Abstract
Relaxin, an endogenous peptide hormone, elicits vascular relaxation by its direct effect or by modulating the endothelium-dependent relaxation response and is clinically evaluated for the treatment of coronary artery disease. However, its effect on penile tissue has not been explored yet. This study aimed to investigate the effect of serelaxin, recombinant human relaxin-2, on rat corpus cavernosum (CC) under healthy and hyperglycemic conditions. Strips of CC obtained from thirty-nine male Wistar rats weighing 300–350 g were used in organ baths for isometric tension studies to investigate the serelaxin-mediated relaxation (10−12–10−7 M) under normoglycemic conditions and the effect of serelaxin on endothelium-dependent [nitric oxide (NO)- and prostacyclin-mediated] relaxation responses under hyperglycemic conditions. The in vitro hyperglycemia model was created by 3 h of incubation with 44 mM glucose monohydrate +120 μM methylglyoxal. NO-dependent relaxation responses were evaluated by cumulative acetylcholine (10−9–10−4 M) administration in the presence of indomethacin (10−6 M). Prostacyclin-mediated relaxation was evaluated by cumulative administration of iloprost (10−9–10−6 M), a prostacyclin analog. Maximum relaxation responses to serelaxin were not significantly different compared to the time-control (p = 0.480). Three hours of incubation of rat CC in hyperglycemic conditions impaired NO- and prostacyclin-mediated relaxation responses (p = 0.032 and p = 0.047, respectively). Serelaxin coincubation worsened NO-mediated relaxation responses (p = 0.016) but did not affect prostacyclin-mediated responses (p = 0.425). Together, our results demonstrate that in vitro administration of serelaxin does not cause relaxation in penile tissue and short-term in vitro serelaxin treatment in hyperglycemic conditions mimicked diabetes modulates endothelium-dependent responses by worsening NO-mediated responses. Serelaxin exerts different effects via different mechanism on endothelium-dependent responses depending on the dose and duration of exposure. Therefore, proper timing and dosing of serelaxin administration in the penile tissue need to be investigated in further studies in diabetic animal models.

Similar content being viewed by others
Introduction
Penile erection is a complex physiological process that occurs with neurological stimulation and vascular relaxation followed by the capture of incoming blood by the enlarged sinusoids and increased intracavernosal pressure after veno-occlusion [1]. The integrity and function of the endothelium is very important for the physiology of penile erection because vasodilation, which is responsible for the initiation and maintenance of erection, occurs via endothelial-derived substances in the corpus cavernosum (CC). Nitric oxide (NO) is the essential substance mediating the relaxation of CC smooth muscle [2] and is formed by the activation of the Ca2+/calmodulin/neuronal NO synthase (nNOS) pathway as a result of neuronal stimulation. NO synthesized via nNOS is responsible for penile blood flow at the onset of the erection and creates the initial phase of erection [3]. Initially, increased penile blood flow induces shear stress and activates the phosphatidylinositol-3-kinase (PI3K)/Akt/endothelial NO synthase (eNOS) pathway, resulting in NO-mediated relaxation supporting sustained maximal penile erection [3]. In addition to NO, prostacyclin is another vasodilator released from the cavernosal arteries and endothelium in the CC. The human penis has been shown to synthesize considerable amounts of prostacyclin [4]. Hyperglycemia induces the formation of advanced glycation end products (AGEs) and increases oxidative stress. Thus the functional responses of penile endothelial cells are impaired [5, 6], resulting in the regulatory mechanisms of endothelial cells on penile smooth muscle are damaged and diabetic erectile dysfunction occurs [7]. Revealing the effectiveness of new substances that cause relaxation of the penile tissue and modulate endothelial function can provide different perspectives for research on the treatment of diabetic erectile dysfunction.
Relaxin hormone was first described by Frederick L. Hisaw in 1926 for its relaxing effect on the pubic ligaments in the female reproductive system [8]. There are three types of relaxin: relaxin-1, relaxin-2, and relaxin-3. Relaxin-2 is the major circulating and biologically significant form of relaxin in humans [9]. Serelaxin is the recombinant form of the relaxin-2 peptide. Apart from the female reproductive system, the effects of relaxin have also been demonstrated in the male reproductive system. Relaxin is produced in the reproductive system of male animals, released into the seminal fluid and may increase fertility by increasing the motility of spermatozoa [10, 11]. Relaxin immunoreactivity was identified in the seminal plasma, the glandular epithelium of the prostate, the seminal vesicles and the ampullary part of the vas deferens in human males [12, 13]. The mRNA expression of relaxin family peptide receptor 1 (RXFP1) has been shown in the human prostate gland in both normal and cancer tissues [14]. The RXFP1 receptor was also identified on ejaculated human spermatozoa [15, 16]. Ferlin et al. reported that relaxin positively affects human sperm functions linked to fertilizing ability by decreasing sperm apoptosis and increasing sperm mitochondrial activity, acrosome reaction, intracellular calcium levels and hyperactivating motility. These effects seemed to be mediated by its receptor RXFP1 [15].
Recent studies also highlight the importance of relaxin in the cardiovascular system. These studies indicate that relaxin directly induces relaxation in some blood vessels, such as small human gluteal resistance arteries, mouse mesenteric arteries, rat and mouse small renal arteries, and human subcutaneous arteries, by endothelium-dependent mechanisms [17,18,19]. Despite the importance of endothelium-dependent relaxation in the CC being recognized, the relaxation response to serelaxin has not been investigated in CC tissue. In addition, relaxin has been shown to ameliorate in vitro-induced endothelial dysfunction in the aorta by modulating endothelial-derived vasodilators such as NO and prostacyclin [20, 21]. It has been previously shown that in vitro hyperglycemic conditions cause endothelial dysfunction in the CC [22]. In light of this knowledge, we first investigated the serelaxin-mediated relaxations in the CC in in vitro normoglycemic conditions, and second, we investigated the effect of serelaxin on endothelium-dependent relaxation responses in rat CC under in vitro hyperglycemic conditions that mimicked diabetic conditions.
Materials and methods
Animals
This study was approved by the Institutional Animal Care and Investigational Committee (02/2020) in accordance with the Guide for the Care and Use of Laboratory Animals published by the National Institutes of Health (NIH) in the United States and conforms to the ARRIVE guidelines. Thirty-nine healthy male Wistar albino rats weighing 300–350 g were used for all experiments. All animals were housed in identical cages under standard laboratory conditions (temperature 23 °C, 12-h light-dark cycle). All animals were fed a standard plain diet and were allowed free access to water.
In vitro organ bath studies
The animals were ethically euthanized by cervical dislocation. Then, the penile tissue was excised and placed in Krebs solution composed of the following compounds (mM): NaCl 118, KCl 4.7, CaCl2.2H2O 2.5, MgSO4 1.2, KH2PO4 1.2, NaHCO3 25 and glucose monohydrate 11. Tunica albuginea and corpus spongiosum tissue were removed, and two CC strips were prepared (2 × 2 × 10 mm3) from one animal’s penile tissue. The strips were suspended in organ baths containing 10 mL of Krebs solution under 500 mg of tension. The solution was kept at 37 °C and gassed continuously with a 95% O2 and 5% CO2 gas mixture. The tissues were washed with Krebs solution every 15 min during the equilibration period of 60 min. After the equilibration period, CC strips were contracted with 80 mM potassium chloride (KCl) at the beginning of the experiment to verify the viability of the tissues, and noncontractile tissues were excluded from the study. Each study group included n = 6–7 strips. Isometric tensions were recorded with an amplifier system (MP30 Biopac Systems Inc., Santa Barbara, CA, USA) on a computer by using the Biopac computer program.
Evaluation of serelaxin-mediated relaxations in CC tissue under normoglycemic conditions
Serelaxin was applied cumulatively (10−12–10−7 M) to the CC tissues precontracted with phenylephrine (3 × 10−5 M). The time-control of serelaxin was also studied while obtaining cumulative dose responses to rule out possible time-dependent spontaneous relaxation. In the serelaxin time-control group, tissues were precontracted with phenylephrine (3 × 10−5 M) and then subjected to time-dependent spontaneous relaxation (Fig. 1A).
In vitro hyperglycemia model
To obtain hyperglycemic conditions, CC tissues were incubated for 3 h with Krebs buffer containing 44 mM glucose monohydrate + 120 μM methylglyoxal. Every 1 h, the Krebs solution in the organ baths was refreshed. Endothelial dysfunction due to hyperglycemia was determined by acetylcholine-mediated relaxation responses. At the beginning of this experiment, acetylcholine was applied cumulatively (10−9–10−4 M) to the CC tissues precontracted with phenylephrine (3 × 10−5 M). After the tension of the tissues reached the baseline value, the tissues were incubated under hyperglycemic conditions for 3 h. At the end of the incubation period, the acetylcholine dose‒response curve was obtained again. The same protocol was applied in normoglycemic conditions (Fig. 1B).
Effects of serelaxin on endothelium-dependent relaxation responses in hyperglycemic conditions
Endothelium-dependent relaxation responses were evaluated by NO- and prostacyclin-mediated relaxation responses. Acetylcholine was applied cumulatively (10−9–10−4 M) to CC tissues precontracted with phenylephrine (3 × 10−5 M) to obtain NO-mediated relaxation responses after 3 h of incubation under normoglycemic conditions, hyperglycemic conditions and hyperglycemic conditions in the presence of serelaxin (10−8 M) (Fig. 1C). Because prostacyclin is also a mediator of acetylcholine-induced vasodilatation, indomethacin (10−6 M), a cyclooxygenase (COX) inhibitor, was added to the organ bath to inhibit prostacyclin formation 30 min prior to contraction with phenylephrine. COX is known to be a key enzyme associated with the production of prostaglandin H2, a precursor for numerous vasodilators [23]. Iloprost, a prostacyclin analog, was applied cumulatively (10−9–10−6 M) [24] to CC tissues precontracted with phenylephrine (3 × 10−5 M) to obtain prostacyclin-mediated relaxation responses after 3 h of incubation in normoglycemic conditions, hyperglycemic conditions and hyperglycemic conditions in the presence of serelaxin (10−8 M) (Fig. 1C).
To show that dimethyl sulfoxide (DMSO), the solvent of indomethacin and iloprost, does not have a relaxing effect on CC, acetylcholine-mediated relaxation responses were obtained in the presence and absence of DMSO. A control group was made for only the 0.055% DMSO concentration. Since an effect of 0.055% DMSO on CC tissue was not observed, the effect of lower concentrations was not studied.
Chemicals
Acetylcholine chloride (A6625), phenylephrine hydrochloride (P6126), indomethacin (I-7378), iloprost (SML 1651) (a potent prostacyclin analog), and methylglyoxal solution (M0252) were purchased from Sigma‒Aldrich® (St. Louis, MO, USA); recombinant human relaxin-2 (serelaxin) (A1917, Cat no 0314424) was purchased from PeproTech® (Rocky Hill, NJ, USA); and DMSO was purchased from Merck® (Darmstadt, Germany). Phenylephrine, acetylcholine, and serelaxin were dissolved in distilled water. Iloprost (0.01%) and indomethacin (0.055%) were initially dissolved in DMSO.
Statistical analysis
Data are expressed as the mean ± standard error of the mean (SEM). Relaxation responses to acetylcholine, serelaxin and iloprost were calculated based on the percentage of phenylephrine contraction. Statistical analysis was performed by two-way analysis of variance and the post hoc Bonferroni test in the case of multiple concentration comparisons. Paired or unpaired t tests were used for two-group comparisons, and one-way analysis of variance and post hoc Bonferroni tests were performed for three-group comparisons (GraphPad Prism 9.3.1, San Diego, CA, USA). P values < 0.05 were considered statistically significant. The potency of agonists was assessed by the pD2 values, which are -logEC50 (M).
Results
Evaluation of serelaxin-mediated relaxations in CC tissue under normoglycemic conditions
Cumulative addition of serelaxin caused a 45.6% ± 4.6% maximal relaxation response in the CC tissue. When the maximal relaxation responses of serelaxin and the time-matched control group were compared, the differences were not statistically significant (p = 0.480) (Fig. 2).
Dose‒response curve of serelaxin (10-12–10−7 M) and spontaneous relaxation curve after precontraction with phenylephrine. The number of strips in all groups: n = 6. Relaxation responses are expressed as a percentage of phenylephrine-induced contraction. Two-way ANOVA and the post hoc Bonferroni test were used in the comparison of groups.
In vitro hyperglycemia model
Hyperglycemia-induced endothelial dysfunction was confirmed by a decreased relaxation response to acetylcholine. The maximal relaxation to acetylcholine after 3 h of incubation under hyperglycemic conditions was decreased compared to the maximal relaxation responses obtained before the incubation period (29.0% ± 6.1% and 44.7% ± 3.2%, respectively, p = 0.048) (Fig. 3A). However, a 3 h incubation period under normoglycemic conditions did not cause a change in the maximal relaxation to acetylcholine compared with that obtained before the incubation period (41.2% ± 4.3% and 41.8% ± 2.5%, respectively, p = 0.920) (Fig. 3B).
A Effect of 3 h of incubation in hyperglycemic conditions on the maximum relaxation to acetylcholine in the CC. B Effect of 3 h of incubation in normoglycemic conditions on the maximum relaxation to acetylcholine in the CC. The number of strips in all groups: n = 6. Relaxation responses are expressed as a percentage of phenylephrine-induced contraction. A paired t test was used in the comparison of groups. NS nonsignificant. *p = 0.048 vs. before hyperglycemic conditions.
Effects of serelaxin on endothelium-dependent relaxation responses in hyperglycemic conditions
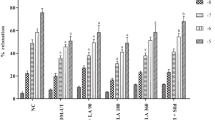
The relaxation responses to acetylcholine in the presence of indomethacin were only decreased with the maximal dose in the hyperglycemia group compared to the normoglycemia group (29.3% ± 3.1% and 40.6% ± 2.5%, respectively, p = 0.032) (Fig. 4). The pD2 values of acetylcholine (potency of acetylcholine) were also significantly decreased in the hyperglycemia group compared to the normoglycemia group (p = 0.034) (Table 1). The relaxation response to acetylcholine was decreased at all doses in the hyperglycemia group in the presence of serelaxin compared to the hyperglycemia group alone (p = 0.021, p = 0.014, p = 0.042, p = 0.028, p = 0.035, and p = 0.016 for concentrations of 10−9 M, 10−8 M, 10−7 M, 10−6 M, 10−5 M, and 10−4 M, respectively) (Fig. 4). The pD2 values of acetylcholine were not different between the two groups (p = 0.077) (Table 1). Serelaxin did not normalize the impairment; in contrast, the damage due to hyperglycemia was potentiated in the presence of serelaxin. To evaluate whether DMSO causes relaxation in the CC, acetylcholine dose‒response curves were obtained in the presence and absence of DMSO. Maximal relaxation responses to acetylcholine in the presence of DMSO were not significantly different compared to maximal relaxation responses to acetylcholine in the absence of DMSO [40.5% ± 4.6% (with DMSO) n = 7, 41.2% ± 4.3% (without DMSO) n = 6] (p = 0.920).
Effect of 3 h of incubation in normoglycemic, hyperglycemic and hyperglycemic conditions in the presence of serelaxin (10-8 M) on NO-mediated relaxation in the CC. Relaxation responses to acetylcholine were obtained in the presence of indomethacin (10-6 M). The number of strips in all groups: n = 7. Relaxation responses are expressed as a percentage of phenylephrine-induced contraction. Two-way ANOVA and the post hoc Bonferroni test were used in the comparison of groups. #p = 0.032 vs. normoglycemic conditions; *p = 0.021, p = 0.014, p = 0.042, p = 0.028, p = 0.035, and p = 0.016 for concentrations of 10−9 M, 10−8 M, 10−7 M, 10−6 M, 10−5 M, and 10−4 M, respectively, vs. hyperglycemic conditions.
Relaxation responses to iloprost at each concentration except 10−9 M were significantly decreased in the hyperglycemia group compared to the normoglycemia group, suggesting the possible impairment in iloprost-mediated relaxation due to hyperglycemia in the CC tissues (p = 0.054, p = 0.025, p = 0.025, and p = 0.047 for concentrations of 10−9 M, 10−8 M, 10−7 M, and 10−6 M, respectively) (Fig. 5). The pD2 values of iloprost were also significantly decreased in the hyperglycemia group compared to the normoglycemia group (p = 0.004) (Table 1). Iloprost-mediated relaxation responses were not changed at any dose in the hyperglycemia group in the presence of serelaxin compared to the hyperglycemia group (p = 0.434, p = 0.764, p = 0.747, and p = 0.425 for concentrations of 10−9 M, 10−8 M, 10−7 M, and 10−6 M, respectively) (Fig. 5). The pD2 values of iloprost were not different between the two groups (p = 0.974) (Table 1). Serelaxin was unable to normalize the effects of hyperglycemic conditions.
Effect of 3 h of incubation in normoglycemic, hyperglycemic and hyperglycemic conditions in the presence of serelaxin (10−8 M) on prostacyclin-mediated relaxation in the CC. Relaxation responses to iloprost were obtained. The number of strips in all groups: n = 7. Relaxation responses are expressed as a percentage of phenylephrine-induced contraction. Two-way ANOVA and the post hoc Bonferroni test were used in the comparison of groups. #p = 0.025, p = 0.025, and p = 0.047 for concentrations of 10−8 M, 10−7 M, and 10−6 M, respectively, vs. normoglycemic conditions.
Discussion
This study investigated the serelaxin-mediated relaxation responses in the CC and the effect of serelaxin on the endothelium-dependent relaxation responses via prostacyclin and NO under hyperglycemic conditions. Our data revealed that cumulative in vitro serelaxin administration did not cause a relaxation response in CC tissue. Hyperglycemia-induced endothelial dysfunction was demonstrated by a decrease in acetylcholine-mediated relaxation responses. Both NO- and prostacyclin-mediated relaxation responses were reduced under hyperglycemic conditions. Serelaxin did not lead to a change in prostacyclin-mediated responses but worsened the NO-mediated responses in hyperglycemic conditions.
The effects of relaxin and the mRNA expression of the relaxin receptor RXFP1 have been described in the male reproductive system. However, there is only one study investigating the effect of relaxin on erectile function. In this study, administration of relaxin-2 (0.4 mg/kg/day) with a subcutaneous micropump for 4 weeks improved erectile dysfunction caused by cavernous nerve damage [25]. There is no study evaluating the in vitro functional effects of relaxin on the CC. Relaxin-mediated relaxation and its effect on endothelium-dependent responses without the influence of hemodynamic changes have been studied in vessels. Mcguane et al. examined the relaxation effect of relaxin in different animal species and vascular beds. In their study, in vitro cumulative administration of serelaxin (10−6–10−4 M) caused dilation in the human subcutaneous artery and rat and mouse small renal arteries but not in rat mesenteric arteries [19]. Fisher et al. also reported that serelaxin caused a 66% maximal vasodilatation at 10−7 M in the small human gluteal resistance artery but had no effect on the small human pulmonary resistance artery [17]. In vitro serelaxin treatment induced rapid vasodilatation at low doses (10−10 M) in second- and third-order arterioles but not in fourth-order arterioles of hamster cremaster muscle [26]. In another study, a single dose of serelaxin (10−11 M) produced an approximately 50% vasodilator response in mouse mesenteric arteries [18]. In the present study, the relaxation responses of relaxin on CC were investigated with the cumulative addition of serelaxin. According to our data, serelaxin-mediated relaxation in CC tissue was not different from the time-dependent control, similar to the study of Leo et al. [27]. Studies examining relaxin-mediated relaxation in different animal species and vascular beds and our study indicate that the direct effect of serelaxin may vary in different species and even in different tissues of the same species.
Relaxin treatment for different durations has been shown to modulate endothelium-dependent responses by different mechanisms. In Leo et al.’s study, although the in vitro relaxant effect of serelaxin in the rat mesenteric artery was not demonstrated, serelaxin enhanced endothelium-dependent relaxation mediated by bradykinin in healthy rat mesenteric arteries after 3 and 24 h of intravenous injection [27]. In another study by the same researchers, serelaxin infusion for 48 h increased basal NOS activity and eNOS expression, while infusion for 72 h increased prostacyclin production in rat mesenteric arteries [28]. In vitro studies also showed that relaxin protected endothelium-dependent responses in pathologic conditions, as well as healthy conditions. Ng et al. evaluated the effects of serelaxin (10−8 M) on endothelium-dependent responses after a 3-day incubation period under in vitro hyperglycemic conditions in the mouse abdominal aorta. According to their results, coincubation of the mouse aorta with serelaxin improved endothelial dysfunction by ameliorating prostacyclin production [21]. In the present study, we also investigated the effects of serelaxin on endothelium-dependent relaxation via NO- and prostacyclin-mediated responses under hyperglycemic conditions. In contrast to Ng et al., we investigated the short-term effects of serelaxin. Prostacyclin synthesis is known to be decreased due to diabetes in rat penile tissue [29]. This decrease contributes to the endothelial dysfunction that occurs in diabetic conditions. In our study, we showed a decrease in prostacyclin-mediated relaxation responses under hyperglycemic conditions. Unlike Ng et al., in the present study, serelaxin did not ameliorate the reduced prostacyclin-mediated relaxation responses associated with hyperglycemia. We suggest that serelaxin might have a time-dependent effect on the CC, similar to the vessels. Ng et al. also showed that a 3-day serelaxin coincubation did not affect NO-dependent responses. According to their study, serelaxin did not restore the decreased basal NOS activity under hyperglycemic conditions in the mouse aorta [21]. On the other hand, a study indicated that decreased NO responses in rat aortic rings after 48 h of in vitro incubation with tumor necrosis factor-α (TNF-α) were ameliorated by relaxin-2 coincubation. In this study, relaxin-2 coincubation with TNF-α improved the reduced acetylcholine-mediated vasodilation and eNOS activity [20]. In the present study, we showed that short-term serelaxin coincubation further caused deterioration in NO-dependent responses under hyperglycemic conditions. Baccari et al. also evaluated the in vitro effect of relaxin on NO-dependent responses in a short-term period in healthy mouse colon smooth muscle. In this study, while in vitro exposure to relaxin for 10 min increased nNOSβ expression in the myenteric neurons in parallel with the decreased smooth muscle tone, 40 min of relaxin exposure was shown to decrease nNOSα and eNOS expression in smooth muscle, which led to an increase in mouse colon muscle contractions [30]. All these results and our data indicate that the effect of serelaxin on NO might be different according to treatment time.
There are some limitations in our study. First, we only evaluated the in vitro functional response to serelaxin in the CC. We did not evaluate relaxin receptor RXFP1 expression to support our findings regarding functional responses in vitro. Relaxin’s effects on NOS expression and activity have been demonstrated [20, 27, 28]. According to our results, serelaxin worsened NO-dependent responses under hyperglycemic conditions, but we did not investigate the activity or expression of NOS enzymes.
Conclusion
In summary, serelaxin did not induce a direct dose-dependent relaxation response in the CC however modulated endothelium-dependent responses. Under hyperglycemic conditions in which diabetes was mimicked, short-term in vitro serelaxin treatment worsened endothelial dysfunction by decreasing NO-mediated relaxation responses. The results of this study aimed to draw attention to the relationship between relaxin and penile tissue without the influence of hemodynamic changes. Serelaxin exerts different effects on endothelium-dependent responses depending on the dose and duration of exposure and long-term serelaxin treatment has been shown to prevent endothelial dysfunction. In this study, we demonstrated only the early in vitro effects of serelaxin in rat CC under hyperglycemic conditions. Therefore there are more issues that need to be clarified. Firstly the in vitro effect of relaxin needs to be confirmed in human penile tissue. Secondly, the proper timing and dosing of serelaxin administration in the penile tissue need to be demonstrated in diabetic animal models. If the beneficial effects of serelaxin on erectile function are demonstrated with long-term administration, there may be potential for this endogenous peptide hormone to be used in diabetic erectile dysfunction.
References
Lue TF, Takamura T, Schmidt RA, Palubinskas AJ, Tanagho EA. Hemodynamics of erection in the monkey. J Urol. 1983;130:1237–41.
Ignarro LJ, Bush PA, Buga GM, Wood KS, Fukuto JM, Rajfer J. Nitric oxide and cyclic GMP formation upon electrical field stimulation cause relaxation of corpus cavernosum smooth muscle. Biochem Biophys Res Commun. 1990;170:843–50.
Hurt KJ, Musicki B, Palese MA, Crone JK, Becker RE, Moriarity JL, et al. Akt-dependent phosphorylation of endothelial nitric-oxide synthase mediates penile erection. Proc Natl Acad Sci USA 2002;99:4061–6.
Jeremy JY, Morgan RJ, Mikhailidis DP, Dandona P. Prostacyclin synthesis by the corpora cavernosa of the human penis: evidence for muscarinic control and pathological implications. Prostaglandins Leukot Med. 1986;23:211–6.
Castela A, Gomes P, Domingues VF, Paíga P, Costa R, Vendeira P, et al. Role of oxidative stress-induced systemic and cavernosal molecular alterations in the progression of diabetic erectile dysfunction. J Diabetes. 2015;7:393–401.
Costa C, Soares R, Castela A, Adães S, Hastert V, Vendeira P, et al. Increased endothelial apoptotic cell density in human diabetic erectile tissue–comparison with clinical data. J Sex Med. 2009;6:826–35.
Guven H, Durmus N, Hocaoglu N, Guner O, Acar S, Akan P, et al. Protective effects of wheat germ oil against erectile and endothelial dysfunction in streptozotocin-induced diabetic rats. Int J Impot Res. 2022;34:581–7.
Hisaw FL. Experimental relaxation of the pubic ligament of the guinea pig. Proc Soc Exp Biol Med. 1926;23:661–3.
Wilkinson TN, Speed TP, Tregear GW, Bathgate RA. Evolution of the relaxin-like peptide family. BMC Evol Biol. 2005;5:14.
Kohsaka T, Hamano K, Sasada H, Watanabe S, Ogine T, Suzuki E, et al. Seminal immunoreactive relaxin in domestic animals and its relationship to sperm motility as a possible index for predicting the fertilizing ability of sires. Int J Androl. 2003;26:115–20.
Sasaki Y, Kohsaka T, Kawarasaki T, Sasada H, Ogine T, Bamba K, et al. Immunoreactive relaxin in seminal plasma of fertile boars and its correlation with sperm motility characteristics determined by computer‐assisted digital image analysis. Int J Androl. 2001;24:24–30.
Essig M, Schoenfeld C, D’Eletto RT, Amelar R, Steinetz BG, O’Byrne EM, et al. Relaxin in human seminal plasma. Ann NY Acad Sci. 1982;380:224–30.
Yki-Järvinen H, Wahlström T, Seppälä M. Immunohistochemical demonstration of relaxin in the genital tract of men. J Reprod Fertil. 1983;69:693–5.
Feng S, Agoulnik IU, Bogatcheva NV, Kamat AA, Kwabi-Addo B, Li R, et al. Relaxin promotes prostate cancer progression. Clin Cancer Res. 2007;13:1695–702.
Ferlin A, Menegazzo M, Gianesello L, Selice R, Foresta C. Effect of relaxin on human sperm functions. J Androl. 2012;33:474–82.
Gianesello L, Ferlin A, Menegazzo M, Pepe A, Foresta C. RXFP1 is expressed on the sperm acrosome, and relaxin stimulates the acrosomal reaction of human spermatozoa. Ann NY Acad Sci. 2009;1160:192–3.
Fisher C, MacLean M, Morecroft I, Seed A, Johnston F, Hillier C, et al. Is the pregnancy hormone relaxin also a vasodilator peptide secreted by the heart? Circulation. 2002;106:292–5.
Lian X, Beer-Hammer S, König GM, Kostenis E, Nürnberg B, Gollasch M. RXFP1 receptor activation by relaxin-2 induces vascular relaxation in mice via a Gαi2-protein/PI3Kß/γ/Nitric oxide-coupled pathway. Front Physiol. 2018;1234:1–13.
McGuane JT, Debrah JE, Sautina L, Jarajapu YP, Novak J, Rubin JP, et al. Relaxin induces rapid dilation of rodent small renal and human subcutaneous arteries via PI3 kinase and nitric oxide. Endocrinology. 2011;152:2786–96.
Dschietzig T, Brecht A, Bartsch C, Baumann G, Stangl K, Alexiou K. Relaxin improves TNF-α-induced endothelial dysfunction: the role of glucocorticoid receptor and phosphatidylinositol 3-kinase signalling. Cardiovasc Res. 2012;95:97–107.
Ng HH, Leo CH, Parry LJ. Serelaxin (recombinant human relaxin-2) prevents high glucose-induced endothelial dysfunction by ameliorating prostacyclin production in the mouse aorta. Pharmacol Res. 2016;107:220–8.
Boydens C, Pauwels B, Vanden Daele L, Van, de Voorde J. Protective effect of resveratrol and quercetin on in vitro-induced diabetic mouse corpus cavernosum. Cardiovasc Diabetol. 2016;15:46.
Kerstein MD, Saroyan M, McMullen-Laird M, Hyman AL, Kadowitz P, McNamara DB. Metabolism of prostaglandins in human saphenous vein. J Surg Res. 1983;35:91–100.
Bassiouni W, Daabees T, Louedec L, Norel X, Senbel A. Evaluation of some prostaglandins modulators on rat corpus cavernosum in-vitro: Is relaxation negatively affected by COX-inhibitors? Biomed Pharmacother. 2019;111:1458–66.
Liu K, Sun T, Xu W, Song J, Chen Y, Ruan Y, et al. Relaxin-2 prevents erectile dysfunction by cavernous nerve, endothelial and histopathological protection effects in rats with bilateral cavernous nerve injury. World J Mens Health. 2022. https://doi.org/10.5534/wjmh.220003. Online ahead of print.
Willcox JM, Summerlee A, Murrant CL. Relaxin induces rapid, transient vasodilation in the microcirculation of hamster skeletal muscle. J Endocrinol. 2013;218:179–91.
Leo CH, Jelinic M, Parkington HC, Tare M, Parry LJ. Acute intravenous injection of serelaxin (recombinant human relaxin‐2) causes rapid and sustained bradykinin‐mediated vasorelaxation. J Am Heart Assoc. 2014;3:e000493.
Leo C, Jelinic M, Ng H, Tare M, Parry L. Time‐dependent activation of prostacyclin and nitric oxide pathways during continuous iv infusion of serelaxin (recombinant human H2 relaxin). Br J Pharmacol. 2016;173:1005–17.
Jeremy JY, Thompson CS, Mikhailidis DP, Dandona P. Experimental diabetes mellitus inhibits prostacyclin synthesis by the rat penis: pathological implications. Diabetologia. 1985;28:365–8.
Baccari MC, Traini C, Garella R, Cipriani G, Vannucchi MG. Relaxin exerts two opposite effects on mechanical activity and nitric oxide synthase expression in the mouse colon. Am J Physiol Endocrinol Metab. 2012;303:E1142–50.
Acknowledgements
This project was funded by Dokuz Eylül University Scientific Research Projects Coordination Unit (2018.KB.SAG.065).
Author information
Authors and Affiliations
Contributions
ND designed the study. SAS and OG conducted the experiments. SAS and ND did the analysis. SAS, ND, TKT and MA interpreted the data and drafted the manuscript. ND obtained the funding and did supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Animal Care and Investigational Committee of Dokuz Eylül University (02/2020).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Acar-Sahan, S., Guner, O., Ates, M. et al. In vitro effect of relaxin in the rat corpus cavernosum under hyperglycemic and normoglycemic conditions. Int J Impot Res 36, 72–77 (2024). https://doi.org/10.1038/s41443-022-00653-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-022-00653-6
- Springer Nature Limited
This article is cited by
-
Identification of potential biomarkers for atrial fibrillation and stable coronary artery disease based on WGCNA and machine algorithms
BMC Cardiovascular Disorders (2024)