Abstract
Intracavernosal injection therapy (ICI) was the first pharmacologic treatment in the management of erectile dysfunction. ICI allows for customization of medication composition and concentrations, making it a highly effective treatment with an acceptable side effect profile. The objective was to investigate the long-term results of ICI using validated and non-validated instruments. This is a retrospective, single-institution study of 105 patients (mean age 61.6 ± 11.1) patients using ICI. Mean duration of ICI was 8.4 ± 6.25 years. Pre- and post-treatment patient-reported penile rigidity were 41.1% ± 29.3 and 89.6% ± 13.6, respectively (p < 0.05). Statistical changes were also found in the pre and post International Index of Erectile Function (IIEF) scores (33.0 ± 14.4 and 60.0 ± 12.7, p < 0.05), erectile function (11.5 ± 1.3 and 27.3 ± 0.9, p < 0.05) and satisfaction domains (5.3 ± 1.5 and 8.1 ± 1.1, p < 0.05) of the IIEF. There were no statistical differences in questionnaire outcomes between difficult to treat patients (diabetes or radical prostatectomy) and the remainder of queried patients. Complications were rare and included priapism (7.1%), penile curvature (10%; <30°), bruising (7.6%), and mild penile pain (12.4%). Overall, ICI therapy is safe and effective, and compliance may be augmented by patient education, dosing customization, and cost reduction.
Similar content being viewed by others
Introduction
Intracavernosal injection therapy (ICI) has proven to be one of the most effective local pharmacological treatments for erectile dysfunction (ED). Combinations of multiple vasoactive drugs acting synergistically through different pathways have increased the efficacy rate of ICI to nearly 90% and allowed for customization of therapy while minimizing complications [1,2,3]. High discontinuation rates, ranging from 30–80%, are still notable. Studies have attributed it to patient/partner acceptance, adverse effects, and cost [4]. A large, prospective, multi-institutional study, however, reported lower dropout rates (31% over 6 months) with close monitoring and access to free medication [5].
The introduction of phosphodiesterase type 5 (PDE5) inhibitors has decreased the need for second-line management with intracavernosal therapy. However, PDE5 inhibitors are ineffective in 25–32% of patients, which may be due to underlying risk factors such as diabetes, clinically significant vascular disease, or a history of radical prostatectomy [6]. ICI may be effective in many patients, who have failed PDE5 inhibitors. Our institution has employed a customized and patient-centered approach. This consists of a psychological assessment, the use of a highly-trained sexual medicine physician assistant (PA), precise titration of drug mixtures to match a patient’s needs, comprehensive patient education, and a working relationship with a high-volume compounding pharmacy. This carefully formulated approach has resulted in high efficacy and satisfaction. The aim of this study is to investigate the long-term results of intracavernosal therapy using validated and non-validated sexual questionnaires.
Materials and methods
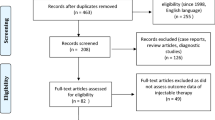
This is a retrospective, single institution, IRB-exempt (H-26793) study of patients on ICI therapy. A 12-page questionnaire including validated [International Index of Erectile Function (IIEF), Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS)], and non-validated questionnaires were completed by 105 patients (mean age 55.1 ± 13.9 years) in the office.
The study further evaluated three cohorts of particular interest: those using ICI for >10 years (mean follow up of 15 years) and those considered to be “difficult to treat” (diabetics and patients status post radical prostatectomy). Pre- and post-treatment measures were asked at the time of survey, relying on patients to recall and assess their initial baseline symptoms.
All patients had previously undergone a thorough medical evaluation including a detailed history, psychological analysis by a licensed sexual therapist, and a physical exam by both a sexual medicine PA and physician. In addition, all patients underwent hemodynamic testing with penile duplex Doppler ultrasound after intracavernosal injection of trimix medication (phentolamine, papaverine, alprostadil) to determine erectile response. All patients had either arteriogenic, mixed arteriogenic and veno-occlusive, or neurogenic dysfunction. Fourteen different mixtures of vasoactive agents were available to patients and appropriate dosing was determined by the physician and titrated to effective doses by the patient with guidance (Fig. 1). If a patient did not respond adequately to the initial injection, redosing would be performed at this time (Fig. 2). Home dosing was determined via an algorithm, illustrated in Fig. 2. Training in administration of the medication was performed by the PA. Patients are evaluated 2 months after their initial training to assess for proper technique, efficacy, satisfaction, and any adverse events. Annual follow up would ensure if the regimen is deemed effective (Fig. 2).
Statistical analysis included the calculation of means and standard deviations for all pertinent data points. Statistically significant improvement in erectile function was assessed with a two-tailed paired t-test to compare the pre- and post-treatment instrument score means, and using a two-tailed unequal variance t-test to compare different patient groups.
Results
Validated sexual questionnaires
Validated questionnaire outcomes data are summarized in Table 1. Pre- and post-treatment IIEF erectile function domain score, IIEF question 3 (ability to achieve penetration during intercourse), and IIEF question 4 (ability to maintain an erection during penetrative intercourse) were statistically significant (p < 0.01). EDITS score was 83.0 out of a possible 100.
Non-validated sexual questionnaires
Pre- and post-treatment patient reported penile rigidity was 41% ± 29.3 and 90% ± 13.6, respectively (p < 0.05). Treatment satisfaction by patient report was 88%, and 94% would recommend this treatment to other patients. The non-validated questionnaire used is depicted in Fig. 3.
Difficult to treat patients
Validated questionnaire outcomes are summarized in Table 2. Of the 105 patients, 10 carried a diagnosis of diabetes mellitus, and 23 patients had previously undergone a radical prostatectomy. There were no statistically significant differences in IIEF, Center for Epidemiological Studies Depression Scale (CES-D) and EDITS scores between difficult to treat patients (diabetes or radical prostatectomy) and the remainder of queried patients (Table 2).
Long-term users (>10 years)
A total of 40/105 patients had used ICI therapy for more than 10 years. The mean length of treatment was 15 years (range 10–25 years) and 8/40 patients had used ICI for 20+ years. Average duration of erection was 69 min ± 52 min, and 78% of patients reported penile rigidity at or greater than 90% with ICI. Patients reported using ICI 4.4 times per month on average. Of long-term users, 85% reported performing the injection alone, without the presence of a partner. Interestingly, 63% of the 40 patients were responsive to PDE-5 inhibitors, but chose to continue using ICI due to better penile rigidity, fewer side effects, and decreased cost of therapy. Pre- and post-treatment IIEF erectile function domain (questions 1, 2, 3, 4, 5, and 15), overall treatment satisfaction domain (questions 13 and 14), question 3 alone, and question 4 alone were statistically significant (p < 0.01) (Table 3). These patients reported no major complications with ICI therapy. However, 18% (n = 7) reported some degree of scarring or penile plaque, 10% (n = 4) reported pain with injections and one patient reported headache.
Reasons for use
Interestingly, in the entire study cohort, 54% used ICI despite acceptable responses to PDE5 inhibitors. When asked why they chose ICI instead of oral therapies, 79% (45/57) stated that they had better results with ICI, 39% (22/57) reported fewer side effects, and 18% (10/57) indicated that ICI was less expensive than oral medication (total adds to >100% as patients were able to choose more than one response).
Complications
Eighty-four percent of patients reported no complications. Of the 17 patients reporting complications, they reported: plaque or scar formation (n = 11, 10%), pain (n = 2, 2%), bruising (n = 1, <1%), irritability (n = 1, <1%), headache (n = 1, <1%), and “tissue damage” (n = 1, <1%).
Patients were also specifically asked about various outcomes including loss of length and penile curvature. Twenty-seven percent of patients reported a loss of penile length, and 20% reported development of penile curvature. Those who experienced loss of penile length subjectively reported an average loss of 1.44 in. Of those who reported loss of length or new penile curvature, none were diabetics. When comparing postprostatectomy patients and long-term users to those without these characteristics, loss of length was seen in 34.8% of postprostatectomy patients and 22.5% of long-term users, compared with 21.1% of the control group (p-values 0.24 and 0.88, respectively). Similarly, new penile curvature was seen in 26.1% of postprostatectomy patients and 15.0% of long-term users, compared with 21.1% of the control group (p-values 0.66 and 0.49, respectively). No statistically significant differences were determined with regards to either loss of length or new penile curvature among postprostatectomy patients and long-term users compared with those without these qualities. A total of 7.1% of patients reported at least one episode of priapism that required alpha-agonist therapy. Penile pain was reported by 12% of patients, and was rated as mild, 2.4 ± 1.07, on a subjective pain scale of 1–10 (1 = no pain, 10 = severe pain).
Discussion
There have been several cohort studies examining the use of intracavernosal injections for erectile dysfunction. The number of patients queried, use of validated instruments (IIEF and EDITS), and length of mean follow-up time (15 years) are strengths of the present study, aiding our understanding of patient experiences with long-term ICI therapy. We found that patients continuing ICI are very satisfied, report little pain and have few complications related to therapy. In addition, ICI is effective for patients with significant risk factors for ED including radical prostatectomy and diabetes.
Many of the included patients used intracavernosal therapy before PDE-5 inhibitors became available in 1998. A number of these patients chose to continue ICI despite responses to PDE5 inhibitors, citing better penile rigidity, fewer side effects, and lower cost. These findings were similar to those reported in the prospective study by Kim et al. in which participants on ICI therapy were temporarily switched to oral therapy. Despite adequate response to oral therapy, many elected to continue ICI as the erections were more rapid, reliable, and of better quality [7]. In 2007, Mulhall and Simmons conducted a study of 178 patients comparing ICI therapy with sildenafil. Mean IIEF and EDITS scores for ICI patients (66 ± 5 and 67 ± 8) were similar to this study’s (60.0 ± 10.95 and 83.0 ± 16.4), suggesting higher efficacy and satisfaction rates in ICI treatment patients versus sildenafil users [8]. In agreement with these results, Kucuk et al. retrospectively evaluated 356 men with ED and also found that there was a higher improvement in IIEF scores in the ICI group compared with those taking oral PDE5 inhibitors [9]. Alexandre et al. reported a satisfaction rate of 78% with ICI therapy, which is similar to our rate of 88% [10]. In addition, they found that 86% would recommend the therapy to friends, comparable with 94% in this current study. Coombs et al. reported high satisfaction, but lower efficacy of ICI in diabetic patients compared with nondiabetic patients [11]. While our cohort consisted of fewer diabetic patients than Coombs’ group, they did share a similar efficacy as their euglycemic counterparts. Our study suggests that ICI therapy is highly effective in three special cohorts: long-term users (>10 years), diabetics, and those who have undergone radical prostatectomy. There were no statistically significant differences in IIEF, CES-D, and EDITS scores between these patient cohorts and the rest of the patients.
Utilizing duplex Doppler ultrasound aids in counseling of these patients by demonstrating the proper techniques of ICI. From the clinical standpoint, knowing how a patient responds to standard solutions helps to further tailor their injections for home use. However, perhaps equally as important, a patient is exposed to the minor discomfort of the injection and the subsequent erection in a controlled clinical setting, such that apprehension for at home self-injection is alleviated. Other studies have revealed high discontinuation rates in part due to the negative conception of the treatment modality [12,13,14,15,16]. In our clinic, patients are dosed with one or both of two standard trimix solutions in attempt to provide a rigid erection for evaluation by ultrasound [17]. Many patients who are initially unenthusiastic about injection therapy are more open to trying it after experiencing the injection in clinic. In a study by Albaugh and Ferrans, 40% of men reported no pain with injection and 65% reported no pain with the medication itself [18]. Twenty percent of patients in this study reported no pain with injections, and the average pain rating was 2.3 on a 1–10 scale. In our clinic, if patients experience PGE1-induced penile pain, their trimix prescription will be modified to lower the concentration of PGE1, as proposed by Goldstein et al. in 1990 [3].
Rates of dropout have ranged from 24 to 80% in previous studies, and the current study did not address attrition or predictors of the same [4, 11,12,13,14,15,16, 19]. According to Coombs’, one of the greatest predictors of failure was trimix dose over 50 units [11]. In our clinic, we attempt to decrease the volume of injected solution by switching patients to more potent mixtures as their ED worsens over time. In this way, we hoped to reduce the rate of dropout as well, but we did not specifically investigate that outcome as part of this study.
Complications and adverse events were rare and mild despite some patients self-injecting an estimated 960 times over 20 years. A total of 7.1% of patients reported at least one episode of priapism (defined as a painful full erection that lasted over 4 h). Incidence of penile curvature as reported by patients was ~20%, which is somewhat higher than the estimated incidence of Peyronie’s disease (PD) in the general population, ~3–9% [20]. However, this patient population, by virtue of their erectile dysfunction, is already at higher risk of the disease if one accepts vascular compromise, diabetes, and age to be risk factors for developing PD [21, 22]. Unfortunately, degree of curvature was not reported or measured in this cohort. Interestingly, when patients were asked, only 16% reported a complication. However, specific questions regarding priapism, loss of length, pain, and curvature resulted in more positive responses. It is possible that patients did not view these outcomes as complications or adverse events, but simply side effects of treatment, which again emphasizes the importance of patient counseling and of setting reasonable expectations.
PDE5 inhibitors continue to be used as first line therapy for patients with ED. For patients who failed oral therapy due to lack of efficacy or who cannot tolerate the side effects (dyspepsia, headaches, allergies, etc.), intracavernosal injections present a viable alternative. This study not only documents durable efficacy and high satisfaction rates but also an acceptable side effect profile. The high rates of satisfaction appreciated in this study may be attributed to the framework of support provided in our clinic, which specializes in men’s health.
This study was limited by its retrospective nature. As patients were asked about pre- and post-treatment measures concurrently at the time of survey, including those who initiated treatment more than 10 years prior, there is potential for recall bias. Moreover, while the study did characterize patients’ complication rates, it did not record the rates of discontinuation or patient rationale for discontinuation. Therefore, predictive patient factors that may contribute to long term use were not determined. However, we theorize that a patient-centered approach of counseling, patient/partner education, and close follow-up will minimize discontinuation rates and improve satisfaction. Furthermore, anecdotal experience in the clinic has shown that patients who tend to continue injection therapy are those that experience treatment effect for ~30–60 min at low doses without prostaglandin E1-induced pain. Other patient factors include those who have good manual dexterity as well as insulin-dependent diabetics as they are comfortable with needles. Finally, race may play a role. Again, based solely on anecdotal experience, Hispanic White men have been more likely to pursue placement of a penile prosthesis compared with non-Hispanic White men who may be more conservative in their treatments. Yearly visits are critical to monitor efficacy and modify the regimen as the patient ages and potentially develops additional comorbid conditions. A prospective study would provide accurate data regarding discontinuation rates and positive management strategies.
Conclusions
Intracavernosal therapy is a highly effective and safe treatment option for patients with ED. It is associated with high satisfaction rates and acceptable side effects. ICI’s strength as a treatment modality may be improved by thorough, ongoing patient education as well as regimented follow-ups. Compliance may be augmented by dosing customization, cost reduction, in addition to improving the drug’s availability. A prospective study will help us to better understand dropout rates and further develop a “patient-centered” approach.
References
Virag R, Becher E, Carrier S, Jardin A, Wagner G. Local pharmacological treatment modalities. In: Jardin A, Wagner G, Khoury S, editors. Erectile dysfunction. Plymouth: Health Publication Ltd; 2000. p. 305–54.
Richter S, Vardi Y, Ringel A, Shalev M, Nissenkorn I. Intracavernous injections: still the gold standard for treatment of erectile dysfunction in elderly men. Int J Impot Res. 2001;13:172–5.
Goldstein I, Borges F, Fitch W, Kaufman J, Damron K, Moreno J. Rescuing the failed papaverine phentolamine erection: a proposed synergistic action of papaverine phentolamine and prostaglandin E1. J Urol. 1990;143:304A.
Mulhall JP, Jahoda AE, Cairney M, Goldstein B, Leitzes R, Woods J, et al. The causes of patient dropout from penile self-injection therapy for impotence. J Urol. 1999;162:1291–4.
Linet OI, Ogrinc FG. Efficacy and safety of intracavernosal alprostadil in men with erectile dysfunction. The Alprostadil Study Group. N Engl J Med. 1996;334:873–7.
Eardley I, Donatucci C, Corbin J, El-Meliegy A, Hatzimouratidis K, McVary K, et al. Pharmacotherapy for erectile dysfunction. J Sex Med. 2010;7:524–40.
Kim SC, Chang IH, Jeon HJ. Preference for oral sildenafil or intracavernosal injection in patients with erectile dysfunction already using intracavernosal injection for >1 year. BJU Int. 2003;92:277–80.
Mulhall JP, Simmons J. Assessment of comparative treatment satisfaction with sildenafil citrate and penile injection therapy in patients responding to both. BJU Int. 2007;100:1313–6.
Kucuk EV, Tahra A, Bindayi A, Onol FF. Erectile dysfunction patients are more satisfied with penile prosthesis implantation compared with tadalafil and intracavernosal injection treatments. Andrology. 2016;4:952–6.
Alexandre B, Lemaire A, Desvaux P, Amar E. Intracavernous injections of prostaglandin E1 for erectile dysfunction: patient satisfaction and quality of sex life on long-term treatment. J Sex Med. 2007;4:426–31.
Coombs PG, Heck M, Guhring P, Narus J, Mulhall JP. A review of outcomes of an intracavernosal injection therapy programme. BJU Int. 2012;110:1787–91.
Nelson C, Hsiao W, Balk E, Narus J, Tal R, Bennett N, et al. Injection anxiety and pain in men using intracavernosal injection therapy after radical pelvic surgery. J Sex Med. 2013;10:2559–65.
Weiss JN, Badlani GH, Ravalli R, Brettschneider N. Reasons for high drop-out rate with self-injection therapy for impotence. Int J Impot Res. 1994;6:171–4.
Althof SE, Turner LA, Levine SB, Risen C, Kursh E, Bodner D, et al. Why do so many people drop out from auto-injection therapy for impotence? J Sex Marital Ther. 1989;15:121–9.
Sundaram CP, Thomas W, Pryor LE, Ami Sidi A, Billups K, Pryor JL. Long-term follow-up of patients receiving injection therapy for erectile dysfunction. Urology. 1997;49:932–5.
Sung HH, Ahn JS, Kim JJ, Choo SH, Han DH, Lee SW. The role of intracavernosal injection therapy and the reasons of withdrawal from therapy in patients with erectile dysfunction in the era of PDE5 inhibitors. Andrology. 2014;2:45–50.
Mulhall JP, Abdel-Moneim A, Abobakr R, Goldstein I. Improving the accuracy of vascular testing in impotent men: correcting hemodynamic alterations using a vasoactive medication re-dosing schedule. J Urol. 2001;166:923–6.
Albaugh J, Ferrans CE. Patient-reported pain with initial intracavernosal injection. J Sex Med. 2009;6:513–9.
Hsiao W, Bennett N, Guhring P, Narus J, Mulhall JP. Satisfaction profiles in men using intracavernosal injection therapy. J Sex Med. 2011;8:512–7.
Pryor JP, Ralph DJ. Clinical presentations of Peyronie’ s disease. Int J Impot Res. 2002;14:414–7.
LaRochelle JC, Levine LA. A survey of primary-care physicians and urologists regarding Peyronie’s disease. J Sex Med. 2007;4:1167–73.
Kadioglu A, Sanli O, Akman T, Canguven O, Aydin M, Akbulut F, et al. Factors affecting the degree of penile deformity in peyronie disease: an analysis of 1001 patients. J Androl. 2011;32:502–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Ricardo Munarriz is a consultant for Coloplast. Kevin O’Brien plans to attend an internship with Pfizer.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bearelly, P., Phillips, E.A., Pan, S. et al. Long-term intracavernosal injection therapy: treatment efficacy and patient satisfaction. Int J Impot Res 32, 345–351 (2020). https://doi.org/10.1038/s41443-019-0186-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0186-z
- Springer Nature Limited
This article is cited by
-
Conservative Non-surgical Options for Erectile Dysfunction
Current Urology Reports (2023)