among older adults. Osteoporos. Int. 32(5), 841–851 (2021).
Looker, A. C. et al. Age, gender, and race/ethnic differences in total body and subregional bone density. Osteoporos. Int. 20(7), 1141–1149 (2009).
Sigurdsson, G. et al. Increasing sex difference in bone strength in old age: The Age, Gene/Environment Susceptibility-Reykjavik study (AGES-REYKJAVIK). Bone. 39(3), 644–651 (2006).
Surís, X. et al. Epidemiology of major osteoporotic fractures: A population-based analysis in Catalonia, Spain. Arch. Osteoporos. 17(1), 47 (2022).
Llopis-Cardona, F. et al. Incidence of subsequent hip fracture and mortality in elderly patients: A multistate population-based cohort study in Eastern Spain. J. Bone Miner. Res. 37(6), 1200–1208 (2022).
Asada, M. et al. Hip fractures among the elderly in Kyoto, Japan: A 10-year study. Arch. Osteoporos. 16(1), 30 (2021).
Yuan, H., Yu, H., Zhu, Y., Xiang, L. & Wang, H. Effect of age on the patterns of traumatic femoral fractures: Seven years of experience at a regional tertiary hospital. Orthop. Surg. 14(9), 2132–2140 (2022).
Mattila, H., Keskitalo, T., Simons, T., Ibounig, T. & Rämö, L. Epidemiology of 936 humeral shaft fractures in a large Finnish trauma center. J. Shoulder Elbow. Surg. 32(5), e206–e215 (2023).
Souza, M. M., Souza, E. M., Nunes, A. A. & Martinez, E. Z. Seasonal variation of femoral fractures in the state of São Paulo, Southeast Brazil. Rev. Saude Publica. 53, 55 (2019).
Johansen, A., Grose, C. & Havelock, W. Hip fractures in the winter-Using the National Hip Fracture Database to examine seasonal variation in incidence and mortality. Injury. 51(4), 1011–1014 (2020).
Douglas, S., Bunyan, A., Chiu, K. H., Twaddle, B. & Maffulli, N. Seasonal variation of hip fracture at three latitudes. Injury. 31(1), 11–19 (2000).
Al-Azzani W, Adam Maliq Mak D, Hodgson P, Williams R. Epidemic of fractures during a period of snow and ice: has anything changed 33 years on? BMJ Open. 2016;6(9):e010582.
Johnson, N. A., Stirling, E., Alexander, M. & Dias, J. J. The relationship between temperature and hip and wrist fracture incidence. Ann. R Coll. Surg. Engl. 102(5), 348–354 (2020).
Yu, F. & Xia, W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Arch. Osteoporos. 14(1), 32 (2019).
Acknowledgements
This work was supported by the Shenyang Science and Technology Project (22-321-33-35), Applied Basic Research Project of Liaoning Province (2023JH2/101700130) and Natural Science Foundation of Liaoning Province (2022-MS-043).
Author information
Authors and Affiliations
Contributions
All authors designed and participated in the whole process of the study and drafted the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gu, H., Shao, B., Hu, Y. et al. Epidemiological characteristics of traumatic spinal fractures among the elderly in China. Sci Rep 14, 19170 (2024). https://doi.org/10.1038/s41598-024-69780-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69780-y
- Springer Nature Limited
Keywords
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.