Abstract
Various observational studies have examined the prevalence and determinants of erectile dysfunction (ED) in men with type 1 diabetes across different geographical areas. Nevertheless, a comprehensive systematic review and meta-analysis to consolidate the worldwide prevalence and risk factors remains lacking. Hence, the primary study objective was to perform an extensive systematic review and meta-analysis that specifically examined ED prevalence and determinants in men with type 1 diabetes. A thorough exploration was conducted by examining electronic databases, such as PubMed, Embase, and Web of Science. The general ED prevalence and a 95% confidence interval (CI) in men with type 1 diabetes were summarized. The relevant risk factors were analyzed by deriving a comprehensive odds ratio (OR) from merging the ORs using fixed- or random-effects models. The sources of heterogeneity were investigated using subgroup analyses and meta-regression. This systematic review and meta-analysis included 19 articles involving 3788 men with type 1 diabetes. The meta-analysis revealed that men with type 1 diabetes had a combined ED prevalence of 42.5% (95% CI: 34.3%–50.8%). This prevalence showed significant heterogeneity (I2 = 96.2%, P < 0.01). Meta-regression revealed that age (P = 0.016) and type 1 diabetes duration (P = 0.004) were significant causes of heterogeneity. Furthermore, the ED risk in men with type 1 diabetes was significantly influenced by age, type 1 diabetes duration, body mass index, glycated hemoglobin (HbA1c), retinopathy, and smoking habits (all P < 0.05). In summary, this systematic review and meta-analysis revealed a significant prevalence of ED in men with type 1 diabetes, highlighting the importance of clinicians addressing concerns regarding ED in this specific group of individuals.
Similar content being viewed by others
Introduction
Diabetes encompasses both type 1 and type 2 diabetes and is a significant global health concern [1]. Compared to type 2 diabetes, type 1 diabetes is frequently more intense and challenging to manage [2]. Type 1 diabetes necessitates lifelong insulin replacement therapy and is associated with a higher number of complications and a less favorable prognosis [3]. The peak onset period for type 1 diabetes is between 20 and 44 years of age, which overlaps with the patient’s sexually active period [4]. Therefore, greater consideration of the sexual function and reproductive well-being of people with type 1 diabetes is crucial.
Erectile dysfunction (ED) refers to the incapability of the male reproductive organ to achieve and sustain an adequate level of firmness required for the successful completion of pleasurable sexual activity [5]. Normal erectile function depends on normal physiological process and coordination of the psychological state, endocrine system, nerves, and blood vessels, and abnormality in any link will lead to ED [6]. Numerous studies demonstrated that diabetes is closely related to ED. For example, diabetes can cause microvascular disease that leads to insufficient blood supply to the cavernous body, and diabetes-induced peripheral neuropathy affects the nerve endings of the cavernous body, leading to ED [7].
Kouidrat et al. reported that ED prevalence was 37.5%, 66.3%, and 57.7% in men diagnosed with type 1 diabetes, type 2 diabetes, and both types of diabetes, respectively [8]. Nevertheless, their investigation primarily focused on mixed types of diabetes and lacked a comprehensive examination of the factors that contribute to ED in men with type 1 diabetes. Hence, the present study objective was to conduct an inclusive systematic examination and meta-analysis emphasizing the ED prevalence and determinants in men with type 1 diabetes.
Materials and methods
This systematic review and meta-analysis was carried out following the guidelines of the PRISMA statement [9]. The INPLASY(International Platform of Registered Systematic Review and Meta-analysis Protocols) recorded the registration of the protocol. The registration number was INPLASY2023100067, and the DOI number was 10.37766/inplasy2023.10.0067.
Literature search strategies
This systematic review and meta-analysis involved a thorough search of electronic databases including Pubmed, Embase, and Web of Science, starting from the beginning of the databases until September 15, 2023. The search terms utilized included the phrases ‘erectile dysfunction’ OR ‘impotence’ OR ‘sexual satisfaction’ OR ‘sexual problem’ AND ‘type 1 diabetes’ OR ‘type 1 diabetes mellitus’ OR ‘diabetes’ OR ‘T1DM’ OR ‘diabetes mellitus’ AND ‘prevalence’ OR ‘risk’ AND ‘man’ OR ‘male’. Furthermore, we thoroughly examined the citations of pertinent publications to discover additional studies regarding the frequency of ED in men diagnosed with type 1 diabetes.
Study selection, inclusion, and exclusion criteria
Two researchers independently screened the eligible literature by reviewing the title, abstract, and full text based on the inclusion and exclusion criteria. The two reviewers resolved any differences through a discussion with the third reviewer. To be eligible for inclusion, the study had to meet the following criteria: (a) it focused on adult males as the primary group of interest; (b) it provided data on the prevalence of ED; (c) the participants were diagnosed with type 1 diabetes. The criteria for exclusion included: (a) studies that did not involve human subjects; (b) data that had been replicated in another article; (c) articles classified as commentaries, reviews, letters, or conference abstracts; and (d) inadequate availability of research data.
Data extraction and quality assessment
The first author’s name, publication time, study design, study region, sample size, average age, average duration of type 1 diabetes, assessment scale for ED, number of ED cases, ED prevalence, and logistic regression results investigating the risk factors for ED prevalence in males with type 1 diabetes (OR, relative risk(RR), or hazard ratio (HR) with their corresponding 95% CI) were independently extracted by two researchers. The two reviewers resolved any differences through a discussion with the third reviewer. The primary outcome of interest was the ED prevalence among men diagnosed with type 1 diabetes. Potential risk factors for ED, including age, duration of type 1 diabetes, depression, BMI, blood pressure, HbA1c level, fasting glucose, insulin dose, microalbuminuria, total cholesterol, smoking, alcohol consumption, and retinopathy were secondary outcomes. We evaluated the quality of every study included by employing the quality assessment criteria for observational studies as suggested by the Agency for Healthcare Research and Quality (AHRQ). Every individual item was evaluated and categorized as either ‘affirmative’, ‘negative’, or ‘ambiguous’. Research with a score of 8 or more points were classified as high quality, while those with 6−7 points were classified as medium quality, and those with 5 or fewer points were classified as low quality.
Data synthesis and analysis
The statistical analyses were conducted using Stata 16 (StataCorp LLC, College Station, TX, USA). The general ED prevalence and a 95% confidence interval (CI) in men diagnosed with type 1 diabetes were compiled. Additionally, the prevalence in subcategories was examined based on the study region, publication year, research methodology, sample size, study quality, and the ED assessment measure. Heterogeneity among the included studies was evaluated using the Q-test and I2 statistics. I2 > 50% or P < 0.05 indicated heterogeneity, and a random-effects model was utilized. Otherwise, a fixed-effects model was applied. The ORs were combined using fixed- or random-effects models to obtain an overall OR to analyze the relevant risk factors (age, type 1 diabetes duration, body mass index [BMI], glycated hemoglobin [HbA1c] level, smoking, alcohol consumption, and retinopathy). The sources of variation were investigated using subgroup analyses and meta-regression, examining potential factors such as publication year, average age, average diabetes duration, sample size, and study quality. Sensitivity analysis was conducted by excluding each study individually from the meta-analysis to assess its impact. Publication bias was assessed using both Egger’s regression test and Begg’s test. The findings were visualized by examining the funnel plot symmetry.
Results
Literature search results
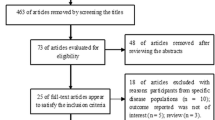
Initially, a thorough search of electronic databases yielded 2561 relevant studies: 523 from PubMed, 1923 from Embase, and 115 from Web of Science. Reviewing the titles and abstracts eliminated 2524 articles, leaving 37 articles for additional evaluation. Examining the full texts eliminated 18 articles(supplement Table 1) due to data from identical samples (n = 10) and unreported or uncomputable required data (n = 7), and one article was a review (n = 1). The 19 studies included in this systematic review and meta-analysis involved 3788 men with type 1 diabetes [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. Figure 1 presents the flowchart illustrating the literature search process, which involved step-by-step reading, screening, and inclusion.
Characteristics of included studies
Table 1 summarizes the essential details of the included studies, patient attributes, and research quality. Most included studies were conducted in Europe (n = 11), followed by North America (n = 5) and Asia (n = 3). Fifteen studies were cross-sectional studies, and four studies were cohort studies. The Agency for Healthcare Research and Quality (AHRQ) quality scores of the studies ranged between 5 and 11. Nine studies were classified as high-quality, nine as moderate-quality, and one as low-quality. ED was predominantly assessed using the International Index of Erectile Function (IIEF-5) questionnaire in >50% of the included studies. ED was detected in 20.11%–70.63% of the participants.
Prevalence of ED in men with type 1 diabetes
The meta-analysis revealed that the combined ED prevalence among men with type 1 diabetes was 42.5% (95% CI: 34.3%–50.8%). This result demonstrated significant variation (I2 = 96.2%, P < 0.01), indicating the requirement for a random-effects model. Figure 2 presents a forest plot derived from the meta-analysis. The ED prevalence in the individual studies was between 20.11% and 70.63%, with the weight of each study ranging from 3.92% to 5.81%. Sensitivity analysis determined that the overall prevalence remained consistent regardless of the exclusions (Fig. 3). The funnel plot exhibited symmetry, indicating no evidence of publication bias (Fig. 4). Begg’s test (P = 0.675) and Egger’s regression test (P = 0.141) supported this finding.
Subgroup analyses of ED prevalence
Table 2 presents the ED prevalence among men with type 1 diabetes according to the subcategories geographic location, publication year, sample size, research methodology, study quality, and the ED assessment measure. After 2018, the ED prevalence in men with type 1 diabetes was 32.8% (22.3%–43.3%), which was lower than the prevalence observed before 2018 (48.1%, 35.9%–60.3%) based on subgroup analysis of the publication year. Geographically, Asia had the highest ED prevalence (49.4%, range: 22.3%–76.5%), whereas Europe had the lowest prevalence (39.5%, range: 31.3%–47.7%). In cross-sectional studies, the ED prevalence was 40.2% (range: 31.7%–48.7%), while ED prevalence in cohort studies was 50.5% (range: 31.0%–70.1%). Furthermore, the subgroup analysis indicated that ED prevalence in the group that completed the IIEF-5 questionnaire was 45.5% (range: 35.0%–56.0%), which was greater than the prevalence in the group that did not complete the questionnaire (35.6%, range: 26.8%–44.5%).
Meta-regression analysis
The primary outcome was subject to high heterogeneity (I2 = 96.2%, P < 0.01). Nevertheless, the subgroup analysis (Table 2) revealed that none of the factors could account for the heterogeneity. A meta-regression analysis was performed to investigate the influence of possible confounding factors on ED prevalence. The meta-regression analysis included the covariates of publication year, mean age, mean diabetes duration, sample size, and study quality. The analysis determined that age (P = 0.016) and type 1 diabetes duration (P = 0.004) were associated with ED prevalence among men with type 1 diabetes (Table 3).
The influence of type 1 diabetes on ED
Three studies [11, 12, 20] investigated whether type 1 diabetes affected the ED risk. As the three studies did not involve substantial variation (I2 = 43.8%, P = 0.169), a fixed-effects model was used instead of a random-effects model. Type 1 diabetes significantly affected the ED risk (OR = 7.52, 95% CI: 4.69–12.08, P < 0.001). Figure 5 presents the OR estimates with 95% CIs for each study and the combined OR.
ED risk factors in men with type 1 diabetes
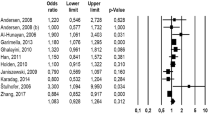
Table 4 presents the findings from the systematic analysis of factors that increase the likelihood of ED in men with type 1 diabetes. The meta-analysis assessed seven risk factors: age, type 1 diabetes duration, BMI, HbA1c level, smoking, alcohol intake, and retinopathy. Figure 6 demonstrates that age (OR = 1.10, 95% CI: 1.06–1.14, P < 0.001), type 1 diabetes duration (OR = 2.81, 95% CI: 1.11–7.11, P = 0.03), BMI (OR = 1.70, 95% CI: 1.24–2.34, P = 0.001), HbA1c (OR = 1.98, 95% CI: 1.53–2.57, P < 0.001), retinopathy (OR = 2.42, 95% CI: 1.89–3.11, P < 0.001), and smoking (OR = 1.68, 95% CI: 1.23–2.29, P = 0.001) were significant risk factors for ED in men with type 1 diabetes.
Discussion
ED, also termed impotence, is a condition where men cannot attain or sustain an erection while engaging in sexual activity [5]. ED is a common and frequent disease among men, which not only seriously affects their physical health but also exerts psychological pressure. ED affects men’s self-esteem and confidence, causing them to experience negative emotions such as anxiety, depression, shame, and self-guilt [29]. These negative emotions might exacerbate mental health issues, affecting social and emotional relationships [30]. ED might also negatively affect partner relationships. Due to the inability to meet sexual needs, sexual communication barriers and mutual pressure might lead to tension, arguments, and disharmony in sexual relationships. Approximately 322 million men globally will experience different levels of ED by 2025, and this figure continues to rise and is also affecting younger men [31, 32].
Most observational studies primarily documented ED prevalence in men with type 2 diabetes. Nonetheless, there is limited information on ED prevalence among men with type 1 diabetes. The main reason for this limited information is that type 1 diabetes is significantly less prevalent than type 2 diabetes. Type 1 and 2 diabetes have distinct pathogeneses. Type 1 diabetes is generally caused by heredity and is more common in children and adolescents. Type 1 diabetes stems from pancreatic islet cell damage, where the cells cannot secrete insulin [2]. In contrast, type 2 diabetes features normal islet cells but a weakened role of insulin, i.e., insulin resistance [33]. As type 1 diabetes is more common in children and adolescents, and young men are at the age of peak sexual life and fertility, the relationship between type 1 diabetes and ED warrants more attention.
To our understanding, this is the initial comprehensive examination and meta-analysis focused on assessing ED prevalence in men with type 1 diabetes. Kouidrat et al. reported that ED prevalence was 37.5%, 66.3%, and 57.7% in men with type 1 diabetes, type 2 diabetes, and both types of diabetes, respectively [8]. Nonetheless, their investigation concentrated on diabetes of various combinations and did not thoroughly examine the factors that contribute to ED prevalence in men with type 1 diabetes. Despite including 145 studies in their systematic review and meta-analysis, only a limited number of studies examined ED prevalence in men with type 1 diabetes. Furthermore, a greater number of studies published after 2017 examined ED frequency in men with type 1 diabetes.
The present systematic review and meta-analysis revealed that ED prevalence among men with type 1 diabetes was 42.5% (95% CI: 34.3%–50.8%). Hence, the present study reports a greater ED prevalence in this population than the study by Kouidrat et al. (42.5% vs. 37.5%). The prevalence estimation accuracy was hindered by the significant between-study heterogeneity (I2 = 96.2%, P < 0.001), as prevalence rates varied from 20.11% to 70.63% across studies. However, subgroup analyses could not explain any source of between-study heterogeneity. Thus, a meta-regression analysis was conducted to evaluate how factors such as publication year, average age, average diabetes duration, sample size, and study quality affect ED prevalence in men with type 1 diabetes. Ultimately, the analysis determined that ED prevalence among men with type 1 diabetes was associated with their age and type 1 diabetes duration. The sensitivity analysis demonstrated that the meta-analysis was relatively robust, enhancing the study’s dependability.
Subgroup analyses were conducted to examine the influence of various population traits on ED prevalence in men with type 1 diabetes. The subgroup analysis based on geographical location determined that ED prevalence was highest in the Asian population (49.4%) and lowest in the European population (39.5%). The variation could be attributed to variances in medical conditions and the effect of treatment on type 1 diabetes across geographical areas. Most European countries are developed countries, while most Asian countries are developing countries, with a significant gap in medical conditions between the two continents. The better medical conditions in Europe might result in better blood glucose control in the male population with diabetes, thus reducing ED prevalence. Additionally, it was determined that ED prevalence in men with type 1 diabetes decreased significantly after 2018 (32.8%) compared to pre-2018 (48.1%). The decrease may be attributed to economic status and healthcare advancements, leading to enhanced blood sugar management. Furthermore, ED prevalence was notably influenced by various ED assessment instruments (45.5% in the IIEF-5 questionnaire group vs. 35.6% in the non-IIEF-5 questionnaire group). Evidence-based medicine has proven that IIEF-5 questionnaire is a reliable, multilingual, cross-cultural, and effective ED measurement scale. The IIEF-5 questionnaire is internationally recognized as an ED self-assessment questionnaire and is widely used globally [34]. Therefore, it is recommended that future studies use IIEF-5 questionnaire, which would enable better comparability among different study populations.
The present investigation aimed to determine if type 1 diabetes increases the likelihood of experiencing ED. The meta-analysis demonstrated that men with type 1 diabetes face a 7.52-fold greater risk of developing ED compared to those without type 1 diabetes. Clinicians and scientists are greatly interested in the underlying mechanisms connecting type 1 diabetes and ED. Several pathogenic and etiological mechanisms have been identified to elucidate this potential association. For example, Maiorino et al. reported that men with type 1 diabetes and ED had decreased levels of circulating endothelial progenitor cells (EPCs). The researchers also determined that the quantity of these cells was an autonomous risk factor for ED [35]. Furthermore, Pajovic et al. reported that men with type 1 diabetes exhibited considerably greater susceptibility to arterial ED compared to men with type 2 diabetes. Arterial dysfunction might be the main cause of ED in type 1 diabetes male patients [36]. Azmi et al. reported that small-fiber neuropathy was a notable occurrence in patients with type 1 diabetes and was strongly correlated with ED [11].
This systematic review and meta-analysis also examined the factors that contribute to ED in men with type 1 diabetes. Ultimately, the factors of age, type 1 diabetes duration, BMI, HbA1c levels, retinopathy, and smoking were significant in ED development in men with type 1 diabetes. The disease duration is an important factor affecting type 1 diabetes complications. The present study determined that disease duration was a significant risk factor for ED among men with type 1 diabetes. The angiopathy and neuropathy of type 1 diabetes are significantly related to the disease course and lead to ED occurrence [2]. Epidemiological studies verified that the primary determinant for ED in the overall populace is advancing age [37]. The present study determined that age was a notable contributing factor to ED development among men with type 1 diabetes. Most type 1 diabetes cases are in young people, specifically children and teenagers. Type 1 diabetes prevalence in elderly men is not well-known, but it is expected to be extremely rare [38]. Hence, a person’s age can partially indicate their type 1 diabetes duration. In the present study, HbA1c emerged as a notable contributing factor for ED in men with type 1 diabetes. HbA1c reflects the patient’s average blood glucose level between four and eight weeks before the blood test and indicates the long-term stability of blood glucose levels. The Epidemiology of Diabetes Interventions and Complications (EDIC) study reported that the intensive treatment group had notably higher ED prevalence than the conventional treatment group, which aligned with the present results [39]. Hence, the healing impact of diabetes was strongly associated with ED prevalence in men with type 1 diabetes. The authors also determined that tobacco use was a notable contributing factor for ED in men with type 1 diabetes. Bortolotti et al. investigated the role of smoking in diabetic men and indicated that smoking affected the likelihood of ED development in men with diabetes. A higher risk was associated with longer and more intense smoking habits [40]. Their result was consistent with the present finding. The present study determined that alcohol consumption was not a significant risk factor for ED. However, only two studies investigated this aspect. Consequently, more research is needed to confirm these results. The association between depression and ED is well-established in the general population [41]. A comprehensive analysis and meta-analysis demonstrated that people with type 1 diabetes had a considerably greater occurrence of depression [42, 43]. Furthermore, genetic evidence from a Mendelian randomization study suggested that depression increases ED risk [44]. Hence, depression is probably a crucial risk element for ED in men with type 1 diabetes. In the present systematic review, two studies [13, 14] indicated that depression was a notable risk element for ED in men with type 1 diabetes (Table 4). Despite the lack of 95% CI in the data from these two studies, the authors believe that depression potentially contributes to ED development in men with type 1 diabetes, rendering it a notable risk factor.
To the authors’ best knowledge, this study is the initial comprehensive examination and meta-analysis exploring the worldwide prevalence and determinants of ED in men with type 1 diabetes. However, this study has several limitations. First, the significant between-study heterogeneity hindered the prevalence estimation accuracy. The meta-regression analysis revealed that age and disease duration were the sources of heterogeneity. Fortunately, the sensitivity analysis demonstrated that the meta-analysis was relatively robust, enhancing the study’s dependability. Second, only 11 included studies evaluated ED using the IIEF-5 questionnaire. Evidence-based medicine has proven that the IIEF-5 questionnaire is a reliable, multilingual, cross-cultural, and effective ED measurement scale. The IIEF-5 questionnaire is internationally recognized as an ED self-assessment questionnaire and is widely used globally [34]. Therefore, it is recommended that future studies use the IIEF-5 questionnaire, which would enable better comparability among different study populations. Furthermore, while age was a noteworthy determinant of ED prevalence in men with type 1 diabetes, it is important to note that this age relates to the time the questionnaire survey was conducted. Besides, numerous recent studies demonstrated a significant correlation between the age at which type 1 diabetes develops and its associated complications [45, 46]. Therefore, future research should also explore the effect of type 1 diabetes onset age on ED prevalence. Finally, most study populations were in North America and Europe. Thus, the present findings might not accurately represent the worldwide ED prevalence in men with type 1 diabetes due to insufficient research in areas such as Oceania, Africa, and South America. Therefore, more studies in these regions are needed to supplement these results.
Conclusion
The present systematic review and meta-analysis revealed high ED prevalence in men with type 1 diabetes, highlighting the importance of clinicians in addressing ED-related concerns in this specific population group. Furthermore, the ED risk in men with type 1 diabetes was significantly influenced by age, type 1 diabetes duration, BMI, HbA1c levels, presence of retinopathy, and smoking habits. More studies in different regions globally are needed to supplement the results. It should be noted that it is recommended that ED be evaluated using the IIEF-5 questionnaire. Additionally, more risk factors, such as age of onset, require further investigation.
Data availability
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
References
Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The growing epidemic of diabetes mellitus. Curr Vasc Pharm. 2020;18:104–9.
Atkinson MA, Eisenbarth GS, Michels AW. Type 1 diabetes. Lancet. 2014;383:69–82.
Melendez-Ramirez LY, Richards RJ, Cefalu WT. Complications of type 1 diabetes. Endocrinol Metab Clin North Am. 2010;39:625–40.
Xu G, Liu B, Sun Y, Du Y, Snetselaar LG, Hu FB, et al. Prevalence of diagnosed type 1 and type 2 diabetes among US adults in 2016 and 2017: population based study. BMJ. 2018;362:k1497.
Yafi FA, Jenkins L, Albersen M, Corona G, Isidori AM, Goldfarb S, et al. Erectile dysfunction. Nat Rev Dis Prim. 2016;2:16003.
MacDonald SM, Burnett AL. Physiology of erection and pathophysiology of erectile dysfunction. Urol Clin North Am. 2021;48:513–25.
Chitaley K, Kupelian V, Subak L, Wessells H. Diabetes, obesity and erectile dysfunction: field overview and research priorities. J Urol. 2009;182:S45–50.
Kouidrat Y, Pizzol D, Cosco T, Thompson T, Carnaghi M, Bertoldo A, et al. High prevalence of erectile dysfunction in diabetes: a systematic review and meta-analysis of 145 studies. Diabet Med. 2017;34:1185–92.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Brunner GA, Pieber TR, Schattenberg S, Ressi G, Wieselmann G, Altziebler S, et al. [Erectile dysfunction in patients with type I diabetes mellitus]. Wien Med Wochenschr. 1995;145:584–6.
Azmi S, Ferdousi M, Alam U, Petropoulos IN, Ponirakis G, Marshall A, et al. Small-fibre neuropathy in men with type 1 diabetes and erectile dysfunction: a cross-sectional study. Diabetologia. 2017;60:1094–101.
Bacon CG, Hu FB, Giovannucci E, Glasser DB, Mittleman MA, Rimm EB. Association of type and duration of diabetes with erectile dysfunction in a large cohort of men. Diabetes Care. 2002;25:1458–63.
Caruso P, Cirillo P, Carbone C, Sarnataro A, Maiorino MI, Bellastella G, et al. Sexual dysfunctions and short-term glucose variability in young men with type 1 diabetes. Hormones. 2021;20:475–82.
Hylmarova S, Stechova K, Pavlinkova G, Peknicova J, Macek M, Kvapil M. The impact of type 1 diabetes mellitus on male sexual functions and sex hormone levels. Endocr J. 2020;67:59–71.
Dan A, Chakraborty K, Mondal M, Neogi R, Chatterjee S, Makhal M. Erectile dysfunction in patients with diabetes mellitus: its magnitude, predictors and their bio-psycho-social interaction: a study from a developing country. Asian J Psychiatr. 2014;7:58–65.
Fedele D, Bortolotti A, Coscelli C, Santeusanio F, Chatenoud L, Colli E, et al. Erectile dysfunction in type 1 and type 2 diabetics in Italy. On behalf of Gruppo Italiano Studio Deficit Erettile nei Diabetici. Int J Epidemiol. 2000;29:524–31.
Kulecki M, Naskret D, Kaminski M, Kasprzak D, Lachowski P, Klause D, et al. Arterial stiffness and the non-dipping pattern in type 1 diabetes males with and without erectile dysfunction. Sci Rep. 2023;13:7265.
Kaminski M, Kulecki M, Lachowski P, Kasprzak D, Kulczycka A, Kozlowska M, et al. Erectile dysfunction in individuals with Type 1 diabetes is associated with long-term metabolic control and diabetic complications: a cross-sectional study. Int J Angiol. 2022;31:97–106.
Nisahan B, Kumanan T, Rajeshkannan N, Peranantharajah T, Aravinthan M. Erectile dysfunction and associated factors among men with diabetes mellitus from a tertiary diabetic center in Northern Sri Lanka. BMC Res Notes. 2019;12:210.
Maiorino MI, Bellastella G, Della Volpe E, Casciano O, Scappaticcio L, Cirillo P, et al. Erectile dysfunction in young men with type 1 diabetes. Int J Impot Res. 2017;29:17–22.
Kalter-Leibovici O, Wainstein J, Ziv A, Harman-Bohem I, Murad H, Raz I, et al. Clinical, socioeconomic, and lifestyle parameters associated with erectile dysfunction among diabetic men. Diabetes Care. 2005;28:1739–44.
Klein R, Klein BE, Moss SE. Ten-year incidence of self-reported erectile dysfunction in people with long-term type 1 diabetes. J Diabetes Complicat. 2005;19:35–41.
Pop-Busui R, Braffett BH, Wessells H, Herman WH, Martin CL, Jacobson AM, et al. Diabetic peripheral neuropathy and urological complications in Type 1 diabetes: findings from the epidemiology of diabetes interventions and complications study. Diabetes Care. 2022;45:119–26.
Van Cauwenberghe J, Enzlin P, Nefs G, Ruige J, Hendrieckx C, De Block C, et al. Prevalence of and risk factors for sexual dysfunctions in adults with type 1 or type 2 diabetes: results from Diabetes MILES - Flanders. Diabet Med. 2022;39:e14676.
Wang F, Dai S, Wang M, Morrison H. Erectile dysfunction and fruit/vegetable consumption among diabetic Canadian men. Urology. 2013;82:1330–5.
Turek SJ, Hastings SM, Sun JK, King GL, Keenan HA. Sexual dysfunction as a marker of cardiovascular disease in males with 50 or more years of type 1 diabetes. Diabetes Care. 2013;36:3222–6.
Georgescu O, Reghina A, Ioacara S, Fica S. Androgen deficiency, erectile dysfunction and chronic microvascular complications in male diabetic patients. Rom J Diabetes Nutr Metab Dis. 2013;20:401–7.
Jamieson F, Chalmers J, Duncan C, Prescott RJ, Campbell IW. Erectile dysfunction in type 1 diabetic males. Br J Diabetes Vasc Dis. 2008;8:232–4.
Manalo TA, Biermann HD, Patil DH, Mehta A. The temporal association of depression and anxiety in young men with erectile dysfunction. J Sex Med. 2022;19:201–6.
Li H, Gao T, Wang R. The role of the sexual partner in managing erectile dysfunction. Nat Rev Urol. 2016;13:168–77.
Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–56.
Nguyen HMT, Gabrielson AT, Hellstrom WJG. Erectile dysfunction in young men-a review of the prevalence and risk factors. Sex Med Rev. 2017;5:508–20.
Hunter CS, Stein RW. Evidence for loss in identity, de-differentiation, and trans-differentiation of Islet beta-Cells in Type 2 diabetes. Front Genet. 2017;8:35.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26.
Maiorino MI, Bellastella G, Petrizzo M, Della Volpe E, Orlando R, Giugliano D, et al. Circulating endothelial progenitor cells in type 1 diabetic patients with erectile dysfunction. Endocrine. 2015;49:415–21.
Pajovic B, Dimitrovski A, Fatic N, Malidzan M, Vukovic M. Vacuum erection device in treatment of organic erectile dysfunction and penile vascular differences between patients with DM type I and DM type II. Aging Male. 2017;20:49–53.
Shamloul R, Ghanem H. Erectile dysfunction. Lancet. 2013;381:153–65.
Toschi E. Type 1 diabetes and aging. Endocrinol Metab Clin North Am. 2023;52:389–403.
Wessells H, Penson DF, Cleary P, Rutledge BN, Lachin JM, McVary KT, et al. Effect of intensive glycemic therapy on erectile function in men with type 1 diabetes. J Urol. 2011;185:1828–34.
Bortolotti A, Fedele D, Chatenoud L, Colli E, Coscelli C, Landoni M, et al. Cigarette smoking: a risk factor for erectile dysfunction in diabetics. Eur Urol. 2001;40:392–6.
Liu Q, Zhang Y, Wang J, Li S, Cheng Y, Guo J, et al. Erectile dysfunction and depression: a systematic review and meta-analysis. J Sex Med. 2018;15:1073–82.
Farooqi A, Gillies C, Sathanapally H, Abner S, Seidu S, Davies MJ, et al. A systematic review and meta-analysis to compare the prevalence of depression between people with and without Type 1 and Type 2 diabetes. Prim Care Diabetes. 2022;16:1–10.
Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2016;70:70–84.
Ma K, Song P, Liu Z, Yang L, Wang L, Zhou J, et al. Genetic evidence suggests that depression increases the risk of erectile dysfunction: a Mendelian randomization study. Front Genet. 2022;13:1026227.
Rawshani A, Sattar N, Franzen S, Rawshani A, Hattersley AT, Svensson AM, et al. Excess mortality and cardiovascular disease in young adults with type 1 diabetes in relation to age at onset: a nationwide, register-based cohort study. Lancet. 2018;392:477–86.
Hietala K, Harjutsalo V, Forsblom C, Summanen P, Groop PH, FinnDiane Study G. Age at onset and the risk of proliferative retinopathy in type 1 diabetes. Diabetes Care. 2010;33:1315–9.
Funding
The research was funded by the Shaoxing Health Science and Technology Project (Grant Number 2022KY012).
Author information
Authors and Affiliations
Contributions
XLZ provided the presented idea. XLZ, ZRZ, and GLT performed the data analysis. XLZ wrote the manuscript. GLT did critical reading and editing the manuscript. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Zhu, Z. & Tang, G. Global prevalence of erectile dysfunction and its associated risk factors among men with type 1 diabetes: a systematic review and meta-analysis. Int J Impot Res 36, 365–374 (2024). https://doi.org/10.1038/s41443-024-00855-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-024-00855-0
- Springer Nature Limited