Abstract
Patients with left ventricular dysfunction (LVD) undergoing cardiac surgery have a high mortality rate. Levosimendan, a calcium sensitizer, improves myocardial contractility without increasing myocardial oxygen demand. It is not clear whether levosimendan can reduce mortality in cardiac surgery patients with LVD. The PubMed, Embase, and Cochrane Central databases were searched to identify randomized trials comparing levosimendan with conventional treatment in cardiac surgery patients with LVD. We derived pooled risk ratios (RRs) with random effects models. The primary endpoint was perioperative mortality. Secondary endpoints were renal replacement treatment, atrial fibrillation, myocardial infarction, ventricular arrhythmia, and hypotension. Fifteen studies enrolling 2606 patients were included. Levosimendan reduced the incidence of perioperative mortality (RR: 0.64, 95%CI: 0.45–0.91) and renal replacement treatment (RR:0.71, 95%CI:0.52–0.95). However, sensitivity analysis, subgroup analysis and Trial Sequential Analysis (TSA) indicated that more evidence was needed. Furthermore, levosimendan did not reduce the incidence of atrial fibrillation (RR:0.82, 95%CI:0.64–1.07), myocardial infarction (RR:0.56, 95%CI:0.26–1.23), or ventricular arrhythmia (RR:0.74, 95%CI:0.49–1.11), but it increased the incidence of hypotension (RR:1.11,95%CI:1.00–1.23). There was not enough high-quality evidence to either support or contraindicate the use of levosimendan in cardiac surgery patients with LVD.
Similar content being viewed by others
Introduction
More than 1 million patients undergo cardiac surgery with cardiopulmonary bypass (CPB) in the United States and Europe every year1. Despite the reduction in perioperative mortality observed over the past two decades, the risk of cardiac surgery in patients with severe left ventricular dysfunction (LVD) remains high, especially with regard to the likelihood of developing postoperative low cardiac output syndrome (LCOS)2. Up to 20% of patients developed acute perioperative LVD after cardiac surgery3,4, which is a major complication of cardiac surgery and increases mortality significantly5. This syndrome may necessitate inotropic drugs (catecholamines and phosphodiesterase type 3 [PDE-3] inhibitors) and mechanical circulatory support (intra-aortic balloon pump). Although these agents may increase cardiac output, they are associated with an increase in morbidity and mortality6,7. New drugs without obvious adverse effects are needed.
Levosimendan, a calcium sensitizer, improves myocardial contractility without increasing myocardial oxygen demand8. It has been proven to be effective by small clinical trials and meta-analyses in patients with LVD undergoing cardiac surgery9,10,11,12,13,14. However, 3 recent, large, randomized, clinical trials (RCT) produced results inconsistent with previous findings and did not found that levosimendan used either prophylactically or after cardiac surgery is effective in reducing mortality in cardiac surgery patients15,16,17. Given the conflicting evidence about the use of levosimendan in patients with LVD undergoing cardiac surgery, we performed this meta-analysis to evaluate the use of levosimendan in patients with LVD undergoing cardiac surgery.
Methods
Search strategy and selection criteria
This meta-analysis was performed in accordance of the Preferred Reporting Items for System Reviews and Meta-analyses (PRISMA) Statement18. We systemically searched PubMed, Embase, and Cochrane Library for relevant articles published before September 1, 2017. The search term was “levosimendan.” The search was combined with filters to identify RCTs in the PubMed and EMBASE databases. Results were limited to trials published in English. We manually searched the reference lists of relevant studies, reviews, editorials, and letters to identify further articles. We used Endnote (Thompson ISI ResearchSoft, Philadelphia, PA, US) to manage relevant articles and remove duplicate articles.
Study criteria, quality assessment, and data extraction
Studies were included if they met the following criteria: (1) the study design was a RCT; (2) all patients were with LVD before or after cardiac surgery; (3) patients were randomly assigned to levosimendan group or the traditional treatment group; (4) relevant data were retrievable. The definition of LVD was defined by each included study. When relevant data were missing, authors were contacted by e-mail, before excluding the references for inaccessibility of data.
The primary endpoint was perioperative mortality. Secondary endpoints included renal-replacement therapy, atrial fibrillation, myocardial infarction, ventricular arrhythmia, and hypotension. All clinical endpoints were evaluated according to per protocol definitions. We judged study quality by evaluating trial procedures for random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), and incomplete outcome data (attrition bias). The Cochrane Reviewer’s Handbook 4.2 was used to assess risk of bias.
Relevant data abstraction was completed by 2 independent investigators (PF Chen and JB Huang). Disagreements were resolved by consensus or a third investigator (XQ Hu). We abstracted the following data from the selected articles: first author, publication date, study design, characteristics of included participants, total number of levosimendan group and conventional treatment group, events in the levosimendan group and conventional treatment group, duration of follow-up, primary study endpoints, and other key outcomes.
Data analysis
Reported event frequencies were used to calculate risk ratios (RRs) with 95% confidence intervals (CI). Heterogeneity between studies was checked and quantified using the I2 statistic, with I2 < 25% considered low and I2 > 50% high. The random-effects model was used in this analysis. The random effects model has wider confidence intervals and provides more conservative and robust results than the fixed-effect model, better accounting for inter-study differences. Data analysis was performed on an intention-to-treat basis. Sensitivity analyses were performed to assess the contribution of each study to the pooled estimation by excluding individual trials one at a time and recalculating the pooled RR estimation for the remaining studies. Publication bias was assessed using the Egger linear regression test and visual inspection of funnel plots. All analyses were performed using Review Manger Software (Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014).
Trial Sequential Analysis (TSA)
Cumulative meta-analyses are prone to produce type I and type II errors because of repeated testing of significance as trial data accumulates. Statistically significant small trials are often overruled when results from adequately powered and bias-protected trials emerge19,20. TSA is similar to interim analyses in a single trial in which monitoring boundaries are used to determine whether a trial could be terminated early when a P value is sufficiently small to show the anticipated effect. Analysis was performed using Trial Sequential Analysis Viewer (0.9.5.9 Beta) anticipating a 25% relative risk reduction for efficacy outcome, α = 5% and 1 − β = 80% and estimating the required diversity adjusted information size. This methodology has been described in detail21,22.
Outcomes
Search results and bias assessment
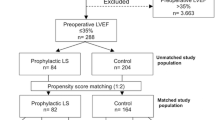
As reported in Fig. 1, the combined search strategy identified 273 potential relevant manuscripts, 22 studies were finally retrieved for more detailed assessment. Finally, 15 RCTs were included in this meta-analysis, covering a total of 2606 patients11,12,13,15,16,17,23,24,25,26,27,28,29,30,31. Characteristics of the included trials were shown in Table 1. Clinical heterogeneity was mostly due to differences in inclusion criteria, left ventricular ejection fraction (LVEF), levosimendan dose, traditional treatment, and duration of follow-up. Here, 10 studies used levosimendan in CABG. The 5 remaining studies included CABG and valve surgery. LVEF varied between 18% and 50%. Dose varied between 10 and 12 μg/kg as intravenous bolus and between 0.025 and 0.2 μg/kg as a continuous infusion. The duration of follow-up varied greatly as well. Most studies were confined to hospitalization. Six trials were multi-center. We used the Cochrane Reviewer’s Handbook 4.2 to assess risk of bias (Supplementary Fig. 1). Study quality appraisal indicated that studies were of variable quality and that 5 of them had a low risk of bias.
Quantitative Data Synthesis
Perioperative mortality
Our analysis showed that use of levosimendan in patients with LVD undergoing cardiac surgery was associated with a significant reduction in perioperative mortality (RR: 0.64, 95%CI:0.45–0.91, P = 0.01, I2 = 15%) (Fig. 2). However, in the TSA, the cumulative Z-curve crossed the traditional boundary (P = 0.05) but not the trial sequential monitoring boundary, indicating lack of a firm evidence for a 25% reduction in perioperative mortality with levosimendan treatment compared with traditional treatment (Fig. 3). The small sample size was not large enough to draw this conclusion that levosimendan reduced perioperative mortality. Sensitivity analyses were performed by excluding individual trials one at a time and recalculating the pooled RR estimation for the remaining studies, which indicated that both Levin29 and Levin13 could influence the overall effect (Table 2). In this way, the results of sensitivity analysis and TSA showed that this result is not solid. Subgroup analysis was performed to produce more robust results (Table 3). The results of subgroup differed greatly. The reduction in mortality was confirmed when the studies comparing levosimendan with other inotropic agents (catecholamines and phosphodiesterase type 3 [PDE-3] inhibitors) were included (RR:0.37, 95%CI:0.19–0.69, P = 0.003, I2 = 0%). However, compared with placebo, levosimendan did not reduce perioperative mortality (RR:0.75, 95%CI:0.49–1.14, P = 0.17, I2 = 18%). Multi-center studies did not demonstrate that levosimendan could reduce perioperative mortality (RR:0.75, 95%CI:0.39–1.09, P = 0.10, I2 = 53%). Studies with levosimendan loading bolus showed that levosimendan could improve clinical outcomes (RR:0.51, 95%CI:0.34–0.77, P = 0.001, I2 = 0%). The reduction in mortality was not confirmed in patients undergoing valve surgery (RR:0.64, 95%CI: 0.12–3.38, P = 0.6, I2 = 31%). However, perioperative mortality was lower in patients undergoing CABG (RR:0.45, 95%CI: 0.29–0.71, P = 0.0005, I2 = 0%).
Secondary endpoints
Renal-replacement therapy was lower in the levosimendan group in random effects (RR:0.71, 95%CI:0.52–0.95, P = 0.01, I2 = 0%) (Supplementary Fig. 2). However, in the TSA, the cumulative Z-curve crossed the traditional boundary (P = 0.05) but not the trial sequential monitoring boundary, indicating lack of a firm evidence for a 25% reduction in renal replacement with levosimendan treatment compared with traditional treatment (Supplementary Fig. 3). The small sample size was not large enough to draw this conclusion that levosimendan reduced the incidence of renal-replacement treatment. We performed sensitivity analyses and found Levin29, Levin13, Baysal25, and Mehta17 all affected the overall effect (Supplementary Table 1). All of this evidence indicated that there was not enough evidence to support the idea that levosimendan could reduce renal-replacement therapy. Levosimendan did not reduce the incidence of atrial fibrillation (RR:0.82 95%CI: 0.64–1.07, P = 0.38, I2 = 66%)(Supplementary Fig. 4), myocardial infarction (RR:0.56, 95%CI:0.26–1.23, P = 0.15, I2 = 33%) (Supplementary Fig. 5), or ventricular arrhythmia (RR:0.74, 95%CI:0.49–1.11, P = 0.14, I2 = 45%) (Supplementary Fig. 6). Levosimendan increased the incidence of hypotension (RR:1.11,95%CI:1.00–1.23, P = 0.14, I2 = 0%) (Supplementary Fig. 7).
Discussion
This meta-analysis, which contained the largest number of patients with LVD undergoing cardiac surgery of any such analysis, demonstrated that there is no solid evidence suggesting that levosimendan treatment could reduce perioperative mortality, renal replacement treatment and atrial fibrillation, myocardial infarction, or ventricular arrhythmia. In fact, levosimendan might increase the incidence of hypotension.
Previous trials have demonstrated that levosimendan can increase cardiac stroke volume without increasing myocardial oxygen demand, and reduce peripheral resistance32, and levosimendan treatment was associated with lower incidence of perioperative LCOS and atrial fibrillation, shorter mechanical ventilation and ICU stays, and lower 30-day mortality relative to traditional treatments among LVD patients undergoing cardiac surgery29,33. However, most trials were small, single-center studies without robust evidence. The 3 recent large randomized clinical trials (LEVO-CTS, CHEETAH, and LICORN) provided new evidence. None of these 3 trials indicated that levosimendan had benefits with respect to clinical outcomes, which was consistent with our analysis15,16,17.
There are many possible reasons for the heterogeneous results of studies with levosimendan in the situation of cardiac surgery. Other inotropic agents (catecholamines and phosphodiesterase type 3 [PDE-3] inhibitors) are associated with an increase in morbidity and mortality. The benefits of levosimendan may be attributed to decreased usage of other inotropic agents in previous studies. As suggested in previous clinical trials and meta-analyses, levosimendan may benefit only patients who had severe LVD at baseline, and needed more inotropic agents17,34. Many confounding factors, such as patient’s baseline characteristics, coexisting diseases, medications, or surgeon’s experience may affect the outcomes. With the advancement of surgical techniques, the declining death rate makes it harder to demonstrate a minor benefit of additional therapy with regard to overall mortality. An adequately convincing clinical study evaluating the effect of levosimendan treatment on perioperative mortality would require more patients, including high-risk patients. All of these factors contributed to the varied outcomes.Our meta-analysis did not find that levosimendan infusion could reduce the incidence of atrial fibrillation in patients with LVD undergoing cardiac surgery. The effects of levosimendan on atrial fibrillation differed greatly. The recent large randomized clinical trials (LEVO-CTS, CHEETAH, and LICORN) did not indicate an increased incidence of atrial fibrillation in the levosimendan group. However, the REVIVE II study reported a greater rate of atrial fibrillation in the levosimendan group35. Given this confusing situation, more clinical trials are needed.Although our meta-analysis did not demonstrate that levosimendan treatment was associated with a significant reduction in renal replacement treatment relative to traditional treatment, levosimendan groups tended to have fewer patients undergoing renal replacement therapy, even when Levin29 and Levin13 were excluded. Fedele et al. demonstrated that levosimendan has both an immediate renoprotective effect, mediated by a selective arterial and venous renal vasodilating action, and a slower cardiac-enhancing function32. Yakut N et al. also found that levosimendan significantly alleviated ischemia reperfusion injury in the renal tubules36. However, all of these studies had very small sample sizes, which does not lend confidence to their conclusions. Large clinical trials with convincing evidence are needed to resolve this confusing situation.
Limitations
Our conclusions should be viewed in the context of the limitations of this work. First, although there was no apparent heterogeneity in statistical analysis, the heterogeneity in clinical trials and methodology were inevitable. This included different risk profiles of the included patients, and varied dosage of levosimendan. Second, although we performed an extensive search strategy, some trials might not be included in our meta-analysis. However, this meta-analysis is the largest population-based analysis of levosimendan in patients with LVD undergoing cardiac surgery. More clinical trials are needed to evaluate the effects of levosimendan.
Conclusion
There was not enough high-quality evidence to either support or contraindicate the use of levosimendan in cardiac surgery patients with LVD.
References
Mozaffarian, D. et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation 133, e38–360 (2016).
Algarni, K. D., Maganti, M. & Yau, T. M. Predictors of low cardiac output syndrome after isolated coronary artery bypass surgery: trends over 20 years. Ann Thorac Surg 92, 1678–1684 (2011).
Mebazaa, A. et al. Clinical review: practical recommendations on the management of perioperative heart failure in cardiac surgery. Crit Care 14, 201 (2010).
Lomivorotov, V. V., Efremov, S. M., Kirov, M. Y., Fominskiy, E. V. & Karaskov, A. M. Low-Cardiac-Output Syndrome After Cardiac Surgery. J Cardiothorac Vasc Anesth 31, 291–308 (2017).
Maganti, M. et al. Predictors of low cardiac output syndrome after isolated mitral valve surgery. J Thorac Cardiovasc Surg 140, 790–796 (2010).
Hillis, L. D. et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J Am Coll Cardiol 58, e123–210 (2011).
Hillis, L. D. et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 143, 4–34 (2012).
Takahashi, R., Talukder, M. A. & Endoh, M. Inotropic effects of OR-1896, an active metabolite of levosimendan, on canine ventricular myocardium. Eur J Pharmacol 400, 103–112 (2000).
Pollesello, P., Parissis, J., Kivikko, M. & Harjola, V. P. Levosimendan meta-analyses: Is there a pattern in the effect on mortality. Int J Cardiol 209, 77–83 (2016).
Landoni, G. et al. Reducing mortality in cardiac surgery with levosimendan: a meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 24, 51–57 (2010).
De Hert, S. G., Lorsomradee, S., Cromheecke, S. & Van der Linden, P. J. The effects of levosimendan in cardiac surgery patients with poor left ventricular function. Anesth Analg 104, 766–773 (2007).
Erb, J. et al. Influence of levosimendan on organ dysfunction in patients with severely reduced left ventricular function undergoing cardiac surgery. J Int Med Res 42, 750–764 (2014).
Levin, R., Degrange, M., Del, M. C., Tanus, E. & Porcile, R. Preoperative levosimendan decreases mortality and the development of low cardiac output in high-risk patients with severe left ventricular dysfunction undergoing coronary artery bypass grafting with cardiopulmonary bypass. Exp Clin Cardiol 17, 125–130 (2012).
Lim, J. Y. et al. Levosimendan Reduces Mortality in Adults with Left Ventricular Dysfunction Undergoing Cardiac Surgery: A Systematic Review and Meta-analysis. J Card Surg 30, 547–554 (2015).
Cholley, B. et al. Effect of Levosimendan on Low Cardiac Output Syndrome in Patients With Low Ejection Fraction Undergoing Coronary Artery Bypass Grafting With Cardiopulmonary Bypass: The LICORN Randomized Clinical Trial. JAMA 318, 548–556 (2017).
Landoni, G. et al. Levosimendan for Hemodynamic Support after Cardiac Surgery. N Engl J Med 376, 2021–2031 (2017).
Mehta, R. H. et al. Levosimendan in Patients with Left Ventricular Dysfunction Undergoing Cardiac Surgery. N Engl J Med 376, 2032–2042 (2017).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339, b2700 (2009).
Ioannidis, J. P. Contradicted and initially stronger effects in highly cited clinical research. JAMA 294, 218–228 (2005).
Trikalinos, T. A. et al. Effect sizes in cumulative meta-analyses of mental health randomized trials evolved over time. J Clin Epidemiol 57, 1124–1130 (2004).
Wetterslev, J., Thorlund, K., Brok, J. & Gluud, C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 61, 64–75 (2008).
Wetterslev, J., Thorlund, K., Brok, J. & Gluud, C. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res Methodol 9, 86 (2009).
Al-Shawaf, E. et al. Levosimendan or milrinone in the type 2 diabetic patient with low ejection fraction undergoing elective coronary artery surgery. J Cardiothorac Vasc Anesth 20, 353–357 (2006).
Anastasiadis, K. et al. Effectiveness of prophylactic levosimendan in patients with impaired left ventricular function undergoing coronary artery bypass grafting: a randomized pilot study. Interact Cardiovasc Thorac Surg 23, 740–747 (2016).
Baysal, A. et al. Levosimendan improves renal outcome in cardiac surgery: a randomized trial. J Cardiothorac Vasc Anesth 28, 586–594 (2014).
Eriksson, H. I. et al. Levosimendan facilitates weaning from cardiopulmonary bypass in patients undergoing coronary artery bypass grafting with impaired left ventricular function. Ann Thorac Surg 87, 448–454 (2009).
Kandasamy, A. et al. Comparison of Levosimendan versus Dobutamine in Patients with Moderate to Severe Left Ventricular Dysfunction Undergoing Off-pump Coronary Artery Bypass Grafting: A Randomized Prospective Study. Ann Card Anaesth 20, 200–206 (2017).
Leppikangas, H. et al. Preoperative levosimendan infusion in combined aortic valve and coronary bypass surgery. Br J Anaesth 106, 298–304 (2011).
Levin, R. L. et al. The calcium sensitizer levosimendan gives superior results to dobutamine in postoperative low cardiac output syndrome. Rev Esp Cardiol 61, 471–479 (2008).
Lomivorotov, V. V. et al. Levosimendan versus an intra-aortic balloon pump in high-risk cardiac patients. J Cardiothorac Vasc Anesth 26, 596–603 (2012).
Shah, B. et al. Study of levosimendan during off-pump coronary artery bypass grafting in patients with LV dysfunction: a double-blind randomized study. Indian J Pharmacol 46, 29–34 (2014).
Fedele, F. et al. Levosimendan improves renal function in acute decompensated heart failure: possible underlying mechanisms. Eur J Heart Fail 16, 281–288 (2014).
Landoni, G. et al. Effects of levosimendan on mortality and hospitalization. A meta-analysis of randomized controlled studies. Crit Care Med 40, 634–646 (2012).
Harrison, R. W. et al. Effect of levosimendan on survival and adverse events after cardiac surgery: a meta-analysis. J Cardiothorac Vasc Anesth 27, 1224–1232 (2013).
Packer, M. et al. Effect of levosimendan on the short-term clinical course of patients with acutely decompensated heart failure. JACC Heart Fail 1, 103–111 (2013).
Yakut, N. et al. The influence of levosimendan and iloprost on renal ischemia-reperfusion: an experimental study. Interact Cardiovasc Thorac Surg 7, 235–239 (2008).
Author information
Authors and Affiliations
Contributions
Xinqun Hu and Zhenhua Xing designed the study. Xiaofan Peng and Jiabing Huang provided methodological expertise in systematic reviews and searching strategies. Pengfei Chen and Jiabing Huang searched the databases and performed tables. Liang Tang drafted the manuscript. All authors read, provided critical feedback, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xing, Z., Tang, L., Chen, P. et al. Levosimendan in patients with left ventricular dysfunction undergoing cardiac surgery: a meta-analysis and trial sequential analysis of randomized trials. Sci Rep 8, 7775 (2018). https://doi.org/10.1038/s41598-018-26206-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-26206-w
- Springer Nature Limited