Abstract
Oral antiretroviral agents provide life-saving treatments for millions of people living with HIV, and can prevent new infections via pre-exposure prophylaxis1,2,3,4,5. However, some people living with HIV who are heavily treatment-experienced have limited or no treatment options, owing to multidrug resistance6. In addition, suboptimal adherence to oral daily regimens can negatively affect the outcome of treatment—which contributes to virologic failure, resistance generation and viral transmission—as well as of pre-exposure prophylaxis, leading to new infections1,2,4,7,8,9. Long-acting agents from new antiretroviral classes can provide much-needed treatment options for people living with HIV who are heavily treatment-experienced, and additionally can improve adherence10. Here we describe GS-6207, a small molecule that disrupts the functions of HIV capsid protein and is amenable to long-acting therapy owing to its high potency, low in vivo systemic clearance and slow release kinetics from the subcutaneous injection site. Drawing on X-ray crystallographic information, we designed GS-6207 to bind tightly at a conserved interface between capsid protein monomers, where it interferes with capsid-protein-mediated interactions between proteins that are essential for multiple phases of the viral replication cycle. GS-6207 exhibits antiviral activity at picomolar concentrations against all subtypes of HIV-1 that we tested, and shows high synergy and no cross-resistance with approved antiretroviral drugs. In phase-1 clinical studies, monotherapy with a single subcutaneous dose of GS-6207 (450 mg) resulted in a mean log10-transformed reduction of plasma viral load of 2.2 after 9 days, and showed sustained plasma exposure at antivirally active concentrations for more than 6 months. These results provide clinical validation for therapies that target the functions of HIV capsid protein, and demonstrate the potential of GS-6207 as a long-acting agent to treat or prevent infection with HIV.
Similar content being viewed by others
Main
HIV-1 capsid protein (p24; hereafter abbreviated CA) has essential roles throughout the viral replication cycle, making it an attractive target for therapeutic intervention11,12. Unlike the viral enzymes (protease, reverse transcriptase and integrase) that are currently targeted by small-molecule antiretroviral drugs, CA functions through interactions between proteins; targets that function in this way have historically posed considerable challenges for interventions using small-molecule drugs13. CA is initially expressed within the Gag and Gag–Pol polyproteins, and provides key interactions between proteins that are necessary for assembly of the virion14. In the virion, CA is released by precursor cleavage mediated by HIV-1 protease, and self-assembles into a conical capsid composed of about 250 CA hexamers and 12 pentamers15. The correct formation and integrity of the capsid are essential for virus infectivity14. Upon infection of a new cell, controlled intracellular transport and disassembly of the viral capsid is regulated, in part, by interactions with host factors, and supports reverse transcription and proviral DNA integration16,17,18.
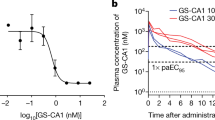
We assayed small molecules for effects on the kinetics of in vitro CA assembly, and identified multiple inhibitor and accelerator series. Potency improvements through chemical modification were limited for compounds that inhibited CA assembly, presumably because these compounds could not overcome mass action and excess of the CA subunit in the virion (about 4 mM)19,20. Compounds that worked in concert with mass action to increase the rate and extent of CA assembly proved more amenable to improvement of their antiviral activity. Ultimately, extensive potency and pharmacokinetic optimization was required to discover a clinical candidate directed against HIV CA. The activity of GS-CA1 has previously been reported21. Here we report on GS-6207 (Fig. 1a), a CA-targeting inhibitor of HIV replication that is even more potent and more metabolically stable than GS-CA1 and that is suitable for clinical trials22. GS-6207 showed a dose-dependent increase in the rate and extent of in vitro CA assembly (Fig. 1b). In a cellular context, this acceleration of CA assembly produced malformed capsids that are morphologically distinct from mature and immature particles (Fig. 1c, d). Importantly, GS-6207 showed a mean half-maximum effective concentration (EC50) of 105 pM in MT-4 cells infected with HIV-1, which makes this inhibitor significantly more potent than all of the approved HIV antiretroviral drugs that we tested (Fig. 1e). GS-6207 showed picomolar mean EC50 values in primary human CD4+ T cells (32 pM) and macrophages (56 pM) infected with HIV-1, and remained broadly active against 2 HIV-2 isolates (885 pM) and 23 clinical HIV-1 isolates (50 pM, range of 20 to 160 pM) in human peripheral blood mononuclear cells (Fig. 1f). GS-6207 exhibited minimal cytotoxicity in human cell lines and primary cells, showing a mean half-maximal cytotoxic concentration (CC50) in peripheral blood mononuclear cells of >50 μM and a therapeutic index (CC50/EC50) of more than 1,000,000 (Extended Data Table 1). When combined with other antiretroviral agents, GS-6207 displayed synergy (Extended Data Table 2) and retained full activity against HIV-1 variants that are resistant to current drug classes (Extended Data Table 3), which demonstrates its potency in combination and against drug-resistant strains of HIV.
a, GS-6207. b, Light scattering (absorbance at 350 nm) responses showing the rate and extent of in vitro CA (20 μM) assembly in 2 M NaCl, in the presence and absence of GS-6207. Data are representative of four independent experiments (n = 2 biological replicates each). c, Representative thin-section electron micrograph images of HIV-1 produced in the presence of 0.2% dimethyl sulfoxide (DMSO) (left), GS-6207 (15 nM) (middle) or the HIV-1 protease inhibitor atazanavir (500 nM) (right). Scale bars, 50 nm. d, Quantification for c. Data are mean ± s.d. from representative images of HIV-1 produced in one of two independent experiments. DMSO, n = 737 virions; GS-6207, n = 591 virions; atazanavir (ATV), n = 618 virions. P values in all figures are by unpaired two-tailed Student’s t-test with Welch’s correction. ****P < 0.0001. e, Inhibition of HIV-1 strain IIIB in MT-4 cells. Data are mean ± s.d. from 4 biological replicates in each of 8 to 115 independent experiments. GS-6207 (n = 8), rilpivirine (RPV) (n = 113), efavirenz (EFV) (n = 113), dolutegravir (DTG) (n = 115), bictegravir (BIC) (n = 20), ATV (n = 113), darunavir (DRV) (n = 60) and tenofovir alafenamide (TAF) (n = 15). ****P < 1 × 10−15. f, Inhibition of HIV-2 and HIV-1 group M (subtypes A–G, circulating recombinant forms (CRFs)), N and O clinical isolates. Data represent individual isolates (n = 3 biological replicates each). g, X-ray crystal structure of GS-6207–CA hexamer complex. Top and side views of CA hexamer (individual CA monomers coloured alternately in cyan and grey). The GS-6207 binding site, located between the NTD of one CA monomer and the CTD of an adjacent monomer, is boxed. h, Space-filling view of GS-6207 in its binding site (X-ray structure). i, Hydrogen bonds (dashed black lines, n = 7) and cation–π interactions (dashed yellow lines, n = 2) are shown between GS-6207 and CA residues.
The molecular underpinnings of the role of GS-6207 as an accelerator of CA monomer assembly are apparent in a 2.0 Å resolution X-ray crystal structure of GS-6207 in complex with a cross-linked CA hexamer (Fig. 1g–i, Extended Data Table 4). In this structure, GS-6207 binding is located between the N-terminal domain of one subunit of the CA hexamer (CANTD) and the C-terminal domain (CACTD) of an adjacent subunit in the hexamer. GS-6207 exhibits notable shape complementarity with adjacent CA monomers (contacting more than 2,000 Å2 of buried protein surface area), and displays extensive hydrophobic and electrostatic interactions that include two cation–π interactions and seven hydrogen bonds. The GS-6207 sulfonamide is the linchpin in a hydrogen-bonding network that bridges from CANTD residues N74 and K70 of one subunit to CACTD residue N183 of the neighbouring subunit, and orders a loop that is unstructured in the apo hexamer crystal (Fig. 1i). Consistent with its binding position between neighbouring CA monomers in this crystal structure, GS-6207 showed saturable dose-dependent binding to Gag and CA; the slow dissociation of GS-6207 from CA multimers is consistent with a tenfold-higher affinity relative to the CA monomer (Extended Data Table 5).
To define the functional consequences of GS-6207 binding to capsid, we measured the potency of GS-6207 during early and late stages of the viral replication cycle in target MT-2 and producer HEK293T cells, respectively. GS-6207 showed sub-nanomolar potency in target cells (EC50 = 23 pM), in a full-cycle assay (EC50 = 25 pM) and in producer cells (EC50 = 439 pM), which indicates that GS-6207 interferes with both the early and late stages of HIV-1 replication but exhibits greater potency against the early stage (Fig. 2a). Time-of-addition studies relative to a non-nucleoside reverse-transcriptase inhibitor and an integrase strand-transfer inhibitor indicated that GS-6207 targets one or more steps that occur after reverse transcription and before integration (Fig. 2b). In quantitative PCR assays, we measured the accumulation of the products of reverse transcription, the formation of two-long-terminal-repeat (2-LTR) circles (which indicate nuclear localization but aborted integration) and proviral integration (Fig. 2c). GS-6207 at 1.25 nM (12.5-fold EC50) did not alter the synthesis of HIV complementary DNA (cDNA) but significantly reduced formation of 2-LTR circles and integrated proviruses. These data suggest that GS-6207 might prevent the nuclear import of viral cDNA—possibly via direct competition with host-cell nuclear import cofactors (such as nucleoporin 153 (NUP153) and cleavage and polyadenylation specificity factor 6 (CPSF6)23,24,25,26) that bind CA and share a CA binding site with GS-6207 (Fig. 2d). In addition to these early effects and the effects on capsid formation, GS-6207 inhibited the production of HIV-1 that contains mature wild-type CA but not the CA(M66I) binding-site mutant that reduces GS-6207 binding affinity to CA oligomers (Extended Data Table 5), as measured by a p24 enzyme-linked immunosorbent assay (Fig. 2e). GS-6207 did not inhibit HIV-1 protease cleavage activity in vitro (half-maximal inhibitory concentration of more than 50 μM) but reduced intracellular Gag and processed CA levels in the producer cells (Fig. 2f), which indicates that the loss of p24 production probably reflected GS-6207 binding to CA precursors, and a reduction in Gag and/or Gag–Pol stability, trafficking and/or viral assembly.
a, Antiviral activity of GS-6207 throughout a full replication cycle, or when selectively present during target-cell infection (early events) or virus production (late events). Data are mean ± s.d. from 4 independent experiments (n = 3 biological replicates each). b, Time-of-addition study indicating when GS-6207 inhibits HIV-1 replication relative to rilpivirine (reverse transcriptase inhibitor) and bictegravir (integrase inhibitor). Data are mean from one of two representative independent experiments (n = 8 biological replicates per group in each experiment). h.p.i., hours post-infection. c, Effect of GS-6207 (1.25 nM) on the intracellular abundance of various forms of HIV-1 DNA. Data are mean ± s.d. from one of two representative independent experiments (n = 3 biological replicates each). d, Overlay of GS-6207 with CA-binding peptides from nuclear-import factors CPSF6 and NUP153 (ref. 25) in their shared binding pocket. e, Effect of GS-6207 on HEK293T producer-cell viability, HIV-1 particle production and infectivity. Data are mean from one of three representative independent experiments (n = 3 biological replicates each). M66I, GS-6207 resistance-associated CA-binding-site variant; WT, wild type. f, Effect of GS-6207 on intracellular p24 levels. Data are mean ± s.d. from 3 independent experiments (n = 3 biological replicates each). For gel source data, see Supplementary Fig. 1.
To evaluate drug resistance, we serially passaged HIV-1 in MT-2 cells in the presence of increasing concentrations of GS-6207 for more than three months (Fig. 3a). Sequence analysis identified an N74D substitution in CA (passages 4–6) followed by a CA(Q67H/N74D) variant (passages 7–10). The N74D substitution has previously been shown to alter the viral pathway of nuclear entry27. Viruses with these GS-6207 resistance-associated mutations remained fully sensitive to agents from other antiretroviral classes (Fig. 3b). Selections performed in the presence of fixed concentrations of GS-6207 in human peripheral blood mononuclear cells independently infected with six HIV-1 isolates similarly identified Q67H and N74D as the major resistance-associated mutations, with additional variants (L56I, M66I, K70N, Q67H/N74S and Q67H/T107N) that were each independently detected in a single GS-6207-selected culture (Fig. 3c). These resistance-associated mutations, alone or in combination, conferred reduced susceptibility to GS-6207 (6- to >3,200-fold resistance relative to the wild-type virus), consistent with the assignment of CA as the functional target of GS-6207. All CA residues that confer resistance map to the GS-6207 binding site and are highly conserved across subtypes of HIV-121,28,29,30. Of the mutants that we tested, all but the low-level-resistant Q67H variant (sixfold resistance to GS-6207 relative to wild-type virus) display reduced replication capacity in vitro (Extended Data Table 6).
a, Emergent CA substitutions denoted during resistance selection in MT-2 cells infected with HIV-1 strain HXB2D, by escalation of the GS-6207 dose. Data are representative of one of two biological replicates from a single selection experiment. b, Fold resistance of GS-6207-selected viral isolate passage (P)3 to 10 (each tick mark corresponds to one passage) to GS-6207, and control antiretroviral agents. Data are mean ± s.d. from 3 independent experiments (n = 3 biological replicates each). Red dotted line defines the cut-off for drug resistance. c, Frequency of GS-6207-selected CA variants observed at fixed GS-6207 concentrations in peripheral blood mononuclear cells infected with clinical HIV-1 isolates.
Low hepatic clearance is an essential attribute for a long-acting agent. Thus, along with enhancement of potency, the design process that culminated in GS-6207 also focused on blocking metabolically labile sites through incorporation of electron-withdrawing groups (halogens and sulfonyls), metabolically stable ring systems (cyclopropane and pyrazoles) and rigidifying elements. Tritiation ([3H]) of GS-6207 was necessary to accurately measure the low turnover of GS-6207 in primary human hepatocytes, and showed a predicted rate of hepatic clearance of 0.01 l h−1 kg−1, or 0.8% of the hepatic extraction.
In a single-ascending-dose clinical study that was randomized, double-blind and placebo-controlled, we administered a suspension formulation of 30 to 450 mg GS-6207 to healthy participants (32 active and 8 placebo)—most of whom were male (27 of 40) and in their 30s (median age of 37 years old, range 19 to 44 years old), and had normal kidney and liver function—as a subcutaneous injection (Fig. 4a). Consistent with nonclinical safety studies, GS-6207 was generally safe and well-tolerated. The most frequent adverse events were mild erythema and/or pain at the injection site that resolved in a few days (Extended Data Table 7). GS-6207 pharmacokinetic profiles showed slow, sustained drug release, with a median apparent terminal half-life (t1/2) of about 38 days. Increases in exposure to GS-6207 were approximately dose-proportional. At doses of ≥100 mg, GS-6207 plasma concentrations exceeded the human serum protein-adjusted 95% effective concentration (EC95) for wild-type HIV-1 (4.0 nM or 3.87 ng ml−1 in MT-4 cells) for ≥12 weeks, and doses of ≥300 mg exceeded the human protein-adjusted EC95 for more than 24 weeks.
a, Mean plasma concentration–time profile of GS-6207 after a single subcutaneous administration of 30–450 mg of drug to uninfected individuals (n = 8 within each dosing arm). b, Mean plasma concentration–time profile of GS-6207 after a single subcutaneous administration of 20–450 mg to individuals infected with HIV (n = 6 within each dosing arm). Red dotted line defines protein-adjusted EC95 for GS-6207. c, Mean log10-transformed change in plasma HIV-1 RNA after a single subcutaneous administration of 20–450 mg GS-6207 to 8 individuals with untreated HIV-1 infection randomized to drug (n = 6) or placebo (n = 2) within each dosing arm.
In a subsequent clinical study (which was also randomized, double-blind and placebo-controlled), 20 to 450 mg GS-6207 was administered to trial participants with untreated HIV-1 infection (24 active and 8 placebo) as a single-dose subcutaneous suspension. We conducted a prespecified interim analysis of this part of the study. Most of the participants were male (30 of 32), in their 30s (median age of 34 years old, range 19 to 59 years old) and treatment-naive (25 of 32), and had median HIV-1 RNA loads of log10-transformed copies per millilitre of 4.48 (range of 3.86 to 5.01) and median CD4+ T cell counts of 458 cells per microlitre (range of 200 to 1,009). GS-6207 was generally safe and well-tolerated (Extended Data Table 8), and the concentration–time profiles of GS-6207 were consistent with those in HIV-negative participants through to nine days after administration of the dose (Fig. 4b, Extended Data Table 9). A single subcutaneous administration of 20, 50, 150 or 450 mg GS-6207 led to mean maximum log10-transformed reductions of 1.35, 1.79, 1.76 and 2.20, respectively, in plasma HIV-1 RNA by the ninth day (Fig. 4c, Extended Data Table 10). A genetic mixture of wild-type CA and the CA(Q67H) mutant emerged on day 9 in one participant in the 20-mg cohort, which was associated with a 1.6-fold decrease in phenotypic susceptibility but not with viral escape by day 9 of monotherapy.
These data establish GS-6207 as a first-in-class HIV-1 capsid inhibitor with potent antiviral activity against both wild-type virus and variants that are resistant to current antiretroviral agents. The favourable safety profile, prolonged pharmacokinetic exposure and observed antiviral efficacy in humans support continued clinical development of GS-6207 as a long-acting antiretroviral agent for the treatment of infection with HIV-1, including for people living with HIV who are heavily treatment-experienced and have multidrug-resistant virus. In addition, the infrequent subcutaneous dosing renders GS-6207 an attractive candidate for the simplified prevention of the acquisition of HIV in at-risk populations—making this drug a potentially transformative tool in efforts to end the global HIV epidemic.
Methods
No statistical methods were used to predetermine sample size. The in vitro experiments were not randomized and investigators were not blinded to sample allocation during in vitro experiments and outcome assessment.
Compounds
GS-6207 was synthesized at Gilead Sciences, and chemical identity (1H-nuclear magnetic resonance (NMR), 13C-NMR and high-resolution mass-spectrometry spectra) and sample purity were established using reverse-phase high-performance liquid chromatography (HPLC) (Supplementary Information). The control antiretroviral agents emtricitabine (FTC), tenofovir alafenamide (TAF), elvitegravir (EVG), raltegravir (RAL), bictegravir (BIC), darunavir (DRV), atazanavir (ATV) and bevirimat (BVM) were synthesized at Gilead Sciences, and efavirenz (EFV) and dolutegravir (DTG) were purchased from Toronto Research Chemicals and Porton Shanghai R&D Center, respectively. Puromycin (a control compound for cytotoxicity assays) was purchased from Sigma-Aldrich.
Viruses
The HIV-1 strains IIIB and BaL were obtained from the NIH AIDS Reagent Program and from Advanced Biotechnologies, respectively. Two HIV-2 isolates (CBL20 and CDC310319) and 23 clinical HIV-1 isolates from the Southern Research virus collection were selected for susceptibility profiling: subtype A (92UG031 and 92UG037), subtype B (89BZ_167, 90US_873, YU-2, 91US001, 91US004, 96TH_NP1538, BaL and JR-CSF), subtype C (92BR025 and 98US_MSC5016), subtype D (92UG001 and 98UG_57128), subtype E (CMU02 and CMU08), subtype F (93BR020), subtype G (JV1083), group N (YBF30), group O (BCF01), CRF01_AE (90TH_CM235) and CRF02_AG (01CM0008BBY, 91DJ263). HIV-1 recombinant strains encoding mutation(s) that confer resistance to nucleoside reverse transcriptase inhibitors, non-nucleoside reverse transcriptase inhibitors, integrase strand transfer inhibitors, protease inhibitors or maturation inhibitors have previously been described31,32. Single-cycle HIV-1 encoding firefly luciferase with and without mutations within the capsid gene was made by co-transfecting HEK293T cells with pKS13ΔEnv and pHCMV-G plasmids. Cell-free viral supernatant was collected 3 days after transfection, clarified using a 0.45-μm syringe filter and stored at −80 °C. The amount of HIV in each sample was quantified by p24 antigen enzyme-linked immunosorbent assay (Perkin Elmer) and a reverse transcriptase activity assay (Southern Research).
Cell lines
Human MT-2 and MT-4 T-cell lines were obtained from the NIH AIDS Reagent Program and maintained in RPMI-1640 medium supplemented with 10% heat-inactivated fetal bovine serum (FBS), 100 units ml−1 penicillin, and 10 μg ml-1 streptomycin (complete RPMI). MT-2 cells chronically infected with HIV-1 strain IIIB were cultured in complete RPMI. HEK293T cells were obtained from the Gladstone Institute for Virology and Immunology and maintained in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% FBS, 100 units ml−1 penicillin, and 10 μg ml−1 streptomycin (complete DMEM). The human hepatoma Huh-7 cell line was obtained from ReBLikon and cultured in complete DMEM33. The human hepatoblastoma cell line HepG2, human prostate carcinoma cell line PC-3 and normal human fetal-lung-derived MRC-5 cells were obtained from the American Type Culture Collection. PC-3 and HepG2 cells were adapted to grow in 0.2% galactose-containing, glucose-free DMEM supplemented with 10% FBS, 1% non-essential amino acids, 1% pyruvate, and 1% GlutaMAX. MRC-5 cells were maintained in Eagle’s Minimum Essential Medium (MEM) supplemented with 10% FBS. Each cell culture medium was further supplemented with 100 units ml−1 penicillin and 100 μg ml−1 streptomycin. The above eukaryotic cell lines were not authenticated and were judged to be free of mycoplasma contamination using the MycoProbe Mycoplasma Detection Kit (R&D Systems).
Primary cells
Human peripheral blood mononuclear cells (PBMCs) were collected from healthy volunteers under informed consent; their use was approved by an institutional review board at AllCells. The preparation of human PBMCs, CD4+ T lymphocytes and monocyte-derived macrophage cultures have previously been described31. Before infection, PBMCs and CD4+ T cells were activated for 48 h at 37 °C by addition of 1 μg ml−1 phytohaemagglutinin (PHA) and 50 international units ml−1 recombinant human interleukin 2 (IL-2). Primary human hepatocytes from three independent donors were purchased from Invitrogen and cultured in William’s Medium E medium containing cell maintenance supplement. Donor profiles were limited to 4–65 years of age, non-smokers with limited alcohol consumption. Upon arrival at Gilead Sciences, hepatocytes were allowed to recover in a 37-°C incubator with 5% CO2 and 90% humidity for 12–18 h in complete medium with vendor-supplied supplements before treatment with compounds.
Antiviral assays
The five-day cytoprotection antiviral assays using MT-2 and MT-4 T-cell lines have previously been described31. Data analysis was performed using GraphPad Prism 7.0 to calculate EC50 values. The EC95 value for GS-6207 was calculated from the EC50 and Hill coefficient, n, determined in MT-4 cells using the equation: EC95 = EC50 × (95/5)1/n.
For time-of-addition antiviral assays, MT-2 cells were infected with single-cycle reporter HIV-1 for 1 h at 37 °C, washed and seeded into 96-well plates (75-μl aliquots; 1.5 × 104 cells per well). A 25-μl aliquot of complete RPMI medium was added to 8 uninfected and 8 infected wells as respective minimum (0%) and maximal (100%) infection controls. Twenty-five-microlitre aliquots of 4× drug–medium were added to 8 replicate wells at indicated times after infection. GS-6207 and control antiretroviral agents were tested at concentrations equivalent to 10× and 100× EC50, producing similar results. Assay plates were kept in a humidified 37-°C incubator before and after drug–medium additions. Plates were developed 48 h.p.i. using ONE-Glo Luciferase Assay reagent (Promega) and the resulting luminescence data were collected and analysed using EnVision Manager 1.13.3009 and GraphPad Prism 7.0 software, respectively. When investigating inhibitor potency across the phases of viral replication, single-cycle antiviral assays were performed in MT-2 cells in a manner such that GS-6207 was present selectively at early stage, late stage or during a full course of infection as previously described34. Assays evaluating the effect of GS-6207 on HIV-1 particle production (by p24 antigen enzyme-linked immunosorbent assay) and intracellular CA levels (by anti-p24 and anti-tubulin western blot analyses) have previously been described21.
For in vitro two-drug combination studies, compounds within a test pair were combined in 384-well assay plates to create a two-dimensional matrix of diluted drugs. Positive control (EVG) and negative control (DMSO) wells were included in every assay plate to define 100% and 0% protection from viral replication-mediated cytopathic effect (CPE), respectively. The final DMSO concentration in the assay was 0.5%. MT-2 cells were bulk-infected in complete RPMI medium with HIV-1 strain IIIB at a multiplicity-of-infection (MOI) of 0.01 for 3 h at 37 °C, added to the assay plates (3 × 103 cells per well) and incubated at 37 °C for 5 days. Cell viability was determined by adding CellTiter-Glo reagent and the resulting luminescence data were collected using EnVision Manager 1.13.3009. Data were normalized to positive and negative controls in each plate, expressed as per cent CPE protection and analysed with MacSynergy II software35. Combination data were analysed at the 95% confidence level, with synergy and antagonism volumes defined as follows: high synergy (>100 μM2%), moderate synergy (50 to <100 μM2%), additivity (>-50 to <50 μM2%) and antagonism (<-50 μM2%).
Antiviral assays using HIV-1 strain BaL in primary human CD4+ T lymphocytes and macrophage cultures were conducted using a p24 endpoint assay as previously described36. A seven-day reverse transcriptase endpoint antiviral assay using fresh human PBMCs independently infected with a panel of clinical HIV-1 and HIV-2 isolates was performed by Southern Research as a contracted research study.
Cytotoxicity assays
For cytotoxicity assessment in MT-4 cells, PBMCs, primary human CD4+ T cells and monocyte-derived macrophages, the protocol was identical to that of the respective antiviral assay, including assay duration, except that no virus was added to the plates. Protocols for cytotoxicity assessments in Huh-7, Gal-HepG2, Gal-PC-3 and MRC-5 cell lines, as well as in primary human hepatocytes, have previously been described37. The effect of test compounds on cell viability was measured using CellTiter-Glo. Data analysis was performed using GraphPad Prism 7.0 to calculate CC50 values.
GS-6207 resistance analysis
Dose-escalation selections for drug-resistant HIV-1 variants were performed in MT-2 cells infected with HIV-1 strain HXB2D using twofold incremental increases in GS-6207 concentration as previously described31. The resistance profile of each emergent virus passage was then assessed in the five-day cytoprotection antiviral MT-2 assay after titrating virus inoculums to normalize the MOI across all samples. Viral breakthrough selections were conducted under conditions of fixed, constant drug concentrations over a period of 35 days in human PBMCs independently infected with 6 different HIV-1 isolates (BaL, 92US657, 91US0006, 7406, 7467 and 7576) as previously described21. GS-6207 was tested at fixed drug concentrations equal to 4-fold, 8-fold and 16-fold its EC95 value of 0.23 nM (0.92 nM, 1.9 nM, and 3.7 nM GS-6207, respectively), using 6 replicate cell cultures per experimental condition. Viruses that emerged in the presence of GS-6207 were genotyped by population sequencing. Total RNA was isolated from mock- and GS-6207-selected virus-containing supernatants using the QiaAMP Viral RNA Mini Kit (Qiagen). A 986-bp fragment encoding HIV-1 capsid and the adjacent p2 spacer peptide was amplified by PCR with reverse transcription (RT–PCR) using the Qiagen OneStep RT–PCR Kit in combination with primers 5′-CAGTAGCAACCCTCTATTGTGTGC-3′ and 5′-CCTAGGGGCCCTGCAATTT-3′. RT–PCR products were sequenced by Elim Biopharmaceuticals. To identify codon changes, gene sequences from selected HIV-1 variants were aligned using DNA Sequencher 4.9 Software (Gene Codes) with that of the input virus and virus passaged in the absence of GS-6207. For samples containing >1 codon change, PCR products were subcloned, DNA was isolated from individual bacterial colonies and the gene encoding CA was sequenced to assess the linkage of all observed substitutions.
The resistance profile and infectivity of each GS-6207-selected CA variant was determined in MT-2 cells after introducing each substitution, alone and in combination, into wild-type single-cycle reporter HIV-1. The replication level (fitness) of select CA variants introduced into wild-type replication-competent reporter HIV-1 was evaluated in primary human CD4+ T cells over a period of 19 days21.
Recombinant HIV-1 Gag and CAs
Recombinant HIV-1LAI CA was prepared as previously described38. Soluble cross-linked CA hexamers of HIV-1 strain NL4.3 (wild type and the M66I variant), as well as CA pentamers, were prepared as previously described38,39,40. Recombinant Gag protein of HIV-1 strain NL4.3 was prepared as previously described21.
Crystallization, data collection and structure determination
HIV-1 CA hexamer (25 mg ml−1 in 20 mM Tris, pH 8.0) was thawed and diluted to 12 mg ml−1 in the same buffer and incubated on ice for 10 min with 1 mM GS-6207. Crystallization droplets were assembled in MRC2 microplates with 100 nl of the complex and 100 nl of 12% polyethylene glycol (PEG) 3350, 0.2 M sodium thiocyanate, 0.1 M sodium cacodylate, pH 6.7. The assembled 200-nl droplet was then subjected to vapour diffusion with 50 μl of 1% PEG 3350, 0.2 M sodium thiocyanate, 0.1 M sodium cacodylate, pH 6.7 in the large reservoir. Large hexagonal crystals (30 μm × 160 μm × 160 μm) grew in 4 d at 25 °C and were subsequently cryo-protected for X-ray diffraction in 30% PEG 3350, 7% glycerol, 0.2 M sodium thiocyanate, 0.1 M sodium cacodylate, pH 6.7, and 0.3 mM GS-6207. X-ray diffraction data to 2.0 Å resolution were collected on a single frozen (−180 °C) crystal at the Advanced Light Source, Beamline 5.0.1. The protein–inhibitor complex crystallized in space group P3 with cell parameters: a = 158.3 Å, b = 158.3 Å, c = 55.6 Å, α = 90.0°, β = 90.0° and γ = 120.0°. The data were processed and scaled with the programs DENZO and SCALEPACK (HKL Research), respectively. Initial models were obtained by molecular replacement using the program EPMR41 and using the coordinates from a single monomer of a previously determined HIV-1 CA hexamer–inhibitor complex (with coordinates for the inhibitor atoms removed) as the search model. The molecular replacement solution included six monomers. The initial model was further refined using multiple rounds of simulated annealing in the PHENIX software package42 followed by manual refitting of the model in COOT43. In the later stages of refinement, strong residual electron density in the capsid modulator binding site allowed for unambiguous placement of GS-6207 into the structure followed by final refinement of the model (see Supplementary Fig. 2 for sample inhibitor density). Data collection and model refinement statistics are summarized in Extended Data Table 4.
In vitro HIV-1 CA assembly assay
The in vitro assembly of HIV-1 CA in the presence and absence of small-molecule library compounds (10 μM) or twofold serially diluted GS-6207 was monitored by measuring changes in sample absorbance over time at 350 nm. Final assembly reactions contained 20 μM CA, 2 M NaCl, 50 mM sodium phosphate pH 7.5, 0.005% Antifoam 204 (Sigma-Aldrich) and 1% DMSO. Sample absorbance values at 350 nm were monitored over time at 25 °C in 96-well or 384-well plates using an M5 plate reader (Molecular Devices), corrected for absorbance values in the absence of CA or NaCl, and the data analysed using SoftMax Pro 6.3.1 as previously described38.
GS-6207 binding assay
Surface plasmon resonance biosensor binding experiments were performed using the ProteOn XPR36 platform (CA hexamer and pentamer proteins) or the Biacore T100 platform (CA monomer and Gag proteins) as previously described21. Data were analysed using ProteOn Manager 3.1.0 or Scrubber 2.0 and fit with a simple kinetic model with a term for mass transport added when necessary.
Quantification of HIV-1 DNA
MT-2 cells (2 × 106 cells ml−1) were infected with single-cycle reporter HIV-1, added to 24-well plates containing drug medium and transferred to a humidified 37-°C incubator. For each condition, cells from each of 3 replicate wells were collected at 12 h.p.i. for late reverse transcription product quantification, 24 h.p.i. for 2-LTR circle quantification, and 48 h.p.i. for Alu-LTR product quantification. Viral DNA was isolated from cell pellets using a QIAamp DNA mini kit (Qiagen) and quantified using the TaqMan real-time PCR and ABI Prism 7900HT sequence detection system (Applied Biosystems) or the QX200 Droplet Digital PCR System (Bio-Rad) as previously described21.
Ultrastructural analysis of HIV-1 by electron microscopy
MT-2 cells infected with HIV-1 strain IIIB were washed and cultured at 37 °C in complete RPMI containing 0.25% DMSO, 15 nM GS-6207 or 500 nM ATV. After a four-day incubation, samples were pelleted, fixed, stained, sectioned and imaged on a JEOL JEM-1230 transmission electron microscope as previously described21.
Metabolic stability of [3H]GS-6207 in primary human hepatocytes
A 500-μl suspension of human hepatocytes (1 × 106 cells ml−1) and 0.25 μM [3H]GS-6207 was prepared in Krebs–Henseleit Buffer (KHB) medium and incubated in a humidified 37-°C incubator with 5% CO2 in duplicate wells of a 24-well plate. Propranolol (1 μM final), a compound known to be efficiently metabolized by hepatocytes by oxidation and conjugation, was used as a positive control. A cell-free control was incubated in parallel as a negative control. Aliquots (100 μl) were removed after 0, 1, 3 and 6 h, mixed with 200 μl quenching solution, placed on a shaker for 10 min and then centrifuged at 3,000g for 60 min. The supernatant was transferred to a new plate, diluted with 100 μl water and placed on a shaker for 10 min. The quantification of [3H]GS-6207 and its metabolites was performed by radio flow chromatography using a Perkin Elmer Radiomatic 625TR flow scintillation analyser with a 500 μl flow cell coupled to a Dionex Ultimate 3000 HPLC system. The scintillation cocktail was Perkin Elmer Ultima-Flo and was mixed with the HPLC effluent at a ratio of 1:1. The sample (100 μl) was injected with a Leap Technologies CTC PAL autosampler. Separation was achieved on a Phenomenex Synergi Fusion-RP 80 Å pore size, 4-μm particle size, 150 × 4.6-mm column maintained at 32 °C. Mobile phase A consisted of 95% water, 5% acetonitrile, and contained 0.1% trifluoroacetic acid (TFA). Mobile phase B consisted of 95% acetonitrile, 5% water, and contained 0.1% TFA. Elution was achieved, at a flow rate of 1 ml min−1, by linear gradients: initial condition was 2% B at 0 min which was increased to 75% B over 45 min, holding for 4 min at 75% B and then returning to initial conditions. The column was allowed to re-equilibrate for 12 min between injections. Quantification was by radiochromatographic peak area.
Competitive equilibrium dialysis
Human serum protein binding to GS-6207 was determined by competitive equilibrium dialysis. Human plasma (10%) was spiked with GS-6207 (2 μM) and blank RPMI cell culture medium containing 2% FBS were placed in duplicate into opposite sides of assembled dialysis cells. After a 24-h equilibration period at 37 °C, GS-6207 concentrations in plasma and cell culture medium were determined by a liquid chromatography with tandem mass spectrometry (LC–MS/MS) method and multiplied by 10 to obtain the protein-adjusted shift for 100% human plasma.
Ethical conduct and consent in clinical trials
The clinical trials were conducted in accordance with Good Clinical Practice, as defined by the International Conference on Harmonization and in accordance with the ethical principles underlying the United States Code of Federal Regulations, Title 21, Part 50 (21CFR50). The protocol and the participant informed-consent form received institutional review board, independent ethics committee approval and/or favourable opinion (Advarra) before initiation of the study. Freely given written informed consent was obtained from every individual before participation in the clinical studies.
Single ascending-dose study in healthy participants
For clinical study GS-US-200-4070, we enrolled healthy men and women uninfected with HIV-1, 18–45 years of age, with normal kidney and liver function, body mass index between 19 and 30 kg/m2, and no relevant medical history. Ten trial participants in each dosing arm were randomized in a blinded fashion in a 4:1 ratio to receive either the drug (GS-6207) or placebo (vehicle alone). The primary objectives were to assess the safety and tolerability of escalating single subcutaneous doses of GS-6207 compared with placebo in healthy participants and to assess its pharmacokinetics. GS-6207 was formulated as a sterile, preservative-free, injectable aqueous suspension (100 mg m1−1). Serial blood samples were collected for plasma pharmacokinetics analysis through day 197 (30- and 100-mg cohorts) or day 225 (300- and 450-mg cohorts). Plasma samples were analysed using a validated, high-performance LC–MS/MS bioanalytical method with multiple reaction monitoring and electrospray ionization in the positive mode (Covance Laboratories). Quantification was performed using multiple reaction monitoring of the transitions m/z 968.2 to 869.2 and m/z 974.3 to 875.2 for GS-6207 and an isotopically labelled internal standard, respectively. The bioanalytical method was validated over a calibrated range of 0.5 to 500 ng ml−1. Inter-assay precision, based on coefficient of variation, was ≤ 8.7%, and accuracy ranged from 95.2% to 104.6%. All plasma samples were analysed within the timeframe supported by frozen stability storage data. Pharmacokinetic parameters were estimated using Phoenix WinNonlin 6.4 (Certara, L.P.) software using standard noncompartmental methods. Pharmacokinetics parameters for GS-6207 included area under plasma concentration versus time curve extrapolated to infinity (AUCinf), the per cent of the area that is extrapolated (AUC%exp), and area under the concentration versus time curve from time zero to the last quantifiable concentration (AUClast), maximal concentration (Cmax), time to Cmax (tmax) and t1/2.
Single ascending-dose study in participants living with HIV
For clinical study GS-US-200-4072 (registered with ClinicalTrials.gov, NCT03739866), we enrolled treatment-naive or -experienced, but HIV-capsid-inhibitor-naive and integrase-strand-transfer-inhibitor-naive, men and women, 18–65 years of age with plasma HIV-1 RNA ≥ 5,000 copies ml−1 (via amendment; originally 10,000 copies ml−1) but ≤ 400,000 copies ml−1 and CD4+ T cell counts >200 cells per mm3. Eight trial participants in each dosing arm were randomized in a 3:1 ratio to receive either the drug (GS-6207) or placebo (vehicle alone) (part A). GS-6207 was formulated as a sterile, preservative-free, injectable aqueous suspension (100 mg m1−1).
Plasma HIV-1 RNA levels were determined using the Roche COBAS Ampliprep/COBAS TaqMan HIV-1 test v.2, which has a limit of detection of 20 copies ml−1 and a range of quantification of 20 to 10,000,000 HIV-1 RNA copies ml−1. All samples were analysed by a central laboratory. Serial blood samples were collected for plasma pharmacokinetics through at least day 9. Pharmacokinetics samples were analysed as above for study 200-4070.
HIV-1 resistance analyses for study GS-US-200-4072 were carried out at Monogram Biosciences using the research-grade gag-protease genotyping (population-level sequencing) and phenotyping assay to assess resistance to GS-6207 using HIV-1 DNA fragment of each participant that encompasses the gag-protease HIV-1 region, and/or using the CLIA-certified PhenoSense GT + Integrase or GenoSure PRIme assay to assess resistance to the components of Biktarvy (which was administered to all participants following the 9-day GS-6207 monotherapy). Resistance analyses were conducted at screening and day 9 (last GS-6207 monotherapy visit).
Within part A, we conducted an interim analysis, which was prespecified in the protocol to be conducted after at least 50% of the participants and/or after all participants within each cohort completed the day-10 visit. The purpose of this interim analysis was to select the doses of GS-6207 to evaluate in each subsequent cohort.
Statistics
GraphPad Prism 7.0 was used for statistical analysis. In each case, an unpaired two-tailed Student’s t-test with Welch’s correction was performed for parametric analysis of two groups. A P value < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this paper.
Data availability
All data to understand and assess the conclusions of this research are available in the Article and Supplementary Information. Raw gel source data for Fig. 2f are available in Supplementary Fig. 1. Small-molecule X-ray crystallographic coordinates and structure factor files have been deposited in the Protein Data Bank (PDB) with accession number 6V2F. Study GS-US-200-4072 was registered with ClinicalTrials.gov, NCT03739866. The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Grant, R. M. et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N. Engl. J. Med. 363, 2587–2599 (2010).
Baeten, J. M. et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N. Engl. J. Med. 367, 399–410 (2012).
Molina, J. M. et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N. Engl. J. Med. 373, 2237–2246 (2015).
Thigpen, M. C. et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N. Engl. J. Med. 367, 423–434 (2012).
WHO. HIV/AIDS Fact Sheets, 15 November 2019. https://www.who.int/news-room/fact-sheets/detail/hiv-aids (WHO, 2019).
Emu, B. et al. Phase 3 study of ibalizumab for multidrug-resistant HIV-1. N. Engl. J. Med. 379, 645–654 (2018).
Bangsberg, D. R. et al. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. AIDS 15, 1181–1183 (2001).
Marrazzo, J. M. et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N. Engl. J. Med. 372, 509–518 (2015).
Anderson, P. L. et al. Emtricitabine–tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci. Transl. Med. 4, 151ra125 (2012).
Gulick, R. M. & Flexner, C. Long-acting HIV drugs for treatment and prevention. Annu. Rev. Med. 70, 137–150 (2019).
Thenin-Houssier, S. & Valente, S. T. HIV-1 capsid inhibitors as antiretroviral agents. Curr. HIV Res. 14, 270–282 (2016).
Carnes, S. K., Sheehan, J. H. & Aiken, C. Inhibitors of the HIV-1 capsid, a target of opportunity. Curr. Opin. HIV AIDS 13, 359–365 (2018).
Scott, D. E., Bayly, A. R., Abell, C. & Skidmore, J. Small molecules, big targets: drug discovery faces the protein–protein interaction challenge. Nat. Rev. Drug Discov. 15, 533–550 (2016).
Freed, E. O. HIV-1 assembly, release and maturation. Nat. Rev. Microbiol. 13, 484–496 (2015).
Ganser, B. K., Li, S., Klishko, V. Y., Finch, J. T. & Sundquist, W. I. Assembly and analysis of conical models for the HIV-1 core. Science 283, 80–83 (1999).
Yamashita, M. & Engelman, A. N. Capsid-dependent host factors in HIV-1 infection. Trends Microbiol. 25, 741–755 (2017).
Huang, P. T. et al. FEZ1 is recruited to a conserved cofactor site on capsid to promote HIV-1 trafficking. Cell Rep. 28, 2373–2385 (2019).
Fernandez, J. et al. Transportin-1 binds to the HIV-1 capsid via a nuclear localization signal and triggers uncoating. Nat. Microbiol. 4, 1840–1850 (2019).
Carlson, L. A. et al. Three-dimensional analysis of budding sites and released virus suggests a revised model for HIV-1 morphogenesis. Cell Host Microbe 4, 592–599 (2008).
Briggs, J. A., Wilk, T., Welker, R., Kräusslich, H. G. & Fuller, S. D. Structural organization of authentic, mature HIV-1 virions and cores. EMBO J. 22, 1707–1715 (2003).
Yant, S. R. et al. A highly potent long-acting small-molecule HIV-1 capsid inhibitor with efficacy in a humanized mouse model. Nat. Med. 25, 1377–1384 (2019).
Graupe, M. et al. Therapeutic compounds. US patent 10,071,985 B2 (2018).
Matreyek, K. A., Yücel, S. S., Li, X. & Engelman, A. Nucleoporin NUP153 phenylalanine-glycine motifs engage a common binding pocket within the HIV-1 capsid protein to mediate lentiviral infectivity. PLoS Pathog. 9, e1003693 (2013).
Price, A. J. et al. CPSF6 defines a conserved capsid interface that modulates HIV-1 replication. PLoS Pathog. 8, e1002896 (2012).
Price, A. J. et al. Host cofactors and pharmacologic ligands share an essential interface in HIV-1 capsid that is lost upon disassembly. PLoS Pathog. 10, e1004459 (2014).
Bhattacharya, A. et al. Structural basis of HIV-1 capsid recognition by PF74 and CPSF6. Proc. Natl Acad. Sci. USA 111, 18625–18630 (2014).
Lee, K. et al. Flexible use of nuclear import pathways by HIV-1. Cell Host Microbe 7, 221–233 (2010).
Perrier, M. et al. Prevalence of gag mutations associated with in vitro resistance to capsid inhibitor GS-CA1 in HIV-1 antiretroviral-naive patients. J. Antimicrob. Chemother. 72, 2954–2955 (2017).
Li, G. et al. Functional conservation of HIV-1 Gag: implications for rational drug design. Retrovirology 10, 126 (2013).
Yant, S. R. et al. In vitro resistance profile of GS-6207, a first-in-class picomolar HIV capsid inhibitor in clinical development as a novel long-acting antiretroviral agent. In 10th IAS Conference on HIV Science http://programme.ias2019.org/Abstract/Abstract/683 (IAS, 2019).
Tsiang, M. et al. Antiviral activity of bictegravir (GS-9883), a novel potent HIV-1 integrase strand transfer inhibitor with an improved resistance profile. Antimicrob. Agents Chemother. 60, 7086–7097 (2016).
Margot, N. A., Gibbs, C. S. & Miller, M. D. Phenotypic susceptibility to bevirimat in isolates from HIV-1-infected patients without prior exposure to bevirimat. Antimicrob. Agents Chemother. 54, 2345–2353 (2010).
Nakabayashi, H., Taketa, K., Miyano, K., Yamane, T. & Sato, J. Growth of human hepatoma cells lines with differentiated functions in chemically defined medium. Cancer Res. 42, 3858–3863 (1982).
Balakrishnan, M. et al. Non-catalytic site HIV-1 integrase inhibitors disrupt core maturation and induce a reverse transcription block in target cells. PLoS ONE 8, e74163 (2013).
Prichard, M. N. & Shipman, C. Jr. Analysis of combinations of antiviral drugs and design of effective multidrug therapies. Antivir. Ther. 1, 9–20 (1996).
Bam, R. A. et al. TLR7 agonist GS-9620 is a potent inhibitor of acute HIV-1 infection in human peripheral blood mononuclear cells. Antimicrob. Agents Chemother. 61, e01369-16 (2016).
Warren, T. K. et al. Therapeutic efficacy of the small molecule GS-5734 against Ebola virus in rhesus monkeys. Nature 531, 381–385 (2016).
Hung, M. et al. Large-scale functional purification of recombinant HIV-1 capsid. PLoS ONE 8, e58035 (2013).
Pornillos, O. et al. X-ray structures of the hexameric building block of the HIV capsid. Cell 137, 1282–1292 (2009).
Pornillos, O., Ganser-Pornillos, B. K. & Yeager, M. Atomic-level modelling of the HIV capsid. Nature 469, 424–427 (2011).
Kissinger, C. R., Gehlhaar, D. K. & Fogel, D. B. Rapid automated molecular replacement by evolutionary search. Acta Crystallogr. D 55, 484–491 (1999).
Adams, P. D. et al. PHENIX: a comprehensive Python-based system for macromolecular structure solution. Acta Crystallogr. D 66, 213–221 (2010).
Emsley, P., Lohkamp, B., Scott, W. G. & Cowtan, K. Features and development of Coot. Acta Crystallogr. D 66, 486–501 (2010).
Acknowledgements
We thank D. Cowfer, K. Brendza, G. Czerwieniec, M. Tsiang, K. Wang, G. Lane, M. Kenney, M. Ceo, S. Kazerani, T. Lane, L. Meng, T. Rainey, A. Vandehey, A. Wagner, M. O’Keefe, J. Yoon, S. Neville, W. Lew, B. Ross, Q. Wang, J. Cha, M. Tran and K. Nguyen for their support and contributions, and all the people who participated in the phase-I clinical trials, including the study participants, their families, and the principal investigators and their staff.
Author information
Authors and Affiliations
Contributions
T.C. conceived the project. D.J., M.H. and N.N. conducted protein purifications, and X.L. and R.S. oversaw the analysis. S.R.Y., N.P., T.Z.C., D.K. and L.L designed, conducted and analysed small-molecule library screens. T.C., J.O.L., S.R.Y., R.L.H., W.C.T., M.S.R. and A.E.C. provided project leadership. J.O.L., W.C.T., S.D.S., C.-H.C., E.C., G.B., J.R.Z., J. Li, M.G., P.M., Q.L., Q.W., R.L.H., R.D.S., S.D.S., S.E.L. and S.B. were responsible for the design, synthesis, characterization and scaling-up of small molecules. A.N.-M. conducted and analysed in vitro CA assembly assays. S.R.Y. and A.N.-M. conducted and analysed virion morphology by electron microscopy. G.J.S., S.A. and H.Y. designed, conducted and analysed high-throughput antiviral measurements. G.J.S, S.A., A.M. and Y.X. conducted cell-based assays for cytotoxicity. G.J.S. conducted and analysed in vitro drug combination studies. A.M. and R.R.R. conducted and analysed in vitro antiviral testing against HIV mutants with resistance to existing agents. A.G.V. and R.L.A. conducted protein crystallization studies, J.R.S. collected and analysed X-ray crystallographic data, and T.C.A. prepared the refinement table. C.E.C. and E.Y.H. conducted structural modelling studies to guide small-molecule development. G.A.P., M.H.W., S.A.L., S.C. and L.L. conducted and analysed biosensor binding studies. S.R.Y. A.M., E.S. and L.K.T. conducted and analysed cell-based mechanism-of-action studies. A.L. conducted and analysed biochemical protease assays. A.M., D.H., R.A.B. and S.R.Y. conducted resistance selection assays and characterized emergent HIV-1 CA variants. J.Z., B.L. and J.M. designed and executed preclinical pharmacokinetics and metabolism studies, and summarized results. A.E.C. oversaw all anatomical pathology examinations and analyses of preclinical animal species. W.R., S. Sellers and A.C. designed and tested drug formulations. A.C. and S.A.W. oversaw GS-6207 chemistry, manufacture and control for clinical studies. M.S.R., R.H., R.B. and D.M.B. designed and supervised the clinical studies, and G.I.S., P.J.R., G.E.C., C.K.M. and E.S.D conducted them. R.B., J. Ling, Y.-P. L., N.M. and C.C. conducted and coordinated clinical sample and statistical analyses. W.I.S. provided project guidance during the early discovery phase, and S. Swaminathan and W.E.L. provided long-term project oversight. S.R.Y., M.S.R., J.O.L. and T.C. wrote the manuscript, with input from all authors.
Corresponding author
Ethics declarations
Competing interests
All authors are current or previous employees of Gilead Sciences (except for G.I.S., P.J.R., G.E.C., C.K.M., W.I.S. and E.S.D.) and received salary and stock ownership as compensation for their employment. M.G., J.O.L., W.R., R.D.S., S.D.S., W.C.T. and J.R.Z. are inventors on granted US patent no. 10,071,985B2 covering GS-6207 composition of matter and methods of use. G.I.S. receives research support from Gilead Sciences, Janssen Pharmaceutica, GlaxoSmithKline, Abbvie and Cepheid, and is on the speaker’s bureau and advisory board for Janssen, ViiV Healthcare and Merck. G.E.C. receives grants (investigator research payments) from Gilead Sciences, ViiV Healthcare, Merck and Janssen Pharmaceutica. C.K.M. receives research support from Gilead Sciences, Merck, ViiV Healthcare and Janssen Pharmaceutica, is on the speaker’s bureau for Gilead Sciences, Merck and Insmed, and is on an advisory board for Gilead Sciences. E.S.D. receives research support from Gilead Sciences, Merck and ViiV Healthcare, and has served as a consultant for Gilead Sciences.
Additional information
Peer review information Nature thanks Daniel R. Kuritzkes, Kevan Shokat and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Supplementary information
Supplementary Information
This file contains Supplementary Figures 1-5 and the Chemistry Experimental details.
Rights and permissions
About this article
Cite this article
Link, J.O., Rhee, M.S., Tse, W.C. et al. Clinical targeting of HIV capsid protein with a long-acting small molecule. Nature 584, 614–618 (2020). https://doi.org/10.1038/s41586-020-2443-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-020-2443-1
- Springer Nature Limited
This article is cited by
-
Lenacapavir: First Approval
Drugs (2022)