Abstract
Post-orgasmic illness syndrome (POIS) is a rare, but debilitating cluster of symptoms, occurring after ejaculation with unknown mechanism and uncertain treatment. To the best of our knowledge, this study, which is thought to be the first in the literature, is aimed to investigate the practice patterns of sexual medicine experts towards POIS. Worldwide sexual medicine experts were invited to participate anonymously in an online, open survey using SurveyMonkey between November 14, 2022, and January 15, 2023. In total 211 sexual medicine experts filled the survey. The majority of the participants were urologists (83.9%). Most participants stated that the available information about POIS was inadequate for both patients and physicians. 47.9% of the participants stated psychological disorder, 46.4% stated bio-psycho-social reasons for the responsibility for the pathophysiology of POIS. 56.4% of the participants stated that they would refer the patient for psychotherapy/sexual therapy to a sexologist, 41.7% would prefer antihistamine drugs to manage symptoms. Only 18% of participants reported symptom improvement in more than 30% of the patients. This survey study among sexual medicine experts from different parts of the world has developed representative estimates of knowledge, attitudes and practice patterns regarding POIS worldwide.
Similar content being viewed by others
Introduction
Post-orgasmic illness syndrome (POIS) is a rare condition that was first described in 2002 by Waldinger and Schweitzer in two heterosexual male patients and the affected individuals experience flu-like symptoms such as fever, muscle pain, fatigue, and irritability after an orgasm [1,2,3]. Symptoms can occur within seconds or hours after an orgasm, sexual intercourse, masturbation, or spontaneous nocturnal ejaculation and may last for 2–7 days orgasm [1,2,3]. In order not to be affected by these bothersome symptoms as much as possible, people avoid sexual intercourse or schedule sexual activity according to important social or professional obligations. This can be quite uncomfortable and reduce the quality of life of both the patients and their partners [2, 4].
The prevalence of POIS is unknown and difficult to determine because many affected people do not seek medical help and most doctors are unfamiliar with the syndrome and its impact on quality of life. To date, a limited number of cases have been described in the literature, and most studies on POIS are case reports [3, 5]. The number of self-reported POIS cases on online forums is increasing rapidly. However, the number of patients reporting these concerns is anticipated to increase as the criteria become clearer and the disease is adequately recognized.
Unfortunately, limited information is available on POIS diagnosis, treatment, and disease management. To the best of our knowledge, this global survey, which is thought to be the first in the literature, aims to investigate the practice patterns of sexual medicine experts towards POIS. Moreover, this is an attempt to understand how the medical experts around the world approach and manage with POIS patients, as well as how these practices may differ amongst experts.
Materials and methods
Worldwide sexual medicine experts were invited to participate anonymously in an online, self-administered, open survey using Survey Monkey between November 14, 2022, and January 15, 2023. This cross-sectional study was approved by the institutional review board (Approval number: E.245213).
The survey included a brief introduction about POIS and hints about the survey. It consisted of 15 closed-ended questions and 1 open-ended question. Written informed consent was obtained from the participants before participating in the survey. The survey link was shared on various social media groups, on the websites of national and international associations, and via email to reach as many people as possible. The first four questions of the survey included sociodemographic information about the participants, and the remaining questions covered the participants’ current clinical practice models about the physiopathology, diagnosis, and treatment of POIS (Appendix 1).
Individuals who did not give their consent to participate in the study, did not complete the entire survey, were not sexual medicine expert and did not speak English were excluded from the study.
The study, survey design, and distribution were planned according to “The Checklist for Reporting Results of Internet E-Surveys (CHERRIES)” guidelines and checklist [6] (Appendix 2).
Statistical analysis
SPSS V22.0 statistical software package (SPSS, Inc., Chicago, IL, USA) was used for all data analyses. Categorical variables were presented as numbers (percentage).
Results
Overall, 211 sexual medicine experts participated in the survey. The mean age of the participants was 45.4 years (21–80 years), and 83.9% of the participants were male. The majority of the participants were urologists (83.9%), followed by sexual therapists (7.1%) and psychiatrists (4.7%). While 46.9% of the participants had more than 10 years of experience in sexual medicine, 18.9% had between 5 and 10 years of experience, and 34.1% had less than 5 years of experience (Table 1).
Of the participants, 51.2% stated that they manage 1–5 patients with POIS per year, 11.4% stated that they have 6–15, and 6.6% stated that they manage more than 15 patients with POIS per year while 30.8% of the participants stated that they had never seen a patient with POIS. In another words, 146 experts who responded to this survey have seen POIS patients. The majority of the participants (53.5%) considered POIS to be an important sexual dysfunction that should be treated; 40.3% of the participants stated that POIS should only be treated if the patient is really bothered by the condition; and 6.2% did not believe that POIS should be treated. Furthermore, most participants stated that the available information about POIS was inadequate for both patients and physicians (65.9% and 66.3%, respectively).
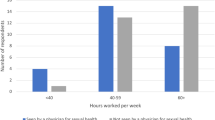
When asked to list of the factors that are responsible for the pathophysiology of POIS, 47.9% of the participants stated psychological disorder, 46.4% stated bio-psycho-social reasons, 41.2% stated a transient deregulation of the autonomic nervous system, and 39.8% stated autoimmune or allergic type reaction (Fig. 1).
In terms of respondents’ treatment approach for a patient diagnosed with POIS, 56.4% of the participants stated that they would refer the patient for psychotherapy/sexual therapy to a sexologist, 41.7% would prefer antihistamine drugs to manage symptoms, and 38.4% would prefer Selective Serotonin Reuptake Inhibitor (SSRI) drugs (Fig. 2). In terms of follow-up frequency, 36.5% of the participants stated that they schedule follow-up visits with POIS patients after 1 month, 23.2% schedule a follow-up visit after 3 months, and 15.2% do not schedule follow-up visits for the patients with POIS. Nearly half of the participants (48.3%) reported symptom improvement in less than 10% of patients with their recommendations, while 32.7% reported symptom improvement in 10–30% of patients, and 18% reported symptom improvement in more than 30% of the patients. 12 of the participants state that they both see 6 or more patients per year and report symptom improvements in 30% or more patients.
Discussion
POIS is a rare and underreported disorder that causes both physical and psychological symptoms [7, 8]. There is currently no standard treatment modality for POIS [9]. To the best of our knowledge, this is the first study in the literature to investigate the knowledge of sexual medicine experts on POIS and their approaches to patients with POIS globally. According to the participants’ statements, the current knowledge about POIS is insufficient for both patients and physicians, there is no consensus on the pathophysiology of POIS, and most specialists refer POIS patients to psychotherapy for treatment. In addition, our findings emphasize that there is a wide variety of treatment practices among sexual medicine experts for this disease, for which no definitive treatment has been reported in the literature and reinforce the differences in how specialists approach POIS.
The literature describes hundreds of POIS cases [2, 9,10,11,12]; internet forums of POIS patients who are looking for information and sharing their experiences have thousands of members (https://poiscenter.com/forums/index.php?PHPSESSID=dfb420efbdab67a4152ef444c63f691e&action=stats, https://www.reddit.com/r/POIS, https://www.facebook.com/groups/1457009341209480/members). Yet, POIS is classified as a rare disease [13, 14]. The reason for this disconnect might be due to a lack of awareness among healthcare professionals about POIS. POIS may be underdiagnosed, misdiagnosed, and underreported [7]. Supporting this view, about 70% of the participants stated that they had seen a patient with POIS per year. Since this many doctors have seen POIS patients, there must be a lot of people with POIS and a lot of doctors have first-hand experience with POIS patients.
The physical and psychological effects of POIS can significantly affect patients’ quality of life [4]. To reduce symptoms, most patients with POIS try to limit sexual activity as much as possible, as well as avoid masturbation or sexual intercourse despite a normal sexual desire [15]. Furthermore, many patients have to schedule sexual activity in advance to avoid discomfort during daily activities such as work or school because ejaculation can reduce the concentration, alertness, and physical capacity of patients with POIS [9, 11]. It has been emphasized that POIS affects not only men but also their partners [2, 7]. Therefore, in one study, it was found that 10% of the patients divorced during follow-up because of avoiding sexual intercourse [2]. Accordingly, more than 50% of the participants in this study considered POIS to be an important sexual problem that should be treated, while about 40% argued that it should be treated if the patient is uncomfortable with his/her current situation. In addition, the majority of participants in the present study noted that the information available for POIS was inadequate, with similar rates for both patients and physicians. This is a core difficulty in disease management, and the need for continuing education in this subject is evident. Adequate and continuous education for sexual medicine experts can help them enhance their knowledge, attitudes, practices, and confidence in the management of POIS for patients.
Despite its significant impact on quality of life, there are few studies examining the etiology of POIS because of its rarity in the general population [2, 5, 8]. Various theories have been proposed about the pathophysiology of POIS, such as dysregulated cytokine or neuroendocrine responses, immunological phenomena, opioid-like withdrawal, Delayed Onset Muscle Soreness (DOMS) and hypersensitivity with transient dysregulation of the autonomic nervous system [2, 4, 5, 16,17,18,19,20]. Consistent with the lack of consensus in the literature, approximately 47% of the participants in the present study reported psychological factors, 46% reported bio-psycho-social reasons, 41% reported a transient deregulation of the autonomic nervous system, and 39% reported autoimmune reasons as etiological factors for POIS.
As in its etiology, there are no accepted and definite practices in the clinical management of POIS, such as diagnosis, follow-up and treatment [10]. Treatment options include various methods such as nonsteroidal anti-inflammatory drugs, analgesics, SSRIs, benzodiazepines, silodosin and hyposensitization therapy, but these methods do not have a confirmed efficacy and have many limitations [2, 8, 9, 16, 18]. The lack of a proven definitive treatment is in line with the varied responses of the participants in this study; accordingly, 56% of the participants refer patients to psychotherapy/sexual therapy, 41% prefer antihistamines, and 38% prefer SSRI treatment. Although psychotherapy/sexual therapy is the most commonly used treatment method, it can be thought that it may be related to the associated symptoms of anxiety, distress, and depressive mood, as clinicians are generally unfamiliar with POIS. Despite POIS is a disturbing condition, it is uncertain whether patients with the disease develop anxiety or depression as a consequence of the disease or whether patients with depression or anxiety are more likely to be diagnosed with POIS. More research is clearly required to determine the actual efficacy and side effects of different treatments for POIS and for educational activities to change the treatment approaches of medical professionals. Furthermore, approximately 36% of the participants followed up POIS patients after 1 month, 23% followed up after 3 months, and 15% did not schedule any follow-up, which indicates that there is no consensus among sexual medicine experts in the management of POIS, as in the literature. In addition, 48% of the participants reported improvement in less than 10% of the patients with their treatment approach, indicating that considerably more research is required to clarify the treatment of the disease. Further studies and education of the patients and physicians are required to improve the management and outcomes of POIS.
This study has some limitations, such as its survey-based design. Moreover, as with all online surveys, it was not possible to completely eliminate the selection bias for participation. In this study, only urologists, sexual therapists, psychiatrists, and a few other low-numbered experts took part. Despite the criticism of internet-based surveys, the survey in this study also offers maximum participation in different countries in a relatively short period of time. Participants may not have accurately responded to the survey; however, given its anonymous nature, this risk is estimated to be minimal. Other limitations include the fact that the study’s data may not fully reflect current clinical practice because it is based on self-report rather than practical observations, the use of an unvalidated questionnaire in the study, and the lack of homogeneity in the participants’ professional backgrounds, experiences, and geographical distribution.
In conclusion, this survey study among sexual medicine experts from different parts of the world has developed representative estimates of knowledge, attitudes and practice patterns regarding POIS worldwide. Differences in POIS knowledge, management, and treatment approaches are noteworthy among sexual medicine experts around the world. Furthermore, sexual medicine experts stated that there is not adequate information available about POIS for physicians and patients. More educational initiatives on POIS are needed for sexual medicine experts to treat and manage patients better and increase their awareness of the disease. On the other hand, it is obvious that more studies such as more detailed survey of experts who report a relatively high success rate in order to find out what specific treatments or approaches they use are needed to shed light on this disease. Moreover, there are many individuals who are searching for a doctor with POIS experience, it would be helpful to create a website that lists those doctors.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Waldinger MD, Schweitzer DH. Postorgasmic illness syndrome: two cases. J Sex Marital Ther. 2002;28:251–5.
Waldinger MD, Meinardi MM, Zwinderman AH, Schweitzer DH. Postorgasmic Illness Syndrome (POIS) in 45 Dutch caucasian males: clinical characteristics and evidence for an immunogenic pathogenesis (Part 1). J Sex Med. 2011;8:1164–70.
Abdessater M, Elias S, Mikhael E, Alhammadi A, Beley S. Post orgasmic illness syndrome: what do we know till now? Basic Clin Androl. 2019;29:13.
Ashby J, Goldmeier D. Postorgasm illness syndrome-a spectrum of illnesses. J Sex Med. 2010;7:1976–81.
Jiang N, Xi G, Li H, Yin J. Postorgasmic illness syndrome (POIS) in a Chinese man: no proof for IgE-mediated allergy to semen. J Sex Med. 2015;12:840–5.
Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e34.
Nguyen HMT, Bala A, Gabrielson AT, Hellstrom WJG. Post-orgasmic illness syndrome: a review. Sex Med Rev. 2018;6:11–5.
Waldinger MD. Post orgasmic illness syndrome (POIS). Transl Androl Urol. 2016;5:602–6.
Reisman Y. Clinical experience with post-orgasmic illness syndrome (POIS) patients-characteristics and possible treatment modality. Int J Impot Res. 2021;33:556–62.
Strashny A. First assessment of the validity of the only diagnostic criteria for postorgasmic illness syndrome (POIS). Int J Impot Res. 2019;31:369–73.
Natale C, Gabrielson A, Tue Nguyen HM, Dick B, Hellstrom WJG. Analysis of the symptomatology, disease course, and treatment of postorgasmic illness syndrome in a large sample. J Sex Med. 2020;17:2229–35.
Rosetti L, Kanani A, Witherspoon L, Flannigan R, Elliott S. Case series: expanding diagnostic markers in postorgasmic illness syndrome. Sex Med. 2023;11:qfac021.
U.S. Department of Health & Human Services. National Institutes of Health. Genetic and rare diseases information center, 2020. Postorgasmic illness syndrome. https://rarediseases.info.nih.gov/diseases/10809/postorgasmic-illness-syndrome.
Le TV, Nguyen HMT, Hellstrom WJG. Postorgasmic Illness Syndrome: What do we know so far? J Rare Dis Res Treat. 2018;3:29–33.
Waldinger MD, Meinardi MM, Schweitzer DH. Hyposensitization therapy with autologous semen in two Dutch caucasian males: beneficial effects in Postorgasmic Illness Syndrome (POIS; Part 2). J Sex Med. 2011;8:1171–6.
Kim TB, Shim YS, Lee SM, Son ES, Shim JW, Lee SP. Intralymphatic Immunotherapy With Autologous Semen in a Korean Man With Post-Orgasmic Illness Syndrome. Sex Med. 2018;6:174–9.
Bignami B, Honore T, Turmel N, Haddad R, Weglinski L, Le Breton F, et al. [Post-orgasmic illness syndrome]. Prog Urol. 2017;27:446–8.
Nguyen T, Dimov V, Bewtra A. Seminal fluid hypersensitivity in a man with postorgasmic illness syndrome (Pois). Ann Allerg Asthma Immunol. 2011;107:A48.
Sonkodi B, Kopa Z, Nyirády P. Post Orgasmic Illness Syndrome (POIS) and Delayed Onset Muscle Soreness (DOMS): Do They Have Anything in Common? Cells. 2021;10:1867.
Acknowledgements
The authors would like to thank the Global Andrology Forum (GAF), European Society for Sexual Medicine (ESSM), Sexual Medicine Society of North America (SMSNA), Society of Urological Surgery in Turkey (SUS) and International Society for Sexual Medicine (ISSM) for their valuable contribution to the distribution of the survey.
Author information
Authors and Affiliations
Contributions
Concept and design; MBD, ECS, data collecting or processing; MBD, RSR, YR, analysis and interpretation of findings; MBD, literature search; MBD, ECS, writing; MBD, ECS, Drafting or revision of the manuscript; MBD, ECS, RSR, YR, Approval of the final version of the manuscript; MBD, ECS, RSR, YR.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Duran, M.B., Rubin, R.S., Reisman, Y. et al. Recognition and practice patterns of sexual medicine experts towards postorgasmic illness syndrome. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00753-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00753-x
- Springer Nature Limited
This article is cited by
-
Post orgasmic illness syndrome: a review
International Journal of Impotence Research (2024)