Abstract
A higher heart rate is recognized as an independent risk factor for all-cause mortality and cardiovascular events in the general population. However, the association between elevated heart rate and clinical adverse outcomes in patients with non-dialysis-dependent chronic kidney disease (CKD) has not been sufficiently investigated. A total of 1353 participants enrolled in the Fukushima CKD Cohort Study were examined to investigate associations between resting heart rate and clinical adverse outcomes using Cox proportional hazards analysis. The primary outcome of the present study was all-cause mortality, with cardiovascular events as the secondary outcome. Participants were stratified into four groups based on resting heart rate levels at baseline (heart rate < 70/min, ≥ 70 and < 80/min, ≥ 80 and < 90/min, and ≥ 90/min). During the median observation period of 4.9 years, 123 participants died, and 163 cardiovascular events occurred. Compared with the reference level heart rate < 70/min group, the adjusted hazard ratios (HRs) for all-cause mortality were 1.74 (1.05–2.89) and 2.61 (1.59–4.29) for the heart rate ≥ 80 and < 90/min group and heart rate ≥ 90/min group, respectively. A significantly higher risk of cardiovascular events was observed in the heart rate ≥ 80/min and < 90/min group (adjusted HR 1.70, 1.10–2.62), but not in the heart rate ≥ 90/min group (adjusted HR 1.45, 0.90–2.34). In patients with non-dialysis-dependent CKD, a higher resting heart rate was associated with increased all-cause mortality.
Similar content being viewed by others
Introduction
An elevated resting heart rate has been identified as an independent risk factor for cardiovascular events and mortality. Notable studies, such as the Framingham Heart Study1, demonstrated that an increased resting heart rate is associated with an elevated risk of cardiovascular events and all-cause mortality across diverse populations.
Several prospective studies have examined the association between resting heart rate and all-cause mortality1,2,3,4,5. This association is not limited to cardiovascular mortality, but extends to deaths from various causes6.
However, specifically in patients with chronic kidney disease (CKD), there has been insufficient exploration of the correlation between heart rate and mortality. Beddhu et al. reported that a higher resting heart rate is associated with increased mortality in CKD7 in a study with a limited number of participants, but more investigation to elucidate the association of heart rate with adverse outcomes in patients with CKD is needed. Therefore, in the present study, the association of resting heart rate with adverse outcomes, such as all-cause mortality and cardiovascular events, was investigated in patients with non-dialysis-dependent CKD using longitudinal data from the Fukushima CKD Cohort Study.
Materials and methods
Study population
The Fukushima CKD Cohort study, a sub-cohort of the Fukushima Cohort study8,9,10,11,12,13, is a prospective survey of patient characteristics and outcomes for participants with non-dialysis-dependent CKD being followed at the Fukushima Medical University Hospital (Fukushima Prefecture, northeastern area of Japan). A total of 2724 patients were enrolled in the Fukushima Cohort study, of whom patients with CKD were included for the Fukushima CKD Cohort study. This study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) UMIN000040848. Patient enrollment was conducted between June 2012 and July 2014. The inclusion criteria were as follows: (1) Japanese patient living in Japan; (2) aged 18 years or older; and (3) CKD according to the definition of an estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 or proteinuria (positive dipstick results ≥ 1 +), with stable renal function for at least three months before entry into the study. The exclusion criteria were as follows: (1) undergoing renal replacement therapy in the last three months; (2) active malignancy; (3) infectious disease; (4) pregnancy; and (5) history of organ transplantation. Patients who had missing data for serum creatinine and heart rate were also excluded. All patients were under the care of nephrology or diabetology specialists. The protocol was approved by the Ethics Committee of Fukushima Medical University (approval no. 2001), and the study was conducted in accordance with the Declaration of Helsinki. All patients provided written, informed consent.
Data collection
Information regarding demographics, comorbidities, and medications at baseline was obtained from the patients’ medical records or blood examination results at registration. Serum creatinine was measured by an enzyme assay method. Estimated GFR (eGFR) was calculated using an estimation formula specifically designed for Japanese subjects14. The body mass index was calculated as weight (kg) divided by height squared (m2). Clinic blood pressures and resting heart rates were measured by trained staff using a standard sphygmomanometer or an automated device with the patient in a sitting position after 5 min of rest. Hypertension was defined as follows: (1) systolic blood pressure ≥ 140 mmHg; or (2) diastolic blood pressure ≥ 90 mmHg; or (3) the use of antihypertensive medication. Diabetes mellitus was identified as follows: (1) fasting plasma glucose concentration ≥ 126 mg/dL; (2) hemoglobin A1c value (National Glycohemoglobin Standardization Program) ≥ 6.5%; or (3) use of insulin or oral antihyperglycemic drugs. Dyslipidemia was defined as follows: (1) triglycerides ≥ 150 mg/dL; (2) low-density lipoprotein cholesterol concentration ≥ 140 mg/dL; (3) high-density lipoprotein cholesterol concentration < 40 mg/dL; or (4) use of antihyperlipidemic medications.
Exposure and outcomes
The primary exposure of interest for this study was resting heart rate. The study cohort was stratified into four groups by heart rate levels (heart rate < 70/min, ≥ 70 and < 80/min, ≥ 80 and < 90/min, and ≥ 90/min). Patients were followed until study withdrawal, loss to follow-up (i.e., transferred to other medical institutions, started maintenance renal replacement therapy, or death), or the end-of-study date (June 30, 2019). The primary outcome was all-cause mortality, and cardiovascular events were also measured as secondary outcomes. The cardiovascular events included fatal or nonfatal myocardial infarction, angina pectoris, sudden death, congestive or acute heart failure, arrhythmias, cerebrovascular disorder, chronic arteriosclerosis obliterans, and aortic disease. Information on cardiovascular events was captured from the medical records by attending physicians.
Statistical analyses
Categorical variables are expressed as percentages, and continuous variables are presented as median and interquartile range values. Values were compared using the Kruskal–Wallis test, nonparametric trend tests (Cuzick’s test), one-way analysis of variance (ANOVA), or Fisher’s exact test, as appropriate. Multiple imputation using chained equations with 20 datasets was used to complement the missing data after logarithmic transformation if the continuous variables did not follow the normal distribution. A Cox proportional hazards model analysis was used to examine the associations between heart rate and incidences of all-cause mortality and cardiovascular events. An unadjusted model and three adjusted models were created to adjust for covariates. Covariates considering to be related to the primary outcome were selected in three adjusted models. Model 1 was the unadjusted model, Model 2 included age and sex, Model 3 included Model 2 plus body mass index, smoking history, and comorbidities (diabetes mellitus, history of cardiovascular disease), and eGFR, and Model 4 included Model 3 plus systolic blood pressure, serum albumin, hemoglobin, proteinuria (dipstick), use of angiotensin-converting enzyme inhibitors (ACEis) or angiotensin II receptor blockers (ARBs), and use of β-blockers. Pearson product-moment, polyserial, or polychoric correlation coefficient, where appropriate, were calculated to confirm the correlation between heart rate and covariates used in the Cox analysis. To evaluate non-linear associations between heart rate and each clinical outcome, restricted cubic splines (Model 4-adjusted) with four knots were used. Subgroup analyses were also performed as sensitivity analyses of the primary and secondary outcomes. All analyses were conducted using STATA MP, version 16.1 (Stata Corp., College Station, TX).
Results
Patients’ characteristics
In the primary analysis, there were missing data for 3.3%, 5.5%, 3.1%, 2.7%, 1.7%, 35.1%, 10.4%, and 2.0% of patients for body mass index, smoking history, history of dyslipidemia, hyperuricemia, proteinuria (dipstick), proteinuria (g/gCr), serum albumin, and hemoglobin, respectively. According to the inclusion and exclusion criteria, a total of 1,353 subjects were enrolled in the present analyses of the 2724 subjects of the Fukushima Cohort study (Fig. 1). Baseline characteristics stratified by the resting heart rate level are shown in Table 1. The median age was 65 years, 56.7% were male, and the median eGFR was 52.2 mL/min/1.73 m2. The median heart rate was 76/min, and female and diabetes mellitus were more frequent in subjects with higher heart rates. Atrial fibrillation was seen in 8.9% of the subjects and were more frequent in subjects with higher heart rate. β-blockers were used in many subjects with heart rate < 70/min and the ≥ 90/min group.
Association between resting heart rate and all-cause mortality
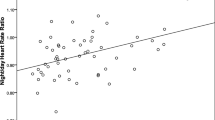
During the median observation period of 4.9 years, 123 of the 1,353 subjects died. The causes of death were: malignancy (n = 42), cardiovascular disease (n = 22), sepsis (n = 18), unknown (n = 15), and others (n = 26). Cox regression analyses showed that the heart rate ≥ 90/min group was at significantly higher risk for all-cause mortality, and this was significant after adjustment for covariates (Table 2). In model 4, the heart rate ≥ 80/min and < 90/min group was also at significantly higher risk for all-cause mortality, and the adjusted hazard ratios (HRs) were 1.74 (95% confidence interval, 1.05 to 2.89) and 2.61 (1.59 to 4.29) for the heart rate ≥ 80/min and < 90/min group and the heart rate ≥ 90/min group, respectively, compared with the reference heart rate < 70/min group. Using restricted cubic spline functions, there was a U-curve relationship between resting heart rate and the risk of all-cause mortality (Fig. 2A). Correlation coefficient between heart rate and covariates included in the multivariate adjusted models were calculated, and no strong correlations requiring consideration of multicollinearity were observed between these covariates. (R < 0.6 for all variables) (Supplemental Table S1).
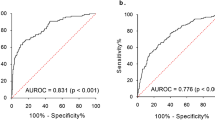
Distributions and Model 4-adjusted restricted cubic splines comparing the relationship of resting heart rate with clinical outcomes in 1,353 participants with non-dialysis-dependent CKD. Solid lines represent adjusted hazard ratio estimates, and dashed lines represent 95% confidence intervals. A All-cause mortality, B cardiovascular events. Model 4: adjusted for age, sex, body mass index, smoking history, diabetes mellitus, history of cardiovascular disease, eGFR, systolic blood pressure, serum albumin, hemoglobin, proteinuria, use of ACEis or ARBs, and use of β-blockers. eGFR, estimated glomerular filtration rate; ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
Association between resting heart rate and cardiovascular events
During the follow-up period, 163 of the 1353 subjects developed cardiovascular events. Details of these events were: heart failure (n = 64), cerebral infarction (n = 18), angina pectoris (n = 16), arrhythmia (n = 16), myocardial infarction (n = 15), cerebral hemorrhage (n = 15), aortic disease (n = 6), arteriosclerosis obliterans (n = 3), sudden death (n = 2), and others (n = 8). Cox regression analyses showed that patients with a higher heart rate were at higher risk for cardiovascular events, but only those with heart rate ≥ 80/min and < 90/min showed a significantly higher risk for cardiovascular events in Model 4, compared with the reference < 70/min group (Table 2). The adjusted HR was 1.70 (95% CI 1.10–2.62). A significantly higher risk of cardiovascular events was not observed in the heart rate ≥ 90/min group (adjusted HR 1.45, 0.90–2.34). Using restricted cubic spline functions, there was a non-linear relationship between resting heart rate and the risk of cardiovascular events (Fig. 2).
Sensitivity analyses
Subgroup analyses were performed for sensitivity analysis of the primary outcome (Fig. 3), and they showed that there were no interactions in subgroups by age, sex, eGFR, diabetes mellitus, proteinuria, and use of β-blockers (P values for interaction were 0.45, 0.49, 0.20, 0.87, 0.30, and 0.23, respectively). In analyses for the secondary outcome (Fig. 4), there were no interactions in subgroups by age, sex, eGFR, diabetes mellitus, proteinuria, and use of β-blockers (P values for interaction were 0.66, 0.92, 0.40, 0.64, 0.55, and 0.73, respectively). Cox regression analyses in subjects except for patients with atrial fibrillation were also performed for sensitivity analysis and the similar results were observed in relation of heart rate to the primary and secondary outcomes (Supplemental Table S2).
Discussion
In this study of the association between resting heart rate and adverse outcomes in patients with non-dialysis-dependent CKD, elevated heart rate was associated with a higher risk of all-cause mortality and cardiovascular events. Typically, the resting heart rate for adults falls between 60 and 100/min. The present results showed that a higher heart rate, even within the normal range, was associated with an increased risk of mortality and cardiovascular events.
Previous studies have consistently identified a higher heart rate (also even within the normal range) as an independent risk factor for all-cause mortality or cardiovascular events, not only in the general population, but also in patients with hypertension or coronary artery diseases1,2,15,16. However, whether this association holds true for the CKD population has not been examined sufficiently. Beddhu et al. investigated 460 CKD patients and found that a higher resting heart rate, even within the normal range (< 100/min), was associated with increased mortality and cardiovascular events7. In comparison with this previous study, the present sample size was larger, and there were adequate numbers of clinical outcomes, allowing for the sufficient and adequate adjustment of clinical parameters in the statistical analyses. From the present study, it can be concluded that a higher resting heart rate is an independent risk factor for all-cause mortality in patients with non-dialysis-dependent CKD.
A previous interventional study suggested that reducing heart rate could improve clinical outcomes17. Ivabradine, a selective inhibitor of the If current in the sinoatrial node of the heart, has shown a protective effect in patients with chronic heart failure by reducing the heart rate. The Systolic Heart failure treatment with the If inhibitor ivabradine Trial (SHIFT) demonstrated a reduced risk of a composite endpoint of cardiovascular death or heart failure hospitalization by adding ivabradine to standard therapy for patients with chronic heart failure and a left ventricular ejection fraction of ≤ 35%18. The patients in SHIFT had a baseline heart rate of ≥ 70/min. The present study supported the idea that reducing heart rate might be effective for CKD patients with a heart rate ≥ 70/min, since the lowest risk of mortality was seen in patients with heart rate < 70/min. This prompts the need for further interventional studies focusing on CKD patients.
Significantly higher risks of all-cause mortality were observed in the heart rate ≥ 90/min group in unadjusted model and any adjusted models, but a significantly higher risk of cardiovascular events was observed in the heart rate ≥ 80/min and < 90/min group only in the multivariate model (Model 4) including use of ACEis or ARBs and use of β-blockers as covariates. Although the close reasons for these results were unclear, use of β-blockers which decrease heart rate could be so important confounding factors between elevated heart rate and the risk of cardiovascular events. Cause-and-effect relationships between heart rate, use of β-blockers, and the risk of cardiovascular events cannot be inferred due to the observational nature of the present study, but it is needed to verify whether intervention for a higher heart rate could improve cardiovascular risk in this population in the future.
The mechanism linking higher resting heart rate to worse clinical outcomes is complex and multifactorial. Several hypotheses, such as reduced coronary artery perfusion19, progression of coronary atherosclerosis20,21, dysregulation of the autonomic nervous system22, increased levels of inflammation23, oxidative stress24, and endothelial dysfunction24,25,26 have been proposed to increase the risk of mortality or cardiovascular events. Although there were no interactions in any subgroups, stronger associations were observed between heart rate and the risk of all-cause mortality and cardiovascular events in groups with eGFR ≥ 45 mL/min/1.73 m2 and those without proteinuria. Effects of higher heart rate on the risk of all-cause mortality and cardiovascular events might be relatively weaker in advanced CKD subjects with decreased eGFR and overt proteinuria due to increasing the effects of other CKD specific risk factors including anemia, inflammation, and malnutrition.
The present study had several limitations. First, most previous studies used heart rate measured by electrocardiography as a parameter, whereas pulse rate measured by a standard sphygmomanometer or an automated device was used for the heart rate in the present study. Heart rate refers specifically to the number of heart beats per minute. Pulse rate also refers to the number of heart beats per minute, but it specifically refers to the pulsation of arteries that occurs as a result of the heart’s contractions. These terms are closely related and are indicative of the same physiological phenomenon, but they can have slightly different meanings, which is a limitation of this study. Second, cause-and-effect relationships between heart rate and clinical outcomes cannot be inferred due to the observational nature of this study. Furthermore, unmeasured variables, such as lifestyle factors (including alcohol consumption, sleeping, or physical activity), underlying health conditions (such as respiratory disorders), socioeconomic factors (including education, income, or access to healthcare), laboratory data (such as C-reactive protein), or other heart rate-modifying medications may act as confounding factors.
In summary, the results of the present study demonstrated that a higher resting heart rate was associated with all-cause mortality and cardiovascular events in patients with non-dialysis-dependent CKD. Interventional studies targeting CKD patients are needed to investigate whether a higher heart rate should be treated to improve clinical outcomes in this population. It is important to note that, though associations between higher heart rate and clinical adverse outcomes have been observed in various studies, the relationship between heart rate and mortality is complex, and other factors such as age, comorbidities, and overall cardiovascular health contribute to the overall risk profile of an individual; therefore, the management of heart rate should be individualized, and decisions regarding treatment strategies should be made based on an assessment of the patient’s overall health.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Gillman, M. W., Kannel, W. B., Belanger, A. & D’Agostino, R. B. Influence of heart rate on mortality among persons with hypertension: the Framingham Study. Am Heart J 125, 1148–1154. https://doi.org/10.1016/0002-8703(93)90128-v (1993).
Benetos, A., Rudnichi, A., Thomas, F. D. R., Safar, M. & Guize, L. Influence of heart rate on mortality in a French population. Hypertension 33, 44–52. https://doi.org/10.1161/01.hyp.33.1.44 (1999).
Kannel, W. B., Kannel, C., Paffenbarger, R. S. Jr. & Cupples, L. A. Heart rate and cardiovascular mortality: The Framingham Study. Am Heart J 113, 1489–1494. https://doi.org/10.1016/0002-8703(87)90666-1 (1987).
Hozawa, A. et al. Predictive value of ambulatory heart rate in the Japanese general population: the Ohasama study. J Hypertens 26, 1571–1576. https://doi.org/10.1097/HJH.0b013e3283041172 (2008).
Fujiura, Y. et al. Heart rate and mortality in a Japanese general population: An 18-year follow-up study. J Clin Epidemiol 54, 495–500. https://doi.org/10.1016/s0895-4356(00)00323-1 (2001).
Dyer, A. R. et al. Heart rate as a prognostic factor for coronary heart disease and mortality: Findings in three Chicago epidemiologic studies. Am J Epidemiol 112, 736–749. https://doi.org/10.1093/oxfordjournals.aje.a113046 (1980).
Beddhu, S., Nigwekar, S. U., Ma, X. & Greene, T. Associations of resting heart rate with insulin resistance, cardiovascular events and mortality in chronic kidney disease. Nephrol. Dial. Transplant. 24, 2482–2488. https://doi.org/10.1093/ndt/gfp057 (2009).
Tanaka, K. et al. Status of anemia according to underlying renal disease in chronic kidney disease: The Fukushima CKD cohort. Ann. Clin. Epidemiol. 3, 27–35. https://doi.org/10.37737/ace.3.1_27 (2021).
Tanaka, K. et al. Association between serum potassium levels and adverse outcomes in chronic kidney disease: The Fukushima CKD cohort study. Clin Exp Nephrol 25, 410–417. https://doi.org/10.1007/s10157-020-02010-7 (2021).
Kimura, H. et al. Association of polypharmacy with kidney disease progression in adults with CKD. Clin. J. Am. Soc. Nephrol. 16, 1797–1804. https://doi.org/10.2215/cjn.03940321 (2021).
Saito, H. et al. Xanthine oxidase inhibitors are associated with reduced risk of cardiovascular disease. Sci Rep 11, 1380. https://doi.org/10.1038/s41598-020-80835-8 (2021).
Saito, H. et al. Hematological parameters of anemia and prognosis of non-dialysis-dependent chronic kidney disease: the Fukushima CKD cohort study. Clin. Exp. Nephrol. https://doi.org/10.1007/s10157-022-02282-1 (2022).
Saito, H. et al. Predicting CKD progression using time-series clustering and light gradient boosting machines. Sci Rep 14, 1723. https://doi.org/10.1038/s41598-024-52251-9 (2024).
Matsuo, S. et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53, 982–992. https://doi.org/10.1053/j.ajkd.2008.12.034 (2009).
Farinaro, E. et al. Heart rate as a risk factor in hypertensive individuals. The Italian TensioPulse Study. Nutr Metab Cardiovasc Dis 9, 196–202 (1999).
Diaz, A., Bourassa, M. G., Guertin, M.-C. & Tardif, J.-C. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur. Heart J. 26, 967–974. https://doi.org/10.1093/eurheartj/ehi190 (2005).
Flannery, G., Gehrig-Mills, R., Billah, B. & Krum, H. Analysis of randomized controlled trials on the effect of magnitude of heart rate reduction on clinical outcomes in patients with systolic chronic heart failure receiving beta-blockers. Am J Cardiol 101, 865–869. https://doi.org/10.1016/j.amjcard.2007.11.023 (2008).
Swedberg, K. et al. Ivabradine and outcomes in chronic heart failure (SHIFT): A randomised placebo-controlled study. The Lancet 376, 875–885. https://doi.org/10.1016/s0140-6736(10)61198-1 (2010).
Kohler, A. et al. Relationship between the resting heart rate and the extent of coronary artery disease as assessed by myocardial perfusion SPECT. Swiss Medical Weekly https://doi.org/10.4414/smw.2012.13660 (2012).
Huikuri, H. V. et al. Heart rate variability and progression of coronary atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 19, 1979–1985. https://doi.org/10.1161/01.atv.19.8.1979 (1999).
Kaplan, J. R., Manuck, S. B. & Clarkson, T. B. The influence of heart rate on coronary artery atherosclerosis. J Cardiovasc Pharmacol 10 Suppl 2, S100–102; discussion S103 (1987).
Arntz, H. R. et al. Circadian variation of sudden cardiac death reflects age-related variability in ventricular fibrillation. Circulation 88, 2284–2289. https://doi.org/10.1161/01.cir.88.5.2284 (1993).
Sajadieh, A. Increased heart rate and reduced heart-rate variability are associated with subclinical inflammation in middle-aged and elderly subjects with no apparent heart disease. Eur. Heart J. 25, 363–370. https://doi.org/10.1016/j.ehj.2003.12.003 (2004).
Custodis, F. et al. Heart rate reduction by ivabradine reduces oxidative stress, improves endothelial function, and prevents atherosclerosis in apolipoprotein E-deficient mice. Circulation 117, 2377–2387. https://doi.org/10.1161/circulationaha.107.746537 (2008).
Chatzizisis, Y. S. et al. Role of endothelial shear stress in the natural history of coronary atherosclerosis and vascular remodeling: molecular, cellular, and vascular behavior. J Am Coll Cardiol 49, 2379–2393. https://doi.org/10.1016/j.jacc.2007.02.059 (2007).
Williams, B. Mechanical influences on vascular smooth muscle cell function. J Hypertens 16, 1921–1929. https://doi.org/10.1097/00004872-199816121-00011 (1998).
Acknowledgements
The authors would like to thank Ayumi Kanno for her assistance in data collection.
Funding
K. Asahi reports receiving research funding from Chugai Pharmaceutical, Kowa Pharmaceutical, and Ono Pharmaceutical. J. J. Kazama reports receiving research funding from Chugai, Kissei, Kyowa-Kirin, Ono, and Tanabe-Mitsubishi. All remaining authors have nothing to disclose.
Author information
Authors and Affiliations
Contributions
HS and KT wrote the paper with input from all authors. All authors have reviewed and approved the manuscript. Research idea and study design: KT; data acquisition: KT, HK; data analysis/interpretation: HS, KT, MS, KA, TW; statistical analysis: HS; supervision or mentorship: TW, JK.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saito, H., Tanaka, K., Ejiri, H. et al. Elevated resting heart rate is associated with mortality in patients with chronic kidney disease. Sci Rep 14, 17372 (2024). https://doi.org/10.1038/s41598-024-67970-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67970-2
- Springer Nature Limited