Abstract
Male partner involvement strongly influences a woman's decision to undergo cervical cancer screening. Women of low socioeconomic status are disproportionately affected by cervical cancer. Women living in low-and middle-income countries often encounter resistance from their partners regarding participation in cervical cancer screening. The lack of men's support for sexual and reproductive health programs, including cervical cancer screening, creates a barrier to women's utilization of health services. To assess Ethiopian men's awareness, knowledge, perceptions, and attitudes toward cervical cancer screening and their support to their female partners during screening. A community-based cross-sectional survey was conducted from June 20, 2023, to August 04, 2023. A multistage sampling procedure was used to recruit 614 male survey participants. Descriptive statistics were used to summarize sociodemographic data. Univariate and multivariate regression analyses were performed to measure the associations between the dependent and independent variables. A p-value of less than 0.05 was considered statistically significant. In this survey, 58.5% (359) of participants supported their partners for cervical cancer screening. More than half 55.9% (343) of the participants had an awareness of cervical cancer disease and 47.2% (290) participants knew the risk factors associated with the development of cervical cancer. In addition to that, 66.8% (410) of men have a positive attitude towards screening and encourage their wives to get screened if they notice symptoms of cervical cancer. Regarding the perceptions of cervical cancer, 37.0% (227) of male participants believed that their female partners were at risk of developing the disease, while 38.3% (235) of men believed that cervical cancer screening was only necessary if the woman showed symptoms. Completion of higher education (AOR = 3.75, 95% CI 1.60–8.79, p = 0.002), living with other people (AOR = 0.09, 95% CI 0.03–0.29, p < 0.0001), not being tested for HIV (AOR = 0.26, 95% CI 0.10–0.74, p = 0.011), and having information about cervical cancer (AOR = 3.33, 95% CI 1.36–8.15, p = 0.009) were statistically significantly associated with men’s support for their partners in cervical cancer screening. Men’s awareness, knowledge, and perceptions of cervical cancer screening were low. On the other hand, men have a positive attitude towards screening and encourage their wives to get screened if they notice symptoms of cervical cancer. This survey will serve as a basis for the development of further strategies and action plans to promote and support male participation in cervical cancer screening in Ethiopia. This can be achieved through the development of strategic plans, including public campaigns, raising awareness among social and community leaders, involving non-governmental organizations focusing on women's health, and community education.
Similar content being viewed by others
Introduction
Human papillomavirus infections (HPV) are associated with the majority of cervical cancer cases, with strains HPV-16 and 18 identified as the most carcinogenic subtypes1,2,3. Most women become infected with HPV shortly after engaging in sexual activity, which means that it is most commonly transmitted into the vaginal canal4,5. Cervical cancer mortality rates remain alarmingly high worldwide, particularly in low- and middle-income countries (LMICs)6,7. It is the fourth leading cause of death among women globally8,9. In 2020, approximately 604,000 new cases and 342,000 deaths were reported, with 90% of cases and deaths occurring in LMICs7. In Ethiopia, cervical cancer accounts for 13.6% of all cancer cases and is the second most prevalent cancer after breast cancer, which accounts for 32.9% of cases. About 6294 new cases of cervical cancer are registered every year with a mortality rate of over 488410. Women in LMICs often face resistance from partners and families to undergo cervical cancer screening, and identifying the social, cultural, and psychological factors underlying male partners' resistance to screening is an important step in reducing barriers to men supporting their wives participating in cervical cancer screening11,12.
Women of low socioeconomic status are disproportionately affected by cervical cancer. The disease can have devastating consequences for patients' living conditions13. In LMICs, cervical cancer is a major problem due to limited awareness among the population, healthcare providers, and policy-makers14. In addition, there is limited access to health services and inadequate screening programs for precursor lesions and early-stage cancer12. Many women who have never undergone screening are only diagnosed with cancer at a later stage, which makes treatment more difficult. This leads to high incidence and mortality rates for cervical cancer15,16. The World Health Organization (WHO) has emphasized the importance of involving men in the prevention of cervical cancer in LMICs17.
Cervical cancer can primarily be prevented by prophylactic HPV vaccination and screening for precancerous lesions. Although screening is currently practiced in some cases, it is still a public health issue due to scarce resources and the fact that it is not performed by all women of childbearing age7,18. The uptake of cervical cancer screening in Ethiopia is not well established. It was only introduced in 2016 and only one in seven women has been screened for cervical cancer19. A meta-analysis conducted in Ethiopia found that the national uptake of cervical cancer screening was 14.79%. The highest utilization of cervical cancer screening is in the Southern Nations, Nationalities, and Peoples region (18.59%) and the lowest in the Amhara region (13.62%), which was the focus of the current survey19. Cervical cancer screening is performed to detect any signs of disease in the cervix before symptoms arise and to identify any precancerous lesions in the early stages15. Regular screening is widely recognized as the most crucial public health strategy to reduce the incidence of cervical cancer and associated deaths18. Research has demonstrated that educational initiatives and community-driven prevention campaigns can effectively enhance awareness and access to screening and treatment services20,21.
Male involvement is increasingly recognized as crucial for the successful implementation of maternal and child health programs worldwide22,23. This assertion is based on the role of men in decision-making within families and relationships and their influence on women's healthcare decisions24,25. The involvement of male partners can greatly affect a woman's decision to undergo screening26,27. This influence can extend to various aspects, such as logistics, education, and psychosocial factors. Partners generously provided financial support to cover transportation costs and also offered valuable emotional support and words of encouragement for cervical cancer screening24. On the other hand, a lack of male partner support in LMICs may hinder women from attending cervical cancer screening28.
Research shows that many men are uninformed about the risks and causes of cervical cancer, and some men even believe that they cannot contribute to the development of this disease in women29,30,31. The lack of men's support for sexual and reproductive health programs, including cervical cancer screening, creates a barrier to women's utilization of health services32. Due to this male partner support for cervical cancer screening and treatment may be critical to reducing cervical cancer deaths. A study conducted in Zimbabwe33, Uganda34, Ghana35, and Kenya24 found that men lacked knowledge about cervical cancer, including its risk factors and prevention. Furthermore, men did not provide women with emotional and financial support when they sought screening and treatments for cervical cancer. However, the literature did not examine the specific support men provided their partners during the screening and treatment of the disease29,36,37. In Ethiopia, a comprehensive study was conducted to gain insight into the obstacles hindering cervical cancer screening, with a specific focus only on the experiences and perspectives of women19. There is no data on men’s knowledge, awareness, and support for attending cervical cancer screening. To address this gap, this is the first exploratory study focused on exploring men’s knowledge and awareness of cervical cancer screening and investigating men’s perceptions and attitudes towards wives’/partners’ support in seeking cervical cancer screening.
Methods and materials
Study setting
The survey was conducted in Debre Berhan City, northeastern Ethiopia. The city is situated 130 km northeast of Addis Ababa and is divided into 10 kebeles (smallest administration units in Ethiopia). The entire area of the city is about 142.71 square km, with an average elevation of 2840 m above sea level. According to the Debre Berhan City Administration, the total population in 2022/23 was 188,513 out of which 54.78% (103,267) are women. There are three hospitals (two governmental and one private), three health centers, nine health posts, 10 private clinics, and 25 community pharmacies in the city that provide health services to the general population. The survey participants were selected from the households of selected kebeles of Debre Berhan city.
Study design and period
A community-based cross-sectional survey was conducted to assess male support for cervical cancer screening during the study period, which lasted from June 20, 2023, to August 04, 2023.
Eligibility criteria
Inclusion criteria: (i) men who had a partner or were married, (ii) age ≥ 18 years, (iii) ability to give informed consent, and willingness to participate in the survey were included. Men who did not live permanently in the study area and men with cognitive impairments who were unable to complete the interview while participating in the survey were excluded from the survey.
Sample size determination
For this survey, the sample size was calculated using a single proportional formula38. Since there were no prior studies conducted in Ethiopia, the prevalence rate (P) was determined to be 50%. Our significance level, α, was set at 0.05, with a confidence interval of 95% and a margin of error (d) of 5%. To calculate the sample size, the following formula was used:
A total of 614 men were selected as survey participants in Debre Berhan city, accounting for a design effect of 1.5 and an anticipated nonresponse rate of 10%.
Sampling procedures
A multistage sampling method was used to select the survey participants from the entire kebeles of Debre Berhan city. There are ten kebeles in the study area. From the 10 kebeles, 5 kebeles were selected using a simple random sampling method (lottery method), and then proportional allocation was performed to select the final survey participants from each selected kebele. The lists of households were obtained from the registration books of the selected Kebeles. The Kebeles administrative office of each selected Kebeles was used as the starting point for selecting the first household. Men who met the eligibility criteria were then invited to participate in the study. The first household was then selected, and the participants were interviewed using the consecutive sampling method until the sample size for each selected kebeles was reached. A suitable time and place, usually the participant's home, were arranged for the interviews. For selected households with more than one eligible interviewee, one was chosen using the lottery method (Fig. 1).
Data collection and management
After a review of the literature on male support for cervical cancer screening34,35,39; semi-structured questionnaires in the Amharic language were prepared for data collection. Data were then collected through interviews with trained clinical pharmacists. The questionnaire was divided into four sections. Section I focused on gathering the sociodemographic characteristics (age, sex, educational status, place of residence, marital status, Professions, social drug use, and HIV status) of the survey participants. Section II included questions related to awareness and knowledge of males for cervical cancer. Section III focused on the male's perception of cervical cancer screening, and section IV also focused on the male’s attitude toward the cervical screening of their partners/wives.
Data quality assurance
Before conducting the main survey, a pretest was conducted on 5% (31 male) of the sample size outside the survey area to ensure data quality. Based on the results of the pretest, the clarity and consistency of the data collection instrument were checked. The survey director spent half a day training the data collectors, recruited from four clinical pharmacists, on the aims of the survey and how to use the instrument to collect data from participants. To ensure the consistency and completeness of the data, the survey director reviewed all data collected daily to ensure data quality.
Data analysis
The data were then entered into the Statistical Package for the Social Sciences (SPSS, IBM Corporation, Armonk, NY, USA) version 26 for the final analysis. Descriptive statistics, including frequencies, percentages, means, and standard deviations, were utilized to analyze the sociodemographic variables. After checking the assumptions, multiple logistic regression analysis was performed to identify possible factors associated with male support for cervical cancer screening. The univariate analysis was performed to obtain candidate variables for the multivariate regression models. In the univariate analysis, factors associated with male support for cervical cancer screening with a p-value of < 0.2 were considered candidates for a multivariate binary logistic regression model to identify strong factors associated with male support for cervical cancer screening. A p-value of < 0.05 was used to determine statistical significance.
Ethical consideration and consent statement
Ethical approval for the study and study protocol was obtained from Addis Ababa University, College of Health Science, School of Allied Health Science Ethical Review Board. The data collector goes to each Kebeles household and clearly explains the aims of the survey to the survey participants. After that written informed consent was obtained from each survey participant and for those who cannot read and write the data collectors read the consent form to the survey participants. The right was given to the survey participants to refuse or discontinue participation at any time they wanted and the chance to ask anything about the survey. For obscurity, the participant’s name was not used at the time of data collection, all other personnel information was kept entirely obscure, and confidentiality was assured throughout the survey period. Moreover, all methods in the present study were performed in accordance with the Declaration of Helsinki.
Results
Sociodemographic characteristics
A total of 614 individuals participated in this survey. The mean age of the participants was 42.96 ± 11.71 years and ranged from 26 to 80 years. More than half of the participants, 51.3% (315) had a diploma or higher education. Out of all the participants who took part in the survey, 15.8% (97) were identified as healthcare professionals. Of those surveyed, 56.7% (348) were employed by the government. Regarding human immunodeficiency virus (HIV) status, 48.5% (298) of survey participants were tested for HIV, and of those tested, only 8.1% (50) of survey participants were HIV positive (Table 1).
Awareness of cervical cancer among men
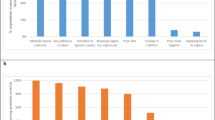
In this survey, more than half of 55.9% (343) of the male participants were aware of cervical cancer (Table 2). Of those who knew about cervical cancer, 49.8% (171) of participants cited health facilities as their main source of information, followed by 29.5% (101) community health education and 25.9% (89) social media such as the internet and Facebook (Fig. 2). However, 44.1% (271) of male survey participants did not know about cervical cancer. The main reasons cited by these participants were that 67.7% (181) had not received health education in the community, 32.8% (89) had limited access to social media, and 9.8% (60) did not have a health facility nearby.
Men's knowledge about cervical cancer
Of the male participants surveyed, 47.2% (290) of participants reported knowledge of risk factors associated with the development of cervical cancer, and 30.9% (190) of study participants considered multiple sexual partners to be the greatest risk factor (Fig. 3). On the other hand, 40.2% (247) knew the symptoms of cervical cancer, and 23.0% (141) considered excessive vaginal discharge to be the most common symptom. Regarding cervical cancer preventive measures, 48.2% (296) of the study participants were aware of cervical cancer preventive measures, and 32.7% (201) of them considered screening to be the most important preventive measure, followed by 21.0% (129) of HPV vaccination (Table 3).
Men's perceptions of cervical cancer screening
In a survey on perceptions of cervical cancer, 37.0% (227) of male participants believed that their female partners were at risk of developing the disease, while 38.3% (235) of men believed that cervical cancer screening was only necessary if the woman showed symptoms. On a positive note, 74.8% (459) of participants believed that cervical cancer was preventable and 54.7% (336) of males realized that HPV infection increased the risk of cervical cancer. On the other hand, 37.8% (232) mistakenly believed that only HIV-positive women were at risk for cervical cancer (Table 4).
Men's attitudes toward cervical cancer screening
Table 5 shows that 66.8% (410) of men would encourage their partner to undergo cervical cancer screening only if she experienced symptoms. However, if their partner was diagnosed with cervical cancer 57.2% (351) of the men believed that it could be treated (Table 5).
Factors associated with men's support for cervical cancer screening
Univariate analysis revealed that ten variables (age, marital status, religion, education level, occupations, professions, who you live with, social drug use, tested for HIV, Having information for cervical cancer) were associated with encouraging men to help their partners screen for cervical cancer. To further investigate the association between these variables, a multivariate binary regression analysis was conducted with ten outcome variables. Finally, through cross-validation using the hierarchical regression method, four variables (educational status, who you live with, tested for HIV, and having information for cervical cancer) were identified as significant associations with encouraging men to support their partners' screening for cervical cancer.
Male survey participants were 3.75 times more likely (AOR = 3.75, 95% CI 1.60–8.79, p = 0.002) to support their partners in screening for cervical cancer among participants with educational status of diploma and above compared to male participants who were not able to read and write. In addition, men were 3.33 times more likely (AOR = 3.33, 95% CI 1.36–8.15, p = 0.009) to support their partners in screening for cervical cancer among participants who had information about cervical cancer than men who had no information about cervical cancer. On the other hand, men's encouragement to help their partners screen for cervical cancer was 90% lower among men who live with others (AOR = 0.09, 95% CI 0.03–0.29, p = 0.000) than among those who lived with family, and men who were not tested for HIV were 74% less likely (AOR = 0.26, 95% CI 0.10–0.74, p = 0.011) to encourage their female partners to screen for cervical cancer than men who were tested for HIV in their lifetime (Table 6).
Discussion
To our knowledge, this is the first survey designed to investigate Ethiopian men's awareness, knowledge, perceptions, and attitudes about cervical cancer screening and the support they provide to their partners during screening. In LMICs, women often encounter resistance from their partners and families when it comes to getting screened for cervical cancer. Understanding the social, cultural, and psychological factors that contribute to men's reluctance to support their wives in participating in cervical cancer screening is crucial for reducing barriers to screening11,12. Importantly, the WHO has emphasized the need for increased male involvement in cervical cancer screening worldwide40.
Male Support for Cervical Cancer Screening at Debre Berhan City was 58.5% (359), which is consistent with studies in Uganda (59.0%)41 and the results of a male focus group study in Ghana29; however, it is lower than studies conducted in Malawi 90%42, Kenya 89.1%43 and India 66% (11). This could be because, in Ethiopia, a lack of adequate health information by healthcare providers and low awareness of the disease were the main factors for the low uptake of cervical cancer screening44,45. Furthermore, a qualitative study carried out in Ghana revealed that male partners had no prior knowledge of the causes, symptoms, and risk factors for the disease until their partners were diagnosed with cervical cancer35.
In this survey, the awareness of cervical cancer screening among men in Debre Berhan city was 55.9% (343), and the main sources of information for cervical cancer disease 49.8% (171) were health facilities, followed by 29.5% (101) were community health education facilities. On the other hand, 44.1% (271) of male participants in this survey were not aware of cervical cancer because 67.7% (181) of survey participants did not receive community health education; due to this increased community education and increased number of health facilities is important to improve the awareness of cervical cancer screening.
According to this survey, the main risk factors for developing cervical cancer cited by males were having multiple sexual partners (30.9%) and early sexual intercourse (17.1%). Research shows that persistent HPV infection is the primary cause of cervical cancer2, but in this survey, only 16.4% of participants thought that HPV infection can cause cervical cancer. Other risk factors include early onset of sexual activity, high-risk sexual partners, history of vulvar or vaginal neoplasia, and immunosuppression46,47,48. In addition, only 40.2% of men knew the symptoms of cervical cancer, and only 48.2% knew about prevention strategies for this disease. In this study, 38.3% of men also believed that screening for cervical cancer was only necessary if the woman showed symptoms. As a result, awareness of HPV as a major risk factor for the development of cervical cancer is low in this study area. To increase awareness of HPV as a risk factor for cervical cancer and increase uptake of HPV screening, increased public education about HPV vaccination and screening programs is needed.
Cervical cancer is highly preventable and can be easily treated if detected at an early stage. The main strategies to prevent cervical cancer are vaccination against HPV and regular screening49. In this survey, only 32.7% and 21.0% of men reported that the most important strategies to prevent cervical cancer are screening and vaccination against HPV, respectively. However, the incidence and mortality of cervical cancer are disproportionately high in LMICs where there are no organized screening and prevention programs, and only 5% of women in LMICs are adequately screened for cervical cancer50. Another study, also conducted in mid-western Uganda, found that limited knowledge among men about the risk factors and causes of cervical cancer, as well as the preventive aspect of HPV vaccination and HPV screening and their respective target populations, limits the uptake of both services34. In addition, cytology programs are not feasible due to the lack of healthcare infrastructure and cost. Therefore, alternative methods of cancer screening, such as visual inspection with acetic acid and the HPV-DNA test, have been intensively studied49,50,51.
Men with higher levels of education (diploma and above) were 3.75 times more likely to support their partners in screening for cervical cancer than male participants who were not literate. In studies conducted in Kenya43, Nigeria52, and Ghana53, men with higher levels of education had significantly greater knowledge about cervical cancer. In addition, men who were knowledgeable about cervical cancer were 3.33 times more likely to support their partners in screening. A study conducted in India11 also shows that men who know about cervical cancer and are aware of screening have a good intention to support their partners in screening for cervical cancer. On the other hand, men's encouragement of their partners to screen for cervical cancer was 90% lower among men who were living with others than men who lived with the family, and men who were not tested for HIV were 74% less likely to encourage their partners to screen for cervical cancer than men who were tested for HIV in their lifetime. This may be due to the integration of HIV treatment with cervical cancer screening services in most setups, which could increase awareness of cervical cancer screening54.
Despite the development of evidence-based prevention strategies for cervical cancer in resource-limited settings, implementation and uptake of services still need to be improved41,55,56,57. To improve the adoption and acceptance of preventive measures, screening, and vaccination programs should actively engage men in creating awareness and the WHO has called for greater involvement of men in cervical cancer screening globally40. Cervical cancer is a significant public health issue in Ethiopia. It is essential to enhance men's understanding of cervical cancer symptoms, risk factors, and prevention strategies within the Ethiopian context. This can be achieved through the development of strategic plans, including public campaigns, raising awareness among social and community leaders, involving non-governmental organizations focusing on women's health, and community education.
Finally, this survey had certain limitations. It was conducted in an urban area of the Amhara region in Ethiopia where most people can read and write and have access to relative health facilities and community education. Therefore, the results cannot be directly applied to rural communities in Ethiopia or LMICs in general. Participation in the study was voluntary and the questionnaires were not self-administered. This may have led to dishonesty among respondents, as cervical cancer can be considered a sensitive topic. The authors used a community-based cross-sectional survey design that did not establish a causal relationship between determinants and men's knowledge, awareness, and perceptions of cervical cancer screening. In addition to that, community-based cross-sectional surveys are not suitable for analyzing men's cervical cancer screening behavior over time. Furthermore, the survey was focused on men living in urban areas and used a cross-sectional study design. The authors suggest further research should take into account various aspects of the Ethiopian population, including geographical location (urban and rural areas), educational status (low and high), age groups (young and elderly), and social status (community and religious leaders, as well as the general population).
Conclusion
Men’s awareness, knowledge, and perceptions of cervical cancer screening were low. The main sources of information about cervical cancer were health facilities and community health education. Increased community education and health facilities are important to improve cervical cancer screening awareness. Limited knowledge among men about the risk factors and causes of cervical cancer, as well as about the preventive aspect of HPV vaccination and cervical cancer screening and their respective target populations, limits the uptake of both services. On the other hand, men have a positive attitude towards screening and encourage their wives to get screened if they notice symptoms of cervical cancer. Statistically significant factors associated with male support for cervical cancer screening included higher educational attainment, living with others, not being tested for HIV, and cervical cancer awareness. To increase participation in screening programs for cervical cancer, many interventions focus on educating and motivating women to take part. However, simply targeting women may not be enough to overcome social obstacles to screening. It is important to recognize the role of male partners and families, particularly in cultures where men or heads of households are primarily responsible for making health-related decisions. By involving and engaging these individuals, we can work towards breaking down barriers to screening and improving overall participation rates. This survey will serve as a basis for the development of further strategies and action plans to promote and support male participation in cervical cancer screening in Ethiopia. In addition, Ethiopian health policymakers (Ministry of Health) should develop new strategic plans to improve men's awareness and knowledge about the symptoms of cervical cancer, the risk factors that favor the development of cervical cancer, and the key prevention strategies for cervical cancer in the Ethiopian context.
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HIV:
-
Human immunodeficiency virus
- HPV:
-
Human papillomavirus
- LMICs:
-
Low- and middle-income countries
- WHO:
-
World Health Organization
References
De Martel, C., Plummer, M., Vignat, J. & Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 141(4), 664–670 (2017).
Olusola, P., Banerjee, H. N., Philley, J. V. & Dasgupta, S. Human papilloma virus-associated cervical cancer and health disparities. Cells 8(6), 622 (2019).
Koh, W.-J. et al. Cervical cancer, version 3.2019, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Netw. 17(1), 64–84 (2019).
Okunade, K. S. Human papillomavirus and cervical cancer. J. Obstet. Gynaecol. 40(5), 602–608 (2020).
Castellsagué, X. et al. Risk of first cervical HPV infection and pre-cancerous lesions after onset of sexual activity: Analysis of women in the control arm of the randomized, controlled PATRICIA trial. BMC Infect. Dis. 14, 1–12 (2014).
Bedell, S. L., Goldstein, L. S., Goldstein, A. R. & Goldstein, A. T. Cervical cancer screening: Past, present, and future. Sex. Med. Rev. 8(1), 28–37 (2020).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Huang, J. et al. Worldwide Burden of, Risk Factors for, and Trends in Pancreatic Cancer. Gastroenterology https://doi.org/10.1053/j.gastro.2020.10.007 (2020).
Arbyn, M. et al. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 8(2), e191–e203 (2020).
Endale H, Mulugeta T, Habte T. The Socioeconomic Impact of Cervical Cancer on Patients in Ethiopia: Evidence from Tikur Anbessa Specialized Hospital. Cancer Manag. Res. 1615–25 (2022).
Dsouza, J. P., Van den Broucke, S., Pattanshetty, S. & Dhoore, W. Factors explaining men’s intentions to support their partner’s participation in cervical cancer screening. BMC Womens Health 22(1), 443 (2022).
Faradisa, E., Ardiana, H., Priyantini, D., Fauziah, A. & Susanti, I. A systematic review of the factors associated with cervical cancer screening uptake among women in low and middle-income Countries. J. Ners. 15(2), 113–119 (2020).
Organization WH. Accelerating cervical cancer elimination-Report by the Director-General. (2018).
Adedimeji, A. A. et al. Challenges and opportunities associated with cervical cancer screening programs in a low income, high HIV prevalence context. BMC Women’s Health 21, 1–4 (2020).
Organization WH, Health WHOR, Diseases WHOC, Promotion H. Comprehensive cervical cancer control: a guide to essential practice: World Health Organization, (2006).
Johnson, C. A., James, D., Marzan, A. B. & Armaos, M. Cervical cancer: An overview of pathophysiology and management. Semin. Oncol. Nurs. 35(2), 166–174 (2019).
Health WHOR, Organization WH, Diseases WHOC, Promotion H. Comprehensive cervical cancer control: a guide to essential practice: World Health Organization, (2006).
Peirson, L., Fitzpatrick-Lewis, D., Ciliska, D. & Warren, R. Screening for cervical cancer: A systematic review and meta-analysis. Syst. Rev. 2, 1–14 (2013).
Desta, M. et al. Cervical cancer screening utilization and predictors among eligible women in Ethiopia: A systematic review and meta-analysis. PloS One 16(11), e0259339 (2021).
Rosser, J. I., Njoroge, B. & Huchko, M. J. Changing knowledge, attitudes, and behaviors regarding cervical cancer screening: The effects of an educational intervention in rural Kenya. Patient Educ. Couns. 98(7), 884–889 (2015).
Huchko, M. J. et al. Cervical cancer screening through human papillomavirus testing in community health campaigns versus health facilities in rural western Kenya. Int. J. Gynecol. Obstet. 141(1), 63–69 (2018).
Östlin, P., Eckermann, E., Mishra, U. S., Nkowane, M. & Wallstam, E. Gender and health promotion: A multisectoral policy approach. Health Promot. Int. 21(suppl 1), 25–35 (2006).
Blanc, A. K. The effect of power in sexual relationships on sexual and reproductive health: An examination of the evidence. Stud. Fam. Plan. 32(3), 189–213 (2001).
Adewumi, K., Oketch, S. Y., Choi, Y. & Huchko, M. J. Female perspectives on male involvement in a human-papillomavirus-based cervical cancer-screening program in western Kenya. BMC Women’s Health 19(1), 1–9 (2019).
Adamu, H., Oche, O. M. & Kaoje, A. U. Effect of health education on the knowledge, attitude and involvement by male partners in birth preparedness and complication readiness in rural communities of Sokoto state, Nigeria. Am. J. Public Health 8(5), 163–175 (2020).
Al-Naggar, R. A., Low, W. & Isa, Z. M. Knowledge and barriers towards cervical cancer screening among young women in Malaysia. Asian Pac. J. Cancer Prev. 11(4), 867–873 (2010).
Baskaran, P. et al. Perceived susceptibility, and cervical cancer screening benefits and barriers in Malaysian women visiting outpatient clinics. Asian Pac. J. Cancer Prev. 14(12), 7693–7699 (2013).
Chapola, J. et al. Barriers to follow-up after an abnormal cervical cancer screening result and the role of male partners: A qualitative study. BMJ Open 11(9), e049901 (2021).
Williams, M. & Amoateng, P. Knowledge and beliefs about cervical cancer screening among men in Kumasi, Ghana. Ghana Med. J. 46(3), 147 (2012).
Tsegay, A., Araya, T., Amare, K., G/tsadik, F. Knowledge, attitude, and practice on cervical cancer screening and associated factors among women aged 15–49 years in Adigrat Town, Northern Ethiopia, 2019: A Community-Based Cross-Sectional Study. Int. J. Women's Health 1283-98 (2021).
Maree, J., Wright, S. & Makua, T. Men’s lack of knowledge adds to the cervical cancer burden in South Africa. Eur. J. Cancer Care. 20(5), 662–668 (2011).
Kura, S., Vince, J. & Crouch-Chivers, P. Male involvement in sexual and reproductive health in the Mendi district, Southern Highlands province of Papua New Guinea: A descriptive study. Reprod. Health 10(1), 1–10 (2013).
Mantula, F. & Toefy, Y. Women and health providers’ perspectives on male support for cervical cancer screening in Gwanda district, Zimbabwe. Plos One 18(10), e0282931 (2023).
de Fouw, M. et al. Involving men in cervical cancer prevention; a qualitative enquiry into male perspectives on screening and HPV vaccination in Mid-Western Uganda. Plos One 18(1), e0280052 (2023).
Binka, C., Doku, D. T., Nyarko, S. H. & Awusabo-Asare, K. Male support for cervical cancer screening and treatment in rural Ghana. PLoS One 14(11), e0224692 (2019).
Thiel de Bocanegra, H., Trinh-Shevrin, C., Herrera, A. P. & Gany, F. Mexican immigrant male knowledge and support toward breast and cervical cancer screening. J. Immigr. Minor. Health 11, 326–333 (2009).
Treviño, M., Jandorf, L., Bursac, Z. & Erwin, D. Cancer screening behaviors among latina women: The role of the latino male. J. Community Health 37, 694–700 (2012).
Wang, J. et al. The estimation of sample size in multi-stage sampling and its application in medical survey. Appl. Math. Comput. 178, 239–249 (2006).
Adewumi, K., Oketch, S. Y., Choi, Y. & Huchko, M. J. Female perspectives on male involvement in a human-papillomavirus-based cervical cancer-screening program in western Kenya. BMC Women’s Health 19, 1–9 (2019).
Pustaka, D., Moscicki, A. B., Smith, R. A., Eyre, H. J., editors. 1. World Health Organization. Comprehensive Cervical Cancer Control. A Guide to Essential Practice. Geneva: WHO; (2006).
Moses, E. et al. Understanding Men’s perceptions of human papillomavirus and cervical Cancer screening in Kampala, Uganda. J. Glob. Oncol. 4, 1–9 (2018).
Lewis, S. et al. “A loving man has a very huge responsibility”: A mixed methods study of Malawian men’s knowledge and beliefs about cervical cancer. BMC Public Health 20(1), 1–12 (2020).
Rosser, J. I., Zakaras, J. M., Hamisi, S. & Huchko, M. J. Men’s knowledge and attitudes about cervical cancer screening in Kenya. BMC Women’s Health 14, 1–7 (2014).
Gebru, Z., Gerbaba, M. & Dirar, A. Barriers to cervical cancer screening in Arab Minch town, southern Ethiopia: A qualitative study. J. Community Med. Health 6(401), 2161–07111000401 (2016).
Bayu, H., Berhe, Y., Mulat, A. & Alemu, A. Cervical cancer screening service uptake and associated factors among age eligible women in Mekelle Zone, Northern Ethiopia, 2015: A community based study using health belief model. PloS One 11(3), e0149908 (2016).
International Collaboration of Epidemiological Studies of Cervical Cancer. Comparison of risk factors for invasive squamous cell carcinoma and adenocarcinoma of the cervix: collaborative reanalysis of individual data on 8097 women with squamous cell carcinoma and 1374 women with adenocarcinoma from 12 epidemiological studies. Int. J. Cancer 120(4), 885–891 (2007).
Akinyemiju, T., Ogunsina, K., Sakhuja, S., Ogbhodo, V. & Braithwaite, D. Life-course socioeconomic status and breast and cervical cancer screening: Analysis of the WHO’s Study on Global Ageing and Adult Health (SAGE). BMJ Open 6(11), e012753 (2016).
Gravitt, P. E. & Winer, R. L. Natural history of HPV infection across the lifespan: Role of viral latency. Viruses 9(10), 267 (2017).
Pimple, S. A. & Mishra, G. A. Global strategies for cervical cancer prevention and screening. Minerva ginecologica. 71(4), 313–320 (2019).
Bradford, L. & Goodman, A. Cervical cancer screening and prevention in low-resource settings. Clin. Obstet. Gynecol. 56(1), 76–87 (2013).
Behtash, N. & Mehrdad, N. Cervical cancer: Screening and prevention. Asian Pac. J. Cancer Prev. 7(4), 683–686 (2006).
Okedo-Alex, I. N., Uneke, C. J., Uro-Chukwu, H. C., Akamike, I. C., Chukwu, O.E. “It is what I tell her that she will do”: a mixed methods study of married men’s knowledge and attitude towards supporting their wives’ cervical cancer screening in rural South-East Nigeria. Pan Afr. Med. J. 36(1), (2020).
Ampofo, A. G., Adumatta, A. D., Owusu, E. & Awuviry-Newton, K. A cross-sectional study of barriers to cervical cancer screening uptake in Ghana: An application of the health belief model. PloS One 15(4), e0231459 (2020).
Sigfrid, L. et al. Integrating cervical cancer with HIV healthcare services: A systematic review. PloS One 12(7), e0181156 (2017).
Derbie, A. et al. Cervical cancer in Ethiopia: A review of the literature. Cancer Causes Control 34, 1–11 (2022).
Ayenew, A. A., Zewdu, B. F. & Nigussie, A. A. Uptake of cervical cancer screening service and associated factors among age-eligible women in Ethiopia: Systematic review and meta-analysis. Infect Agents Cancer https://doi.org/10.1186/s13027-020-00334-3 (2020).
Tsige, A. W. & Beyene, D. A. Cervical cancer: Challenges and prevention strategies: A narrative review. Health Sci. Rep. 7(6), e2149 (2024).
Acknowledgements
The authors would like to thank all the survey participants for their time and willingness to participate in the survey. We would also like to express our sincere gratitude to the data collectors for their support throughout the survey period.
Author information
Authors and Affiliations
Contributions
DAB and AWT contributed to the study design, performed the statistical analysis; wrote, reviewed, and edited both the original draft and final manuscript. SGA and HDW conceptualized and participated in the study design, critically reviewing, modifying, and analyzing the draft of the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Beyene, D.A., Ayele, S.G., Wubneh, H.D. et al. Male support for cervical cancer screening in Debre Berhan City Ethiopia a community based cross sectional survey. Sci Rep 14, 18302 (2024). https://doi.org/10.1038/s41598-024-69439-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69439-8
- Springer Nature Limited