Abstract
Malnutrition is linked to adverse outcomes in post-cardiac surgery patients. This study investigates the correlation between the Geriatric Nutritional Risk Index (GNRI) and adverse hospital outcomes in patients following cardiac surgery. This retrospective study included elderly patients with heart disease who were admitted to the Department of Cardiology, Fujian Medical University Union Hospital from January 2020 to December 2022. Patients were divided into two groups based on the cut-off value (98 g/dL). Data from 407 patients were assessed, with 278 (68.3%) classified as having nutritional risk and 129 (31.7%) as having no nutritional risk. Notable distinctions were observed in body weight, BMI, and left ventricular ejection fraction (P < 0.05). Laboratory indicators indicated lower levels of serum albumin, lymphocytes, red blood cells, hemoglobin, admission blood glucose, and admission triglyceride in the nutritional risk group (P < 0.05). Neutrophils and serum creatinine were higher in the nutritional risk group (P < 0.05). Poor prognosis was prevalent in the nutrition risk group (64.7%), with higher incidences of adverse outcomes (P < 0.05). Univariate and multivariate studies showed that GNRI < 98 g/dL was an independent predictor of postoperative cardiac surgery. Nutritional risk was an important predictor of adverse hospital outcomes after the surgery.
Similar content being viewed by others
Introduction
The global prevalence of cardiovascular disease (CVD) continues to grow, with the number of patients increasing from 271 million in 1990 to 523 million in 2019, which is the main reason for premature death and declining quality of life1. In China, CVD morbidity and mortality are escalating, affecting 330 million individuals2, with projections indicating an increase from 190 to 240 million people aged over 65 by 2030, with 70% of individuals over 60 affected by cardiovascular disease. Surgical interventions have become a crucial treatment for cardiovascular diseases, particularly in the aging population3. However, cardiac surgery in the elderly poses increased complications due to factors such as age, surgical trauma, and others. Studies have highlighted higher incidences of acute renal impairment4, multiple organ failure5, and cognitive dysfunction6, in the elderly post-cardiac surgery. Early identification of prognostically relevant risk factors is imperative.
Malnutrition is commonly observed in elderly patients facing critical illness, and it is associated with a less favorable prognosis. Currently, there is a lack of standardized definitions and universally accepted diagnostic criteria for malnutrition, necessitating clinical identification and diagnosis through various screening and assessment tools7. Commonly used tools include NRS 2022, The Nutritional Risk Index, CONUT score, and GNRI. NRS 2022 is advantageous for predicting malnutrition risk but has limitations in patients with conditions such as bedridden, edema, and ascites. NRI assesses nutrition risk based on serum albumin concentration and weight loss percentage, yet its application is constrained by the impact of weight loss percentage. The diagnostic accuracy of the CONUT score is influenced by statin use8. GNRI, established by Bouillanne et al. in 2005, evaluates the nutritional status of the elderly using serum albumin, height, and weight9 Studies, such as that by Ruan GT et al.10, indicate that GNRI scores could serve as independent risk factors for the long-term prognosis of cancer cachexia in the elderly, with limited discussion on related complications. GNRI has proven predictive efficacy for short-term renal outcomes in hemodialysis patients11 and functions as an indicator for predicting the risk of all-cause mortality and cardiovascular death in elderly individuals with diabetes12. In the context of cardiovascular disease, research indicates that lower GNRI levels can reflect bleeding risk and low thrombosis risk in patients undergoing coronary intervention13, although other adverse outcomes have not been extensively explored. Notably, in the cardiac intensive care unit, patients with a high malnutrition risk experience significantly prolonged hospital and cardiac intensive care unit stays14.
However, its association with adverse outcomes after cardiac surgery remains understudied. This study aims to explore whether GNRI scores can predict adverse outcomes in elderly patients post-cardiac surgery.
Methods
Study design, setting, and participants
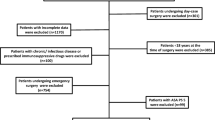
The retrospective study included 407 elderly cardiac patients treated at the Department of Cardiac Surgery, Fujian Medical University Union Hospital, from January 2020 to December 2022. Inclusion criteria were age ≥ 60 years and postoperative admission to the ICU, while exclusion criteria included loss of weight, height, albumin data, and comorbidities such as cancer, sepsis, blood diseases, cachexia, and other wasting diseases. Participants were categorized into groups based on GNRI values, with GNRI < 98 g/dL indicating nutritional risk and GNRI ≥ 98 g/dL indicating no nutritional risk15. This study follows the Declaration of Helsinki and was approved by the Ethics Committee of Fujian Medical University Union Hospital (Number: 2021KY096).
Collect the following data from patients' electronic medical records: (1) essential baseline information (age, gender, height, weight, BMI: calculated as weight divided by height squared); (2) clinical history, encompassing medical conditions (Hypertension:Systolic blood pressure of 140 mmHg or higher, diastolic blood pressure of 90 mmHg or higher, utilization of antihypertensive medications, or self-reported hypertension16; Diabetes mellitus: characterized by fasting blood glucose levels equal to or exceeding 7.0 mmol/L, or glycosylated hemoglobin levels equal to or exceeding 6.5%, Administration of oral anti-diabetic medications or insulin, or previous diabetes diagnosis, cerebrovascular disease, coronary heart disease); (3) history of habits (Smoking: defined according to the World Health Organization in 1997 as persistent and cumulative smoking for 6 months or longer throughout one's lifetime17;Alcohol consumption: average alcohol consumption before admission is ≥ 100 g/week, lasting more than 1 year18; (4) Biochemical indicators (serum albumin, white blood cells [WBC], lymphocytes, neutrophils, red blood cells [RBC], admission blood glucose, admission triglycerides, hemoglobin, serum creatinine [SCr], low-density lipoprotein, high-density lipoprotein); (5) Cardiac function metrics (Left ventricular ejection fraction [LVEF]); (6) Surgical details (operation duration, cardiopulmonary bypass duration [CPB], aortic occlusion duration, type of operation), among others; (7) In this study, prolonged mechanical ventilation (PMV) was defined as patients with mechanical ventilation duration ≥ 48 h; (8) GNRI calculation: [1.489 × albumin (g/L)] + [41.7 × (body weight/ideal body weight)], where the ideal weight is calculated using the Lorentz equation: male height (cm) × 0.75—62.5, female height (cm) × 0.60—40. If the current weight exceeds the ideal weight, the ratio of the current weight to the ideal weight is set to 119.
Outcomes
Primary outcomes encompassed in-hospital death, new postoperative arrhythmia (NOA), pulmonary infection, acute renal insufficiency, and acute liver insufficiency, Secondary outcomes encompassed the duration of stay in both the Intensive Care Unit (ICU) and the hospital. Adverse hospitalization outcomes in this study refer to primary outcomes.
Relevant definitions or diagnostic criteria: (1) Acute renal insufficiency was defined as a 50% increase in SCr for 7 days or a 0.3 mg/dL (26.5 μmol/L) increase in SCr for 2 days or oliguria for ≥ 6 hours20. (2) Acute hepatic insufficiency was defined as postoperative ALT (0–46 IU/L) and/or AST (0–46 IU/L) exceeding normal values. Increased TBIL (2–22 umol/L) and/or DBIL (0–5.9 umol/L)21. (3) Pulmonary infection after cardiac surgery can be diagnosed when the postoperative patient meets both clinical and bacteriological strategies.①.Clinical features: new or progressive imaging infiltration with three clinical features: fever greater than 38℃, leukocytosis or leukopenia, and at least two of the purulent secretions; ②. Pathogenic bacteria were detected twice in sputum culture22.
Statistical analyses
The study utilized SPSS 25.0 statistical software for data entry and analysis. For measurement data that follows a normal distribution, the presentation in the form of mean ± standard deviation (Mean ± SD) was employed as the representation. Inter-group comparisons were conducted using independent sample T-test and analysis of variance. Non-normally distributed measurement data were expressed as median and quartile. Frequency and component ratio were used to describe counting data, and the Chi-square test or rank sum test was utilized for comparing between groups. Univariate logistic regression analysis identified potential risk factors for adverse hospitalization outcomes (P < 0.1), and multivariate logistic regression analysis identified previously significant variables as independent factors (P < 0.05).With results presented as odds ratios (OR) and corresponding 95% confidence intervals (CI). The predictive impact of GNRI on adverse outcomes for patients was evaluated through the construction of a receiver operating characteristic (ROC) curve. The area under the curve (AUC) was calculated using the sensitivity, and specificity to illustrate the predictive value of GNRI. Statistical significance was defined as P < 0.05.
Ethics approval
Ethical Approval was obtained from the Fujian Medical University Union Hospital ethics committee (2021KY096) prior to data collection.
Results
Study population and baseline characteristics
Figure 1 is the flow chart of the study population. A total of 407 subjects were analyzed, and categorized into two groups based on nutritional status: the non-nutritional risk group (n = 129) and the nutritional risk group (n = 278). The nutritional risk group exhibited a body weight of (58.25 ± 10.48)kg, BMI of (22.14 ± 3.35)kg/m2, and left ventricular ejection fraction of (62.19 ± 10.28)%. In contrast, the non-nutritional risk group had a body weight of (63.20 ± 10.25 kg), BMI of (23.93 ± 2.84)kg/m2, and left ventricular ejection fraction of (64.66 ± 8.8)%. Significant differences were observed in body weight, BMI, and left ventricular ejection fraction between the two groups (P < 0.05). Laboratory parameters, including serum albumin, lymphocytes, RBC, hemoglobin, blood glucose, and admission triglyceride were lower in the nutritional risk group compared to the non-nutritional risk group (P < 0.05). Conversely, levels of neutrophils and serum creatinine were higher in the nutritional risk group than in the non-nutritional risk group (P < 0.05). No significant disparities were found in the duration of the operation, cardiopulmonary bypass duration, type of operation, and aortic occlusion duration between the two groups (P > 0.05). However, patients with nutritional risk experienced PMV (P < 0.05). Detailed baseline characteristics are presented in Table 1.
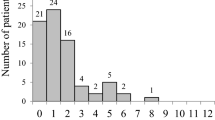
The association between nutritional status and adverse outcomes Table 2 illustrates the outcomes stratified by nutritional status. In the main outcome, the nutrition risk group exhibited 21 in-hospital deaths (7.6%), while the non-nutritional risk group had 8 in-hospital deaths (6.2%), with no statistically significant difference between the two groups (P > 0.05). However, the nutrition risk group showed a higher incidence of new postoperative arrhythmia, pulmonary infection, acute renal insufficiency, and acute liver insufficiency compared to the non-nutritional risk group, and these differences were statistically significant (P < 0.05). Regarding secondary outcomes, the nutrition risk group had a prolonged length of stay in the ICU and more days of hospitalization compared to the non-nutritional risk group, and these differences were statistically significant (P < 0.05).
Univariate results for adverse outcomes are shown in Table 3. Results from the single-factor analysis revealed that several factors were significantly associated with an increased risk of adverse outcomes in elderly patients after cardiac surgery. Specifically, a GNRI < 98 g/dL was strongly correlated with elevated risk (OR = 12.101, 95%CI: 6.868–21.321, P < 0.001). Additionally, lower levels of serum albumin (OR = 0.815, 95%CI: 0.771–0.862, P < 0.001), RBC (OR = 0.508, 95%CI: 0.368–0.702, P < 0.001), and higher serum creatinine (OR = 1.012, 95%CI: 1.004–1.019, P < 0.05) were identified as significant risk factors for adverse outcomes. PMV time was also found to be a substantial risk factor (OR = 3.126, 95%CI: 1.996–4.896, P < 0.001) contributing to the increased likelihood of adverse outcomes in this patient population after cardiac surgery.
In Table 4:The multivariate analysis outcomes of the multivariate analysis demonstrated that gender (OR = 1.917, 95%CI: 1.127–3.263, P < 0.05), serum creatinine (OR = 1.016, 95%CI: 1.004–1.028, P < 0.05), PMV (OR = 2.655, 95%CI: 1.537–4.585, P < 0.001), and GNRI < 98 g/dL (OR = 11.859, 95%CI: 6.419–21.907, P < 0.001) were factors associated with an increased risk of adverse outcomes in elderly patients following cardiac surgery. The risk of adverse outcomes was found to be higher in women than in men (P < 0.05). Serum creatinine levels were higher in patients with nutritional risk compared to those without, and this elevation was significantly linked to overall adverse outcomes (P < 0.05). Patients subjected to PMV exhibited a higher incidence of adverse outcomes (P < 0.001). The study demonstrates that a GNRI < 98 g/dL can autonomously predict adverse clinical outcomes in elderly patients post-cardiac surgery.
Illustrated in Fig. 2, the ROC curve visually depicts the predictive performance of GNRI regarding adverse hospital outcomes. The AUC was calculated as 0.702 (95%CI: 0.651–0.753), demonstrating statistical significance with P < 0.001. This implies that a GNRI < 98 g/dL serves as the critical threshold for prognosticating adverse outcomes, with a sensitivity of 88.3% and specificity of 57.1%. These findings strongly indicate that GNRI can autonomously forecast adverse outcomes in elderly patients post-cardiac surgery.
Discussion
This study marks the inaugural examination of GNRI and its association with negative consequences in elderly individuals after cardiac surgery. The outcomes of the multivariate analysis underscored the predictive roles of gender, PMV, serum creatinine, and GNRI < 98 g/dL in determining adverse outcomes among elderly cardiac surgery patients. In addition, our results showed that the length of ICU stay and hospital stay in patients with nutritional risk group was significantly longer than that in patients without nutritional risk group, and there was a significant difference (P < 0.05).
In this study, 68.3% of patients were identified to have nutritional risk based on the GNRI score, and those with nutritional risk exhibited significantly higher adverse outcomes compared to those without nutritional risk. However, GNRI did not show a significant association with in-hospital mortality in our study (P > 0.05). Notably, Peng JC et al23 found a 28.6% prevalence of severe malnutrition assessed by GNRI in elderly intensive care patients. In their study, patients in the risk group experienced elevated rates of ICU mortality, hospital mortality, and prolonged ICU and hospital stays. Malnutrition, implicated in compromised immune function and heightened inflammation, contributes to unfavorable disease outcomes and increased complication risks. The unique nutritional and metabolic characteristics of elderly heart patients render them susceptible to related complications. Contrary to our findings, Nakamura T et al24 demonstrated a higher incidence of adverse events in male heart failure patients with low GNRI compared to female patients. A study on brittle hip fractures in the elderly identified older age, male gender, lower GNRI score, comorbidities, and lower BI as primary risk factors25. Interestingly, our study diverges from these results, as women emerged as predictors of poor prognosis, linked to poorer short-term postoperative outcomes in various cardiovascular surgical procedures26. At present, the impact of gender differences on clinical outcomes has been extensively studied, but so far, there are still controversies about gender differences in complications and prognosis after cardiac surgery. In one study, female patients experienced atypical or non-angina symptoms longer, leading to delays in the diagnosis, treatment, and recognition of surgical coronary artery disease. The clinical characteristics and prognosis of patients with different genders after cardiac surgery are very different, and the results need to be further explored27. However, the adverse outcome of hospitalization in women in this study may be similar to that in previous studies. The delay in seeing a doctor in women is related to the weakness of the patient, the severity of the disease and the type of surgery, and the prognosis of female patients is worse. The study conducted by Fernandez-Zamora MD et al.28 identified PMV as a predictor of prognosis after cardiac surgery. Mechanical ventilation post-cardiac surgery presents challenges, with airway inflammation and infection potentially triggering systemic inflammatory response syndromes, thereby amplifying adverse outcomes. Supporting our study's conclusions research29 indicated that serum creatinine impacts major renal adverse events in cardiac surgery patients. Even without apparent acute kidney injury, patients undergoing cardiac surgery may experience a decline in function.
GNRI emerges as a promising index, surpassing the predictive efficacy of individual assessments using albumin or BMI alone30. Its popularity in clinical nutrition assessment has surged in recent years, attributed to its convenience and accessibility31. Clinically, GNRI has been linked to the occurrence of various cardiovascular diseases32. Patients undergoing cardiac surgery experience heightened trauma compared to those undergoing other surgical procedures. The increased surgical trauma, coupled with the adoption of cardiopulmonary bypass, renders cardiac surgery patients more susceptible to complications stemming from the systemic inflammatory response syndrome. As malnutrition progresses in these patients, postoperative immunity diminishes, necessitating additional nutritional support33,34. In the study by Zhang Q et al.35, for every one-unit increase in the preoperative GNRI score, the postoperative mortality in gastric cancer patients decreased by 5.6%. Consistent with our findings, research indicates that malnutrition adversely affects physical function and strongly correlates with adverse events, prolonged hospital stays36, and increased mortality37, The comprehensive nature of GNRI as an assessment tool is underscored by its ability to capture multifaceted aspects contributing to postoperative outcomes. In the study of Zhu S et al. BMI cannot reliably reflect body composition and has limitations in patients with water and sodium retention, GNRI is an ideal tool for predicting atrial fibrillation38. NOA was most likely to occur within 5 days after PCI in patients with poor nutritional status39. This also provides a solid theoretical basis for us to study the correlation between GNRI and new arrhythmias after cardiac surgery. Consistent with our study, GNRI has been found to be an independent risk factor for postoperative liver failure and severe postoperative complications40. As CPB is a non-physiological state, there are also factors of poor nutritional status in elderly patients undergoing cardiac surgery, and liver perfusion will be significantly reduced, leading to liver function impairment. Postoperative pneumonia (POP) is the most common of all nosocomial infections in patients undergoing heart surgery. The prevalence of postoperative pulmonary infection was 2%-10%, especially in the first week after surgery, in which age, smoking history, and duration of mechanical ventilation were known risk factors22. Blood contact with the catheter can cause inflammation in various parts of the body. Patients who received CPB for more than 100 min had a 1.7-fold increased risk of postoperative complications and lung infections41. This study strongly proves this point. This study indicated that GNRI was statistically significant for postoperative pulmonary infection.
Few previous investigations have delved into the association between GNRI and unfavorable outcomes in patients with cardiovascular conditions. For instance, in a transcatheter aortic valve implantation study42, the investigation into postoperative nutritional status and one-year all-cause mortality revealed meta-results suggesting a heightened risk of cardiovascular mortality with lower GNRI. The impact on hospital outcomes, however, remained unclear. Li Y et al.14 conducted a study demonstrating GNRI as a dependable indicator for predicting in-hospital mortality in patients within the cardiac intensive care unit (CICU). Furthermore, individuals at a higher risk of malnutrition experienced significantly prolonged hospitalization and CICU stays. Subsequent studies have reaffirmed this association, establishing a link between GNRI, extended hospital stays, and adverse outcomes43. Despite its established association in various settings, the prognostic value of GNRI in cardiac surgery has received limited attention in prior research. Our study contributes by indicating that GNRI can indeed predict the prognostic value of cardiac surgery in the elderly. ROC curve analysis identified an optimal threshold value of 98 g/dL, showcasing potential sensitivity in predicting adverse outcomes. The inverse correlation observed as GNRI increases suggests that clinicians might enhance patient outcomes through more proactive treatment and improved care strategies. These results highlight the GNRI's potential as a valuable instrument for risk assessment in cardiac surgery, urging additional investigation and validation in more diverse populations44,45.
Presently, numerous studies on malnutrition rely on questionnaire-based survey tools46. However, applying these tools to older populations may be constrained by recall bias and communication challenges, potentially leading to inaccurate assessments. GNRI addresses these limitations inherent in survey-based approaches. Clinical routine detection conveniently utilizes serum albumin, height, and weight, with these indicators being easily obtainable. Serum albumin, in particular, serves a crucial physiological role in maintaining colloid osmotic pressure and acting as a carrier for various exogenous and endogenous substances. It serves as an indicator that reflects both overall nutrition and the severity of underlying diseases. Given that the metabolic process of the elderly primarily involves catabolism, necessitating more proteins to compensate for tissue protein consumption47, the decline in serum albumin may indicate a potential inflammatory response in cardiovascular disease. In comparison to other nutritional indicators, GNRI is regarded as a more precise predictor of outcomes related to nutrition in the elderly population48. However, standard weight calculations are not uniformly applicable to all populations and do not accurately reflect the nutritional status of obese or underweight patients. Future research should focus on comparing GNRI with alternative assessment tools to identify patients suitable for cardiac surgery. Additionally, incorporating anthropometric assessments and exploring more detailed or simplified assessment methods will further enhance the utility and reliability of GNRI in clinical practice.
Limitations
This study solely evaluated the initial GNRI in elderly patients undergoing cardiac surgery, neglecting to document and analyze dynamic changes in GNRI over time. This investigation is confined to a retrospective design confined to a single center with restricted sample size, warranting a multicenter study for broader population validation of the current findings.
Conclusion
GNRI emerges as a straightforward and readily measurable tool in clinical practice, playing a crucial role in predicting adverse outcomes among elderly cardiac surgery patients. Furthermore, the study establishes a noteworthy correlation between the length of hospital stay and ICU stay in patients with nutritional risk. GNRI serves as a valuable tool for identifying individuals with an unfavorable prognosis who could benefit from early nutritional intervention. To substantiate the significance of these crucial findings, further exploration through prospective studies is essential.
Data availability
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
References
Vaduganathan, M., Mensah, G. A., Turco, J. V., Fuster, V. & Roth, G. A. The global burden of cardiovascular diseases and risk: A compass for future health. J. Am. Coll. Cardiol. 80, 2361–2371. https://doi.org/10.1016/j.jacc.2022.11.005 (2022).
The, W. Report on cardiovascular health and diseases in China 2022: an updated summary. Biomed. Environ. Sci. 36, 669–701. https://doi.org/10.3967/bes2023.106 (2023).
Morisawa, T. et al. Association between hospital-acquired functional decline and 2-year readmission or mortality after cardiac surgery in older patients: A multicenter, prospective cohort study. Aging Clin. Exp. Res. 35, 649–657. https://doi.org/10.1007/s40520-022-02335-1 (2023).
Xie, T. et al. Construction and validation of a nomogram for predicting survival in elderly patients with cardiac surgery. Front. Public Health 10, 972797. https://doi.org/10.3389/fpubh.2022.972797 (2022).
Au, E. et al. Postoperative outcomes in elderly patients undergoing cardiac surgery with preoperative cognitive impairment: A systematic review and meta-analysis. Anesth. Analg. 136, 1016–1028. https://doi.org/10.1213/ane.0000000000006346 (2023).
Demirjian, S. et al. Predictive accuracy of a perioperative laboratory test-based prediction model for moderate to severe acute kidney injury after cardiac surgery. JAMA 327, 956–964. https://doi.org/10.1001/jama.2022.1751 (2022).
Keller, U. Nutritional laboratory markers in malnutrition. J. Clin. Med. https://doi.org/10.3390/jcm8060775 (2019).
Kinugasa, Y. et al. Diagnostic performance of nutritional indicators in patients with heart failure. ESC Heart Fail 9, 2096–2106. https://doi.org/10.1002/ehf2.13886 (2022).
Bouillanne, O. et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 82, 777–783. https://doi.org/10.1093/ajcn/82.4.777 (2005).
Ruan, G. T. et al. Geriatric nutrition risk index: Prognostic factor related to inflammation in elderly patients with cancer cachexia. J. Cachexia Sarcopenia Muscle 12, 1969–1982. https://doi.org/10.1002/jcsm.12800 (2021).
Maenosono, R. et al. Unplanned hemodialysis initiation and low geriatric nutritional risk index scores are associated with end-stage renal disease outcomes. Sci. Rep. 12, 11101. https://doi.org/10.1038/s41598-022-14123-y (2022).
Shen, X., Yang, L., Gu, X., Liu, Y. Y. & Jiang, L. Geriatric nutrition risk index as a predictor of cardiovascular and all-cause mortality in older Americans with diabetes. Diabetol. Metab. Syndr. 15, 89. https://doi.org/10.1186/s13098-023-01060-7 (2023).
Nakanishi, N. et al. Malnutrition-associated high bleeding risk with low thrombogenicity in patients undergoing percutaneous coronary intervention. Nutr. Metab. Cardiovasc. Dis. 32, 1227–1235. https://doi.org/10.1016/j.numecd.2022.01.016 (2022).
Li, Y., Wang, Z., Sun, T., Zhang, B. & Liang, X. Geriatric nutritional risk index was associated with in-hospital mortality among cardiac intensive care unit patients. Front. Nutr. 10, 1218738. https://doi.org/10.3389/fnut.2023.1218738 (2023).
Lee, M. et al. Association between geriatric nutritional risk index and post-stroke cognitive outcomes. Nutrients https://doi.org/10.3390/nu13061776 (2021).
Ali, S. F. et al. Smoking paradox in patients hospitalized with coronary artery disease or acute ischemic stroke: Findings From Get With The Guidelines. Circ. Cardiovasc. Qual. Outcomes 8, S73-80. https://doi.org/10.1161/circoutcomes.114.001244 (2015).
Dresler, C. M., León, M. E., Straif, K., Baan, R. & Secretan, B. Reversal of risk upon quitting smoking. Lancet 368, 348–349. https://doi.org/10.1016/s0140-6736(06)69086-7 (2006).
Wood, A. M. et al. Risk thresholds for alcohol consumption: combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 391, 1513–1523. https://doi.org/10.1016/s0140-6736(18)30134-x (2018).
Yan, D. et al. Prognostic values of geriatric nutritional risk index (GNRI) and prognostic nutritional index (PNI) in elderly patients with diffuse large B-cell lymphoma. J. Cancer 12, 7010–7017. https://doi.org/10.7150/jca.62340 (2021).
Lameire, N. H. et al. Harmonizing acute and chronic kidney disease definition and classification: report of a kidney disease: Improving global outcomes (KDIGO) consensus conference. Kidney Int. 100, 516–526. https://doi.org/10.1016/j.kint.2021.06.028 (2021).
Zhou, W. et al. Outcomes and risk factors of postoperative hepatic dysfunction in patients undergoing acute type A aortic dissection surgery. J. Thorac. Dis. 11, 3225–3233. https://doi.org/10.21037/jtd.2019.08.72 (2019).
Wang, K. et al. A nomogram predicting pneumonia after cardiac surgery: A retrospective modeling study. J Cardiothorac Surg 19, 309. https://doi.org/10.1186/s13019-024-02797-6 (2024).
Peng, J. C. et al. Association of geriatric nutritional risk index with all-cause hospital mortality among elderly patients in intensive care unit. Front Nutr 10, 1117054. https://doi.org/10.3389/fnut.2023.1117054 (2023).
Nakamura, T., Haraguchi, Y., Matsumoto, M., Ishida, T. & Momomura, S. I. Prognostic impact of malnutrition in elderly patients with acute myocardial infarction. Heart Vessels 37, 385–391. https://doi.org/10.1007/s00380-021-01922-y (2022).
Tsutsui, T. et al. Geriatric nutritional risk index as the prognostic factor in older patients with fragility hip fractures. Osteoporos. Int. 34, 1207–1221. https://doi.org/10.1007/s00198-023-06753-3 (2023).
Cho, L. et al. Cardiac surgery in women in the current era: What are the gaps in care?. Circulation 144, 1172–1185. https://doi.org/10.1161/circulationaha.121.056025 (2021).
Chang, F. C. et al. Sex differences in risks of in-hospital and late outcomes after cardiac surgery: A nationwide population-based cohort study. BMJ Open 12, e058538. https://doi.org/10.1136/bmjopen-2021-058538 (2022).
Fernandez-Zamora, M. D. et al. Prolonged mechanical ventilation as a predictor of mortality after cardiac surgery. Respir. Care 63, 550–557. https://doi.org/10.4187/respcare.04915 (2018).
Priyanka, P. et al. The impact of acute kidney injury by serum creatinine or urine output criteria on major adverse kidney events in cardiac surgery patients. J. Thorac. Cardiovasc. Surg. 162, 143-151.e147. https://doi.org/10.1016/j.jtcvs.2019.11.137 (2021).
Shiroma, K. et al. A nutritional assessment tool, GNRI, predicts sarcopenia and its components in type 2 diabetes mellitus: A Japanese cross-sectional study. Front. Nutr. 10, 1087471. https://doi.org/10.3389/fnut.2023.1087471 (2023).
Kim, H. R. et al. Comparative analysis of three nutrition scores in predicting mortality after acute myocardial infarction. Nutrition 90, 111243. https://doi.org/10.1016/j.nut.2021.111243 (2021).
Bellanti, F., Lo Buglio, A., Quiete, S. & Vendemiale, G. Malnutrition in hospitalized old patients: Screening and diagnosis, clinical outcomes, and management. Nutrients https://doi.org/10.3390/nu14040910 (2022).
Stoppe, C. et al. Role of nutrition support in adult cardiac surgery: A consensus statement from an international multidisciplinary expert group on nutrition in cardiac surgery. Crit Care 21, 131. https://doi.org/10.1186/s13054-017-1690-5 (2017).
Liu, Z. et al. Development and validation of global leadership initiative on malnutrition for prognostic prediction in patients who underwent cardiac surgery. Nutrients https://doi.org/10.3390/nu14122409 (2022).
Zhang, Q. et al. The prognostic value of the gnri in patients with stomach cancer undergoing surgery. J. Pers. Med. https://doi.org/10.3390/jpm13010155 (2023).
Liu, Z., Zang, W., Zhang, P. & Shen, Z. Prognostic implications of global leadership initiative on malnutrition-defined malnutrition in older patients who underwent cardiac surgery in China. Surgery 173, 472–478. https://doi.org/10.1016/j.surg.2022.11.008 (2023).
Efremov, S. M. et al. Effects of malnutrition on long-term survival in adult patients after elective cardiac surgery. Nutrition 83, 111057. https://doi.org/10.1016/j.nut.2020.111057 (2021).
Zhu, S., Zhao, H., Zheng, M. & Peng, J. The impact of malnutrition on atrial fibrillation recurrence post ablation. Nutr. Metab. Cardiovasc. Dis. 31, 834–840. https://doi.org/10.1016/j.numecd.2020.12.003 (2021).
Wu, L. et al. Nutritional status as a risk factor for new-onset atrial fibrillation in acute myocardial infarction. Clin. Interv. Aging 18, 29–40. https://doi.org/10.2147/cia.S387602 (2023).
Li, L. et al. Geriatric nutritional risk index predicts prognosis after hepatectomy in elderly patients with hepatitis B virus-related hepatocellular carcinoma. Sci. Rep. 8, 12561. https://doi.org/10.1038/s41598-018-30906-8 (2018).
Kilic, A. et al. A novel score to estimate the risk of pneumonia after cardiac surgery. J. Thorac. Cardiovasc. Surg. 151, 1415–1420. https://doi.org/10.1016/j.jtcvs.2015.12.049 (2016).
Kazemian, S. et al. Meta-analysis on the association between nutritional status and outcomes after transcatheter aortic valve implantation. Am. J. Cardiol. 186, 109–116. https://doi.org/10.1016/j.amjcard.2022.10.016 (2023).
Liao, D. et al. The prognostic effects of the geriatric nutritional risk index on elderly acute kidney injury patients in intensive care units. Front. Med. Lausanne 10, 1165428. https://doi.org/10.3389/fmed.2023.1165428 (2023).
Dong, C. H., Chen, S. Y., Zeng, H. L., Yang, B. & Pan, J. Geriatric nutritional risk index predicts all-cause mortality in patients with heart failure: A systematic review and meta-analysis. Clinics (Sao Paulo) 76, 2258. https://doi.org/10.6061/clinics/2021/e2258 (2021).
Kanda, D. et al. Impact of nutritional status on prognosis in acute myocardial infarction patients undergoing percutaneous coronary intervention. BMC Cardiovasc. Disord. 22, 3. https://doi.org/10.1186/s12872-021-02448-x (2022).
Dent, E., Wright, O. R. L., Woo, J. & Hoogendijk, E. O. Malnutrition in older adults. Lancet 401, 951–966. https://doi.org/10.1016/s0140-6736(22)02612-5 (2023).
Chen, Z. et al. Predictive value of the geriatric nutrition risk index for postoperative delirium in elderly patients undergoing cardiac surgery. CNS Neurosci. Ther. https://doi.org/10.1111/cns.14343 (2023).
Yenibertiz, D. & Cirik, M. O. The comparison of GNRI and other nutritional indexes on short-term survival in geriatric patients treated for respiratory failure. Aging Clin. Exp. Res. 33, 611–617. https://doi.org/10.1007/s40520-020-01740-8 (2021).
Acknowledgements
We appreciate the financial support of the Fujian Provincial Finance Department for this study.
Funding
Sponsored by Fujian Provincial Health Technology Project (2021CXA017) and Fujian Cardiovascular Disease Medical Center (2021–76).
Author information
Authors and Affiliations
Contributions
Ani Zhao designed the research, Lijun Wu and Xiaoqin Liao conducted the research, Lingyu Lin and Sailan Li analyzed the data, Ani Zhao and Lijun Wu wrote the paper, and Yanjuan Lin and Liangwan Chen had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, A., Wu, L., Lin, L. et al. The geriatric nutritional risk index is related to adverse hospitalization outcomes in individuals undergoing cardiac surgery. Sci Rep 14, 19126 (2024). https://doi.org/10.1038/s41598-024-69668-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69668-x
- Springer Nature Limited