Abstract
The differences between the serum albumin determined by bromocresol green (BCG) and immunonephelometry (IN) were inconsistent in past studies, and the samples were all adults. We sought to determine the differences in children and reveal the impacts of these differences on the clinical diagnosis and treatments of primary nephrotic syndrome (PNS). Repeated measurements from 576 PNS children showed that albumin measured by BCG and IN (ALB-B and ALB-I) were 19.95 (11.15) g/L and 15.30 (11.05) g/L, respectively, and the mean difference was 4.68 g/L (P < 0.001). The cut-offs we calculated for hypoalbuminemia and severe hypoalbuminemia based on the IN were 25 and 15 g/L, which were 5 g/L lower than the cut-offs recommended by KIDGO, respectively. A pair of historical control samples (206 vs. 216) with ALB-B or ALB-I showed that the proportion of severe hypoalbuminemia was 14.60% greater in IN group (75.20% vs. 60.60%, P < 0.001). The misdiagnosis rate of severe hypoalbuminemia by IN was 33.77% when 20 g/L rather than 15 g/L was used as the cut-off. Furthermore, the proportion of patients receiving albumin injections increased by 10.20%, and the average consumption increased by 97.06% (P = 0.01) along with the use of IN. So, our results suggested that the difference between ALB-B and ALB-I led to misdiagnosis and prescription abuse in PNS children.
Similar content being viewed by others
Introduction
Albumin is the most abundant protein in human plasma and plays a variety of physiological roles in the body1,2,3. Hypoalbuminemia is a necessary feature of primary nephrotic syndrome (PNS) and is caused mainly by a large loss of albumin via the urine4. The determination of serum albumin concentration is undoubtedly highly important for diagnosis and clinical strategies for PNS patients.
For years, laboratory medicine specialists have held heated discussions about the accuracy of albumin detection methods. Several technological innovations have been made in the detection of albumin5,6,7,8. At present, bromocresol green (BCG) and bromocresol purple (BCP) are the albumin detection reagents installed in automated biochemical analysers in most hospitals worldwide9. The detection principle of both methods is colorimetry and both methods are easily interfered, especially in patients with nephrotic syndrome10. The new immunological assays based on antigen‒antibody binding are robust, and the immunonephelometric assay (IN) is perceived as the most likely method for accurate quantification of serum albumin in clinical application because it is the most selective11.
Indeed, studies from the field of laboratory medicine have shown that there were numerically significant differences between colorimetric and immunological assays on different detection platforms12,13,14. These biases were particularly pronounced in patients with chronic kidney disease. It was reported that BCG assays overestimate albumin concentration in hemodialysis patients with an absolute deviation of up to 10 g/L compared to that of the immuno-turbidimetric assay15 but Maarten et al. reported that the difference is 5 g/L in dialysis patients16. The observation report of 19 patients with membranous nephropathy (MN) from multiple centers revealed a difference of 5.1–8.0 g/L between the detection of albumin measured by BCG and IN (ALB-B and ALB-I) at different centers17. In a study on PNSs, patients were divided into three groups according to the ALB-I, and the ALB-B within each group were significantly higher than the values determined by IN assay, especially in the severe hypoalbuminemia group12. Currently, only a few papers have reported the biases, but the values of the difference are inconsistent12,15,17. Additionally, no relevant research was claimed in children with PNS.
It was also noted in the Kidney Disease: Improving Global Outcomes 2021 Clinical Practice Guideline (KDIGO 2021) that different detection methods affect the serum albumin concentration18. Most notably, KDIGO 2021 did not specify the detection method used when setting the cut-offs for diagnosis and therapy. In the definition relating to nephrotic syndrome in children, KDIGO stated that hypoalbuminemia was defined as a serum albumin < 30 g/L. It also suggested that intravenous albumin should be considered when patients with an albumin < 20 g/L were diuretics -resistant. Therefore, clinicians are currently using uniform cut-offs for albumin to manage patients without considering the methods used.
The purpose of this study was to analyse the difference between albumin measured by BCG and IN (ALB-B and ALB-I) using a set of repeated measurements. Furthermore, we extracted a set of historical control samples with the aim to reveal the possible impacts on the overdiagnosis of severe hypoproteinaemia and the overuse of clinical albumin preparations.
Results
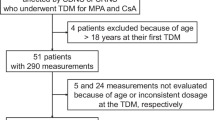
We retrieved 1364 serum samples from 642 hospitalized children with NS discharged between March 2017 and August 2021. Among the children, 591 with PNS were aged between 1 and 18 years. One serum sample was randomly taken from each patient, so the total number of samples obtained was 591, of which 15 were insufficient. Finally, 576 samples were included to repeat the detection of ALB-B and ALB-I. See Fig. 1 for further details.
The median age (IQR) of the participants who underwent repeated measurements was 4.70 (5.47) years, and 72.92% were male. A total of 46.35% of participants had mild edema, and 33.51% had severe edema. ALB-B and ALB-I were 19.95 (11.15) g/L and 15.30 (11.05) g/L, respectively (Table 1). The Bland‒Altman plot analysis showed that the difference between ALB-B and ALB-I was statistically significant (P < 0.001) with a mean of 4.68 (4.50, 4.86) g/L (see Supplementary Fig. S1 online).
The correlation between ALB-B and ALB-I was good, with a correlation coefficient of 0.98 (P < 0.001). According to the Passing‒Bablok regression equation (y = -4.41 + 0.97x) established by using all included samples, when ALB-B is 20 g/L, the corresponding ALB-I is 14.99 g/L, approximately 15 g/L. The corresponding ALB-I was 24.69 g/L, approximately 25 g/L, when ALB-B was 30 g/L (Fig. 2). Specifically, it was more appropriate to use 15 g/L as the cut-off for identifying severe hypoalbuminemia and 25 g/L for detecting hypoalbuminemia in children with PNS when we used IN to detect albumin on our platform. We also used the samples with ALB-B < 30 g/L to explore the threshold for severe hypoalbuminemia and ALB-B > 20 g/L for hypoalbuminemia, and the cut-offs obtained were consistent with that described above (see Supplementary Fig. S2 online).
In the absence of distinctions in the clinical diagnosis and treatment guidelines, we used a pair of historical control groups to explore the impact of measuring ALB by IN on the diagnosis of severe hypoalbuminemia, the use of human albumin injections, and medical expenses. A total of 216 cases were included in the BCG group, and 206 were included in the IN group. The screening process was shown in Fig. 1.
As shown in Table 2, there was no statistically significant difference between the two groups in age and sex (P > 0.05). The difference in admission weight was significant between the two groups (P = 0.02). We considered the severity of disease to be comparable between the two groups, as the hospitalization duration and UV/weight did not significantly differ (P > 0.05). There was a significant difference in ALB between the BCG and IN groups (P < 0.01). The frequency distributions of ALB in the two groups were shown in Fig. 3. The proportion of patients with severe hypoproteinaemia was greater in the IN group than in the BCG group when 20 g/L was used as the cut-off (75.20% vs. 60.60%, P < 0.01), but then, the enhancement was not significant when 15 g/L was used as the cut-off in the IN group (60.60% vs. 62.60%, P = 0.69), for which the misdiagnosis rate reached 33.77%. The proportion of inpatients using human albumin injections increased by 10.20% along with the use of IN (30.09% vs 40.29%, P = 0.01). Among 26 patients with ALB-I between 15 to 20 g/L, 4 (15.38%) used human albumin injections (see Supplementary Fig. S3 online). Furthermore, the average consumption per case of albumin injections increased by 97.06% during hospitalization (0.68 ± 2.35 vs. 1.34 ± 3.71, P = 0.01). The average expenditure per case of albumin injections increased by 99.33% during hospitalization (27.19 ± 94.38 vs. 54.20 ± 150.66, P = 0.01).
Discussion
We verified the difference of serum albumin detected by BCG and IN in children with PNS and it was 4.68 g/L. The increase in proportion of severe hypoproteinemia among historical control samples (60.60% vs. 75.20%) revealed that the wasting of albumin via urine in the patients was overestimated in the IN group. The misdiagnosis rate was up to 33.77% when using 20 g/L as the cut-off compared to 15 g/L in the IN group. The proportion of patients receiving intravenous albumin injections increased by 10.20%, and the average expenditure on albumin injection during hospitalization almost doubled in the IN group.
Previous studies have shown that the differences between albumin detection by BCG and IN were inconsistent in adults with chronic kidney disease, and they almost ranged from 2 to 10 g/L12,13,14,16,17. We found that the difference in PNS children was approximately 5 g/L, which did not conflict with the results of adult studies. The mechanisms by which different methods lead to differences in the detection of albumin has been described in a considerable number of papers. The nonspecific binding of α2-megaglobulin to the BCG dye was an important reason for the overestimation of the serum albumin in patients with NS by the BCG assay. The α2-macroglobulin concentration was positively correlated with the difference between the concentration of albumins determined by BCG and nephelometry12. The addition of α2-macroglobulin to an equal concentration of albumin resulted in a dose-dependent elevation in the test results of albumin by BCG for α2-macroglobulin19.
On the other hand, only one paper has addressed the impacts of biases resulting from different albumin measurement methods on clinical decision-making, and they focused on anticoagulant therapy for patients with membranous nephropathy and nephrotic syndrome17. The serum albumin was an important reference for clinical decision-making regarding intravenous albumin therapy. The impacts of assay bias on clinical decisions were an important issue that we hoped to understand. As mentioned above, in 2019, the clinical laboratory at our hospital began to introduce the IN to detect albumin. At that time, the clinicians were not aware of the changes and possible differences in the serum albumin concentration caused by different assays. We believed that the severity of the disease in IN group was similar to that in the same period last year, as there was no significant difference in urine volume between the two groups. It was clarified that 10% of patients might have been assigned intravenous albumin prescriptions that needed not be involved, of which 20% have ALB-I among 15–20 g/L and others < 15 g/L. By twice the consumption, it can be inferred that clinicians' judgments on the dosages of albumin injections have also been affected, not just whether to use them. Nevertheless, Albumin, as a blood product, is not only expensive but also substantially increases the filtration load of the glomerulus. It even causes damage to glomerular epithelial cells, leading to protein overload nephropathy. In other words, excessive intravenous albumin prescription can aggravate the progression of glomerulosclerosis in children with PNS.
We proposed that the protein consumption status of patients was underestimated when the albumin concentration determined by the BCG method was used. We believe that the diagnostic threshold for the IN method should be lowered. According to the conversion formula proposed in our platform, it may be more appropriate that 25 g/L was the new cut-off for diagnosing hypoalbuminemia by IN, and accordingly, 15 g/L was to diagnose severe hypoalbuminemia by IN. our conclusions came from the data generated by the Beckman biochemical analysis platform in a single center. It should be noted that our conclusions were more informative for users of the Hitachi 7600 and the Beckman Immage 800 analyzers. In fact, the BCG and immunological methods showed substantial variations were platform-dependent, ranging from 3.2 to 4.6% and 2.6 to 5.3%, respectively20. Therefore, researchers should strive to promote the harmonization of the serum albumin measurement worldwide13,21. Meanwhile, we appealed internal comparison within the platform and different clinical centers needed to compare the BCG or BCP data with the IN method in their platforms when they used the IN method to detect albumin.
In this study, we examined only the discrepancies of the two detection assays in PNS and did not include patients with secondary nephrotic syndrome (SNS) and other chronic kidney diseases. The study also lacked comparisons across multiple centers and different platforms. Further in-depth research in this field will improve the understanding of the differences in albumin detection methods among patients with different disease states. The harmonization of albumin measurements and the clarification of diagnostic thresholds should be strong directions for future research.
In summary, we analysed the differences and conversion relationships between serum ALB concentrations detected by BCG and IN in a large number of PNS children. Using IN to detect albumin without adjusting the diagnostic threshold will significantly lead to overestimating the severity of the wasting of albumin in patients and excessive use of intravenous albumin injections. It is important to pay attention to the threshold differences between albumin detection methods to reduce misdiagnosis and inappropriate clinical decisions.
Methods
Participants and samples
This study involved two parts of participants with PNS in which we conducted repeated measurements and historical control analyses of albumin measured by BCG and IN assays. The participants for repeated measurement analyses included 576 PNS children discharged from the hospital between March 2017 and August 2021. The sera were collected from routine laboratory test items, and the residual serum samples were stored in the biological sample library at -80 °C. From these residual samples, we randomly selected one serum sample for each patient. The serum samples were tested for repeated measurements of the concentration of albumin by BCG and IN (ALB-B and ALB-I, g/L).
The set of historical control samples was obtained from children with PNS for whom the albumin concentration was measured during hospitalization. The IN group consisted of children with PNS discharged between September 2019 and January 2020. During this time, IN was just beginning to be implemented at this hospital, replacing BCG, and clinicians and testing personnel were unaware of the differences between the two measured values. Children with PNS discharged in the same month of the previous year (September 2018 to January 2019) were adopted as controls (BCG group). The albumin concentration of children in the BCG group was measured by BCG.
Inclusion and exclusion criteria
In both populations, all the subjects were discharged NS children aged 1–18 years from the Division of Nephrology of a Women and Children's Hospital. The exclusion criteria were as follows: (1) individuals with SNS and congenital nephrotic syndrome (CNS); (2) individuals with a previous history of other acute or chronic kidney disease, patients with abnormal ultrasound examination of the urinary system (e.g., deformities, cysts, hydrops, or stones); (3) patients with an identified acute or chronic illness (diabetes mellitus, thyroid dysfunction, polycystic ovary syndrome, obesity, fatty liver, or familial hypercholesterolemia); and (4) patients with other systemic diseases, such as hematological diseases, cardiovascular diseases, connective tissue diseases, tumors, and obvious infections. Children who were transferred to the intensive care unit during hospitalization were excluded. The diagnostic criteria for PNS in children are proteinuria and hypoalbuminemia with or without edema and hyperlipidemia18. Children with serum ALB < 30 g/L were considered to have hypoalbuminemia.
Instruments and methods for serum albumin
The included serum samples were used for albumin concentration detection via the use of BCG and IN on our platform. The BCG assay was implemented on a Hitachi 7600 automatic analyser using the albumin reagent from Maccura, Inc. The calibrator (Lot: 0422061) of BCG albumin from Maccura was traced to ERM-DA470k/IFCC; the typical value was 47.6 g/L, and the uncertainty was 2.5 g/L (k = 2). IN was implemented on Beckman Coulter-specific protein analysers (Immage 800) using the albumin reagent from Beckman Coulter, Inc., with a goat anti-human albumin antibody. The calibrator (Lot: PN449730) of the IN albumin measuring system from Beckman Coulter was traced to the reference material ERM-DA470k/IFCC; the typical value was 36.1 g/L, and the uncertainty was 0.884 g/L (k = 2). The two methods were performed according to the instructions of each manufacturer.
Demographic, clinical and biochemical information
In addition, we collected data regarding age, sex, admission weight (weight, kg), hospitalization duration, clinical type, histopathologic diagnosis, degree of edema, urinary protein, use of diuretics 24 h before sampling, 24-h urine volume (UV, ml), creatinine (Cr, µmol/L), Cystatin C (CysC, mg/L), urea (mmol/L), total cholesterol (TC, mmol/L), and triglyceride (TG, mmol/L) of the repeated measurement participants with PNS.
Data collected about the historical control participants with PNS included age, sex, weight (kg), hospitalization duration, ALB-B (g/L), ALB-I (g/L), UV/weight (ml/kg), use of human albumin injections and average consumption and expenditure of albumin injections per case/weight during hospitalization (ACAI/weight, g/kg; AEAI/weight, CNY/kg).
Statistics
Variables with skewed distributions were described by medians (interquartile range, IQR). Enumeration data were expressed as incidence rates or constituent ratios. For the repeated measurement data, Wilcoxon paired rank tests and paired chi-square tests were used to compare differences between groups. For historical control data, Wilcoxon rank tests and chi-square tests were used to compare differences between the BCG and IN groups. The above analyses were performed with SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Furthermore, we applied MedCalc Statistical Software version 20.100 (MedCalc Software Ltd, Ostend, Belgium) to perform Spearman correlation analyses. Passing‒Bablok regression analyses were conducted to show the relationship between BCG and IN, and a Bland‒Altman plot was drawn with bias calculations and 95% confidence intervals. The conversion relationship between the two detection values was obtained by the Passing‒Bablok regression equation. All differences were considered to be statistically significant if P was < 0.05.
Ethics statement
This project was approved and the informed consent was waived by Research Ethics Committee of Guangzhou Women and Children’s Medical Center, Guangzhou Medical University (No.: 247A01). The data was de-identified and did not contain any personal information. The study was conducted in compliance with the Declaration of Helsinki as well as in accordance with local guidelines and regulations.
Data availability
The datasets used during the current study are available from the corresponding author upon reasonable request.
References
Peters, T. Jr. Serum albumin. Adv. Protein Chem. 37, 161–245. https://doi.org/10.1016/s0065-3233(08)60065-0 (1985).
De Simone, G., di Masi, A. & Ascenzi, P. Serum albumin: A multifaced enzyme. Int. J. Mol. Sci. 22, 10086. https://doi.org/10.3390/ijms221810086 (2021).
Fanali, G. et al. Human serum albumin: From bench to bedside. Mol. Aspects Med. 33, 209–290. https://doi.org/10.1016/j.mam.2011.12.002 (2012).
Orth, S. R. & Ritz, E. The nephrotic syndrome. N. Engl. J. Med. 338, 1202–1211. https://doi.org/10.1056/NEJM199804233381707 (1998).
Rees, V. H., Fildes, J. E. & Laurence, D. J. The dye-binding capacity of human plasma determined fluorimetrically and its relation to the determination of plasma albumin. J. Clin. Pathol. 7, 336–340 (1954).
Keyser, J. W. Determination of serum albumin. Clin. Chem. 14, 360–367 (1968).
Gulyassy, P. F., Depner, T. A. & Ma, W. K. Four methods for determining albumin in azotemic sera evaluated. Clin. Chem. 27, 322–325 (1981).
Kumar, D. & Banerjee, D. Methods of albumin estimation in clinical biochemistry: Past, present, and future. Clin. Chim. Acta 469, 150–160. https://doi.org/10.1016/j.cca.2017.04.007 (2017).
Garcia Moreira, V. et al. Overestimation of albumin measured by bromocresol green vs. bromocresol purple method: Influence of acute-phase globulins. Lab. Med. 49, 355–361. https://doi.org/10.1093/labmed/lmy020 (2018).
Delanghe, J. R., Speeckaert, M. M., Delanghe, S. E. & De Buyzere, M. L. Albumin assays and clinical decision-making in nephrotic syndrome patients. Kidney Int. 96, 248–249. https://doi.org/10.1016/j.kint.2019.03.025 (2019).
Whicher, J. T., Price, C. P. & Spencer, K. Immunonephelometric and immunoturbidimetric assays for proteins. Crit. Rev. Clin. Lab. Sci. 18, 213–260. https://doi.org/10.3109/10408368209085072 (1983).
Ueno, T., Hirayama, S., Sugihara, M. & Miida, T. The bromocresol green assay, but not the modified bromocresol purple assay, overestimates the serum albumin concentration in nephrotic syndrome through reaction with alpha2-macroglobulin. Ann. Clin. Biochem. 53, 97–105. https://doi.org/10.1177/0004563215574350 (2016).
Bachmann, L. M., Yu, M., Boyd, J. C., Bruns, D. E. & Miller, W. G. State of harmonization of 24 serum albumin measurement procedures and implications for medical decisions. Clin. Chem. 63, 770–779. https://doi.org/10.1373/clinchem.2016.262899 (2017).
Rami Arab, L. et al. Impact of albumin assays in the diagnosis of malnutrition in hemodialysis patients: A cohort study. J. Ren. Nutr. 33, 332–336. https://doi.org/10.1053/j.jrn.2022.10.001 (2023).
Carfray, A. et al. Albumin as an outcome measure in haemodialysis in patients: The effect of variation in assay method. Nephrol. Dial. Transplant. 15, 1819–1822. https://doi.org/10.1093/ndt/15.11.1819 (2000).
Kok, M. B., Tegelaers, F. P., van Dam, B., van Rijn, J. L. & van Pelt, J. Carbamylation of albumin is a cause for discrepancies between albumin assays. Clin. Chim. Acta 434, 6–10. https://doi.org/10.1016/j.cca.2014.03.035 (2014).
van de Logt, A. E. et al. The bias between different albumin assays may affect clinical decision-making. Kidney Int. 95, 1514–1517. https://doi.org/10.1016/j.kint.2019.01.042 (2019).
Kidney Disease: Improving Global Outcomes Glomerular Diseases Work, G. KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int. 100, S1-S276, https://doi.org/10.1016/j.kint.2021.05.021 (2021).
Xu, Y., Wang, L., Wang, J., Liang, H. & Jiang, X. Serum globulins contribute to the discrepancies observed between the bromocresol green and bromocresol purple assays of serum albumin concentration. Br. J. Biomed. Sci. 68, 120–125. https://doi.org/10.1080/09674845.2011.11730338 (2011).
van Schrojenstein Lantman, M. et al. Albumin determined by bromocresol green leads to erroneous results in routine evaluation of patients with chronic kidney disease. Clin. Chem. Lab. Med. 61, 2167–2177. https://doi.org/10.1515/cclm-2023-0463 (2023).
van Schrojenstein Lantman, M., van de Logt, A. E., Thelen, M., Wetzels, J. F. & van Berkel, M. Serum albumin measurement in nephrology: Room for improvement. Nephrol. Dial. Transplant. 37, 1792–1799. https://doi.org/10.1093/ndt/gfaa375 (2022).
Acknowledgements
This research was supported by grants from the Science and Technology Program of Guangzhou (Grant No. 202102010222). Thank Clinical Biological Resource Bank of Guangzhou women and children’s medical center for providing the clinical samples.
Author information
Authors and Affiliations
Contributions
XG, YH, HT and JT designed the study; FL, GL and LW carried out the experiments; YL, JZ, XY, LP XL, XC and ZX collected the samples and data; HT and GL analysed the data and generated the figures; FL and LW contributed the materials and methodology. HT, YH and XG drafted and revised the paper; All authors commented on the manuscript and approved final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tang, H., Liu, F., Li, G. et al. The different serum albumin assays influence the prescriptions in children with primary nephrotic syndrome. Sci Rep 14, 17682 (2024). https://doi.org/10.1038/s41598-024-67441-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67441-8
- Springer Nature Limited