Abstract
In France, 110,000 patients are admitted to hospital per year for stroke. Even though the relationship between stroke and risk factors such as low socio-economic status is well known, research in the spatial distribution (SD) of stroke as a contributing risk factor is less documented. Understanding the geographic differences of the disease may improve stroke prevention. In this study, a statistical spatial analysis was performed using a French cohort (STROKE 69) to describe spatial inequalities in the occurrence of stroke. STROKE 69 was a cohort study of 3,442 patients, conducted in the Rhône department of France, from November 2015 to December 2016. The cohort included all consecutive patients aged 18 years or older, with a likelihood of acute stroke within 24 hours of symptoms onset. Patients were geolocated, and incidence standardized rates ratio were estimated. SD models were identified using global spatial autocorrelation analysis and cluster detection methods. 2,179 patients were selected for analysis with spatial autocorrelation methods, including 1,467 patients with stroke, and 712 with a transient ischemic attack (TIA). Within both cluster detection methods, spatial inequalities were clearly visible, particularly in the northern region of the department and western part of the metropolitan area where rates were higher. Geographic methods for SD analysis were suitable tools to explain the spatial occurrence of stroke and identified potential spatial inequalities. This study was a first step towards understanding SD of stroke. Further research to explain SD using socio-economic data, care provision, risk factors and climate data is needed in the future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Stroke is a growing public health concern in developed countries1. In France, 110,000 patients are hospitalized per year for stroke2. The occurrence of the disease requires responsive management to reduce the risk of complications, making stroke prevention a priority. For this purpose, the relationship between individual risk factors, such as hypertension, diabetes, being overweight, and smoking, and stroke occurrence have been well documented3,4.
The risk of stroke and low socio-economic status is also well known1,5,6, however, research on the existence of spatial distribution (SD) and differences of stroke occurrence is still minimal. Referenced geographical data, such as the GPS coordinates and postal codes of patients or care facilities, can be used to conduct spatial and risk analysis of SD in any given living territory, and may influence towards better targeted health policies for stroke patients. Studies using statistical spatial analysis methods have been performed on other diseases7,8,9,10, however few have been conducted on stroke in the world11,12.The best-known case of significant SD analysis in stroke was the disproportionately high mortality rates measured in the 8-state region in the southeast of the United States, named the Stroke Belt13.
In France, to date, no studies have used this approach to characterize SD of stroke. Existing studies in the country focused on stroke hospitalization rates14 and mortality distribution2,15,16 using an epidemiological approach and a spatial statistical analysis approach respectively. SD studies have not, to date, been conducted to identify differences in stroke occurrence locations. The objective of this study was to describe the SD and geographic differences of stroke using an existing cohort and spatial health tools at a department-scale.
Methods
Study settings and population
The study was conducted in the Rhône department located in the Auvergne-Rhône-Alpes region in France. According to the national census, there were 1,835,90317 inhabitants in the department in 2016, with a population over 65 years around 16%, for an area of 3,249 km².
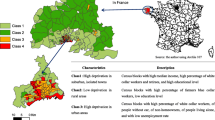
The study was based on patients from the STROKE 69 cohort, which included all consecutive patients aged 18 years or older with the likelihood of acute stroke within 24 hours of symptoms onset, admitted to the emergency departments (EDs), a primary stroke center (PSC) or comprehensive stroke center (CSC) (Fig. 1) from November 2015 to December 2016 (n = 3,442). STROKE 69 aimed to assess the impact of previous stroke awareness campaigns on the management of acute stroke in the Rhône department.
Rhône department stroke care organization and location in France (Source: CorineLandCover and STROKE 69). Maps were created using ArcGIS 10.6.1 Software (Environmental Systems Research Institute [ESRI] Inc., Redlands, CA; http://www.esri.com/).
Ethical approval
STROKE 69 was a non-interventional study funded by the Ministry of Health. Patients were informed of the study and could refuse to participate. A non-return was considered as an informed consent. The study was approved by the ethics committee according to the French legislation and the “Commission Nationale de l’Informatique et des Libertés” (CNIL).
Study protocol
A patient’s place of residence and the place of onset symptoms were collected in the STROKE 69 cohort. Patients were firstly located according to their place of residence, available on the STROKE 69 Case Report Form (CRF) as 82% of patients in the cohort had symptoms at home. From a patient’s home, the SAMU Centre 15, the French emergency medical service (EMS), was contacted and stroke suspected. At the request of the SAMU, patients were transferred to an ED, PSC or CSC, to have the diagnosis confirmed. The final diagnosis of a patient was then registered in the STROKE 69 CRF. All patients with a confirmed diagnosis of hemorrhagic stroke, ischemic stroke (IS) or transient ischemic attack (TIA) were included in the study. A second analysis was conducted on IS and TIA alone, since the management process for IS and TIA differs compared to hemorrhagic stroke.
The place of residence was used to analyze the incidence of stroke. Patients were geolocated with the exact address of residence and age standardization of stroke incidence rates at bundles of statistical information; Ilots Regroupés pour l’Information Statistique (IRIS) scale was performed. The IRIS are small zones grouped for statistical information and are the smallest administrative division in France with respect to demographic and geographical criteria18. During the time of the study, the Rhône department was divided into 769 IRIS.
Data analysis
A protocol with predefined outcome variables was written before any analysis or inspection of the data started (https://clinicaltrials.gov/ct2/show/NCT02596607?term=NCT02596607&rank=1). The STROKE 69 dataset was geocoded based on the residential address of the stroke event using ArcGIS 10.6.1 Software (Environmental Systems Research Institute [ESRI] Inc., Redlands, CA19). Spatial autocorrelation analysis was conducted using ArcGIS 10.6.1. Spatial autocorrelation analysis and cluster detection were the main domain of Geographic Information System (GIS). The identification of spatial models was crucial to understand the behavior of the spatial phenomena20. Spatial autocorrelation methods were based on algorithms “to determine which areas were outliers in comparison to their neighbors and could take the underlying distribution of the population into account”7.
An analysis of global models was first used to describe the SD trends and to identify IRIS with a high incidence risk. Statistically significant spatial clusters were then identified at a local level. This approach characterized the SD of stroke at a territorial level, in its globality, and then locally by IRIS. At the local level, IRIS was statistically identified and represented on a map.
Two statistical tests were used at a global level. The global level was defined as the general trend given for the SD of stroke at the Rhône scale (the global territory without distinction of IRIS). This trend was expressed in the form of a spatial logic of stroke distribution: dispersed, aggregated or without spatial logic, randomly. The first test was the Moran’s Index (Moran’s I), used to measure spatial autocorrelation, which is the trend in spatial distribution. The Moran’s I indicated the level of correlation of the data, between −1 (no correlation, dispersed) and 1 (correlation, clustered). When the value was 0, the correlation was random21. The Moran’s I designated positive spatial autocorrelation but could not make a difference between high-intensity values aggregation (hot-spots) and low-intensity values aggregation (cold-spots). The Getis-Ord General G statistic22 was used as a second test to measure the clustering degree, from 0 (low values) to 1 (high values) to allow the distinction between hot and cold spots. The Getis-Ord General G assumed that the general trend of stroke in the territory was aggregated. The Getis-Ord General G represented the level of clustering of the sample at the Rhône department scale (global scale) in relation to the average values: a significant positive value corresponded to clusters of high values (many strokes) and a significant negative value corresponded to a cluster of low values (fewer strokes). According to the p values and Z scores, the results of the two tools for spatial statistics were interpreted to reject or accept the null hypothesis23.
At the local level, the tests were calculated by IRIS. The assumption was that IRIS were aggregated. The tests were used to determine the form of aggregation. Each IRIS was studied according to the neighboring IRIS. The IRIS that most closely resembled each other were considered aggregated. The aggregates were represented on a map, so that one could include several IRIS. First, the declination of Moran’s I, the Local Indicators of Spatial Association (LISA)21 was used. LISA allowed the identification of both spatial clusters of entities with features of the same magnitude and aberrant spatial points24. It was used to identify locations of statically significant clusters with either higher values (HH) or lower values (LL) than the average age-standardized stroke incidence rates at a statistical significance level of <0.05.
LISA also distinguished the aberrant point where a low value was mainly surrounded by high values (LH), and aberrant point which a high-intensity value was surrounded mainly by low-intensity values (HL). The second local declination was the Getis-Ord Gi*25, the declination of General G statistic. Getis-Ord GI* was used to identify statistically significant spatial clusters with high and low intensities, on condition that the p value was very small. With this method, the higher the statistically significant positive Z scores were, the more intense the cluster of high-intensity values (hot-spot) became. Similarly, the more intense the cluster of low-intensity values (cold-spot) were, the lower the statistically significant negative Z scores became.
Ethical standards
Stroke 69 study was funded by the Ministry of Health and received ethics committee approval according to the French legislation. This study was a non-interventional study where patients were informed and free to refuse participation. It was approved by the ethical committee and the “Commission Nationale de l’Informatique et des Libertés” (CNIL).
Results
Among the 3,442 patients included in the STROKE 69 cohort, 2,694 had an IS, a hemorrhagic stroke or a TIA. Patients that were not located in the Rhône department in France, non-residents and/or patients with an unknown residential address were excluded from the study, so that the study population of 2,179 patients wasanalyzed with the spatial autocorrelation methods (Fig. 2).
There were 1,467 patients diagnosed with stroke and 712 with TIA. Strokes and TIA proportions were higher for patients over 75 years, and for both sexes. The proportion of women was higher for patients aged more than 85 years (44.8% vs 19.4% for IS; 47.3% vs 20.7% for hemorrhagic; 33.8% vs 15.6% for TIA). The mean age was lower for TIA (71.8) than stroke patients (75.5). The age-standardized stroke incidence rates per 100,000 during the period were 41.9 for IS, 8 for hemorrhagic strokes, and 24.1 for TIA (Table 1).
In order to identify geographical patterns, the age-standardized stroke incidence rates were calculated per 1,000 people at the IRIS scale (Fig. 3). Rates were spatially lower in the south location of the department. The higher rates were located in the north. There was no significant difference between all diagnosis and only TIA/IS rates, however TIA/IS incidence had higher rates. Rates of 5.48 per 1,000 and 9.38 were measured in the cities of Ouroux and Saint-Mamert, located at the northern limit of the department.
Age-standardized stroke incidence rates reported to 1,000 persons. (A) for all diagnosis (hemorrhagic stroke, ischemic stroke (IS) and transient ischemic attack (TIA)). (B) only for IS and TIA. Maps created using ArcGIS 10.6.1 Software (Environmental Systems Research Institute [ESRI] Inc., Redlands, CA; http://www.esri.com/).
The calculated Moran’s I for all diagnosis was 0.004, Z score = 1.34, and p value = 0.18. SD of age-standardized stroke incidence per 1,000 persons was thus random. SD was also random for only IS and TIA. Spatial relations were analyzed according to the inverse of distance (10 kms) between stroke occurrence rates. The methodology was tested with the same spatial relation conceptualization, which was the inverse of distance (10 kms) for Getis-Ord General G statistic. The sample was random with calculated Getis-Ord General G statistic (close to 0) (Z score = 0.16 and the p value = 0.87). Both methods measured the sample autocorrelation level. However, the calculation algorithms were different, so indices did not measure autocorrelation in the same way. For the second time, these results were compared at a local level.
The Anselin Local Moran’s I (for studying clusters and outliers) and the Getis-Ord Gi* statistic (for analyzing hot spots and cold spots) were mapped (Fig. 4) to measure autocorrelation on parts of the territory because Moran’s I and General G statistic are global spatial statistics applied to the entire area studied. Even if the distribution was random at a global level, clusters and outliers and hot and cold spots at the local level existed (Fig. 4). The maps on the left of Fig. 4 showed statistically significant clusters of high-rates incidence (HH). Maps on the right of Fig. 4 showed the hot spots. The cities in the north of the department had high rates, including a few cities in the Lyon metropolitan area and its close boundary. Based on the hypothesis that the place of residence was the place of the symptom onset, the clusters of low-rates incidence (LL) may be explained by the border effects, which were the proximity of ED and PSC located at the boundary of the Rhône department, in which patients were admitted and had faster management. These were two different methods of calculating spatial representations and SD of stroke, but cities were common to both approaches, including HH clusters and hot spots in the north of the department and the western part of the metropolitan area.
Mapping of Local Anselin Moran’s I (LISA) (left maps) and Getis-Ord Gi* (right maps) for age-standardized stroke incidence per 1,000 persons. (A) for all diagnosis (hemorrhagic stroke, ischemic stroke (IS) and transient ischemic attack (TIA)). (B) only for IS and TIA. Maps created using ArcGIS 10.6.1 Software (Environmental Systems Research Institute [ESRI] Inc., Redlands, CA; http://www.esri.com/).
Discussion
Analysis of the global spatial distribution of stroke in Rhône department highlighted that stroke incidence was randomly distributed. The random distribution meant there was no logical pattern to explain the incidence of stroke at a county/department level of a country. Clusters and hot spots were, however, observed when local indicators of spatial analysis methods were calculated. The general distribution logic on the department was not necessarily the same, at a local scale, as shown by LISA and Getis-Ord Gi* (Fig. 4). In addition, there was no clear difference observable between the whole sample and the only IS and TIAs sample. Thus, SD of stroke was not homogeneous and geographic differences existed.
This main strength of this study relied on its internal validity based on the statistical analysis conducted and the quality of collected data. The STROKE 69 cohort demonstrated to provide a comprehensive account of the stroke occurrence in the Rhône department, which may show the same in any given area over any given time period. The spatial model analyses were thus representative of the studied territory and represented an effective management of stroke in the Rhône department. The presence of the exact residential address of patients (identical to the occurrence place in 82% of cases) was also necessary to carry out a fine granulometric analysis of the territory at the IRIS scales. The smaller the scale, the more significant the spatial distribution analysis of the real trends in the territory were made10,26,27.
Another advantage of this study was the complementary use of two statistical analysis tools, which made it possible to confirm and validate the results7,28 for the identification and validation of clusters of high stroke rates common to both. Areas with statistically higher stroke rates were particularly relevant to identify as a first step in targeting effective preventative actions and understanding the cause of high numbers of stroke patients in those areas. This complementarity was useful for tools at a global scale: Moran’s I identified the SD trend and Getis-Ord General G statistic confirmed the results in the case of a trend towards aggregation, by specifying whether the aggregates were globally distributed in high or low values. At a local level, if clusters of high and low values (HH and LL) were identified by LISA, they would be confirmed by Getis-Ord Gi* (hot and cold spots). These techniques were robust and allowed us to identify statistically different areas.
The main study limitation was the small sample size due to the limited inclusion period for the STROKE 69 cohort study, which was not designed for spatial model analysis. This issue was particularly observed at the global level analysis based on Moran’s I and Getis-Ord General G statistics. The sample size may partly explain the non-significant results leading to a random distribution, especially since clusters at the local level still seemed to exist. The inclusion of a larger number of patients may have allowed for a greater statistical power and validation of the results from the spatial model analysis. The concern of a limited sample size could be addressed using data from a regional stroke registry, over a longer period of time, as it has been the case in France16,26 and in the United States to study SD of stroke mortality11.
Increasing the scale of analysis may however decrease the geographical accuracy in patient location and data compliance. In France, the availability of a large-scale administrative database from Hospital Discharge Diagnosis Records based on the International Classification of Disease (10th revision) only included patient location at a postal code level. Additionally, the validity of medical data recorded in this database was questioned29,30. The risk associated with the use of these databases is based particularly on the confirmed diagnosis of stroke, at the risk of analyzing false positives and dismissing false negatives.
Another limitation to this study was the presence of clusters of low values (LL) identified by the LISA method, due to the edge effects principle. Patients were located in the IRIS situated at the border with neighboring departments. Some ED or PSC were located in these neighboring departments, but closer to patients than an ED or PSC in the Rhône department, making patient care faster. The presence of these LL clusters was therefore potentially due to the admission of these patients to an ED or PSC other than those of the Rhône department based on the hypothesis that the place of residence was the place of symptom onset and management. While not all patients with a stroke and/or residents of the Rhône department were included, the cohort still reflected the reality of management in the department. The population identified as having a high spatial logic of stroke incidence in the Rhône department, corresponded to the population that could be managed and treated in the departmental ED and PSC.
The presence of areas containing IRIS with high values raised concerns as well,. The first hypothesis based on existing literature may have linked it to the rural location31,32 of the clusters/hot spots, and the socio-economic level of the population1,33, particularly on the level of social deprivation34,35. Analysis, however, based on the socio-economic level have to consider the age in the choice of explanatory variables as stroke mostly affects the elderly. Similarly, and in direct link with deprivation, data on eating habits and sedentary life profiles3,36 of included patients could be worth collecting.
The density of the supply of care could also be considered, specifically with general practitioners to determine if there could be a relation between stroke occurrence risk and the density of general practitioners per inhabitant37. In addition, the spatial analysis could be supplemented by a temporal analysis of stroke incidence. A trend analysis would determine whether specific periods are more likely to result in a stroke. This would rely on climatic variables, such as air temperature38, air pressure or humidity39, or air pollutants40 to explain potential trends. The analysis of explanatory factors for the presence of clusters may also become the subject of future research. The identification of clusters was a necessary step in formulating hypotheses on the presence of stroke risk occurrence places, and therefore at identifying a population at risk to a worsened access to treatment.
Conclusion
Methods of SD analysis were suitable tools at explaining stroke occurrence based on an epidemiological cohort and identifying a risk population of worsened access to treatment. The analyses conducted in this study based on the STROKE 69 cohort, at a department level in France, identified areas at risk of over incidence, particularly in the north region of the department where over incidence clusters (HH) and hot spots were observed.
To our knowledge, and to date, this was the first study based on a spatial analysis tool in France which analyzed stroke incidence. This study is a step forward towards understand SD for stroke. Further research to explain SD using socio-economic data, care provision, risk factors and climate data is needed in the future.
References
Cox, A. M., McKevitt, C., Rudd, A. G. & Wolfe, C. D. Socioeconomic status and stroke. Lancet Neurol. 5, 181–188 (2006).
Lecoffre, C. et al. L’accident vasculaire cérébral en France: patients hospitalisés pour AVC en 2014 et évolutions 2008-2014. Bull. Épidémiologique Hebd. 5, 84–94 (2017).
O’Donnell, M. J. et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. The Lancet 376, 112–123 (2010).
Liao, Y., Greenlund, K. J., Croft, J. B., Keenan, N. L. & Giles, W. H. Factors Explaining Excess Stroke Prevalence in the US Stroke Belt. Stroke 40, 3336–3341 (2009).
Brown, P., Guy, M. & Broad, J. Individual socio-economic status, community socio-economic status and stroke in New Zealand: A case control study. Soc. Sci. Med. 61, 1174–1188 (2005).
Kunst, A. E. et al. Socioeconomic inequalities in stroke mortality among middle-aged men an international overview. Stroke 29, 2285–2291 (1998).
Sasson, C. et al. Identifying High-risk Geographic Areas for Cardiac Arrest Using Three Methods for Cluster Analysis: identifying high-risk geographic areas for cardiac arrest. Acad. Emerg. Med. 19, 139–146 (2012).
Fontanella, C. A. et al. Mapping suicide mortality in Ohio: A spatial epidemiological analysis of suicide clusters and area level correlates. Prev. Med. 106, 177–184 (2018).
Kihal-Talantikite, W. et al. Developing a data-driven spatial approach to assessment of neighbourhood influences on the spatial distribution of myocardial infarction. Int. J. Health Geogr. 16, 22 (2017).
Roth, G. A. et al. Trends and Patterns of Geographic Variation in Cardiovascular Mortality Among US Counties, 1980-2014. JAMA 317, 1976–1992 (2017).
Karp, D. N. et al. Reassessing the Stroke Belt: Using Small Area Spatial Statistics to Identify Clusters of High Stroke Mortality in the United States. Stroke 47, 1939–1942 (2016).
Schieb, L. J., Mobley, L. R., George, M. & Casper, M. Tracking stroke hospitalization clusters over time and associations with county-level socioeconomic and healthcare characteristics. Stroke 44, 146–152 (2013).
Lanska, D. J. Geographic distribution of stroke mortality in the United States: 1939-1941 to 1979-1981. Neurology 43, 1839–1851 (1993).
Lachkhem, Y., Minvielle, É. & Rican, S. Geographic Variations of Stroke Hospitalization across France: A Diachronic Cluster Analysis. Stroke Research and Treatment https://www.hindawi.com/journals/srt/2018/1897569/ https://doi.org/10.1155/2018/1897569 (2018).
Lecoffre, C. et al. Mortalité par accident vasculaire cérébral en France en 2013 et évolutions 2008-2013. Bull. Épidémiologique Hebd. 5, 95–100 (2017).
Roussot, A. et al. The use of national administrative data to describe the spatial distribution of in-hospital mortality following stroke in France, 2008–2011. Int. J. Health Geogr. 15, (2016).
Populations légales des départements en 2016 − Populations légales |Insee. https://www.insee.fr/fr/statistiques/3677771?sommaire=3677855 2016.
Définition - IRIS|Insee. https://www.insee.fr/fr/metadonnees/definition/c1523.
ESRI- GIS Mapping Software, Solutions, Services, Map Apps, and Data. http://www.esri.com/.
Griffith, D. A. Spatial autocorrelation: a primer. Assoc. Am. Geogr. (1987).
Anselin, L. Local Indicators of Spatial Association—LISA. Geogr. Anal. 27, 93–115 (1995).
Ord, J. K. & Getis, A. Local spatial autocorrelation statistics: distributional issues and an application. Geogr. Anal. 27, 286–306 (1995).
Moran, P. A. The Interpretation of Statistical Maps. J. R. Stat. Soc. Ser. B Methodol. 10, 243–251 (1948).
Renard, F. Flood risk management centred on clusters of territorial vulnerability. Geomat. Nat. Hazards Risk 8, 525–543 (2017).
Getis, A. & Ord, J. K. Local spatial statistics: An overview. in Spatial Analysis: Modeling in A GIS Environment 261–277 (1996).
Grimaud, O. et al. Incidence of Stroke and Socioeconomic Neighborhood Characteristics An Ecological Analysis of Dijon Stroke Registry. Stroke 42, 1201–1206 (2011).
Pedigo, A. & Aldrich, T. & others. Neighborhood disparities in stroke and myocardial infarction mortality: a GIS and spatial scan statistics approach. BMC Public Health 11, 1 (2011).
van Rheenen, S., Watson, T. W. J., Alexander, S. & Hill, M. D. An Analysis of Spatial Clustering of Stroke Types, In-hospital Mortality, and Reported Risk Factors in Alberta, Canada, Using Geographic Information Systems. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 42, 299–309 (2015).
Goldberg, M., Coeuret-Pellicer, M., Ribet, C. & Zins, M. Cohortes épidémiologiques et bases de données d’origine administrative - Un rapprochement potentiellement fructueux. médecine/sciences 28, 430–434 (2012).
Haesebaert Julie et al. Can Hospital Discharge Databases Be Used to Follow Ischemic Stroke Incidence? Stroke 44, 1770–1774 (2013).
Humphreys, J. S. Delimiting ‘Rural’: Implications of an Agreed ‘Rurality’ Index for Healthcare Planning and Resource Allocation. Aust. J. Rural Health 6, 212–216 (1998).
Mullen, M. T. et al. Disparities in accessibility of certified primary stroke centers. Stroke 45, 3381–3388 (2014).
Kapral, M. K., Wang, H., Mamdani, M. & Tu, J. V. Effect of socioeconomic status on treatment and mortality after stroke. Stroke 33, 268–275 (2002).
Havard, S. et al. A small-area index of socioeconomic deprivation to capture health inequalities in France. Soc. Sci. Med. 67, 2007–2016 (2008).
Macleod, M., Lewis, S. & Dennis, M. Effect of deprivation on time to hospital in acute stroke. J. Neurol. Neurosurg. Psychiatry 74, 545–546 (2003).
Diaz, K. M. et al. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: A national cohort study. Ann. Intern. Med. 167, 465–475 (2017).
Souty, C. & Boëlle, P.-Y. Improving incidence estimation in practice-based sentinel surveillance networks using spatial variation in general practitioner density. BMC Med. Res. Methodol. 16, (2016).
Lichtman, J. H., Leifheit-Limson, E. C., Jones, S. B., Wang, Y. & Goldstein, L. B. Average Temperature, Diurnal Temperature Variation, and Stroke Hospitalizations. J. Stroke Cerebrovasc. Dis. 25, 1489–1494 (2016).
Gantelet, M. Pneumothorax et pression atmosphérique: étude multicentrique de type cas/croisée en France. Rev. D’épidémiologie Santé Publique 64, (2016).
Mateen, F. J. & Brook, R. D. Air Pollution as an Emerging Global Risk Factor for Stroke. JAMA 305, 1240–1241 (2011).
Acknowledgements
This work was performed within the framework of the RHU MARVELOUS (ANR-16-RHUS-0009) of Université Claude Bernard Lyon 1 (UCBL), within the program “Investissements d’Avenir” operated by the French National Research Agency (ANR). The authors gratefully acknowledge Nathalie Perreton, Claire Della Vecchia, Héla Kerd, Ouazna Tassa, Johanna Vivard, Audrey Maurin, Elodie Castelletta, Adèle Perrin, Xue Yufeng, Julie Martin, Jeanice Amiot, Marine Barral, Guillaume Pinte, Cécile Foukoun-Matchikou and Aurélie Rochefolle for their efficient participation in data collection, entry and management. We also would like to gratefully thank Anaïs Giroux and TLM360 for their proofreading and help with the English editing. The authors would also like to thank the two anonymous reviewers and editor for their comments on an earlier draft of this paper. The STROKE 69 investigators were Laurent Derex, Serkan Cakmak, Sylvie Meyran, Bruno Ducreux, Christelle Pidoux, Thomas Bony, Marion Douplat, Véronique Potinet and Alain Sigal.
Author information
Authors and Affiliations
Contributions
J.F., F.R. and K.T. conceived the study. J.F., F.R., K.T., L.D., C.E.K. and A.M.S. participated in the design. A.T., A.C., E.B. and M.D. participated in the collection, entry and management of data. JF carried out the GIS, statistical and mapping analyses, and drafted the manuscript. All authors read and approved the final manuscript. All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Freyssenge, J., Renard, F., Khoury, C.E. et al. Spatial distribution and differences of stroke occurrence in the Rhone department of France (STROKE 69 cohort). Sci Rep 10, 9910 (2020). https://doi.org/10.1038/s41598-020-67011-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-67011-8
- Springer Nature Limited