Abstract
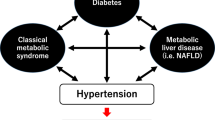
This review article introduces some basic studies that were recently published in this journal, as a part of Hypertension Research 2024 Update and Perspectives. Including recent basic research trends in other scientific journals, we would like to summarize basic research on keywords such as hypertension and its associated organ damage, new treatments, and others. It is expected that the accumulation of basic studies will lead to breakthroughs in hypertension treatment in the future and lead to the definitive treatment of hypertension beyond blood pressure control with anti-hypertensive drugs.

Similar content being viewed by others
As a part of Hypertension Research 2024 Update and Perspectives, this review focuses on and introduces some basic studies recently published in Hypertension Research with related articles in light of recent research trends in other research journals as well. This author apologizes for not being able to introduce all of the basic studies recently published in Hypertension Research, but there are many interesting and important articles regarding basic research that cannot be introduced here. We urge potential readers to check original articles in Hypertension Research, that are not picked up, as well.
Piezo ion channels and renal injury associated with hypertension
Blood flow exerts mechanical forces on tissues and cells. Thus, the cells have a system for sensing these mechanical stimuli. Piezo ion channels, which are known to sense mechanical stimuli and induce Ca2 influx into cells, not only work just as a sensor for mechanical stimuli but also transduce hemodynamic forces in vascular cells [1,2,3]. It has been reported that Piezo also has various biological functions such as red blood cell homeostasis and platelet aggregation [1]. Recent studies have shown that Piezo1, as a mechanosensory, regulates lymphatic vessel growth in response to external physical stimuli, works as a mechanosensor of capillaries and regulates blood flow in the central nervous system, and senses mechanical stimuli also in muscle capillaries and its dysfunction induces muscle atrophy [4,5,6,7]. Other recent findings are that Piezo1 agonists restore brain-cerebrospinal fluid perfusion in aged mice and that Piezo1, as a mechanosensory, regulates urinary potassium excretion in the distal nephron of the kidney [8, 9]. Regarding tissue injury, a recent study reported that macrophage-specific Piezo1-knockout mice exhibit suppression of renal fibrosis in unilateral ureteral obstruction or folic acid-induced renal fibrosis model [10]. As shown in these reports, Piezo is an important molecule that is attracting attention as various new functions have been discovered recently.
Nagase’s group has published two Piezo-related studies in Hypertension Research [11, 12]. They found that Piezo1 expression is upregulated in podocytes, mesangial cells, and distal tubular cells in mice with an aldosterone/salt-induced renal injury model, which exhibits hypertension, albuminuria, podocyte damage, and glomerular damage [11]. In this study, they also found that mechanical stimulation increases the markers of podocyte damage and the changes in markers are suppressed by Piezo1 blockade in Piezo1-expressed cultured podocytes [11]. These findings suggest that Piezo1 is involved in the mechanical stimulation-associated podocyte injury. In the study using Dahl salt-sensitive hypertensive rats, Piezo2 expression in mesangial cells and renin1-positive cells was increased in high salt-fed rats that exhibit hypertension and renal injury compared with normal salt-fed rats [12]. Furthermore, they also found that Piezo2 negatively regulates transforming growth factor-b1 expression, suggesting that changes in Piezo2 expression may be associated with renal injury in salt-sensitive hypertension [12]. These studies suggest that Piezo ion channels could be novel basic research and therapeutic targets for hypertensive kidney injury. As hypertension, as the name implies, exerts “pressure” on cells and tissues, basic research regarding blood pressure and Piezo would be important.
Immune cells associated with hypertension
Immune cells are known to be involved in the pathophysiology of hypertension and its associated tissue injury [13]. New findings in basic research related to immune cells have also been published in Hypertension Research.
It has been reported that Jumonji domain containing (JMJD) 3 regulates tissue inflammation and fibrosis [14,15,16], and Gao et al. examined the roles of bone marrow cells/JMJD3 in the development of deoxycorticosterone acetate (DOCA), a mineralocorticoid receptor agonist, /salt-induced hypertension model [17]. They first identified that DOCA/salt increases JMJD3 expressions in CD45-positive cells in the renal interstitium [17]. Bone marrow cell-specific JMJD3-deficient mice did not alter DOCA/salt-induced high blood pressure, but significantly attenuated histological damage, inflammation, and fibrosis in the kidney coupled with reductions in blood urea nitrogen and albuminuria compared with wild-type mice [17]. These results suggest that JMJD3 in bone marrow cells is a novel therapeutic target for renal injury associated with mineralocorticoid receptor-associated salt-sensitive hypertension.
It is well known that T cells contribute to the development of hypertension and its associated tissue injury [18]. Of note, high salt intake induces T helper (Th) 17 cells and elevates blood pressure [19]. Kim et al. examined the difference in Th 17 cells between Dahl salt-sensitive and salt-resistant rats regarding the development of salt-sensitive hypertension [20]. In the cultured T cells derived from the spleen, hypertonic salt solution induced more Th17 cells in Dahl salt-sensitive rats than salt-resistant rats [20]. Also, high salt intake significantly increased blood pressure, serum interleukin (IL)-17a levels, and Th17 cell polarization in Dahl salt-sensitive rats but not salt-resistant rats [20]. These results suggest that differences in sensitivity or polarity changes of T cells to salt are a key mechanism of the development of hypertension. However, Kim et al focused on only the differences in Th 17 cells and did not perform any intervention for that [20].
Many basic studies have reported that immune cells contribute to the development of hypertension and its associated organ damage including the above studies. However, various basic research has not yet led to specific treatment methods for hypertensive patients. On the other hand, recent T-cell-related research topics have focused on chimeric antigen receptor (CAR) T-cells in the treatment of cancer, inflammation, and cardiac injury [21,22,23,24,25]. In this approach, T cells are once collected from the patient, and then reprogrammed and back into the patient to induce specific functions of Car T-cells for treatment [26]. What is important in the future would be the development of specific ways of regulating immune cells and treating hypertension and organ damage, like CAR T-cell therapy.
Hypertension and its associated organ damage
Tamura’s group has been studying the roles of angiotensin II type-I (AT1) receptor-associated protein (ATRAP), an endogenous protein that suppresses excessive activation of AT1 receptors by promoting receptor internalization, in the development of hypertension and organ damage [27]. The renin-angiotensin system and sympathetic nervous system in the brain are involved in the development of hypertension, and Sotozawa et al. examined angiotensin II-induced blood pressure elevation in rats with ATRAP-overexpression of the paraventricular hypothalamic nucleus (PVN), which is an important site for sympathetic nervous system regulation in the brain [28, 29]. The ATRAP/AT1 receptor expression ratio in PVN was significantly decreased in angiotensin II-induced hypertensive rats, and they induced ATRAP-overexpression in PVN of rats by administering an ATRAP-expressing lentivirus [29]. In the PVN-ATRAP-overexpressed rats, angiotensin II-induced high blood pressure and cardiac hypertrophy were significantly attenuated, and these changes were associated with a reduction in urinary adrenaline excretion [29]. These findings suggest that ATRAP in PVN is a new target for angiotensin II-associated hypertension. The group also reported another finding in Hypertension Research that ATRAP deficiency combined with angiotensin II infusion can enhance diabetic kidney injury in the C57BL/6 strain mouse, which is resistant to the development of kidney injury [30].
It has focused on the contribution of the vascular transient receptor potential vanilloid (TRPV) 4 channels to hypertension and organ damage. For example, a recent study reported that smooth muscle cell-specific TRPV4-deletion suppresses the enhanced vasoconstriction and increase in blood pressure in diet-induced obesity model mice [31]. Not only vascular smooth muscle cells, but also endothelial cell-specific TRPV4-deficient mice also exhibited attenuation of cardiac dysfunction and fibrosis in pressure-overload transverse aortic constriction (TAC) model mice [32]. In Hypertension Research, Wen et al. examined the effects of vascular TRPV4 channels on high salt-induced blood pressure [33]. Endothelial cell-specific TRPV4-deficient mice showed partial suppression of increase in blood pressure by high salt intake compared with wild-type mice [33]. This partial suppression is because TRPV4 in vascular smooth muscle cells, as well as endothelial cells, also regulates vascular tone [33]. Indeed, they demonstrated that TRPV4-mediated intracellular Ca2+ influx/interferon regulatory factor 7/inositol trisphosphate receptor 2 axis induces vasoconstriction in vascular smooth muscle cells by using isolated aorta and cultured vascular smooth muscle cells, which could contribute to the increase in blood pressure during high salt intake [33]. TRPV4 in both vascular endothelial cells and smooth muscle cells could be a new therapeutic target for hypertension. Although it is not directly associated with hypertension, another new finding regarding TRPV4 is that TRPV4 in microglia, the macrophages of the central nervous system, may become a novel target for the treatment of chronic pain [34].
Pericytes, which cover capillaries, are the cells that play important roles in vascular homeostasis such as structure stability, blood flow, and permeability. Although it is known that the heart has abundant pericytes, recent research has reported several roles for cardiac pericytes and focus. Regarding new findings in cardiac pericytes, recent studies showed that cardiac pericytes are involved in arteriogenesis and angiogenesis in the ischemic heart [35] and regulate cardiac remodeling after myocardial infarction [36, 37]. On the other hand, congestive heart failure leads to body fluid overload and an increase in venous pressure, resulting in renal congestion and its associated renal injury. It has been reported that renal injury induces pericyte detachment from the capillaries and pericyte-myofibroblast transition, which contributes to renal fibrosis [38, 39]. In Hypertension Research, Ito et al. reported the pericyte detachment during a renal injury in renal congestion model rats [40]. They used high salt-fed Dahl salt-sensitive rats, which exhibit renal congestion, and evaluated the right kidney as a model of renal congestion while the left kidney was decapsulated to reduce the renal interstitial hydrostatic pressure [40]. The right kidney of high salt-fed Dahl salt-sensitive rats showed renal tubulointerstitial injury and pericyte detachment from the vascular wall [40]. In the left kidney with attenuated interstitial hydrostatic pressure, the tissue damage was ameliorated. Pericyte detachment from the vascular wall was also observed in human renal tissue from patients with heart failure patients [40]. These findings suggest that pericyte detachment associated with an increase in interstitial hydrostatic pressure is one of the key factors during the development of renal injury and fibrosis. Also, renal congestion and subsequent pathophysiological alternations could be therapeutic targets for renal injury associated with heart failure.
Beyond oral administration
Although various antihypertensive drugs have been developed and blood pressure control in hypertensive patients has improved, there are still patients with refractory hypertension. Even if blood pressure can be well controlled with antihypertensive drugs, patients need to keep taking oral medications every day, therefore, there are medication adherence issues. To solve these issues regarding hypertensive therapy, it is important to study novel hypertension treatments and therapeutics, and several basic studies challenging these issues were published in Hypertension Research.
While novel antihypertensive treatments such as renal denervation which targets the nervous system have received much attention, Dai et al. examined the antihypertensive effects of celiac ganglia neurolysis (CGN) in spontaneously hypertensive rat (SHR) and Dahl salt-sensitive rat [41]. CGN significantly decreased blood pressure in SHRs and high salt-fed Dahl salt-sensitive rats, and these antihypertensive effects of CGN were associated with inhibition of the renin-angiotensin-aldosterone system and an increase in nitric oxide [41]. This basic study indicates that CGN, like renal denervation, may be effective in the treatment of refractory hypertension. Of note, since CGN is also effective in pain relief, it is expected that CGN would be applied to the treatment of hypertension in patients who require pain relief, such as abdominal disease and cancer [42].
It is well known the association between the adrenal gland and blood pressure [43]. For instance, the removal of the adrenal gland is used in the treatment of primary aldosteronism. Wang et al. have examined the possibility that unilateral chemical ablation of the adrenal gland is effective in the treatment of hypertension other than primary aldosteronism [44]. They performed unilateral adrenal ablation in SHR and normotensive Wistar Kyoto rat (WKY) by anhydrous ethanol injection [44]. Adrenal ablation significantly reduced blood pressure in SHRs, and this reduction in blood pressure was associated with suppressions in renin, angiotensin, aldosterone, noradrenaline, and adrenaline levels. On the other hand, adrenal ablation did not affect blood pressure or these hormones in WKYs. Adrenal ablation also attenuated cardiac, renal, and vascular injury in SHRs [44]. Although further studies are required to determine how adrenal ablation can be applied to hypertensive patients other than primary aldosteronism, further basic research is expected, which targets adrenal function for blood pressure control including the development of aldosterone synthase inhibitors [45].
While vaccines are important in the research field of infection, their potential in the cardiovascular and cancer research fields is also attracting attention [46, 47]. For example, a recent study reported that administration of a peptide vaccine targeting ADAMTS-7 (a disintegrin and metalloproteinase with thrombospondin type 1 motif 7), which is associated with human coronary atherosclerosis, alleviated intimal thickening in a carotid artery ligation model mice, neointimal formation in a wire injury model mice, and atherosclerosis in both hyperlipidemic ApoE- and LDLR-deficient mice [48]. The development of vaccines has also received attention in the research field of hypertension, with Ke et al. reporting the efficacy of a vaccine targeting the adrenergic β1 receptor (β1-AR) [49]. β receptors play an important role in the pathogenesis of hypertension and chronic heart failure, and they developed a vaccine targeting β1-AR [49]. They evaluated its efficacy in NG-nitro-L-arginine methyl ester (L-NAME), a nitric oxide synthase inhibitor, -induced hypertensive rats, TAC, and myocardial infarction (MI) model mice [49]. In the L-NAME-treated model, the β1-AR vaccine significantly decreased blood pressure and attenuated cardiovascular injury [49]. The β1-AR vaccine also improved cardiac function and cardiovascular injury in both TAC and MI model mice [49]. These findings suggest that the development of novel vaccines that block existing therapeutic targets may improve medication adherence and treatment regarding hypertension and heart failure.
A typical oral antihypertensive agent is a calcium channel blocker, and Jana et al. have developed a nifedipine formulation using polymeric dissolving microneedles (DMNs) patch [50]. They showed that this DMNs patch can provide a steady and sustained release of 96% of the drug for up to 48-72 hours without loss of nifedipine [50]. This kind of drug delivery system would have various possible advantages for long-term therapy such as improvements in treatment compliance and adherence associated with a decrease in daily dosing frequency. The novel drug delivery system may also solve some issues of various existing drugs as well as nifedipine. In addition, since nifedipine is effective not only in hypertension but also in angina pectoris, pre-eclampsia, and other conditions, it will be important to further research the drug delivery system of existing drugs, including other diseases.
As described above, the basic studies regarding novel methods for hypertension treatment will continue to develop, and the author expects a future in which a new way to treat hypertension that does not require daily medication will become widespread.
References
Coste B, Delmas P. PIEZO ion channels in cardiovascular functions and diseases. Circ Res. 2024;134:572–91.
Wang H, Yuan Z, Wang B, Li B, Lv H, He J, et al. COMP (cartilage oligomeric matrix protein), a novel Piezo1 regulator that controls blood pressure. Hypertension. 2022;79:549–61.
Fei L, Xu M, Wang H, Zhong C, Jiang S, Lichtenberger FB, et al. Piezo1 mediates vasodilation induced by acute hyperglycemia in mouse renal arteries and microvessels. Hypertension. 2023;80:1598–610.
Harraz OF, Klug NR, Senatore AJ, Hill-Eubanks DC, Nelson MT. Piezo1 is a mechanosensor channel in central nervous system capillaries. Circ Res. 2022;130:1531–46.
Choi D, Park E, Yu RP, Cooper MN, Cho IT, Choi J, et al. Piezo1-regulated mechanotransduction controls flow-activated lymphatic expansion. Circ Res. 2022;131:e2–e21.
Hirata Y, Nomura K, Kato D, Tachibana Y, Niikura T, Uchiyama K, et al. A Piezo1/KLF15/IL-6 axis mediates immobilization-induced muscle atrophy. J Clin Invest. 2022;132:1–13.
Bartoli F, Debant M, Chuntharpursat-Bon E, Evans EL, Musialowski KE, Parsonage G, et al. Endothelial Piezo1 sustains muscle capillary density and contributes to physical activity. J Clin Invest. 2022;132:e141775.
Matrongolo MJ, Ang PS, Wu J, Jain A, Thackray JK, Reddy A, et al. Piezo1 agonist restores meningeal lymphatic vessels, drainage, and brain-CSF perfusion in craniosynostosis and aged mice. J Clin Invest. 2023;134:e171468.
Carrisoza-Gaytan R, Mutchler SM, Carattino F, Soong J, Dalghi MG, Wu P, et al. PIEZO1 is a distal nephron mechanosensor and is required for flow-induced K+ secretion. J Clin Invest. 2024;134:e174806.
He Y, Deng B, Liu S, Luo S, Ning Y, Pan X, et al. Myeloid Piezo1 deletion protects renal fibrosis by restraining macrophage infiltration and activation. Hypertension. 2022;79:918–31.
Ogino S, Yoshikawa K, Nagase T, Mikami K, Nagase M. Roles of the mechanosensitive ion channel Piezo1 in the renal podocyte injury of experimental hypertensive nephropathy. Hypertens Res. 2024;47:747–59.
Ochiai K, Mochida Y, Nagase T, Fukuhara H, Yamaguchi Y, Nagase M. Upregulation of Piezo2 in the mesangial, renin, and perivascular mesenchymal cells of the kidney of Dahl salt-sensitive hypertensive rats and its reversal by esaxerenone. Hypertens Res. 2023;46:1234–46.
Harrison DG, Patrick DM. Immune mechanisms in hypertension. Hypertension. 2024;81:1659–74.
Liang H, Liu B, Gao Y, Nie J, Feng S, Yu W, et al. Jmjd3/IRF4 axis aggravates myeloid fibroblast activation and m2 macrophage to myofibroblast transition in renal fibrosis. Front Immunol. 2022;13:978262.
Huang M, Wang Q, Long F, Di Y, Wang J, Zhun Zhu Y, et al. Jmjd3 regulates inflammasome activation and aggravates DSS-induced colitis in mice. FASEB J. 2020;34:4107–19.
He C, Larson-Casey JL, Gu L, Ryan AJ, Murthy S, Carter AB. Cu,Zn-superoxide dismutase-mediated redox regulation of Jumonji domain containing 3 modulates macrophage polarization and pulmonary fibrosis. Am J Respir Cell Mol Biol. 2016;55:58–71.
Gao Y, Yu W, Song J, Nie J, Cui Z, Wen S, et al. JMJD3 ablation in myeloid cells confers renoprotection in mice with DOCA/salt-induced hypertension. Hypertens Res. 2023;46:1934–48.
Norlander AE, Madhur MS, Harrison DG. The immunology of hypertension. J Exp Med. 2018;215:21–33.
Wilck N, Matus MG, Kearney SM, Olesen SW, Forslund K, Bartolomaeus H, et al. Salt-responsive gut commensal modulates T(H)17 axis and disease. Nature. 2017;551:585–9.
Kim JY, Lee S, Jang S, Kim CW, Gu BH, Kim M, et al. T helper cell polarity determines salt sensitivity and hypertension development. Hypertens Res. 2023;46:2168–78.
Mailankody S, Devlin SM, Landa J, Nath K, Diamonte C, Carstens EJ, et al. GPRC5D-targeted CAR T cells for myeloma. N. Engl J Med. 2022;387:1196–206.
Arcangeli S, Bove C, Mezzanotte C, Camisa B, Falcone L, Manfredi F, et al. CAR T cell manufacturing from naive/stem memory T lymphocytes enhances antitumor responses while curtailing cytokine release syndrome. J Clin Invest. 2022;132:e150807.
Jaspers JE, Khan JF, Godfrey WD, Lopez AV, Ciampricotti M, Rudin CM, et al. IL-18-secreting CAR T cells targeting DLL3 are highly effective in small cell lung cancer models. J Clin Invest. 2023;133:e166028.
Mackensen A, Müller F, Mougiakakos D, Böltz S, Wilhelm A, Aigner M, et al. Anti-CD19 CAR T cell therapy for refractory systemic lupus erythematosus. Nat Med. 2022;28:2124–32.
Rurik JG, Tombácz I, Yadegari A, Méndez Fernández PO, Shewale SV, Li L, et al. CAR T cells produced in vivo to treat cardiac injury. Science. 2022;375:91–96.
Baker DJ, Arany Z, Baur JA, Epstein JA, June CH. CAR T therapy beyond cancer: the evolution of a living drug. Nature. 2023;619:707–15.
Tamura K, Azushima K, Kinguchi S, Wakui H, Yamaji T. ATRAP, a receptor-interacting modulator of kidney physiology, as a novel player in blood pressure and beyond. Hypertens Res. 2022;45:32–39.
Patel KP, Katsurada K, Zheng H. Cardiorenal syndrome: the role of neural connections between the heart and the kidneys. Circ Res. 2022;130:1601–17.
Sotozawa M, Kinguchi S, Wakui H, Azushima K, Funakoshi K, Nakajima W, et al. Enhancement of angiotensin II type 1 receptor-associated protein in the paraventricular nucleus suppresses angiotensin II-dependent hypertension. Hypertens Res. 2024;47:67–77.
Taguchi S, Azushima K, Yamaji T, Suzuki T, Abe E, Tanaka S, et al. Angiotensin II type 1 receptor-associated protein deletion combined with angiotensin II stimulation accelerates the development of diabetic kidney disease in mice on a C57BL/6 strain. Hypertens Res. 2024;47:55–66.
Zhu Y, Chu Y, Wang S, Tang J, Li H, Feng L, et al. Vascular smooth muscle TRPV4 (transient receptor potential vanilloid family member 4) channels regulate vasoconstriction and blood pressure in obesity. Hypertension. 2023;80:757–70.
Adapala RK, Katari V, Kanugula AK, Ohanyan V, Paruchuri S, Thodeti CK. Deletion of endothelial TRPV4 protects heart from pressure overload-induced hypertrophy. Hypertension. 2023;80:2345–56.
Wen X, Peng Y, Peng Y, Zhu Y, Yu F, Geng L, et al. Aortic smooth muscle TRPV4 channels regulate vasoconstriction in high salt-induced hypertension. Hypertens Res. 2023;46:2356–67.
Hu X, Du L, Liu S, Lan Z, Zang K, Feng J, et al. A TRPV4-dependent neuroimmune axis in the spinal cord promotes neuropathic pain. J Clin Invest. 2023;133:e161507.
Avolio E, Katare R, Thomas AC, Caporali A, Schwenke D, Carrabba M, et al. Cardiac pericyte reprogramming by MEK inhibition promotes arteriologenesis and angiogenesis of the ischemic heart. J Clin Invest. 2022;132:e152308.
Quijada P, Park S, Zhao P, Kolluri KS, Wong D, Shih KD, et al. Cardiac pericytes mediate the remodeling response to myocardial infarction. J Clin Invest. 2023;133:e162188.
Alex L, Tuleta I, Hernandez SC, Hanna A, Venugopal H, Astorkia M, et al. Cardiac pericytes acquire a fibrogenic phenotype and contribute to vascular maturation after myocardial infarction. Circulation. 2023;148:882–98.
Lin SL, Kisseleva T, Brenner DA, Duffield JS. Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Am J Pathol. 2008;173:1617–27.
Duffield JS. Cellular and molecular mechanisms in kidney fibrosis. J Clin Invest. 2014;124:2299–306.
Ito H, Hirose T, Sato S, Takahashi C, Ishikawa R, Endo A, et al. Pericyte detachment and renal congestion involve interstitial injury and fibrosis in Dahl salt-sensitive rats and humans with heart failure. Hypertens Res. 2023;46:2705–17.
Dai S, Zhao L, Wang G, Chen C, Li C, Xiao B, et al. Celiac ganglia neurolysis suppresses high blood pressure in rats. Hypertens Res. 2023;46:1771–81.
Kamata K, Kinoshita M, Kinoshita I, Imai H, Ogura T, Matsumoto H, et al. Efficacy of EUS-guided celiac plexus neurolysis in combination with EUS-guided celiac ganglia neurolysis for pancreatic cancer-associated pain: a multicenter prospective trial. Int J Clin Oncol. 2022;27:1196–201.
Azizan EAB, Drake WM, Brown MJ. Primary aldosteronism: molecular medicine meets public health. Nat Rev Nephrol. 2023;19:788–806.
Wang X, Luo T, Yang Y, Zhou Y, Hou J, Wang P. Unilateral chemical ablation of the adrenal gland lowers blood pressure and alleviates target organ damage in spontaneously hypertensive rats. Hypertens Res. 2023;46:2693–704.
Tuttle KR, Hauske SJ, Canziani ME, Caramori ML, Cherney D, Cronin L, et al. Efficacy and safety of aldosterone synthase inhibition with and without empagliflozin for chronic kidney disease: a randomised, controlled, phase 2 trial. Lancet. 2024;403:379–90.
Huff AL, Jaffee EM, Zaidi N. Messenger RNA vaccines for cancer immunotherapy: progress promotes promise. J Clin Invest. 2022;132:e156211.
Nakagami H. Challenges in the development of novel therapies, vaccines and siRNAs for the treatment of hypertension. Hypertens Res. 2023;46:1812–5.
Ma Z, Mao C, Chen X, Yang S, Qiu Z, Yu B, et al. Peptide vaccine against ADAMTS-7 ameliorates atherosclerosis and postinjury neointima hyperplasia. Circulation. 2023;147:728–42.
Ke F, Kuang W, Hu X, Li C, Ma W, Shi D, et al. A novel vaccine targeting β1-adrenergic receptor. Hypertens Res. 2023;46:1582–95.
Jana BA, Shivhare P, Srivastava R. Gelatin-PVP dissolving microneedle-mediated therapy for controlled delivery of nifedipine for rapid antihypertension treatment. Hypertens Res. 2024;47:427–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kitada, K. Hypertension research 2024 update and perspectives: basic research. Hypertens Res (2024). https://doi.org/10.1038/s41440-024-01878-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41440-024-01878-2
- Springer Nature Singapore Pte Ltd.